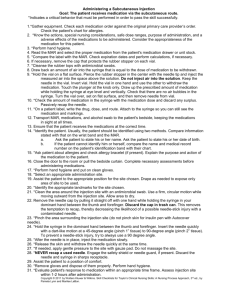
Staple removal and dressing change - HH Introduce Check doctors order, and confirm with patient name tag See if patient needs analgetics for pain Position and drape patient appropriately only exposing necessary area Patient is comfortable and appropriate position Gather all supplies. Open sterile dressing tray away from me (garbage) Green forceps sterile drape shiny side down, hand in front Put forceps where you can reach them with green Place garbage bag and tape. In hole at bedside table Open up more sterile gause and place in dressing tray ABD pad put in sterile field Open staple remover (on edge) Steri strips Put sterile saline in tray on gause dressing tray closer to patient Remove tape parallel to skin – move away and see it amount and charertictics Apply clean gloves top to bottom, most contaminated to least. Do not have to dry if overly wet, not to wet not to dry Now Dry, Assess using REEDA Now remove staples, does not matter if you start at top or bottom. Flat part parallel to patient skin. Both ends underneath before you squeeze. STAPLES SHOULD go in sharps container but will put in dressing kit knowing that is not contaminated. Only take every other staple. If concerned about incision advise reassess approximation looks well approximated to continue If need to embrace hand on patient abdomen place 2.5 cm away from incision Place stable remover in same container as containers. Now clean and dry the incision again. Do not reassess all only reassess approximation. Apply sterristrips take tab on top and one at a time and place inside boarder, pull to support boarder place gauze over top. Can touch with hand for abd dressing on blue side. See how patient tolerates it. Place tape across. Place tape across top with date and time and initials. Suture removal and dressing change - HH - Introduce - Check doctors order, and confirm with patient name tag - See if patient needs analgetics for pain - Position and drape patient appropriately only exposing necessary area - Patient is comfortable and appropriate position - Gather all supplies. Open sterile dressing tray away from me (garbage) Green forceps sterile drape shiny side down, hand in front Put forceps where you can reach them with green Place garbage bag and tape. In hole at bedside table Open up more sterile gause and place in dressing tray ABD pad put in sterile field Open staple remover (on edge) Steri strips Put sterile saline in tray on gause dressing tray closer to patient Remove tape parallel to skin – move away and see it amount and charertictics Apply clean gloves top to bottom, most contaminated to least. Do not have to dry if overly wet, not to wet not to dry Now Dry, Assess using REEDA Use silver forceps and suture removal scissors (curved hook) Everyother cuture first Grasp knot with forceps and slide blade underneath and pull away from patient and as close to the skin as possible. And grasp the knot and pull it across and out. With scissors grasp knot and cut with knot Now clean and dry the incision again. Do not reassess all only reassess approximation. Apply sterristrips take tab on top and one at a time and place inside boarder, pull to support boarder place gauze over top. Can touch with hand for abd dressing on blue side. See how patient tolerates it. Place tape across. Place tape across top with date and time and initials Dressing change with Jackson Pratt Drain Removal. After removal of dressing – assess drainage and REEDA – patient bare three gs gloves green forceps and and do HH and face shield Clean whatever is in the top first either incision or stip – most to least 5 swipes DRAIN - Closest to drain in circular motion, use three gauze working your way out. THAN DRY BOTH INCION AND DRAIN - Access both drain and incision using REEDA – for approximation note how the drain is held in place NOW YOU CHANGE THE DRAIN - Place blue pad underneath drain , careful not to touch bluepad with it incision - Need pink sterile container, take plug out and slowly remove it. (if contacted tip you need to wipe with alcohol swab for 15 secs) empty into the container. If only emptying drain than squeeze than place back. If removing drain than no need for suction. TO remove the drain you need to wear sterile gloves - Use bottom part of table - ONLY TOUCH WHATS IN