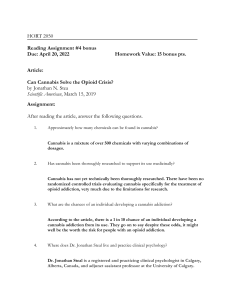
Journal of Psychiatric Research 156 (2022) 690–697 Contents lists available at ScienceDirect Journal of Psychiatric Research journal homepage: www.elsevier.com/locate/jpsychires Does cannabis use impact cognitive behavioural therapy outcomes for anxiety and related disorders? A preliminary examination Mélise J. Ouellette a, c, Karen Rowa a, b, c, *, Duncan H. Cameron a, Ashleigh Elcock a, Noam Soreni a, b, Elizabeth J. Pawluk a, b, Randi E. McCabe a, b, c a b c Anxiety Treatment and Research Clinic, St. Joseph’s Healthcare, 100 West 5th St., Hamilton, Ontario, L8N 3K7, Canada Department of Psychiatry and Behavioural Neurosciences, McMaster University, 1280 Main Street West, Hamilton, Ontario, L8S 4L8, Canada Department of Psychology, Neuroscience, and Behaviour, McMaster University, 1280 Main Street West, Hamilton, Ontario, L8S 4L8, Canada A R T I C L E I N F O A B S T R A C T Keywords: Cannabis Marijuana Cognitive behavioural therapy (CBT) Anxiety Cannabis use disorder Objectives: The current study examined whether cannabis use frequency and cannabis-related problem severity (as per the Cannabis Use Disorder Identification Test-Revised) predicted outcomes of cognitive behavioural therapy (CBT) for anxiety and related disorders. It was predicted that greater frequency of cannabis use and greater cannabis-related problem severity would be associated with dampened treatment outcomes compared to less severe cannabis use presentations. Methods: Participants were 253 adults seeking treatment for anxiety and related disorders. Cannabis use was categorized as non-use (n = 135), infrequent use (using monthly to 4 times per month; n = 45), and frequent use (using 2 or more times per week; n = 73). Individuals who reported using cannabis completed cannabis use and cannabis-related problem measures before starting a CBT group. Participants also completed a weekly symptomspecific measure of anxiety symptoms throughout CBT. Results: As hypothesized, frequent cannabis use was associated with poorer outcomes in CBT for anxiety and related disorders compared to non-use. Despite this, individuals who used cannabis frequently still experienced a statistically significant decrease in their anxiety symptoms from pre-to post-CBT, with a large effect size (d = − 0.87). Cannabis-related problems was not a significant predictor of CBT outcomes. Conclusions: Cannabis use frequency was associated with poorer CBT outcomes for anxiety and related disorders, however these individuals still made notable treatment gains. The mechanism driving this relationship remains unclear. Future studies should attempt to replicate the current findings and examine possible mechanisms. 1. Introduction Cognitive behavioural therapy (CBT) is considered the gold standard anxiety and related disorders (i.e., trauma- and stressor related and obsessive-compulsive and related disorders; Beck, 1993; Otte, 2011) treatment. CBT provides patients with cognitive and behavioural skills to manage anxiety and related disorder symptoms, which are practiced between sessions to enhance outcomes (Kazantzis et al., 2010; Rowa et al., 2019). Individuals seeking treatment for anxiety and related disorders often endorse cannabis use (Ouellette et al., 2019). Cannabis may be used to manage anxiety symptoms (Simons et al., 1998; Skalisky et al., 2019), and cannabis use and anxiety may be mutually maintaining (Buckner et al., 2012; Stewart and Conrod, 2008). For example, individuals with anxiety may use cannabis as a subtle avoidance strategy to manage their anxiety symptoms in the short term (but maintains anxiety in the long-term; Buckner et al., 2019; McManus et al., 2008; Salkovskis et al., 1999), and to manage symptoms such as cannabis craving and with­ drawal which have been associated with anxiety (American Psychiatric Association, 2013; Buckner et al., 2012; Cornelius et al., 2008). Addi­ tionally, after therapy for cannabis dependence, residual anxiety symptoms have been associated with poorer outcomes, while reduced anxiety has been associated with better outcomes, suggesting that anx­ iety may increase the risk of cannabis relapse (Buckner and Carroll, 2010; Stewart and Conrod, 2008). Taken together, cannabis use and anxiety appear to be associated and may be important to consider in treatment planning. Cannabis may be used to avoid or escape negative emotions (e.g., * Corresponding author. Anxiety Treatment and Research Clinic, St. Joseph’s Healthcare, 100 West 5th St., Hamilton, Ontario, L8N 3K7, Canada. E-mail addresses: ouellemj@mcmaster.ca (M.J. Ouellette), krowa@stjoes.ca (K. Rowa). https://doi.org/10.1016/j.jpsychires.2022.10.054 Received 10 June 2022; Received in revised form 23 October 2022; Accepted 26 October 2022 Available online 31 October 2022 0022-3956/© 2022 Elsevier Ltd. All rights reserved. Downloaded for Anonymous User (n/a) at Pontifical Catholic University of Chile from ClinicalKey.com by Elsevier on February 21, 2023. For personal use only. No other uses without permission. Copyright ©2023. Elsevier Inc. All rights reserved. M.J. Ouellette et al. Journal of Psychiatric