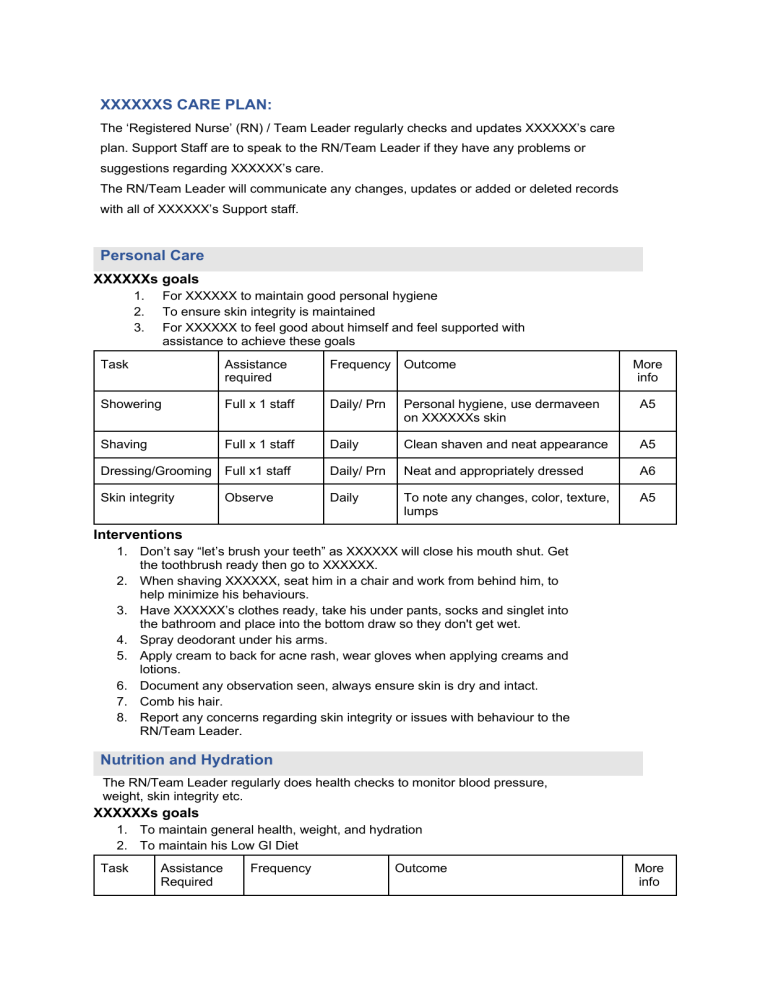
XXXXXXS CARE PLAN: The ‘Registered Nurse’ (RN) / Team Leader regularly checks and updates XXXXXX’s care plan. Support Staff are to speak to the RN/Team Leader if they have any problems or suggestions regarding XXXXXX’s care. The RN/Team Leader will communicate any changes, updates or added or deleted records with all of XXXXXX’s Support staff. Personal Care XXXXXXs goals 1. 2. 3. For XXXXXX to maintain good personal hygiene To ensure skin integrity is maintained For XXXXXX to feel good about himself and feel supported with assistance to achieve these goals Task Assistance required Frequency Outcome Showering Full x 1 staff Daily/ Prn Personal hygiene, use dermaveen on XXXXXXs skin A5 Shaving Full x 1 staff Daily Clean shaven and neat appearance A5 Dressing/Grooming Full x1 staff Daily/ Prn Neat and appropriately dressed A6 Skin integrity Daily To note any changes, color, texture, lumps A5 Observe More info Interventions 1. Don’t say “let’s brush your teeth” as XXXXXX will close his mouth shut. Get the toothbrush ready then go to XXXXXX. 2. When shaving XXXXXX, seat him in a chair and work from behind him, to help minimize his behaviours. 3. Have XXXXXX’s clothes ready, take his under pants, socks and singlet into the bathroom and place into the bottom draw so they don't get wet. 4. Spray deodorant under his arms. 5. Apply cream to back for acne rash, wear gloves when applying creams and lotions. 6. Document any observation seen, always ensure skin is dry and intact. 7. Comb his hair. 8. Report any concerns regarding skin integrity or issues with behaviour to the RN/Team Leader. Nutrition and Hydration The RN/Team Leader regularly does health checks to monitor blood pressure, weight, skin integrity etc. XXXXXXs goals 1. To maintain general health, weight, and hydration 2. To maintain his Low GI Diet Task Assistance Required Frequency Outcome More info Drinking Full x 1 staff Offer fluid every hour To maintain his hydration A2 L1 Food 3 meals and 3 snacks a day On low GI diet refer to L1 in care plan To maintain XXXXXX’s weight, have good general health and wellbeing A2 L1 Minimal x 1 staff Interventions 1. Offer XXXXXX fluid every hour, water, whey powder drink with Almond milk drink. 2. Fill glass and place it in his hand, if XXXXXX only has a few sips, repeat the process. Always leave the glass with water at the end of the kitchen bench. 3. Give support to his right arm, to reduce the risk of him dropping the glass. 4. Ketogenic Diet, make breakfast, lunch and dinner, refer to menu planning 5. Serve meals, cut up XXXXXX’s meals into bite size pieces, place food in front of him, provide XXXXXX with assistance using a fork and spoon. 6. Assist XXXXXX to sit at the table 7. XXXXXX requires full supervision at all times 8. Report to RN/Team leader if XXXXXX is not drinking enough or is not eating. Medication Administration XXXXXXs Goals 1. To ensure XXXXXX receives the correct medication as prescribed. 2. To ensure the PRN medication is given as per his Doctors orders, to reduce the risk of overdose. Tasks Assistance Frequency Outcome required Webster Pack Full x1 For regular medications PRN Medications / As required in webster pack Full x1 As Per webster pack As per drug chart / GP instructions More info For medication to be given correctly and for XXXXXX to be appropriately medicated G1 XXXXXX to remain pain free and comfortable. Avoid Status epilepticus and brain damage. K1 H4 K1 The RN/Team Leader will monitor the administration of all medication, Interventions 1. 2. 3. 4. 5. 6. 