THE STERILE FIELD - Grab 4x4 gauze and place near drain site and apply counter pressure – part of it will touch skin and pull with other hand and apply firm and steady pressure and pull. - Clean drain site if required and now that your gloves are not sterile you can move back and touch the tweezers. - Apply dressing over incision and drain site - Silver forceps go in sharps container and rest in garbage. - Ask patient if they are comfortable - Thank them for their time. Dressing Change with HEMOVAC drain removal - Clean gloves Face masks also after you remove dressing. And before you put gloves Gently remove suction, place blue pad, plug out and place hemovac drain out and put in cup. Inspect the drainage for amount, color and type of drainage. Non dominant hand with gauze on drain and dominant pull Irrigation and Packing a Complex Wound - check charting for previous dressing changes to see what to expect for irrigation and incision - drainage, etc. appropriate position. Raise the head and lower the feet. Apply blue pad at the base, can place kidney basin at bottom Sterile dressing tray Sterile cotton applicator to measure complex wound – sterile cue tip in sterile field, and keep the package for measure and culturet container outside. To irrigate keep bottle on side Use normal saline in tray. 35 mil sringe and 19 gauage needle attach them together after removing the cover off the syringe and place in sterile field 250 ml bottle into sterile dressing tray Remove dressing, and assess the drainage for color consistency and amount PUT on face shield Irrigate top to bottom and most to least the 60 mil twist of top and lip a bit and squeeze a bit 2.5 cm from the wound. ZIG ZAG , continue until the stream runs clean 35 ml syringe, withdraw amount from sterile container and same fashion top to bottom, zig zag steady steam - - And put outside sterile field. Now clean outside top to bottom, only one gauze per swipe 3 times on each side. Sterile gauze and put it inside the patient and hold it there you want the wound bed not to wet and not to dry. Dry the edges of the wound MEASURE Measure -Took packet and measured the length with the swab and width and depth looking for exudate (drainage on packing that she took out) and appearance (what the wound bed looks like) – I can see that it is nice red granulation tissue with new epithelial Suffering – assess the comfort level before during and after - Undermining or tunneling Revaluating – based on previous documentation and the documentation that I do today Edges – not attached open wound bed - Now you do a culture sensitivity swab – sterile cue tip – choose area of healthy looking tissue and put a little bit of pressure and rotate in a 1 cm square diameter enough to get fresh cells and exudate out - Take culture tube package out and take off tube lib and place the swab inside. - PACK wound - Remove face shield use sterile gloves – use 4x4 gauze in sterile field and put in saline and ling it out and open it back up. Then gently place it inside the mound bed and make sure not to touch the wound with fingers. You fluff it you do not stuff it. Than grab another gauze from sterile field and place over top. Date and time etc. and put patient in comfortable position. - Indwelling Male Catheterization - HH, doctors orders, drape, privacy. - Supine, with legs slightly abducted - Inspect perineal area make sure clean and dry if not than clean with soap and water - Also assessing urinary status and when they voided last and also previous medical history and possible surgeries in the past that may make the insertion complicated. 1. Place waterproof pad underneath legs 2. HH , get supplies ready (urinary bag, universal catheterization kit, sterile gloves, and 14 French catheter which is normal for adult male) 3. Open urinary drainage bag and place it nearby on bed– has sterile cap at the end 4. Open catheter bag and place it on the table it has a inside bag and tape it to table so you can grab the inside with sterile gloves 5. Open Catheterization kit and using wrapping as garbage bag and place it nearby on bed 6. For the kit – pull outside flap away from me and than outside flap and last flap towards – do not touch cath 7. Put on sterile gloves - on slide out tray 8. Put drape and grasp with thumb and put back of hands on sterile part