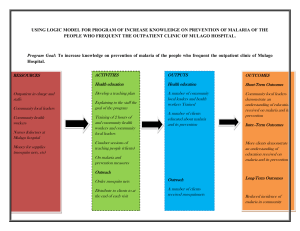
Option F: Food and health 2. Food systems and spread of diseases ● One detailed example of a vector-borne disease and one detailed example of a water-borne disease Vector-Borne Disease - Malaria: What is malaria and how does it spread? ● Malaria is an infectious disease spread by the mosquito, the vector for the malaria parasite, which thrives in tropical areas (~32°C) in stagnant water, estuaries or densely populated agricultural regions ● Symptoms of malaria appear 10-15 days after bite (including fever, tiredness, vomiting, and headaches, death in severe cases) ● Africa is home to 93% of malaria deaths, and malaria is considered a disease of poverty Malaria is a life-threatening disease for humans caused by the plasmodium parasite and transmitted to people via the bite of the female Anopheles mosquito. Here are some key facts about malaria: ● In 2015, 95 countries and territories had ongoing malaria transmission. ● About 3.2 billion people – almost half the world’s population – are at risk of malaria. ● Malaria is preventable and curable and increased efforts are dramatically reducing the malaria burden in many places. ● Between 2000 and 2015, malaria incidence among populations at risk (the rate of new cases) fell by 37 per cent globally. At the same time, malaria death rates in populations at risk fell by 60 per cent globally among all age groups and by 65 per cent among children under ve. ● Sub-Saharan Africa carries a disproportionately high share of the global malaria burden. In 2015 the region suffered 88 per cent of malaria cases and 90 per cent of malaria deaths What factors enable the spread (diffusion) of malaria? ● Human factors ○ Urbanisation/population growth ■ Creation of mosquito breeding sites (garbage dumps, tires, discarded containers) ■ High population density, allows for rapid spread of disease ○ Low educational levels ■ Failure to receive adequate guidance regarding prevention and dosage and as such, fail to adhere to prescription ■ Improper use of drugs results in adaptation of resistance in mosquitoes ○ Economic status ■ Malaria is easily treatable and preventable if funds are present, so disease is concentrated on the poor ● Geographical factors ○ Climate ■ Concentrated on tropical areas as mosquitos can only survive in said areas Landforms ■ Malaria is found only around rivers or other bodies of water as other parts of the country can be quite dry ■ Transmission is reduced due to lack of proper breeding sites for mosquitos Environmental preferences The malarial parasite (plasmodium) thrives in the humid tropics where a minimum temperature of 20°C allows it complete its life cycle. The mosquito is a primary host and the human is secondary. The mosquito’s ideal environment is stagnant water, estuaries, deltas and irrigation channels. These are usually found in densely populated agricultural regions. The disease is often triggered by natural events such as cyclones and ooding or by human conicts such as war, which often results in refugees. They are likely to live in temporary camps with inadequate drainage (open sewers), which are ideal breeding grounds for the mosquito. ○ The cost of treating malaria Global nancing for malaria control increased from an estimated $960 million in 2005 to $2.5 billion in 2014. Malaria interventions led to health service savings of $900 million in sub-Saharan Africa between 2001 and 2014, owing to the reduced number of cases. The direct cost of malaria to individual households includes medication, doctors’ fees and preventative measures such as bed nets, which help to reduce transmission. Infected individuals are unable to work, which can reduce family incomes during the attacks. The symptoms of malaria The rst symptoms – fever, headache, chills and vomiting – appear seven days after the mosquito bite, and they may be mild at rst and difcult to recognize as malaria. If not treated within 24 hours, malaria can progress to severe illness, often leading to death. Children with severe malaria frequently develop one or more of the following symptoms: severe anaemia, respiratory distress in relation to metabolic acidosis, or cerebral malaria. In adults, multi-organ involvement is also frequent. In malaria-endemic areas, people may develop partial immunity, allowing asymptomatic infections to occur. Who is at risk? Some population groups are at considerably higher risk of contracting malaria and developing severe disease than others. These include infants, children under ve years of age, pregnant women and patients with HIV/AIDS, as well as non-immune migrants, mobile populations and travellers. National malaria control programmes need to take special measures to protect these population groups from malaria infection, taking into consideration their specic circumstances. Transmission In most cases, malaria is transmitted through the bites of female Anopheles mosquitoes. There are more than 400 different species of Anopheles mosquito; around 30 are malaria vectors of major importance. All the important vector species bite between dusk and dawn. The intensity of transmission depends on factors related to the