7. Make sure the tablets come from the correct time slot in the pack. Place tablets in XXXXXX's mouth, ensuring your hand is placed under his chin, hand XXXXXX a glass of water. If XXXXXX is resistive (spitting his tablets out) place him in front of the bench and replace the tablets back into his mouth and give the glass of water to him. Ensure he has swallowed the tablets. Sign the medication chart in the correct place. Record date, time, dose, sign example: (20/11/20, 1100 hrs, 2 tablets, Sign) If unsure about PRN or regular medications speak to the RN/Team Leader Communication XXXXXXS GOALS 1. To enable XXXXXX to express his thoughts, needs, desires, and choices. 2. To enable XXXXXX to interact with others in conversation. Communication aids Support/ assistance required. Frequency Outcome Lightwriter Physical support at hand, wrist, or forearm. When using communication Participation and increased self esteem. D, E I Pad Set up a device. Physical support at hand, wrist, or forearm. When using a device to communicate. Participation and promote creativity. D, E Alphabet Boards Physical support at hand, wrist, or forearm. For quick communication. For XXXXXX to communicate quicker . D, E Yes/ No responses Physical support to forearm or shoulder as needed. When a quick simple response is required. XXXXXX will be able to accept or reject quickly and with less support . D, E Choices Indicate 3 choices in front of XXXXXX for food, music, or television/ always have a choice of “something else” available to him. When XXXXXX needs to make a simple selection. XXXXXX will be able to make simple choices. Interventions 1. 2. 3. 4. 5. 6. 7. 8. 9. Physical support is required for all communication, by supporting XXXXXXs hand so he can point with his finger. Place XXXXXX in the wheelchair when communicating with his computer, I Pad, Lightwriter, as it supports his body and allows him to concentrate on his fingers. As communication requires XXXXXX to concentrate, he tires easily. If XXXXXX becomes tired, stop communicating and give him a break. Ask Yes/No questions for quick responses from XXXXXX example: (Would you like a smoothie for breakfast. He will respond yes or no on the alphabet board on the fridge, or the yes no signs on the bench) If XXXXXX indicates a no response offer another breakfast option. Give three choices then say something else if he is not happy with the three choices. Give XXXXXX time to respond if he feels pressured, he finds it harder to communicate. Ask one question at a time Report to RN/Team Leader if there are any issues with XXXXXX’s communication or if you have had a particularly successful communication interaction with XXXXXX. More info Q2 / Q7 D2 Mobility and Dexterity The RN/Team Leader will monitor the effectiveness of XXXXXX’s Physiotherapy plan and liase with the Physiotherapist. XXXXXXs Goals 1. To maintain his independence. 2. To improve his mobility and balance. 3. To build up his core body strength. Task Assistance required Frequency Outcome More info Physiotherapy Full x1 As required To build muscle tone B Treadmill Full x1 As required To build muscle tone B2 Walking Full x1 As required To build muscle tone B2 Swimming Full x2 As required To build muscle tone Interventions 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. To follow the physiotherapy plan. Aim for each day- Walk on treadmill 5-10 minutes Walk outside x 10-30 minutes, encourage XXXXXX to look ahead and lift his feet. Beach and forest walks. Exercises Biceps curls (holding velcro 0.5mg - 1kg weights) reps x 10, 2 sets each repeat both arms Hand to ceiling (holding velcro 0.5- 1.0kg weights reps x 10, 2 sets, repeat both arms Try indoor soccer/basketball with a soft ball. Throw/catch with a textured ball Ensure XXXXXX is wearing his ankle support brace when exercising. If unsure of physiotherapy interventions speak to the RN/Team Leader. Risk and Safety Management The RN/Team leader will frequently review and update the risk management plan. XXXXXXs Goals 1. 