and roll it around hands, thumb on opposite shiny side 9. Place underneath the legs and penis and overtop the thighs 10. Take out cath and only touch sterile inside piece package and take out and garbage rest 11. Take kit and place it on bed near patient as it is sterile from outside 12. Take sterile water (10 ml) and connect to balloon port 13. Sterile bedadine on cotton balls to clean 14. Lubricate catheter 12.5 to 17.7 5 cm and rid of lubricant and set in tray 15. Once you touch penis your dominant hand it no longer sterile and hold by shaft if foreskin retract it 16. Use sterile bedadine cotton ball clean from meatus to glans with green twizzer – Repeat 3 times for total of 4 cotton balls dispose of green twizzer 17. Take catheter out of sterile kit and insert into urethral meatus – I am going to insert it for 17 – 22.5 cm or until I get urine return and than advance 2.5 cm and slowly inflate the balloon and tip of catheter stays on top of collection container 18. Release penis connect connect drainage bag 19. Dispose urine kit and dispose it 20. HH and Change gloves 21. Take tape and secure cath to upper thigh and take cath drainage and place below level of bladder and not on bed rail 22. Help perform peri care with wet soapy wipes, starting from meatus and work my way down and dry peri wipe 23. Take away all of garbage and do HH and hep pt cover up and get into comfortable position Indwelling Female Catheterization 1. Grab 2 14 french cath bags 2. Position patient in dorsal recumbent position with knees flexed and knees relaxed, 3. HH, doctors orders, drape, privacy. 4. Supine, with legs slightly abducted 5. Inspect perineal area make sure clean and dry if not than clean with soap and water Also assessing urinary status and when they voided last and also previous medical history and possible surgeries in the past that may make the insertion complicated. 6. HH put on clean gloves and put water proof pag underneath – take off gloves 7. Take out cath drain bag on bed 8. Open outside cath bag and tape to table, 9. take out universal cath tray and pull first away and side side nad than towards use bag as garbage 10. put on sterile gloves 11. use sterile drap with shiny side down and tuck under thighs, ensuring not to contaminate sterile gloves 12. take out cath and put in cath kit and place near bed 13. Take bed solution and put on cotton balls 14. Attach sterile water syringe to balloon port 15. Open lubricant and lub 2.5 cm to 5 cm and throw out 16. Retract labia and use cotton ball with green thingy first far side labia, than close side each with different swab (Top to bottom) than last one urethral meatus top to bottom 17. Take cath and insert in urethral meatus and insert 5-7.5 cm or until I see urine return and once I see urine return than I will advance it another 2.5 cm 18. With urine flowing I am going to inflate with all 10 ml and connect to urine drainage bag with the end staying sterile – note color and characteristic of urine 19. Remove extra garbage aside and perform peri care and remove blue pad – with wet peri wipe clean from cleanest to dirtiest. 20. Teaching – drainage bag should be below the level of waist and discuss how to solve different problems with urinary issues. look at potter for more education 21. Place drainage below the level of waist and assist patient to comfortable position Specimen Collection via Indwelling Catheter 1. HH, introduce, 2. Check name band and confirm with doctors orders 3. Explain the procedure 4. Aseptic technique Gather supplies (Green top for urine culture and sensitivity (min 3ml) and clear one for urine analysis (requires 4 ml) , cath clamps, 12 ml syringe, alcohol swabs 5. Normally done overtop of toilet demo over blue pad, take supplies to bed side and expose to patient tubing making sure there is urine 6. Clamp tubing distal to port for urine to collect 7. Clean port with alcohol swab for 15 sec 8. Ensuring it does not touch anything else, take 12 ml sringe and put in port and draw urine, requires 9. Disconnect and unclamp and cover patient and take to work station with blue pad 10. Over graduated cylinder take out green tube and spray gently spray on each side roughly 3 ml each side and shake off excess and and set off green one to side for urine analysis – open cap place with sterile side up. 6 ml in container and put cap back on 11. Label and send to lab Removal of indwelling catheter and emptying a urine drainage bag Male 1. 