Research 156 (2022) 690–697 Buckner et al., 2014; Buckner et al., 2019). Avoidance ultimately maintains anxiety (McManus et al., 2008; Salkovskis et al., 1999) and a core feature of CBT for anxiety is to approach, rather than avoid, anxiety-inducing stimuli (Aderka et al., 2013; Riccardi et al., 2017). Using cannabis as an avoidance strategy may dampen treatment out­ comes for anxiety and related disorders if left unaddressed. Additionally, there is evidence of cognitive impairments and amotivation associated with cannabis use (Broyd et al., 2016; Meier and White, 2018) that may be challenging in a cognitively and motivationally demanding treatment like CBT. Research on cannabis use’s impact on CBT outcomes is sparse and equivocal. Some studies suggest no effect of cannabis use on outcomes of brief CBT for anxiety and depression and integrated CBT for anxiety and substance use (Bricker et al., 2007; Ruglass et al., 2017). Notably, these studies excluded individuals with more severe cannabis use pre­ sentations (e.g., cannabis dependence), which may be an important factor in treatment outcomes (Bricker et al., 2007; Ruglass et al., 2017). Other research has reported a moderating effect of baseline cannabis use and problems on outcomes for those with comorbid Cannabis Use Dis­ order (CUD) and an anxiety disorder (Buckner et al., 2021). An inte­ grated cannabis and anxiety reduction CBT protocol led to better outcomes than motivational enhancement and CBT (MET-CBT) for CUD in those who had more severe baseline cannabis use and related prob­ lems, but those with less severe cannabis use and problems experienced better outcomes with MET-CBT than the integrated protocol. Therefore, individuals with more severe cannabis use may not experience optimal treatment outcomes if only one concern is addressed at once. While research on integrated treatments is highly valuable, traditionally, treatment for co-occurring anxiety and substance use disorders have been separate (Brady et al., 2013), thus it is likely that most clinicians trained in anxiety disorders are not trained in integrated anxiety and substance use treatments, and refer individuals to substance use-focused programs (Skinner et al., 2004). Additionally, studies that have found no impact of cannabis use on outcomes have used brief protocols and no research has investigated this question using standard protocols. Taken together, it is important to know if various cannabis use severity levels dampen CBT outcomes using standard protocols to inform best practices in this area. This study’s purpose is to examine whether cannabis use frequency and cannabis-related problem severity at baseline are associated with standard-length CBT outcomes for anxiety and related disorders. Higher cannabis use frequency was predicted to be associated with poorer CBT outcomes than non-use given the mutually maintaining relationship between cannabis use and anxiety. It was predicted that individuals with more severe cannabis-related problems would likely reflect more severe cannabis-related functional impairment, which would also dampen CBT outcomes. week” or “4 or more times a week”, and non-use was defined as denial of cannabis use in the past 6 months. Cannabis use frequency categories were chosen to be similar to other studies (e.g., Buckner and Schmidt, 2008; Henry et al., 2014). 2.2. Procedure Participants were referred to an anxiety and related disorders clinic for specialized assessment and intervention services. Referred in­ dividuals had the opportunity to provide informed consent to use their clinical data for research. Participants’ mental health symptoms were assessed by trained clinicians. Sixty-eight percent of participants were assessed using the Diagnostic Assessment Research Tool (DART; McCabe et al., 2017; Schneider et al., 2021), 22% received a psychiatric consult, and 4% received an assessment from a nurse specialized in anxiety and related disorders. To address their presenting concerns, individuals were referred to a symptom-specific CBT group for either social anxiety dis­ order (SAD), generalized anxiety disorder (GAD), panic disorder (PD) and/or agoraphobia, obsessive-compulsive disorder (OCD), or post­ traumatic stress disorder (PTSD). CBT groups were composed of 12, 2-hour weekly sessions. CBT protocols included psychoeducation and cognitive and behavioural skills (e.g., exposure to anxiety-inducing sit­ uations) tailored to the disorder being treated. The only protocol without behavioural skills was the PTSD group as the type of CBT used was Cognitive Processing Therapy (Resick et al., 2016). Within the two weeks prior to beginning group CBT, participants completed measures of cannabis use patterns, cannabis-related problems, anxiety-related functional impairment, and disorder-specific anxiety symptoms. They completed weekly symptom-specific anxiety measures throughout CBT. The institution’s local research ethics board approved the collection and use of this data, and all participants provided written and informed consent. 