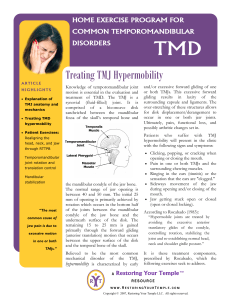
Summary Notes Kinesiology of the TMJ CPP- Tight Clench CP- limited opening Dislocation- fracture of the mandible body is most common though mediolateral dislocation most likely dislocation Reminder: joint type- synovial joints with fibrocartilage Two separate joint spaces Superior joint space: Plane synovial joint between intra-articular disc and condylar fossa Inferior joint space: Hinge synovial joint between intra-articular disc and mandibular condyle Ligamentous support Temporomandibular lig- Limits opening, retrusion and lateral deviation Stylomandibular and sphenomandibular lig- suspends the mandible Intra-articular disc- firmly attached medial lateral, loosely attached anterior posterior. Painful clench without tongue depressor suggests discal or tissue involvement Painful clench without tongue depressor suggests muscular involvement Movements Mandibular depression and elevation Rotation at the inferior joint (anterior rotation of condyle on the disc aka roll and glide in the opposite direction) Gliding in the superior joint (disc and condyle move together anteriorly) Mandibular Protrusion and retrusion Translatory movement that only occurs in the superior joint (no rotation) Limited retrusion Lateral deviation Observe condylar spinning ipsilaterally Observe condylar translation contralaterally Relationship with the cervical spine Head carriage often affects position of the TMJ Anterior head- TMJ protrusion (TMJ laxity and increased freeway space) Military head/Retrusion- TMJ retrusion (Retrodiscal tissue damage and decreased freeway space) TMJ function can also be influenced by: Bruxism Hard objects cracking Thumb sucking or mouth breathing Lengthy dental procedures Relevant muscles of the TMJ Digastric (anterior belly mylohyoid, posterior belly facial nerve) Medial and lateral Pterygoids (trigeminal n) Lateral contracts concentrically during mandibular depression Medial contracts concentrically in mouth closing Temporalis and masseter (trigeminal n) Assists in protrusion and elevation of mandible