2. 3. 4. HH, double check doctors order and with wrist band Introduce and explain procedure to patient. First empty bag, use gloves and face shield Take graduated cylinder and go below the level of the bag and keep end sterile and then reclasp silver one 5. Measure urine and inspect it and dispose of it in appropriate place 6. Remove gloves than face shield and HH 7. Put on new gloves (grab 12 ml syringe, blue pad, and peri wipes) 8. Expose patient and take supplies towards bed 9. Place blue pad underneath legs 10. Position pt in supine with legs slightly abducted (for men) 11. Take drainage bag and place bed and remove tape on thigh 12. Take 12 ml syringe and attach to balloon port check chart and but also says on the tube port 13. Encourage it to drain (will drain itself) 10 ml back 14. Disconnect 15. Explain before you remove – take deep breath in and when they exhale you take out – it helps them to relax 16. Hold penis and take it out gently and wrap it in blue pad and dispose 17. Perform peri care – working from urethral meatus down to shaft and dry 18. Cover pt back and assist to comfortable position Intermittent Male Catheterization 1. Same shit as before 2. Clean gloves etc 3. Put water proof pad underneath 4. Take off and do hh and open catheterization tray 5. Put on sterile gloves 6. Put drape under thighs 7. Do not use specimen containers – do not use bedadine swab sticks and add cotton swabs 8. Remove sterile gloves add cotton swabs before 9. Lub 12.5- 17.5? cm 10. Clean with swabs – 3 times 11. Insert cath 17-22.5 cm – end of cath in tray – when urine out than in and let flow and empty fully than let them exhale and remove cath 12. Remove with blue pad 13. Measure urine and note color and characteristics. 14. Clean peri care Intermittent Female Catheterization 1. Put sterile cotton balls to tray 2. Put on sterile gloves 3. Put drape down 4. Than move tray bed side 5. Insert 5 – 7.5 cm after flow advance 2.5 cm 6. Can educate patient while flow is going Vial Reconstitution - Step 1 HH Step 2 gather appropriate supplies, (powered medication, dilutent, blunt needle, syringe, alcohol swab Step 3 check package insert for dilutent and volume Step 4 -remove caps on both vials and alcohol swab for 15 secs and allow to dry Step 5 – attach needle to syringe – pull back air equivalent for amount Step 6 – vial on flat surface and insert needle on rubber seal and inject air into vial airspace Step 7 – invert vial and draw out diluent – tip on needle stays below fluid level Step 8 – Pull back on air syringe and push access air bubbles out with putting it 90 degrees Step 9 – Insert tip of needle in the powder and inject. Removed needle Step 10 – Put needle back by placing it flat on the table Step 12 – Roll vial in palm of hand Step 13 – dispose of needle in sharps Step 14 – Vial is ready Oral Medications Step 1 – Introduce and do HH Step 2 – check for allergies – check band Step 3 – Check any contraindications (ability to swallow, nausea or vomiting) Step 4 – Go to medication room to prepare order – CHECK MAR AGAINST PHYSICIAN ORDER – confirm name and medication name – dose, route, time & Frequency. Also check for allergies on MAR and doctor’s order. Step 5 – using nursing central or drug book check for appropriate medication dosage range – safe range state. Step 6 – Ensure appropriate assessment prior to administering medication – such as lab reports, blood glucose, vital signs or access pain heart rate. Step 7 – Clean technique – 1 check – when you pull out mar – COMPARE PACKAGE WITH MAR NAME AND DOSE Step 8 – ENSURE EACH TABLET IS THE RIGHT DOSE – if it needs to be cut make sure it is scored. And cut appropriately. PUT ON GLOVES AND SPLIT WITH CLEAN TECHNIQUE Step 9 – Prepare liquid medication – 1st check Label on bottle with MAR and correct medication calculation Step 10 – Gently shake container and remove cap to not contaminate inside of bottle – put bottle with label in palm – if drawing less 10 ml than syringe – if more than 10 ml than syringe or cup – hold at eye level and fill– wipe lip of bottle – and recap Step 11- label medication cup – with the medication and the dose – CHECK 2 – compare medication cup to bottle Step 12 – CHECK 2 – compared all medication with labels and MAR 6/10 done Step 13 – keep meds that require different assessments from meds that do not Step 14 – Go to pt bedside with MAR and medications and check name band and date of birth Step 15 – assist pt to siting position at edge of bed or raise head of bed Step 16 – Do appropriate assessments and provide appropriate education and allow patient the right to refuse. – Do you have any questions about the medications Step 17 – Take medication out of packaging and compare with MAR – 3rd and final check – offer pt water to take medication and offer in medication cup. Step 18 – stay at bedside until pt has swallowed all medication. Step 19 – Close ill be back to check on you Step 20 – document – when the medication was administered including the4 digit time and include initial and designation. Topical Medications Part 3 – Preparing Unit dose - ONLY OPEN UNIT WRAPPER WHEN YOU ARE READY TO ADMINISTER Do not administer medication if less than 60 beats per min and do not administer and notify provider REMOVING MEDICATION tablet from a bottle Splitting Tablet medication - MAKE SURE TO CHECK EXPIRATION DATE - HH, GLOVES - Remove from package – - CHECK AGAIN against mar Put one half in package and one is disgarded Preparing Liquid Medication - READ AT BOTTOM OF MENICSUS – WIPE LIP OF BOTTLE - Compare again with MAR Administering Oral Medications - Slower onset – - Purpose Oral and Topical Medications Part 8 – unexpected medications - Pill falls on floor it is wasted - Not leave the medication by bedside – bring medication back later - This doesn’t look like the pill I took yesterday – recheck mar with administration time, Gastric Tube - Liquid medication Administering Medications via a Gastric Tube - Clamp tube and remove cap - Attach syringe and aspirate – should be no residual – apply clamp again and remove syringe – remove plunger from syringe – reinsert syringe without plunger and pour 30 ml unclamp and infuse via gravity than add medication. And clamp tube. Than pour 10 ml in same medication cup and pour in syringe and unclamp. Shake liquid medication and pour in. unclamp and administer – reclamp and pour in some water and unclamp. Reclasp – Now pour 60 ml in syringe and unclamp to allow water to flush and clamp and remove - Document – Rectal Suppository - HH, arm band - Turn onto side. - Gloves and lubricate both suppository and gloves and take a few deep breaths. - Insert suppository beyond the internal sphincter – 4 inches and 2 inches in infants and children - Remain still for the next 5 and it has to remain in place up to 30-45 min Metered-Dose Inhaler - MDI – handheld inhaler that distributes mist – lungs - Listen to lungs sounds and pulse rate. Allergies Attach mdi to spacer Depress canister - Inhale slowly and deeply and hold for 10 seconds and exhale slowly with purse lips 2 puffs-1 -5 min – Gargle and rinse after using MDI – related to dry mouth. Clean MDI and spacer Confirm administration of medication Administering Medication via a Small – Volume Nebulizer - Check chest and pulse – Raise bed and head of bed - Remove cup of nebulizer from and place medication in cup of nebulizer – cup attach all parts And other end to oxygen Grip with teeth and lips - Inhale slowly and deeply - 15 mins – gently flip side of cups - Water – rinse and wash as it minimizes risk of stuff - Document etc Intro to injectable meds Preparing Medication From an Ampule - Vitamin k - Sterile syringe Administering Intramuscular Injections Deltoid site – skin - 1-1.5 inches - 20-25 gauge needle - 90 degress injection - Volume – 1-4 ml , no more than 1-2 ml at deltoid site - 1-2 ml max for children HH check name and band Allergies Check med two times beforehand with MAR Than once at bedside Clean gloves Three fingers below the acromion process z-track – shift skin to the left or back and form triangle with point at mid axillary line – injection site thickest part of muscle -Clean area with antimicrobial swab with firm circular motion moving out from site and let dry - remove needle cap – hold syringe in dominant hand with thumb and forfinger - inject at 90 degree angel -carefully move fingers to end of plunger without removing syringe -slowly inject at 10 sec per ml Than wait 10 sec - Remove slowly and steadily at the same angle and avoid massaging - Dispose needle in sharps - Document with the site of administration – and response to medication Proper Insulin Pen Technique: Prepare pen for use - pull the safety seal cap off o Double check the expiry date & Correct insulin type o Correct pt identity on pen. 1 pen = 1 pt o If pen is cloudy, roll with the palm of hands 10 times and invert the pen 10 times until it becomes clear. o Wipe alcohol rub on rubber seal Attach the BD autosheild Safety Pen needle o Peel the tab, hold the outer cover, push and twist the Needle into the pen and turn it clockwise until tight, Pull off the outer cover Prime Pen o Injection flow must be verified in the pen needle o Dial to 2 units, and facing up, push the plunger o Should see liquid come out = primed pen Select insulin Dose o Dial the amount of dose indicated to pt Perform Injection o Choose site: Free of Lumps, bumps, and scars. o Hold the needle in a palm grip with thumb on plunger. o At a 90º into flat skin until the clear sheild retracts, and the white part flushes into skin Ensures needle has penetrated the tissue o Hold for a count of 10 seconds. (And the dose dial should go down to 0) Dispose pen o Remove needle from pen by twisting it CCW. And put it in sharps container. FAQ: o If pt in pain after injection: Do not press too hard while injecting the pen o Insulin is observed on the skin: Shake off any excess insulin on needle. Make sure to inject the needle into the tissue. Hold for 10 sec. o Could not prime - dial up 2 more unitsl o Safety locked before injecting: Do not lift the injection before it it is injected. Preparing Med from Ampule: Supplies: o Sterile syringe, filter needle, Administration needle, Ampule Medication, MAR, small gauze pad Compare the Med order to the original order by prescriber. o Look for Expiry, Allergies, Name, DOB Read the MAR and Take out med (1st check) Compare Med to the MAR (2nd check) Take the ampule and flick it on the top to put the med on the bottom. Break off the stem with a dry a gauze pad (so the broken glass does not poke you) & set it down on surface o Away from your body Attach the syringe with the filter needle (open cap) Insert the needle in the ampule and withdraw the medication in the injection o Be careful not to contaminate the needle tip by touching the rim of the ampule. o Could also invert ampule, make sure not bubbles Turn the needle up, tap the syringe and push the plunger to remove any air bubbles. Recap the needle Compare the amount of med in the syringe with the amount on MAR (3rd check) Remove filter needle, attach the Administration needle o Lock cart, dispose the ampule and needle in the sharps container Go to pt and check again (3rd check) and administer Preparing Med from Vial: Supplies: o Sterile (insulin) syringe, Vial medication, MAR, alcohol wipes Compare original order with MAR Read the MAR and Take out med (1st check) Compare Med to the MAR (2nd check) Agitate the content in the Vial (roll the vial in the palms) Clean the rubber thingy with alcohol swab for 15 sec Take syringe, uncap needle, Draw air equal to the medication dose o Do not inject air into the solution, want to inject the air into the airspace in the vial Invert the vial, and withdraw the amount of prescribe medication. Cap the needle Compare the vial label and the insulin needle to the order/ MAR (3rd check) o Store the vial when finished. Go to pt and check again (3rd check) and administer Mixing 2 Insulins in one syringe: Check if 2 of the drugs are compatible on the compatibility table or drug administration book Review MAR and order. o (eg. Humulin N (15 units) & Humulin R (5 units) - SQ injection - 30 min before breakfast) Supplies o Insulin Syringe, Insulin Vials, MAR, alcohol swab. Compare the Med order to the original order by prescriber. o Look for Expiry, Allergies, Name, DOB o Do drug calculations Take out the vials and check it against MAR (1st check) Agitate or Roll the Humulin vials to mix the contents Swab the rubber stoppers with alcohol pad Remove cap from needle Inject air into the vials o Start with the vial with a suspension (Humulin N) o Draw in air equal to the dose of N (15units), then Inject into the air layer and take it out. o Take the R vial and inject air as per it's dose This time do not remove the needle o Invert vial and draw (make sure no air