2. 3. Task To ensure XXXXXX is as safe as possible with minimal constraints. To ensure XXXXXX feels secure and his environment is free from clutter. To minimize the risks XXXXXX faces every day. Assistance required Frequency Outcome More info Hazards Assist x1 at all times Constantly For XXXXXX to remain safe To assess the risks Assist x1 constantly To ensure XXXXXX feels secure Interventions 1. 2. 3. 4. 5. 6. To never leave knives or forks on the bench, as XXXXXX will pick them up and tap his teeth with them and could injure himself. Maintain all areas inside the house free from clutter, as XXXXXX will pace around the living areas and could trip/ or fall when he has a drop seizure When cooking, place XXXXXX in his wheelchair and involve him in the cooking, as when he is left to wander he could burn himself. Ensure the safety switch is on when not using the oven or hotplates, as XXXXXX will fiddle with the knobs and turn the stove on. Make sure the safety alarm mats are on and working every shift. Report any potential hazards to RN/Team Leader. Head Injuries Management Plan: Mild 1. 2. 3. 4. 5. 6. 7. 8. 9. Assess XXXXXXs head and neck before moving him- he will grimace if touched and is painful. Complete a Glasgow Coma Scale assessment on XXXXXX before getting him up. If XXXXXX is unconscious or vomited more than once, ring ambulance/ team leader. Monitor for signs of concussion- this is a mild traumatic brain injury that alters the way the brain functions. The signs include altered levels of consciousness, headaches, confusion, dizziness and visual disturbance. Assess for any injuries such as cuts, bruising ,check if he can move his limbs. Apply first aid if required. Nothing to eat or drink for 4hrs post the head strike. Documentation- falls chart, incident report, daily diary In any concerns contact the RN/Team Leader. Moderate to severe: 1. 2. 3. If blood or clear fluid is escaping from the ears or nose keep XXXXXX on the left lateral position, ring ambulance/ RN/Team Leader. If XXXXXX is unconscious for more than five minutes, which means not responding to any stimuli, ring ambulance/ RN/Team Leader Complete all documentation as soon as possible. Continence Management The RN/Team leader will frequently review and update the risk continence plan. XXXXXX Goals: 1. To ensure XXXXXX remains continent B 2. 3. 4. 5. 6. To regulate XXXXXXs bowel and bladder patterns To maintain fluid intake 2.0 liters daily To maintain privacy and dignity at all times To ensure exercise to aid with bowel elimination To ensure skin integrity dry and intact Interventions 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Scheduled toileting times, (every two hours until bedtime) No longer than 5 minutes on the toilet Do not ask XXXXXX if he needs the toilet, take him as per the the scheduled times Pre and post toilet hygiene Aid XXXXXX with re- adjusting clothes Staff to remain with XXXXXX at all times when using the bathroom Ensure the bathroom door is closed when using the toilet If incontinent please document time, bowels/ bladder on toileting schedule Observe for any changes to his skin XXXXXX to wear pull ups when going to bed and have waterproof protection on his bed. Report any continence issues or changes to the RN/Team Leader. Outcomes 1. 