parasite, the vector, the human host and the environment. Country Example: Ethiopia ● ● ● ● ● 5 mil cases a year, 70k deaths a year Transmission peaks bi-annually during harvesting seasons (large migrations from highlands to lowlands for agricultural work) Lack of communications technology to communicate information on the epidemic Changes from rain-fed agriculture to large scale irrigation agriculture increases river damming for hydroelectricity and increases stagnant water ○ Irrigated crops eg. cotton and sugarcane require lots of water and warm tropical temperatures increases breeding of malaria vectors Impacts: ○ reduction in productivity of adult workforce and ability of children to attend school (Ethiopia highly dependent on labour-intensive agricultural sector) ○ An overwhelmed healthcare sector lacking in skills, resources and staff training ○ Loss of investment & tourism (tourists reluctant to visit) What barriers, treatment & prevention strategies exist? ● Prevention ○ Vector control by long-lasting insecticide-treated mosquito nets and indoor residual spraying ■ sleeping under a bed net reduces child mortality by as much as 20% ■ Nets reduce the overall lifespan of mosquitoes, limiting further transmission ○ Spraying with insecticides (DDT), fully effective when >80% of houses in targeted areas are sprayed ○ Environmental management, favoured in Ethiopia (destroying breeding sites, digging proper toilets to prevent water accumulation) ○ Increased govt primary health care initiatives, introducing up to 30,000 HCW by 2009 ○ Rapid diagnostic tests to distinguish between non-malarial fevers ○ Drug treatment (quinine and recently chloroquine) Prevention Vector control is the main way to prevent and reduce malaria transmission, as recommended by the WHO. Two forms of vector control – insecticide-treated mosquito nets and indoor residual spraying – are effective in a wide range of circumstances. If coverage of vector control interventions within a specic area is high enough, then a measure of protection will be conferred across the community. Long-lasting insecticidal nets (LLINs) are the preferred form of insecticide-treated mosquito nets (ITNs) for public health programmes. In most settings, WHO recommends LLIN coverage for all people at risk of malaria. The most cost-effective way to achieve this is by providing LLINs free of charge, to ensure equal access for all. In parallel, effective behaviour change communication strategies are required to ensure that all people at risk of malaria sleep under an LLIN every night, and that the net is properly maintained. Indoor residual spraying (IRS) with insecticides, including DDT, is a powerful way to rapidly reduce malaria transmission. Its full potential is realized when at least 80 per cent of houses in targeted areas are sprayed. In some settings, multiple spray rounds are needed to protect the population for the entire malaria season. Antimalarial medicines can also be used to prevent malaria. For travellers, malaria can be prevented through chemoprophylaxis, which suppresses the blood stage of malaria infections, thereby preventing malarial disease. ● Barriers ○ Antimalarial drug and insecticide resistance mean more combinations of drugs need to be developed ○ Insecticide nets and cheap drugs require routine monitoring Insecticide resistance Vector control is highly dependent on the use of pyrethroids, the only class of insecticides currently recommended for ITNs or LLINs. In recent years, mosquito resistance to pyrethroids has emerged in many countries. In some areas, resistance to all four classes of insecticides used for public health has been detected. Fortunately, this resistance has only rarely been associated with decreased efcacy of LLINs, which continue to provide a substantial level of protection in most settings. Rotational use of different classes of insecticides for IRS is recommended as one approach to manage insecticide resistance. To ensure a timely and coordinated global response to the threat of insecticide resistance, the WHO worked with a wide range of stakeholders to develop the “Global Plan for Insecticide Resistance Management in Malaria Vectors (GPIRM)”, which was released in May 2012. Diagnosis and treatment Early diagnosis and treatment of malaria reduces disease and prevents deaths. It also contributes to reducing malaria transmission. The best available treatment, particularly for P. falciparum malaria, is artemisininbased combination therapy (ACT). Antimalarial drug resistance Resistance to antimalarial medicines is a recurring problem. Resistance of P. falciparum to previous generations of medicines, such as chloroquine and sulfadoxine-pyrimethamine (SP), became widespread in the 1970s and 1980s, undermining malaria control efforts and reversing gains in child survival. The WHO recommends the routine monitoring of antimalarial drug resistance, and supports countries to strengthen their efforts in this important area of work. Surveillance Surveillance entails tracking the disease and taking action based on the data received. Malaria eradication is dened as the permanent reduction to zero of the worldwide incidence of malaria