bubbles) remove needle from vial, and put cap back on of needle (sterile) Clean the N vial again with swab & Insert needle into vial and draw up medication of amount required o Do not push in medication into vial Compare the vial label and the insulin needle to the order/ MAR (3rd check) o Label the vials and return them to storage. Administering Intradermal Injection: o Avoid sites with: Scars, Tattoos, Hair, Redness, Rashes, bruises, wounds o Avoid Massaging or putting pressure on the injection site after administration Introduce pt, HH, comfort pt of needle fear, Identity check Look and assess the forearm for injection site Clean the inner aspect of forearm with alcohol using circular motion, moving outwards from the injection site. Allow to dry Glove Take the syringe in dominant hand and remove the cap. Do not touch needle With non-dominant hand, spread the injection site. ( do not touch the cleansed area) Hold the needle 15º to skin, bevel side up " you are to feel a prick now" Insert needle about 1/8th of inch, (can see needle through the skin)(and dermis barely covers the bevel of the needle) Slowly inject the med, and watch for the small wheel or bump to form Quickly Withdraw the needle as the same angle it was inserted Apply the needle cap, and discard in the sharps container Educate pt: to not put pressure or rub the skin surface Document: time, date, Medication, site Administering Subcutaneous Injection: Administered into the adipose tissue, below the dermis, there are only few blood vessels there so the drugs will have slow sustained absorption. Need 25- 30 G and 3/8 in - 1 in needle can be used (usually up to 5/8 in) o Want to make sure that the prefilled needle is usually that size. IF not, then needs to be transferred into allowable needle size. Site of administratoin: Back of the upper arm, below the Costal margin in the Abdomen to the iliac crest (heparin site), Anterior aspect of Thigh, Upper back, Upper Ventrogluteal area. 45º - 90º of injection. o Decide based on the amount of subcutaneous tissue present and length of needle. Needle length - Depends on the subcutaneous tissue present and the pt's build and body wieght o Usually = 3/8 inch at 90º = 5/8 inch at 45º Amount of solution given = 1ml o Adding more may lead to pt discomfort and poor absorption Consider the appropriateness of medication, route, purpose of action, special nursing consideration, safe dosing, adverse affects Go to pt room Check on pt, identify identity, explain procedure and purpose. Raise bed o Check pt for allergies Prepare med, and check the label with MAR (check 1 and 2) Check 3 - pt bedside. Gloves Assess for site of administration (Abdomen) o No bruising or lumps Clean with alcohol swab in circular motion and allow to dry Remove the needle cap with non-dominant hand. Pinch the Skin/ site with non-dominant hand and injection with the other Insert at a 90º o "May feel a little pinch" Slowly inject the medication (at a rate of 10 sec/ ml) o Ask pt during procedure "how are they doing" Withdraw the needle quickly with the angle that it was inserted at while supporting the surrounding tissue Apply gauze and gentle pressure. (Do not massage, may cause damage underlying tissue) Cover the needle and throw it in the sharps o Glove off and HH Documentation - Include Site of administration. Date, time, medication, Locating Intramuscular sites: Injected Directly into the muscle layer Site: Ventral gluteal, Vastus laterlalis, Deltoid. 90º VentroGluteal Pt laying on side, hip and knee flexed. Place the palms of hand on the Greater Trochanter with fingers pointed towards his head. o Use your right hand on pt left hip. (opposite hands) Form a triangle with index and middle finger, by o putting the index finger on the Anterior Superior iliac spine. o Middle finger - dorsally, and palpate the crest of the ilium o Injection site - Center of the triangle Vastus Lateralis Pt on side or sitting position- Divide the anterior thigh into 1/3 horizontally and vertically. o Site is on the Outer middle third of the thigh Deltoid o Roll onto the side, Define the site Draw an Imaginary line with 1-3 fingers below the acromion process of scapula. o Base of a trangle. The pointy port of triangle is in the mid point of the axila The Site is at the thickest part of the muscle over mid-axillary line