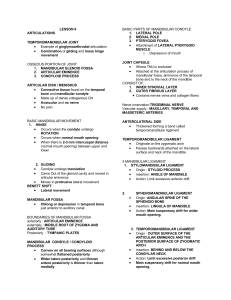
CLASSIFICATION OF • Myofascial pain and Dysfunction (MPD) • most common cause of masticatory pain and limited function • source is muscular with masticatory muscles developing tenderness and pain as a result of abnormal muscular function or hyperactivity • Pain is frequently, but not always, associated with daytime clenching or nocturnal bruxism • multifactorial, but bruxism resulting from stress and anxiety with occlusion being a modifying or aggravating factor is the most commonly accepted cause. • MPD may also occur because of internal joint problems such as disk displacement disorders or degenerative joint disease (DJD) USUAL COMPLAINTS: • Diffuse, poorly localized, preauricular pain (which may also involve temporalis and medial pterygoid muscles) • Decreased jaw opening with pain during functions such as chewing • Bi-temporal headaches • Pain is more severe during periods of tension and anxiety (role of stress) UPON EXAMINATION: • Diffuse tenderness of the masticatory muscles • TMJ is non-tender to palpation • No joint sounds present (isolated MPD) • Decreased mandibular movements associated with deviation of mandible toward the affected side. • Teeth frequently have wear facets RADIOGRAPHIC FINDINGS: • Usually normal (with some evidence of degenerative changes such as altered surface contours, erosion, or osteophytes, in selected cases) TMJ • The condyle articulates with the articular/mandibular/glenoid fossa and functions in a hinge and sliding/gliding fashion (ginglymoarthrodial joint) • It is considered as a compound joint* • Synovial joint* • Boundary lubrication* • Weeping lubrication* • Ligaments • Functional Ligaments • Collateral/ Discal Ligaments* • Capsular Ligament* • Temporomandibular Ligament* • Accessory Ligaments • Sphenomandibular Ligament* • discomalleolar ligaments • Stylomandibular Ligament* FULL OPENING Condyle rotates on a hinge axis and also translates forward to a position near the most inferior portion of the articular eminence. FUNCTION The biconcave disk remains interpositioned between the condyle and fossa, with the condyle remaining against the thin intermediate zone during all phases of opening and closing. • Anterior Disc Displacement with Reduction • Anterior Disc Displacement without Reduction Internal Derangements • Wilkes Staging Classification for Internal Derangement of the TMJ Anterior Disk Displacement with Reduction • Disk is positioned anterior and medial to the condyle in the closed position OPENING • Condyle moves over the posterior band of the disk and eventually returns to the normal condyle-disk relationship, resting on the intermediate zone CLOSING • Condyle slips posteriorly and rests on the retrodiscal tissue, with the disk returning to the anterior, medially displaced position • Patients with Stage I ID generally have no symptoms except minor joint noise (clicking) commonly when opening, but some cases it can be heard or palpated during closing • The opening click corresponds to the disk reducing to more normal position • The reciprocal/closing click corresponds to the disk failing to maintain its normal position between the condylar head and the articular eminence and slipping forward to the anteriorly displaced position. • Crepitus may be present as a result of articular movement across irregular surfaces • The clinical hallmark of disc displacement with reduction is limited mouth opening, usually accompanied by deviation of the mandible to the involved side, until a pop or click (reduction) occurs. After the pop, the patient is able to open the mouth fully with a midline position of the mandible. Arthrograms show anterior disc displacement in centric occlusion, but the disc is normally located in the open-mouth position. • Similar joint noises but will reveal joint tenderness. • Other symptoms may include muscle tenderness, temporal headaches, or transient joint locking • With additional episodes of limited mouth opening which can last for various lengths of time • Patients may describe it as “hitting an obstruction” when opening is attempted. The “obstruction” may disappear spontaneously or the patient may be able to manipulate the mandible beyond the interference. Arthrographically, stage two is similar to stage one. Anterior Disk Displacement without Reduction • Stage III/ Closed lock. The disk displacement cannot be reduced and thus the condyle is unable to translate to its full extent, w/c prevents maximal opening and causes deviation of the mandible to the affected side • No clicking occurs because patients are unable to translate the condyle over the posterior aspect of the disk. • The patient complains of TMJ pain and chronic limited opening, with the opening usually less than 30 mm. • Examination will reveal preauricular tenderness and deviation of the mandible to the affected side with mouth opening and protrusive movements. • In chronic closed lock episodes, if the condition