infection as a result of deliberate efforts. Once eradication has been achieved, intervention measures are no longer needed. In countries with high or moderate rates of malaria transmission, national malaria control programmes aim to maximize the reduction of malaria cases and deaths. Vaccines against malaria There are currently no licensed vaccines against malaria or any other human parasite. Clinical trials are currently being held, and it is expected that there will be a vaccine by 2020. In October 2015, two WHO advisory groups recommended pilot implementations of RTS, S/AS01 (a malaria vaccine) in a limited number of African countries. The WHO strategy The WHO Global Technical Strategy for Malaria 2016–30 – adopted by the World Health Assembly in May 2015 – provides a technical framework for all malaria-endemic countries. It is intended to guide and support regional and country programmes as they work towards malaria control and elimination. The strategy sets ambitious but achievable global targets, including: ● reducing malaria incidence by at least 90 per cent by 2030 ● reducing malaria mortality rates by at least 90 per cent by 2030 ● eliminating malaria in at least 35 countries by 2030 ● preventing a resurgence of malaria in all countries that are malaria-free Water-Borne Disease - Cholera: What is cholera and how does it spread? ● Acute diarrheal disease (vibrio cholerae) transmitted through oral routes (water, food); often found in estuary ecology ● It strikes in pandemics in LICs and NICs (newly industrialised countries), and can easily be brought to other countries through network/relocation diffusion. ● There are 3-5 mil cases annually, killing 100,000, but reported cases only represent 5-10% of actual cases ● Symptoms include large amounts of watery diarrhea, vomiting and muscle cramps, dehydration and death if left untreated Cholera is an infection of the small intestine caused by the bacterium Vibrio cholerae. There are several strains of the bacterium, some causing worse symptoms than others. It is a waterborne disease, although it can also be transmitted by contaminated food. For cholera outbreaks to occur, there must be two conditions: 1. There must be signicant breaches of water sanitation leading to contamination by the bacterium Vibrio cholerae 2. Cholera must be present in the population. This infection is mostly asymptomatic or causes mild gastroenteritis. However, about 5 per cent of infected persons develop severe dehydration and acute diarrhoea, which can kill within hours. There are 28,000–142,000 deaths from cholera every year. Even those who are symptom-free can carry the bacteria in their faeces and the disease is easily transmitted if sanitation arrangements are inadequate. What factors enable the spread (diffusion) of cholera? ● Social ○ Hunger present in a population leads to weakened immune systems, making it easier to be infected ○ A lack of sanitation and food safety practices increase the risk of transmission ○ High living density in urban areas & rapid urbanisation ○ Low diffusion of education (particularly regarding health & proper treatment of disease) ● Economic ○ ● ● Corruption prevents sanitation and medical supplies to reach those in need Environmental ○ Irrigation and water insecurity in the area (epidemics begin during the end of the dry season when people are forced to accumulate at fewer water resources) Political ○ Difficulty of access to rural areas to conduct government censuses Risk factors Transmission of Vibrio cholerae is relatively easy in areas of poor housing and inadequate sanitation. It is particularly the curse of displaced populations living in overcrowded camps. Children under ve are particularly vulnerable. The transmission of Vibrio cholerae Open-air defecation or leaking sewers Country Example: Ethiopia ● deaths of 684 people and infection of nearly 60,000 others in less than a year (2007) ● 33,000 cases of cholera and 776 deaths (2017) ● Forced migration due to drought and below average rains (as a result of the El Niño event) ● Most prevalent in refugee camps with poor infrastructure and crowded conditions ● The WFP (World Food Programme) needed $268 million to provide food assistance in Ethiopia from Jan 2017 until July What barriers, treatment & prevention strategies exist? ● Treatment: reducing deaths ○ Rehydrating patients and replacing electrolytes lost through vomiting and feces ○ Emphasising chlorinated, boiled water for use during oral rehydration, food preparation, hand washing, and cleaning ● Prevention: preventing new cases ○ Intensive public education, environmental sanitation campaigns (eg. education programmes about latrine safety) ○ Surveillance, allowing healthcare personnel to detect cases early and to assess size, density of outbreak to distribute resources ○ Assembling a response team to fully cover all aspects of disease identification, treatment & recovery - lab techs to identify symptoms, environmental health experts to identify causes, creating stockpiles of oral rehydration salts Cholera symptoms Infection of the small intestine Water abstracted for domestic use Contaminated water used for washing hands