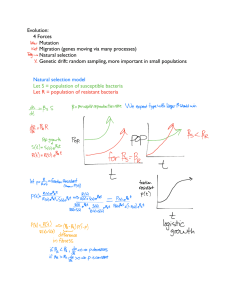
Antibiotic resistance and it’s impact on healthcare settings Antibiotics are the agents that either kill or inhibit the growth of bacteria and they are also called as anti-bacterial. Antibiotics can be administrated in the body by both means: orally or intravenously. Antibiotics work against infections caused by bacteria and certain parasites. They do not work against infections that are caused by viruses (for example, the common cold or flu), or fungi or fungal infections of the skin. In fact, they specifically target bacteria rather than human cells. A broad-spectrum antibiotic can be used to treat a wide range of infections where as a narrow-spectrum antibiotic is only effective against a few or specific types of bacteria. Antibiotic resistance occurs when a microorganism or bacteria is able to survive and grow in the presence of a concentration of antibiotics that usually inhibit or kill the organism of same species. Antibiotic resistance has become a global threat. Resistant bacteria can spread between individuals, animals, and the environment. The broad increase in antibiotic resistance in cattle, food, hospitals, and the general public is a result of our overuse and misuse of antibiotics in humans, animals, and agriculture. This has caused a threatening remark in the healthcare system as well. Over the past ten years, rates of antibiotic resistance among hospital and community infections have significantly grown. It is becoming more difficult to treat infections brought on by these resistant strains with the "standard" medications. When caused by bacteria resistant to antibiotics, common diseases (including pneumonia, as well as skin and urine infections) become more and more difficult to cure and endanger an increasing number of people worldwide. Different patient outcomes are impacted by bacteria that are resistant to antibiotics. The presence of resistance in a bacterial pathogen can cause a delay in the administration of the proper antimicrobial therapy, and the antimicrobial therapies needed to treat resistant pathogens may be toxic or insufficient. Resistance genes can change the fitness of a bacterial pathogen, making it more or less virulent. Antibiotic-resistant infections could necessitate more harsh treatment, which could have unfavorable effects. There is a significant risk of renal failure when colistin is used to treat infections caused by highly resistant Pseudomonas or Acinetobacter. Vancomycin, for example, is used to treat severe methicillin-resistant Staphylococcus aureus (MRSA) infections. Some medications used to treat the resistant strain of an organism are also less effective than medications used to treat the susceptible strain of the organism. Finally, patients with infections that are not susceptible to surgical debridement have significant death rates. Patients with infections that are not receptive to surgical debridement frequently require surgical treatments to remove the nidus of infection. Cancer treatment will be significantly hampered by antibiotic-resistant bacteria for decades, and the number of cancer patients will continue to climb. Higher mortality, more difficult and expensive treatment, as well as numerous side effects and long-term impacts, could all result for the patients. One of the most typical consequences for cancer patients is a bacterial infection. Infections and a compromised immune system can be fatal for people with life-threatening illnesses. Many individuals need antibiotics after surgery to manage infected wounds. Chemotherapy and radiation therapy kills cancer cells, but they also destroy immune system cells that help us fight off infections. This implies that infections frequently arise in radiation or chemotherapy patients that need to be treated with antibiotics. Without antibiotics, it is also impossible to perform immunotherapy and transplants. The price of therapies is significantly impacted by resistance. A resistant bacterial infection is thought to cost 700 US dollars or more to treat on average. This is equivalent to more than a year's earnings for a rural Indian worker. Many people are unable to afford the medications since novel treatments for multidrug-resistant infections can cost up to tens of thousands of US dollars. Treatment delivery becomes increasingly challenging, necessitating increased expertise among medical professionals as well as the usage of less vetted techniques and therapies. Without antibiotics, many medical procedures' infection problems would occur far too frequently, damage patients, and even be fatal causing a more difficult challenge to tackle for healthcare system. Therefore, antimicrobial stewardship and awareness on the deadly effect of antibiotic resistance should be carried out.