progresses, the condyle may steadily push the disc forward to achieve almost normal ranges of mouth opening, in spite of the presence of a nonreducing disc. Degenerative Joint Diseases (DJD) Degenerative Joint Disease • Includes anatomic findings such as irregular, perforated, or severely damaged disks in association with articular surface abnormalities such as articular surface flattening, erosions, or osteophyte formation •Mechanisms of injury • Direct Mechanical Trauma- result from significant and obvious trauma to the joint or much less obvious microtrauma such as excessive mechanical loading. • Hypoxia reperfusion injury- excessive intracapsular hydrostatic pressure within the TMJ may exceed the blood vessel perfusion pressure resulting in hypoxia • Neurogenic inflammation- result from a variety of substance released from the periapical neurons. 1. Direct Mechanical Trauma • The excessive stress produced in the joint can lead to molecular disruption and the generation of free radicals, with resulting oxidative stress and intracellular damage. • Excess loading can also affect local cell populations and reduce the reparative capacity of the joint. 2. Hypoxia-Reperfusion Theory • Suggests that excessive intracapsular hydrostatic pressure within the TMJ may exceed the blood vessel perfusion pressure resulting in hypoxia. • This type of increased intracapsular pressure has been clearly demonstrated in patients during clenching and bruxing. • When pressure in the joint is decreased and perfusion is re-established, freeradicals are formed. • These free-radicals may interact with other substances in the joint (e.g. hemoglobin) to produce even more damage 3. Neurogenic Inflammation • Results when a variety of substance are released from peripheral neurons. • It is hypothesized that in cases of disk displacement, the compression or stretching of the nerve-rich retrodiscal tissue may result in release of proinflammatory neuropeptides. • The compounds released can serve as biologic markers that may help to diagnose and eventually treat pathologic conditions of the joint. • The dx of DJD or osteoarthritis is a broad term that encompasses both Wilkes Stage IV and V internal derangements • Pts with DJD frequently experience pain associated with clicking or crepitus located directly over the TMJ with obvious limitation of opening, and symptoms increase with function Radiographic findings are variable but generally exhibit decreased joint space, surface erosions, osteophytes, and flattening of the condylar head. (seen on panoramic radiographs and ct scans) Irregularities in the fossa and articular eminence may be present Perforation of the disc or its posterior attachments delineates the difference between stage IV and V derangement • Rheumatoid arthritis Systemic Arthritic Conditions Rheumatoid Arthritis • Pannus formation- result of an inflammation in rheumatoid arthritis. It is the abnormal proliferation of synovial tissue. • Symptoms may occur at an earlier stage than those associated with DJD • Usually affects TMJ bilaterally • Radiographic findings show erosive changes in the anterior and posterior aspects of the condylar heads • Changes may progress to large eroded areas that leave the appearance of a small, pointed condyle in a large fossa. • Eventually, the entire condyle and the condylar neck may be destroyed • Destruction of condyles bilaterally may result in loss of condylar-ramus height, resulting in premature contact of posterior teeth and an anterior open-bite malocclusion • Lab tests such as rheumatoid factor and erythrocyte sedimentation rate may be helpful in confirming the diagnosis of rheumatoid arthritis. Chronic Recurrent Dislocation Chronic Recurrent Dislocation • Caused by mandibular hypermobility • Subluxation is a displacement of the condyle, which is self-reducing and generally requires no medical management. • Dislocation can be unilateral or bilateral and may occur spontaneously after opening the mouth widely (yawning, eating, or during a dental procedure) • A more serious condition occurs when mandibular condyle translates anteriorly in front of the articular eminence and becomes lock in that position (open lock) • Dislocations should be reduced as soon as possible. • Apply downward pressure on the posterior teeth and upward pressure to the chin, accompanied by posterior displacement of the mandible • If muscular spasms prevent a simple reduction, anesthesia of the auricular temporal nerve and the muscles of mastication may be necessary. Sedation to reduce anxiety and provide muscular relaxation may also be required • Instruction to resist mandibular opening for 2-4 weeks and moist heat and NSAIDs are needed Ankylosis • Intracapsular Ankylosis • Extracapsular Ankylosis Intracapsular Ankylosis • Fusion of joints (disk + fossa complex + condyle) • A result of fibrous tissue formation, bone fusion or both • Leads to reduced mandibular opening that ranges from partial