Vibrio cholerae in stream Vibrio cholerae in faeces Clinical treatment ● Prompt administration of oral rehydration therapy is sufcient to treat 80 per cent of patients. ● Very dehydrated cases need intravenous uids. ● Antibiotics are useful while V. cholerae is still being excreted, but prolonged treatment can lead to antibiotic resistance – a serious problem in treating all infectious illness. ● Oral cholera vaccine (OCV) can be effective, but it is important to adopt prevention and control measures as well. The role of the World Health Organization The WHO Global Task Force on cholera control works to: ● support and implement global strategies to prevent and control cholera ● provide a forum for cooperation and to strengthen a country’s capacity to prevent and control cholera ● support research ● increase the visibility of cholera as an important global health problem 3. Stakeholders in food and health ● One case study of the issues affecting a famine-stricken country or area Yemen & Famine What is famine? ● A legal condition required to declare a state of emergency in a country, where a) 20% of households in a given country face extreme food deficits b) 30% children are acutely malnourished c) mortality rates exceed 2 people per 10,000 population per day as a result of food deficit ● There are currently 4 countries worldwide on the brink of famine, and $4 billion is needed by UN to alleviate all of them, with only 14% of that amount available from aid and donations What is causing Yemen’s famine? ● Violent conflict ○ The Arab Spring in 2011 resulted in a power shift from an authoritarian president (part of the Hadis) ○ As a result, a rebel Houthi Muslim movement took control of the capital city, with Saudi Arabia and other states (backed by the US) bombing the Houthis to try and restore the Hadis ○ The proxy war in the region has killed nearly 10,000 people since 2015, with 2 million IDPs (internally displaced people) ○ The war escalated to an international proxy war when the US, UK & France stepped in to lend military assistance in the form of bombings and airstrikes to try and subdue the Houthis ○ The strategic location of Yemen neighbouring other Middle Eastern nations enables geopolitical conflict ● Climate change ○ Yemen is naturally dry and dusty, with less than 3% of its land supporting 28 million people ○ Less rainfall means less harvest and shorter growing seasons, so minimal (if any) food is stored for periods of crisis and people are less likely to survive during conflict ○ Water insecurity and unsustainable resource practices and use have lead to a depletion of Yemen’s groundwater/aquifers, further increasing the insecurity of their minimal food production What are the impacts of Yemen’s famine? ● Economic ○ The Yemeni economy will be unable to generate sufficient foreign exchange, depreciating the currency and continuing to increase food prices/inflation ○ 12,000 out of the 14,000 schools in Yemen have now shut down ● Social - a shortfall in food availability & health ○ Due to Saudi naval, land and air blockade on Yemen’s ports blocking Iranian and international food/humanitarian aid ○ 85% of food supplies prevented from entering ○ Resurgence of preventable diseases like malaria and cholera ■ 1.26 million suspected cholera cases in the country with 1.5 million malnourished children ○ Collapse of the health system & international aid ■ hospitals, schools, food-storage facilities targeted in bombings ■ NGO Medecins Sans Frontiers (Doctors Without Borders) had 19 personnel killed in a bombing, causing them to withdraw all international staff in the region ■ 600 health facilities out of action due to fighting ■ 50 kilo tonnes of wheat (enough for 3.7 million people for a month) from the World Food Programme prevented from reaching Yemeni borders ● Environmental Degradation ○ Saudi bombings target power generation sites, causing blackouts and impacting water supplies ○ direct & indirect pollution from destruction of infrastructure causing heavy metals and particulates to be released into surrounding atmosphere and water sources Famine in Ethiopia Social impacts: ● Ethiopia has been plagued by famines since the 16th century. In recent times, famine struck the country in 1973 (40,000 starved in the north-east and around 55,000 died in the Ogaden region) and between 1983 and 1985, when areas of northern Ethiopia and Eritrea were affected in what is regarded as the country’s worst famine in a century. Estimates of the number of deaths ranged from 400,000 to one million people. Millions of others were made destitute. The 1983–5 famine was widely reported in the media and received much publicity. It also led to the Band Aid and Live Aid concerts. Environmental impacts: ● In 2015, the seasonal rains that usually fall between June and September in north-eastern, central and southern Ethiopia did not arrive. According to the UN, this was Ethiopia’s worst drought in 30 years. Around 90 per cent of cereal production is harvested in autumn, after the summer long rainy season, and the rest at the end of spring after the end of the short rainy season. Political (role of government) ● These days, early-warning