2. 3. 4. For XXXXXX to remain continent To ensure XXXXXX has maintained a regular bowel and bladder regime To ensure XXXXXX is well hydrated For XXXXXX to sleep well and maintain his personal hygiene Transport and Escort The RN/Team leader will organise any services or repairs to XXXXXXs’s car. XXXXXXs Goals 1. For XXXXXX to live a full active life in his community and beyond. 2. For XXXXXX to travel safely and feel safe in the car. Task Assistance required Frequency Outcome More info XXXXXXs car Carers to drive XXXXXXs car Anytime C, H5 To ensure XXXXXX reaches his goals in the community Interventions 1. 2. 3. 4. 5. 6. 4. 5. Assist XXXXXX to the car and to get in/out of the car. The child proof lock on the back door must be on. Ensure his seat belt is properly fastened. Make sure the car is refuelled for the next shift and place the receipt in the book. Ensure the car is clean at the end of your shift, cord free vacuum is on charge in the shed. Once a month take though the car wash. XXXXXX is not responsible for any speeding or parking fines. If concerns about XXXXXX’s car report these to the RN/Team Leader. Use of Wheelchair – Short term only The RN/Team leader will review and update the use of the wheelchair on a regular basis. XXXXXXs Goals 1. 2. 3. 4. To ensure XXXXXX’s safety To reduce the falls risk To provide body support while aiding XXXXXX to achieve his goals (communicating, painting, writing, and social outings, meal preparation) For use in emergencies- Fire while preparing to leave house/ Venus Bay Interventions 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. While preparing to move due to potential fire outbreak, so care staff know where he is at all times The chair allows staff to move XXXXXX quickly to a safer environment as needed When going away from home for an extended period, place chair in car boot If XXXXXX is unsteady on his feet, or his balance is off, place XXXXXX in his wheelchair for his safety Every hour XXXXXX is to have a 15-minute break from the wheelchair, take him for a walk and to the toilet as per his scheduled toilet times Always ask XXXXXXs approval for going in the wheelchair (except if it’s for his safety, reasons must be documented in daily diary) Do not leave XXXXXX without any stimulation whilst in his chair, music, audible books, reading etc. Place lap buckle under his shirt as he may unbuckle it while fiddling with it. Staff can place XXXXXX in his wheelchair when they need to use the bathroom for XXXXXX’s safety whilst you leave the room (ask XXXXXX if it’s ok to sit in the chair whilst you go to the toilet) Always ask XXXXXX if he is ok with staying in the chair- direct questions Yes/No responses, if unsure use yes/no indicators on the kitchen bench When XXXXXX is communicating using the computer, ipad, or lightwriter, place XXXXXX in wheelchair to support his core body Any problems with XXXXXX’s use of the wheelchair, or mechanical issues with the chair itself, should be reported to the RN/Team Leader. Outcomes 1. 2. 3. 4. XXXXXX will have a reduced falls risk, and ensure his safety XXXXXX will be able to communicate and have more control over his fingers, if he doesn't have to think about his core body movement To improve achieving his goals To assist XXXXXX if he crashes and is unable to walk When the Chair should Not Be Used 1. 2. 3. It is NEVER to be used as a restraint It should not be used as an alternative to XXXXXX walking himself should he be able to do so It should never be used as a disciplinary measure Nursing and Allied Health Services The RN/Team leader will organise in-services for staff and liase with Allied Health workers regarding XXXXXX’s program. XXXXXXs Goals 1. 