End-of-Life Care: Focus, Assessment, and Psychosocial Support
advertisement

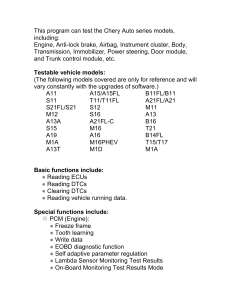
What is the focus of EOL care? Nurses spend more time with patients near the EOL than any other health care professionals. Respect, dignity, and comfort are important for the patient and family. Although there is no cure for the patient’s disease, the treatment plan still consists of assessment, planning, implementation, and evaluation. The main difference is that the focus of care is on the management of the symptoms. What is the importance of the assessment in EOL care? Nurses should be concise when completing assessments on EOL patients. Utilize resources available such as the health history data in the medical record to avoid tiring the patient with an interview. Assess the patient’s functional status, intake, patterns of sleep and rest, and response to the stress of the terminal illness. Review their coping skills and the family’s ability to manage the needed care and cope with the illness. Physical Assessment The physical assessment focuses on changes that accompany terminal illness and the specific disease process. Depends on the patient’s stability: o Done at least every 8 hours in the agency setting. o For patients cared for in their homes by hospice programs, assessment may occur weekly. Pay attention to patients who are nonverbal for subtle changes in their condition. As changes occur, documentation may be needed more often. Social Assessment Key elements of a social assessment include the relationships and patterns of communication among the family. Actively listen to concerns and evaluate the goals of the patient and family. Differences in expectations and interpersonal conflict can produce disruptions during the dying process and after the death of the loved one. Patient Monitoring Monitor the patient for multiple systems failing with attention to subtle physical changes. Neurologic assessment is especially important and includes level of consciousness, presence of reflexes, and pupil responses. Vital signs, skin color, and temperature show changes in circulation. Monitor and describe respiratory status, character and pattern of respirations, and characteristics of breath sounds. Assess nutrition and fluid intake, urine output, and bowel function since this gives data about renal and gastrointestinal functioning. Assess skin condition on an ongoing basis since fragile skin may easily break down. Limiting Assessments In the last hours of life, limit assessments to those that determine patient comfort. Assessment of pain and respiratory status may be the most important during this time. May be more comforting to the patient and family if you refrain from measuring blood pressure or checking for pupillary response. As death approaches, provide emotional and psychosocial support to the patient and family. Limit tasks that will not impact the comfort or outcome for the patient What are the clinical problems and the overall goals for the dying patient and their family? Clinical problems for the patient who is dying and their family include: Grief Dying process The overall goals for the patient who is dying are that the patient will: Make decisions about EOL care Experience a peaceful death It is important for the nurse to: Involve the patient and family in planning and coordinating EOL care Develop a comprehensive plan to support, teach, and evaluate patients and families Care goals during the last stages of life: Involve comfort and safety measures and care of the patient’s emotional and physical needs May include determining where the patient would like to die and whether this is possible o For example, the patient may want to die at home, but the family may object or be unable to manage the care. What is the role of the nurse as the patient prepares for death? Nurses should advocate for the patient’s wishes to be met. Patients and families need ongoing information on the disease, the dying process, the care the nurse will be providing, and how to cope. Denial and grieving may be barriers to learning for both the patient and family. As death approaches, respond appropriately to the patient’s psychosocial manifestations at the EOL (Table 10.7). Table 10.7 Nursing Management: Psychosocial Care at End of Life Dimensions Nursing Management Preparing for Death Serious illness can create strain on relationships. It is important to facilitate meaningful discussions for the patient and family to prepare for death. They may reconcile the past to find meaning in the present. Spiritual Needs Religion, faith, and spirituality may be sources of strength for patients and families Patients and family members may experience spiritual longing. Unusual Communication This may indicate altered coping that may