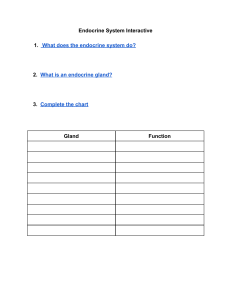
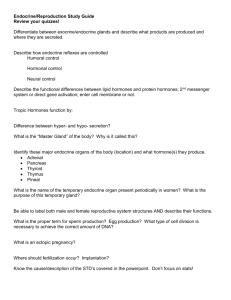
ENDOCRINE SYSTEM • OUTLINE • Introduction • Secretions of endocrine cells • Distribution of endocrine cells Introduction • Endocrine tissue is made up essentially of cells that produce secretions which are poured into the blood • The secretions of endocrine cells are called hormones • Endocrine organs co-ordinate and control the metabolic activities and the internal environment of the body; along with the autonomic nervous system • Endocrine tissues are highly vascular • The secretory pole of an endocrine cell is toward the wall of a capillary (sinusoid). Secretions of the endocrine cells • Secretions of the endocrine cells are called hormones • Hormones travel through blood to target cells • Hormones influence the function of target cells • Some hormones act only on one organ or on one type of cell, while other hormones may have widespread effects Types of hormones • Hormones belong to four main types; based on their chemical structure • A. amino acid derivatives eg; adrenalin, nor-adrenalin and thyroxine • B. small peptides eg; encephalin, vasopressin, and thyroid releasing hormone. • C. proteins eg; insulin, parathormone and thyroid stimulating hormone. • D. steroids eg; progesterone, estrogens, testosterone and cortisol Distribution of endocrine cells • The cells are distributed in 3 different ways: • 1. some organs are entirely endocrine in function. They are called endocrine glands(ductless gland) eg; hypophysis cerebri (or pituitary), the pineal gland, the thyroid gland, the parathyroid glands and the suprarenal(or adrenal) glands • 2. groups of endocrine cells may be present in organs that have other functions. Eg; the islets of the pancreas, the interstitial cells of the testes and the follicles and corpora lutea of the ovaries. Also some cells of the kidneys, thymus and the placenta • 3. isolated endocrine cells may be distributed in the epithelial lining of an organ; as seen in the gut(endocrine cell of the gut), also in the epithelium of the respiratory passages. Cells in other locations in the body produce amines that have endocrine functions. Many of these amines also act as neurotransmitters or neuromodulators and are grouped together as neuroendocrine system or APUD cell system. • APUD represents amine precursor uptake and decarboxylation cell system. HYPOPHYSIS CEREBRI • Also called pituitary gland • Approximately the size of a pea • It is suspended from the floor of the third ventricle of the brain by a narrow funnel shaped stalk called the infundibulum • It lies in a depression on the upper surface of the sphenoid bone, called sella turcica • One of the most important endocrine glands and produces several hormones some of which profoundly influence the activities of other endocrine tissues and is sometimes referred as ‘master endocrine glands’ • Pituitary gland activity is influenced by hypothalamus and pineal body PINEAL GLAND • The pineal gland or body is a small piriform structure present in relation to the posterior wall of the third ventricle of the brain • It is called epiphysis cerebri • The name pineal is b/cos it was taught to be a vestigial organ of no functional importance, but now it is known to be an endocrine gland of great importance Microscopic features • Pinealocytes : • The cells of the pineal gland are the pinealocytes • Each cell has a polyhedral body containing a spherical oval or irregular nucleus • The cell body gives off long processes with expanded terminal buds that end in relation to the walls of capillaries and in relation to the ependymal of the third ventricle • The cell bodies of the pinealocytes contain; granular and agranular endoplasmic reticulum, a well developed golgi complex and many mitochondria • Canaliculate lamellar bodies may be present; which is an organelle of unusual structure made up of groups of microfibrils and perforated lamella • The processes of pinealocytes contain numerous mitochondria • The terminal buds contain vesicles in which there are monamines and polypeptide hormones • Neurotransmitter; gamma-amino-butyric acid is also present Hormones produced by pinealocytes • The pinealocytes produce • 1. melatonin; (so called because it causes changes in skin colour in amphibian). It is an amino acid • 2. serotonin (5-hydroxytryptamine). This is a precursor of melatonin and is present within the pineal gland. Interstitial cells • The pinealocytes are separated from one another by neuroglial cells that resemble astrocytes in structure • These are the interstitial cells • They lie in proximity to the blood vessel and pinealocytes • Recent studies show that the organ does not degenerate with age Thyroid gland • Thyroid is a bi-lobed gland • Each lobe is situated on either side of the trachea below larynx, in the lower neck • The 2 lobes are connected to each other by isthmus in front of the trachea • It stores large quantity of its hormonal secretion extracellularly as colloid Structure of thyroid gland • The gland is covered by a fibrous capsule • Septa extending into the gland from the capsule divide it into lobules Microscopic examination • Each lobule is seen to be made up of an aggregation of follicles • Each follicle is lined by follicular cells, that rest on the basement membrane • The follicle has a cavity which is filled by a homogeneous material called colloid(this appears pink in h&e stained sections • The spaces between the follicles are filled by a stoma • The stroma comprises of delicate connective tissue in which are numerous capillaries and lymphatics. The capillaries lie in close contact with the walls of follicles • Apart from follicular cells the thyroid gland contains C-cells or parafollicular cells • These cells intervene between the follicular cells and the basement membrane Follicular cells • Vary in shape depending on the level of their activity • At an average level of activity, the cells are cuboidal and the colloids in the follicles is moderate