2. To enable XXXXXX to live a healthy and active life. To in-service support staff on matters of diet, general health and mental and physical wellbeing, medication administration, sleep, continence etc. Item Support required Frequency Outcome Nursing Medication, Diet, General Health, first aide, record keeping, inservicing staff, rostering of staff. When required and new staff. XXXXXX will live a healthy and active life and staff will approach their role with knowledge and confidence. G Physiotherapy In-service of support staff. Personal physical program for XXXXXX. 3 monthly Support staff will be able to assist XXXXXX with his physical program on a daily basis with knowledge and confidence. B Monthly XXXXXX will have short cut toe nails. Review of progress. Podiatry Toe nail cutting Ankle brace Toe support Ankle brace and toe support will assist when mobilizing. Toe support will ensure he doesn’t wear hole in the insoles of his shoes. Dietician Checking and monitoring XXXXXX’s Ketogrnic diet Cooking Ketrogenic means and snacks. RN/Team Leader creates menu in liason with the Dietician. Monthly XXXXXX will maintain a healthy, varied Ketogenic diet. XXXXXX will have fewer epileptic seizures. More info Behaviour Management The RN/Team leader will update XXXXXX’s behaviour management plan and in-service support workers regarding intervention strategies. Behaviour Goals 1. 2. 3. 4. Keeping my hands to myself. Staying with my support worker and don't wander off. To pick up my feet when walking and not kick at stones. Not to hurt carers when pinching/ lashing out. Behaviour: Interventions: Outcomes: Pinching and hitting/lashing out. To hold XXXXXX from behind or beside when assisting him to walk. Minimizes him hurting himself. Support workers or others close by. Maintain acceptance in the community. Wandering Maintain visual sight of XXXXXX at all times. XXXXXX will feel confident and supported. XXXXXX will remain safe. Dragging feet and Ankle brace when mobilizing kicking stones. Reminder to lift feet and not kick stones. XXXXXX will be able to walk over rough terrain. He will avoid tripping and falling. Any issues with XXXXXX’s behaviour need to be reported the RN/Team leader. More info Toileting Schedule: EXAMPLE Date Day Mon Bladder/ Bowel Time XXXXXX is to be toileted two hourly. 0700 0900 1100 1300 1500 1700 1900 2100 2300 C/ PU D T4/C D D D I/PU D D LG Tues Wed Thur Fri Sat Sun Mon Tues Wed Thur Fri Sat Sun LEGEND: If XXXXXX urinates and is continent, mark C/ PU or I/PU passed urine in appropriate time and day If XXXXXX uses his bowel’s, mark C- continent, I – incontinent, use bowel chart T1,2,3 then amount LG, MED, SM C = Continent (urinated successful on toilet) I = Incontinent (involuntary loss of urine) D = Dry (when checked and did not urinate) Mark as Continent, Incontinent, or Dry in hour checked. OVERNIGHT CODE: S – Asleep A – Awake but Settled O - out of bed W – Wet X – Attention Instructions Fill this in each night. Keep comments clear and note times for each item in each hour. Use the codes at the top for clarity and consistency. MONDAY Date 11 12 Worker 1 2 Checked Team Leader 3 4 5 6 TUESDAY Date 9th Jan 11 Worker 1 Checked Team Leader 3 11.30 (S) 3.45 (A) settled, placed radio on 12 12.45 (O) Back to bed 12.50 2 2.15 (W) (X) 4 4.20 (S) back in bed 2.45 Rechecked 3.55 (S) 5 6 Notes: 9th Jan 02.15 Tues changed bedding, gave XXXXXX a wash, clean Pj’s back in bed ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………