prevent the patient from resolving issues and letting go. Encourage the patient and family to share their feelings of love, sadness, loss, and forgiveness. Saying goodbye can be therapeutic. Encourage the use of physical touch (e.g., hand holding, hugging) and expressions such as crying. Allow the patient and family privacy to express their feelings and comfort one another. Assess spiritual needs, cultural norms, hopes, values, and fears Address the needs of the family and caregivers Allow patient to express concerns about quality of life, fear of death or dying, spiritual practices, and significant relationships. Recognize the presence of spiritual or existential distress. Promote visits by spiritual care service provider, chaplain, family member. Assess for depression, anxiety, and/or delirium. Encourage the family to talk with and reassure the patient. Dimensions Comorbid psychiatric conditions may worsen. Patients may become restless and agitated, which may be a manifestation of terminal delirium. End-of-Life Dreams and Visions Patients may be seen talking to persons who are not there or seeing places and objects not visible. They may report dreams of living or deceased loved ones. These experiences may comfort the patient in coming to terms with meaning in life and transition from it. Withdrawal This may be an emotional response or part of grieving. Patient near death may seem withdrawn from the physical environment, maintaining the ability to hear but unable to respond. Nursing Management Coordinate with the IPT to assist with counseling and communication. Assess for the presence, distress, or comfort from these visions. Affirm the patient’s experience as a part of transition from this life. Teach families and caregivers about the patient’s experiences. Allow the patient to sleep and rest. Converse as though the patient were alert, using a soft voice and gentle touch. Provide education to families and caregivers. Encourage meaningful tasks and discussions during periods of wakefulness. How does the nurse manage psychosocial elements near EOL? Patients experience many different emotions near the end of life. Anxiety and Depression Causes may include: Uncontrolled pain and dyspnea o Respiratory distress and dyspnea are common near the EOL. o The sensation of air hunger results in anxiety for the patient and family. o Current treatments include opioids, bronchodilators, and oxygen, depending on the cause of the dyspnea. Psychosocial factors related to the disease process or impending death Altered physiologic states Drugs used in high dosages Anxiety often related to fear Encouragement, support, and teaching may help alleviate anxiety. Management may include both medications and nonpharmacologic interventions. Relaxation strategies, such as relaxation breathing, muscle relaxation, music, and imagery, may be useful. Anxiety-reducing agents (e.g., anxiolytics) may help produce relaxation. How does the nurse manage psychosocial elements near EOL? Patients experience many different emotions near the end of life. Anxiety and Depression Anger Anger is a normal response to grief. A grieving person cannot be forced to accept the loss. The surviving family members may be angry with the dying loved one who is leaving them. Encourage the expression of feelings. The nurse may be the target of the anger. o Understand the anger response and avoid reacting on a personal level. Hopelessness and Powerlessness Feelings of hopelessness and powerlessness are common. Encourage realistic hope within the limits of the situation. Support the patient’s involvement in decision making to foster a sense of control and autonomy. Allow the patient and family to deal with what is within their control and help them recognize what is beyond their control. Fear Fear is a typical feeling associated with dying. Specific fears include fear of pain, fear of shortness of breath, fear of loneliness and abandonment, and fear of meaninglessness. Some fear death is painful but do not want the medication side effects of grogginess or sleepiness. o Pain relief measures do not have to deprive the patient of the ability to interact with others. o Assure the patient and family that medication will be given promptly when needed and that any side effects will be managed. o As many EOL patients are unable to swallow, other routes, such as patches, sublingual, and rectal, may be used. o Consider alternative methods like massage, music, aromatherapy, and mindfulness. Most terminally ill and dying people do not want to be alone. Being present offers support and comfort (Fig. 10.8). Holding hands, touching, and listening are important nursing interventions. Providing companionship allows the patient a sense of security. Fear of meaninglessness leads people to review their