in amount • When the cells are inactive or resting; the cells are squamous or flat and the follicles are distended with abundant colloid • Thirdly, when the cells are highly active, they become columnar and the colloid is scanty • The follicular cells show the presence of apical microvilli, abundant granular endoplasmic reticulum, a prominent supranuclear golgi complex, lysosomes, microtubules and microfilaments. The apical part of the cell contains many secretory vacuoles • The activity of follicular cells is influenced by thyroid stimulating hormones(TSH or thyrotropin) produced by the pituitary gland • Also sympathetic stimulation may also influence the activity of follicular cells Hormones secreted by follicular cells • Follicular cells secret 2 hormones; • 1. triodothyronine or T3 • 2. tetraiodothyronine, T4 or thyroxine • The essential constituent of these hormones is iodine. • T3 is more active than T4 Synthesis of thyroid hormone • The synthesis and release of thyroid hormone takes place in 2 phases • Phase 1; • Thyroglobulin, a glycoprotein is synthesized by granular endoplasmic reticulum and packed into secretory vacuoles in the golgi complex • The vacuoles travel to the luminal surface where they release thyroglobulin into the follicular cavity by exocytosis • Here the thyroglobulin combines with iodine to form colloid • Colloid is iodinated thyroglobulin • Phase 2; • Particles of colloid are taken back into the cell by endocytosis • Within the cell, the iodinated thyroglobulin is acted upon by enzymes present in the lysosomes releasint T3 and T4 which pass through the cell and are released into the blood • Hormones produced in the thyroid gland is mainly T4 • Percentage of produced T3 is less than 10% • T4 is converted to T3 in the liver and kidneys by removal of one iodine molecule • Circulating T4 and T3 are bound to thyroxine binding globulin; a protein(TBG) • The bound form is inactive(not active) C- cells (Parafollicular cells) • Also called clear cells or light cells • Cells are polyhedral, with oval eccentric nuclei • Typically lie between the follicular cells and their basement membrane • May also lie between adjoining follicular cells, but do not reach the lumen • May lie in connective tissues between follicles in some species • C-cells are included in APUD cell system and share similar features Hormones secreted • C-cells secrete thyrocalcitonin • This hormone has action opposite that of parathyroid hormone on calcium metabolism • When the serum calcium level is high, this hormone lowers the calcium level by suppressing the release of calcium ions from the bone. This is achieved by suppressing bone resorption by osteoclasts clinicals • Hyperthyroidism; a hypermetabolic clinical and biochemical state caused by excess production of thyroid hormones. Also called thyrotoxicosis. More common in females. Associated with rise in T3 and T4 levels, though increase in T3 level is higher than T4. • Hypothyroidism; hypometabolic clinical state resulting from inadequate production of thyroid hormones for prolonged periods, or rarely from resistance of the peripheral tissues to the effects of thyroid hormones. • Clinical manifestation depends on age of onset of disorder; there are 2 forms • Cretinism; which occurs during infancy and childhood • Myxedema; which is the adulthood hypothyroidism • Graves’ disease; also known as Basedow’s disease, primary hyperplasia, exophthalmic goiter and diffuse toxic goiter. More frequent between 30 and 40years. More in females. This is characterized by a triad of features; • Hyperthyroidism(thyrotoxicosis) • Diffuse thyroid enlargement • Ophthalmopathy PARATHYROID GLANDS • So called because they lie in close relationship to the thyroid gland • There are 2 parathyroid glands; one superior and one inferior, on either side; • There are 4 glands in all • Sometimes; there may be as many as 8parathyroids Structure of parathyroid gland • Each gland has a connective tissue capsule from which some septa extend into the gland substance. • Within the gland a network of reticular fibers supports the cells • Many fat cells, adipocytes, are present in the stroma • The parenchyma of the gland is made up of cells that are arranged in cords • Numerous sinusoids lie in close relationship to the cells Cells of parathyroid glands • 2 main types; • 1. chief cells (or Principal cells) • 2. oxyphil cells(eosinophil cells) Chief cells • Much more numerous • Seen to be small round cells with vesicular nuclei when viewed with light microscope • Cytoplasm is clear (either mildly eosinophil or basophil) • Cell sometimes accumulates glycogen and lipids and looks clear • 3 types of chief cells have been described; light , dark and clear • Active chief cells; have abundant granular endoplasmic reticulum and well developed golgi complexes • Both active and inactive cells contain glycogen • The chief cells produce the parathyroid hormones or parathormone • The hormone tends to increase the level of serum calcium level by; • Increasing bone resorption through stimulation of osteoclastic activity • From renal tubule by inhibiting phosphate resorption • Enhancing calcium absorption from the gut Oxyphil cells • Much larger than the chief cells • Contain granules that stain strongly with acid dyes • Nuclei smaller and stain more intensely than those of chief cells • Absent in the young and appear a little before the age of puberty Clinicals • Hyperparathyroidism; hyperfunction of the parathyroid glands due to excessive production of parathyroid hormones • Classified into 3types; • Primary hyperparathyroidism; oversecretion of parathyroid hormone due to the disease of parathyroid gland • Secondary hyperparathyroidism; due to disease in other parts of the body • Tertiary hyperparathyroidism; from secondary hyperplasia after removal of the cause of secondary hyperplasia • Hypoparathyroidism; • Deficiency or absence of parathyroid hormone secretion causes hypoparathyroidism. • Thank you for your attention.