reduction in function to complete immobility of the jaw. • Most common cause: Microtrauma associated with condylar fractures • Other cause: previous surgical treatment that resulted in scaring and, in rare cases, infections • Clinical Evaluation: severe restriction of maximal opening, deviation to the affected side, and decreased lateral excursions to the contralateral side • Radiographic findings: Irregular articular surfaces of the condyle and the fossa with varying degrees of calcified connection between these articulating surfaces Extracapsular Ankylosis • Involves the coronoid process and the temporalis muscle • Causes: coronoid process enlargement, or hyperplasia, trauma to the zygomatic arch area, and infection around the temporalis muscle • Clinical Evaluation: limitation of opening and deviation to the affected side Radiographic Findings: • elongation of the coronoid process • CBCT and submental vertex radiograph may be useful in demonstrating impingement caused by a fractured zygomatic arch or zygomaticomaxillary complex Neoplasia • Rare cases • clinical manifestations are usually related to the temporomandibular dysfunction (TMD) and include preauricular swelling, pain, trismus, deviation of mandibular movement and malocclusion Osteochondroma Osteochondroma is a common slow-growing tumor that cartilage-capped bony projection arising from the outside surface of bone containing a marrow cavity that is continuous with that of the underlying bone Osteochondroma is usually located at the medial surface of mandibular condyle. The average age of occurrence is 16.5 and males are affected 3 times as often as females • The most common clinical symptoms are malocclusion, with unilateral posterior open bite on the affected side and a crossbite on the contralateral side, and progressive facial asymmetry, limited and often painful mandibular movements and clicking • Osteochondromas can be treated by total condylectomy or local resection of the lesion and condylar replacement if the tumor involves the mandibular condyle. On the other hand, if the tumor affects limited part of the condylar surface, preservation of the remaining part of the condyle and reshaping can be done Chondroblastoma Chondroblastoma is a rare benign, cartilaginous, destructive tumor derived from immature cartilage cells Chondroblastoma shows similar clinical symptoms associated with temporomandibular disorders such as sound in the joint, decreased range of motion, swelling, pain, trismus and changing occlusion. If chondroblastoma occurs at the temporal bone, additional symptoms such as otalgia, paresthesia, hearing loss, ear noise and facial nerve weakness may be seen Computerized imaging (CT) and magnetic resonance imaging (MRI) are the most common diagnostic imaging techniques to identify chondroblastoma. On imaging, round radiolucent lesions with sharp bony edges are found in bone Treatment alternatives are curettage, resection and excision. Chondroblastoma can be treated by conservative curettage when infiltration of bone has not occurred or is limited. Complete excision of the tumor reduces recurrence Synovial Chondromatosis Synovial chondromatosis (SC) is a rare benign nodular cartilaginous proliferative non-neoplastic lesion arising from the synovial membrane or the fibrocartilaginous disc of the joints becoming loose bodies within the joint space Synovectomy with removal of loose body from the joint space is the most preferred procedure. It can be applied in combination with discectomy or condylectomy. No recurrence when loose bodies are removed Clinical signs and symptoms of SC is local diffuse pain, pre-auricular swelling, limitation of mandibular movement, joint sounds, tenderness, deviation of mouth opening Computerized imaging (CT), magnetic resonance imaging (MRI) and orthopantomography are the most common diagnostic imaging techniques. The main findings are widening of the joint space, changes in bone surface of joint and calcified loose bodies Osteoma Osteomas are benign osteogenic tumors involving compact or cancellous bone proliferation and arising from periosteum (peripheral osteoma), endosteum (central osteoma) and even extra-skeletal soft tissue, but they are actually hamartomas that can be seen in membranous bone The growth of osteomas occurring in TMJ may result in morphologic and functional disturbances, including facial asymmetry, malocclusion and limited mouth opening Osteomas of the condyle are lobulated Histologically, compact type osteomas (ivory) consist primarily of dense lamellar bone, and cancellous type osteomas have an abundance of bone marrow Large osteomas at TMJ can be treated by condylectomy and tumor resection. No recurrence is reported after surgery Infections Infections involving TMJ • Rare cases • Extension of infectious process from middle ear infection may occasionally involve the TMJ (in countries where antibiotic therapy is unavailable) • Results in intracapsular ankylosis