lives. Assist patients with life review to help them recognize the value. Practical ways of helping may include looking at photo albums or collections of important mementos while sharing thoughts and feelings. Fig. 10.8 Dying patients often want someone whom they know and trust to stay with them. (© KatarzynaBialasiewicz/iStock.com) Patients and family members may have difficulties expressing their feelings. Empathy and active listening are essential at EOL. Recognize that silence is often an effective communication technique. A family conference can create a good environment for communication and help to prepare family members for changes in the patient’s emotional and cognitive function as death nears. What does physical care focus on at EOL? Physical care at the EOL focuses on symptom management and comfort (Table 10.8). Priority is meeting the patient’s physiologic and safety needs. Physical care focuses on the needs for oxygen, nutrition, pain relief, mobility, elimination, and skin care. People who are dying deserve and require the same physical care as people who are expected to recover. Discuss the goals of care with the patient and family before treatment begins. Table 10.8 Nursing Management: Physical Care at End of Life Manifestation Nursing Management Anorexia, Dehydration, Nausea, and Vomiting May be caused by complications of disease process Hunger and thirst decrease at EOL Dehydration is common Medications contribute to nausea Constipation, impaction, and bowel obstruction can cause anorexia, nausea, vomiting Assess the patient for nausea or vomiting, and possible contributing causes Provide antiemetics as needed and before meals if ordered Offer and provide frequent meals with small portions of favorite foods. Offer culturally appropriate foods Manifestation Nursing Management Bowel Patterns Immobility, opioid use, depression, lack of dietary fiber in the diet, dehydration, obstructive cancer can cause constipation Diarrhea may occur from laxative use, obstruction, fecal impaction, infection, medications, chemotherapy Do not force the patient to eat or drink Provide frequent mouth care Encourage consumption of ice chips and sips of fluids or use moist cloths to moisten the mouth Use moist cloths and swabs for unconscious patients to avoid aspiration Apply lubricant to the lips and oral mucous membranes as needed Ensure uninterrupted mealtimes Teach family that hunger and thirst naturally decreases at EOL. Assess bowel function and associated symptoms Assess for and remove fecal impactions Encourage movement and physical activities as tolerated Encourage fiber in the diet if appropriate. Discuss the role of IV fluids in context of goals of care Use suppositories, stool softeners, laxatives, and/or enemas as ordered, especially if on opioids Assess for confusion, agitation, restlessness, and pain, which may indicate constipation. Encourage the intake of simple carbohydrates, if appropriate, Manifestation Nursing Management and use of antidiarrheals as needed. Oral Conditions Candidiasis may be present due to chemotherapy, immunosuppression Xerostomia or dry mouth is common. This may be due to comorbidities, medication, radiation, dehydration Delirium and Restlessness Develops over a short period of time with severity fluctuating through the day Characterized by confusion, disorientation, restlessness, clouding of consciousness, incoherence, fear, anxiety, excitement, hallucinations May be misidentified as depression, psychosis, anger, anxiety Contributing factors include medications, underlying disease, environment, sensory impairment, metabolic problems Associated with adverse outcomes Considered reversible Common in final days of life Assess oral cavity and cause of problems If ordered, give oral antifungal Clean dentures and other dental appliances to prevent reinfection Provide oral hygiene and use soft toothbrush or sponge Perform a thorough assessment for delirium using a validated tool Assess for risk factors for delirium, including pain, constipation, and urinary retention and treat as needed. Include nonpharmacologic interventions as appropriate Provide a room that is quiet, well lit, and familiar to reduce the effects of delirium Reorient the patient to person, place, and time with each encounter Give ordered antipsychotics, benzodiazepines, and sedatives as needed Stay physically close to frightened patient. Reassure in a calm, soft voice with touch and slow strokes of the skin Avoid physical restraints whenever possible Manifestation Difficulty Swallowing May occur due to cancer, neurologic problems, weakness Common at EOL May lead to aspiration of liquids and/or solids, pneumonia, malnutrition, dehydration, death Drooling/inability to swallow secretions may be present Nursing Management