systems (Figure F.47) alert the government when famine threatens, and in 2015 the government was able to respond more quickly to the crisis than in 1983–5. There is evidence that in 2015–16 the Ethiopian government made provision to mitigate the impact of poor harvests, such as establishing a social security net so that poorer farmers can access funds for public works such as digging water holes. ● The Ethiopian government pledged $192 million for emergency food and other assistance, diverting money from projects such as road construction. The “international community” promised a further $163 million. Aid agencies suggested that $600 million was needed. The drought was caused by the El Niño weather system, and resulted in a 90 per cent reduction in crop yields. (economic, role of organiations) Political factors: poor governance and state neglect. The key factors driving the famine,then and now, include the selling off of land to international corporations for industrial farming – that is, “land grabs”. Another criticism was that in 1983–5 much food relief was channelled towards the military. Social factors: The large number of refugees in Ethiopia More than 650,000 refugees from Somalia, South Sudan, Sudan and Eritrea are in Ethiopia, and this places a large burden on water and land resources. Political (role of the government) At first, some in the Ethiopian government claimed the country could handle the drought itself. In December, they said about 10.2 million people were in need of $1.4 billion in aid, with 400,000 children severely malnourished. This is in addition to 8 million people supported by the government safety net even before the drought. Social impacts (role of the media): To date, less than 50 per cent of the appeal has been met, and the worst could be yet to come. In 2015–16 international donors were distracted by a string of humanitarian disasters around the world, such as in Syria and South Sudan. This meant that there was much less media coverage, and so less publicity compared with 1983–5. Events in Syria were more dramatic than the failure of the rains, although the failure of the rains probably caused more deaths. Role of organizations and aid Nevertheless, a number of organizations are working in Ethiopia, including the World Food Programme (WFP), Save the Children and the FAO. The WFP is helping to feed the refugees and also supporting the government’s second ve-year Growth and Transformation Plan (GTP), a school meals programme and a vulnerability and mapping unit (VAM). Save the Children Ethiopia reported substantial livestock losses in the Afar region. It had also mobilized $100 million, while the FAO announced a $50 million plan to assist agriculture- and livestock dependent households. 4. Future health and food security and sustainability ● One case study of attempts to tackle food insecurity Management of European Fish Stocks What is the issue? ● Nearly 70% of the world’s fish stocks are in need of management ○ Cod stocks in the North Sea are less than 10% of 1970 levels ● World wild food fish demand has increased from average of 9.9 kg per capita to 19 kg per capita, putting more strain on already taxed fisheries, particularly those being fished above Maximum Sustainable Yield (MSY) What is being done? ● Management of biotic resources of oceans in the EU under the Common Fisheries Policy (CFP) ● Management can be input control, output control or a combination ● input controls: ○ Limiting the number of vessels in certain waters: fishing permits ○ fishing effort controls limiting capacity of vessels ○ technical measures: Small meshed nets, minimum landing size → protect juveniles ● output controls: ○ limiting catches through total allowable catches and quotas, matching supply to demand ○ surveillance: check landings by EU → apply penalties to overfishing and illegal landings ○ Tariff policy: Minimum import prices → to ensure EU preference ● Development of aquaculture practices ○ Aquaculture now accounts for ~20% of fish production ○ Aims to double aquaculture in the EU by 2030 ● ● Conservation measures & environmental legislation (Marine Strategy Framework Directive) to safeguard biodiversity surrounding the fish stocks & address human activities (fisheries) affecting the oceans as a result, pressure on European stocks in 2013 declined by 50% ○ While EU legislation regarding management of insecure stocks was not enacted as quick as other countries, 74% of European fish stocks previously fished below Maximum Sustainable Yield are currently rebuilding successfully ● One case study of a contemporary pandemic and the lessons learned for pandemic management in the future Ebola & Pandemic Management ● A pandemic is an epidemic (a sudden increase in cases above the norm of disease outbreaks in an area) spread over countries/continents What is ebola? ● An often fatal illness contracted through infection with the Ebola virus, transmitted through human-to-human contact. ● Extremely prevalent 2014-2016 in Liberia, Sierra Leone, Guinea ● Epidemiology: transmitted through human-to-human contact & infected wild animals; through bodily fluids, organs etc of infected persons (blood, dead bodies, sweat etc) ● Symptoms: 8-10 days incubation highly flu-like (fever, fatigue, muscle pains), extreme escalation in the 2-3 days after (internal bleeding, vomiting, diarrhea) What was the temporal & spatial dispersal of ebola? ● began in Guinea 2013 after a boy died at a regional trading point from contracting the virus from a bat ● boy’s family became infected & died, disease spread to other villages when people travelled ● traditional burial practices in West African culture involves evacuating the body of bowels, food etc., making the spread of the disease extremely prevalent in this region ● Proper cases were not reported until March 2014 as it is tradition for sick relatives to be cared for at home in West Africa ● 28,657 total reports of infection, of which 11,325 died (a high mortality rate of 39.5%) ● The disease spread to the slums of capital cities, causing rapid spikes in number of cases per day What role did social marginalisation play in this pandemic? ● Social Marginalisation: an extreme tension between communities due to lack of awareness about how the disease spreads and infects others ● ● ● The borders & markets between Liberia and neighbouring countries have closed, even though cross-border trade and relationships are vital for border economies and building trust Survivors & their quarantined families completely shunned within communities due to fear of infection The role of local governments was key in minimising stigma - an organisation called District Platforms for Dialogue (DPD) educated villagers about ebola in the local dialect ○ forums and discussions were facilitated by DPD, with town chiefs, women leaders and healthcare workers in attendance to remind communities of life before ebola How can social media be used to manage pandemics? ● Organisation ‘Africa Stop Ebola’ used well-respected public figures with social weight & music to perform a song in French and other local languages ● Local media portrayal of the pandemic contrasts with Western media, who were very slow to report on initial outbreak ○ reporting in US only began after an American who travelled to Liberia returned home to the US and fell ill in 2014; widespread European reporting only after a volunteer Spanish nurse fell ill ● Note the social media penetration is 14% in Africa vs. 66% in NA and 54% in Europe, meaning the media isn’t always accessible to the majority of the population and thus its effectiveness in dealing with or reporting news about the ebola pandemic can be limited in certain areas ● Newspaper media coverage is crucial to frame pandemics in the right light ○ The ebola pandemic was initially framed as localised African crisis ○ Media coverage transitioned to focusing on danger to Western countries rather than humanitarian disaster in Africa ■ This limited donations for medical equipment & travel of volunteer health workers ● Human interest stories shown to be effective at humanising the crisis ● Amplified panic on social media micro-posts can be used to detect real time emergence of crises through the use of semantic data mining How can ebola be controlled and treated? ● By diagnosing, tracing and isolating contact of every single Ebola patient to prevent new chains of transmission was necessary to fully contain the disease ● The use of chlorine concentrate to treat food, water, clothes etc ● Biosecure Emergency Care Units for Outbreaks (cubes) cost $USD17,000 but allow workers to administer care externally, and for families to communicate with patients without risk of contamination How can ebola be prevented? ● Household prevention kits containing soap, chlorine, masks etc distributed by WHO, UNICEF ● educating public on transmission, using personal protection equipment effectively, ebola transmission campaigns aired on radio & television ● ensuring free treatment in isolated regions is essential for early detection & eradication What are the barriers to prevention? ● Fear amongst locals and communities ○ There was a great fear amongst locals who didn’t understand ebola and the treatment process of never seeing loved ones again - family members that were ill were taken away by healthcare workers in hazmat suits & masks; they often didn’t return alive due to the high prevalence of disease ○ Pervasive messaging spread among communities that ebola has no cure due to the high death toll, when in reality treatment and containment is possible given proper resources ● poor infrastructure & communication, cultural beliefs ● Ebola suspect’s dilemma ○ The early symptoms of ebola are extremely similar to malaria, a common and preventable disease also found on the African continent ○ A person suffering from these symptoms either has malaria & will likely survive if they get malaria medication, but if they have ebola and go without treatment, they will die and likely infect others ○ Patients have a choice whether to go to an ebola treatment centre or not the probability of dying can be seen in the following graphic: ○ ○ overall mortality risk for staying at home vs treatment is 35% to 40%. suspects can maximise chance of survival by staying at home, but risk becoming sub spreaders of the virus