Provide family with emotional support and encouragement in their efforts to cope with the behaviors associated with delirium Assess level of alertness and safety of oral intake Collaborate with IPT for evaluation based on goals of care. Referral for speechlanguage pathologist If needed, use alternative routes for (rectal, buccal, transdermal, IV) drug administration for symptom management Modify diet to focus on comfort or pleasure, as tolerable by patient Teach family on safety and risk for aspiration Review medications and stop nonessential medications Hand feed small meals Elevate the head for meals and at least 30 minutes after What is the nurse’s role in managing physical care manifestations at EOL? Table 10.8 concludes with further discussions about physical nursing care that should be provided at end of life. Table 10.8 Nursing Management: Physical Care at End of Life – cont’d Manifestation Nursing Management Dyspnea, Terminal Secretions, and Cough Can significantly impair quality of life. Dyspnea is often accompanied by chest tightness, fear of suffocation, anxiety Terminal secretions, or death rattle, is noisy breathing from secretion accumulation. Very common in the hours before death Presence of terminal secretions can be distressing to family members Cough is a reaction to an irritation of the respiratory tract, and can be debilitating Myoclonus Mild to severe abnormal movements Can be caused by medications, metabolic Assess respiratory status regularly Assess for anxiety and other associated symptoms including pain and fatigue Elevate the head and/or position patient on side to improve chest expansion Use a fan or air conditioner to help movement of cool air Teach and encourage the use of pursedlip breathing Teach relaxation and guided imagery techniques for relaxation Administer medications as needed: o Opioids for dyspnea o Benzodiazepines for associated anxiety o Anticholinergics for secretions o Antitussives, mucolytics, and expectorants Oxygen use should be based on the goals of care at the EOL Avoid deep suctioning. Gentle oral suctioning may be used Teach the patient and family on these symptoms and treatments. Provide emotional support for caregivers Assess for onset, duration, any discomfort or distress Review potential causes, including medications Treat symptoms with benzodiazepines Manifestation imbalances, central nervous system damage Nursing Management Provide education and emotional support to patient and family Assess pain thoroughly and regularly to determine the onset, duration, quality, intensity, location, and aggravating and alleviating factors Pain Is a major symptom at EOL, can contribute to suffering, and the most feared Often associated with other symptoms and sources of distress Can be acute or chronic, neuropathic, nociceptive, inflammatory, and/or mechanical Often requires opioids for management Bone pain can be caused by metastases, fractures, arthritis, immobility Physical and emotional stressors can worsen pain Assess for associated symptoms including anxiety, social or spiritual distress Skin Breakdown Give medications around the clock, in a timely manner, and on a regular basis to provide constant relief rather than waiting until the pain is unbearable and then trying to relieve it Provide nonpharmacologic interventions, such as guided imagery, massage, and relaxation techniques as needed o Frequently evaluate effectiveness of pain relief measures Ensure that the patient is on a correct, adequate drug regimen Monitor for side effects of opioids, such and nausea and constipation, and treat as appropriate Teach the patient on all interventions and medications Do not delay or deny pain relief measures to a terminally ill patient Manifestation Skin integrity is hard to maintain at end of life Immobility, urinary and bowel incontinence, dry skin, malnutrition, anemia, friction, and shearing forces lead to a high risk for skin breakdown Disease and other processes may impair skin integrity In the last days of life, circulation to the extremities decreases and they become cool, mottled, cyanotic Nursing Management Assess skin for signs of breakdown or injury Assess risk factors for skin breakdown and implement protocols to prevent Perform wound assessments as needed Follow protocols for dressing wounds Premedicate if turning, repositioning, or wound care cause discomfort Follow protocols to prevent skin irritation and breakdown from urinary and bowel incontinence Use blankets to cover for warmth. Use lotions to prevent dryness Urinary and Bowel Incontinence May result from disease progression or changes in the level of consciousness, medications, decreased mobility As death becomes imminent, the perineal muscles relax, causing incontinence of bowel and bladder Urine production is decreased at EOL Weakness and Fatigue Decline in mental status and energy is expected Causes include metabolic demands related to disease, underlying chronic condition, cancer, Assess urinary and bowel function Use absorbent pads for incontinence and barrier creams to prevent irritation Follow protocols for the use and management of indwelling or external catheters Follow protocols to prevent skin irritation and breakdown from urinary and bowel incontinence Assess the patient’s tolerance for physical and mental activities Help the patient identify and complete valued or desired activities Modify and time nursing interventions to conserve energy Manifestation malnutrition, insomnia, infection Nursing Management Refer to physical and occupational therapy for safe movement Review nutrition and hydration based on goals of care Give frequent rest periods and adjust environment to allow for quiet surroundings What are the steps to providing postmortem care? After a patient is pronounced dead, the nurse will need to prepare or delegate preparing the patient’s body for immediate viewing by the family. Consider cultural customs and follow agency policy for postmortem care (Table 10.9). When the death is unexpected, preparing the patient’s body for viewing or release to a funeral home depends on state law and agency policy. Be respectful and allow the family privacy and as much time as they need with the deceased patient. Table 10.9 Nursing Management: Postmortem Care Provide privacy throughout the process. Teach family and caregivers on process if present. Assess cultural and/or religious preferences or rituals about this process from family or caregivers before starting. Obtain supplies needed before starting. This may include a kit or individual items. Ask for help if needed. Wash hands, and use protective equipment as needed. Close the patient’s eyes and jaw. Replace dentures; if unable, place in labeled cup. Remove jewelry, eyeglasses, and other personal belongings. Remove tubes and dressings (per policy). Wash the body as needed then apply clothes selected by the patient or family (home), or a clean gown (agency). Comb and arrange the hair neatly. Place a waterproof pad or incontinence brief to absorb urine and feces. Straighten the body, placing the arms at their sides or across the abdomen with palms down. Follow instructions per policy in home or agency setting. What are the signs of abnormal grief reactions with caregivers at EOL? Family caregivers are important in meeting the patient’s physical and psychosocial needs. Role includes working and communicating with the patient and other family members, supporting the patient’s concerns, and helping the patient resolve any unfinished business. Families often face emotional, physical, and economic consequences from caring for a family member who is dying. The caregiver’s responsibilities do not end when the patient is admitted to an acute care, inpatient hospice, or long-term care agency. Being present during a family member’s dying process can be highly stressful. Recognize signs and behaviors of abnormal grief reactions among family members. Warning signs may include: o Dependency and negative feelings about the dying patient o Inability to express feelings o Sleep problems o A history of depression o Difficult reactions to previous losses o Perceived lack of social or family support o Low self-esteem o Multiple previous bereavements o Alcohol or substance use Caregivers with concurrent life crises (e.g., divorce) are especially at risk. Encourage family caregivers and other family members to continue their usual activities where possible to maintain some control over their lives. Inform caregivers about resources for support, including respite care, community counseling, and local support in working through grief. Encourage caregivers to build a support system of extended family, friends, faith community, and clergy to call on to express any feelings they are experiencing. What are the special needs of nurses who provide EOL care? Caring for patients and their families at the EOL is rewarding but is also challenging, intense and emotionally charged. Nurses who care for the dying need to recognize their own needs when dealing with grief and dying. Be aware of how grief personally affects you. Express feelings of sorrow, guilt, and frustration. Recognize own values, attitudes, and feelings about death. o Realizing that it is okay to cry with the patient or family during the EOL may be important for your well-being. To meet personal needs, focus on interventions to decrease stress: o Hobbies o Adequate sleep o Personal time o Peer support system o Support system beyond the workplace. Many hospice agencies offer support groups and discussion sessions that can help nurses cope.