2.3. Measures The Cannabis Use Disorder Identification Test-Revised (CUDITR) is an 8-item self-report screening tool for CUD in the past 6 months (Adamson et al., 2010) and was used in this study to reflect cannabis-related problems. All 8 items were summed for a total score. Total scores of 13 or above indicate likely CUD (Adamson et al., 2010). This study’s Cronbach alpha on the CUDIT-R at baseline was 0.81, suggesting good internal consistency. Illness Intrusiveness Rating Scale (IIRS) is a 13-item self-report measure of illness-related daily life disruptions (Devins, 2010; Devins et al., 1983). It was adapted to measure the functional impact of anxiety with the question stem of “How much does your anxiety and/or its treatment interfere with your:” (e.g., health, work). This study’s pre-treatment alpha value was 0.83 and post-treatment value was 0.90. The Social Phobia Inventory (SPIN) is a self-report measure of SAD symptoms (Connor et al., 2000). The current study included only those with total scores within the “moderate” SAD symptom range and above (total scores of 31 and above; Moscovitch et al., 2011; Moser et al., 2008). The SPIN had a Cronbach alpha that ranged from 0.74 to 0.95 from pre-to post-treatment in this study. The Penn State Worry Questionnaire (PSWQ) is a self-report measure of trait worry and a screener for GAD symptoms, administered at pre- and post-treatment (Fresco et al., 2003; Meyer et al., 1990). The PSWQ-Past Week (PSWQ-PW; Stöber and Bittencourt, 1998) was also administered weekly throughout CBT. The PSWQ and PSWQ-PW demonstrated good internal consistency in this study, with Cronbach alphas ranging from 0.85 to 0.97 from pre-to post-treatment. The Panic Disorder Severity Scale (PDSS) is a self-report measure of PD (Furukawa et al., 2009; Shear et al., 1997). The current study’s PDSS showed good internal consistency with Cronbach alphas ranging from 0.76 (acceptable) to 0.97 (excellent). The Obsessive-Compulsive Inventory-Revised (OCI-R) is a measure of OCD symptoms (Foa et al., 2002). The current 2. Methods 2.1. Participants Participants were 253 adults seeking treatment for anxiety and related disorders (i.e., trauma- and stressor related and obsessivecompulsive and related disorders). Based on diagnostic assessment re­ sults by a psychiatrist, clinical psychologist, graduate-level clinical psychology student, or other mental health professional, they were referred to a symptom-specific CBT group at the clinic. Additionally, participants had to score above the cut off of a relevant symptom mea­ sure at pre-treatment, indicating clinically significant symptoms matching their CBT group. Participants’ cannabis use was categorized into non-use (n = 135), infrequent use (n = 45), and frequent use (n = 73) based on self-reported use frequency on the Cannabis Use Disorder Identification Test-Revised (Adamson et al., 2010). Infrequent use was defined as using “Monthly or less” or “2–4 times a month”, frequent use was defined as “2–3 times a 691 Downloaded for Anonymous User (n/a) at Pontifical Catholic University of Chile from ClinicalKey.com by Elsevier on February 21, 2023. For personal use only. No other uses without permission. Copyright ©2023. Elsevier Inc. All rights reserved. M.J. Ouellette et al. Journal of Psychiatric Research 156 (2022) 690–697 study’s Cronbach alpha ranged from 0.55 to 0.83 for the OCI-R, which is likely a reflection of the small sample size of participants with OCD. The PTSD Checklist for DSM-5 (PCL-5) measures PTSD symptoms (Weathers et al., 2013), with total scores between 31 and 33 and above indicating likely PTSD (Bovin et al., 2016). To be conservative, the current study used the cut off score of 33 to be included in the study. The PCL-5 showed good internal consistency with Cronbach alphas ranging from 0.86 to 0.97 from pre-to post-treatment in the current study. Given that the SPIN, PSWQ, PDSS, OCI-R, and PCL-5 measure spe­ cific symptoms for some of the most common anxiety and related dis­ orders (Kessler et al., 2012), collectively they provide a broad representation of core symptoms of the anxiety and related disorders population. possible, sample means for non-anxious controls were used to calculate z-scores to represent the general population mean, which were 48.8 (SD = 13.8) for the PSWQ (Meyer et al., 1990), 18.82 (SD = 11.10) for the OCI-R (Foa et al., 2002), and 6.10 (SD = 6.00) for the PDSS-SR (Shear et al., 2001). The two exceptions were the PSWQ-PW and the SPIN. No control sample was available for the PSWQ-PW. Given that the baseline PSWQ and PSWQ-PW scores were comparable between baseline and session 1, and session 12 and post-treatment (ps > .05), we used a comparable score from its validation study (Stöber and Bittencourt, 1998) which was the mid-treatment mean of 45.43 (SD = 16.48). The non-anxious controls’ SPIN score is 12.10 (SD = 9.30). This score is low compared to sample means for SAD and therefore, results in overly-inflated z-scores relative to the other disorder-specific samples in the current study. Additionally, some researchers support a higher cut-off value of 30 on the SPIN, rather than the proposed cut-off of 22.10 (Moscovitch et al., 2011; Moser et al., 2008). As such, the “mildly-im­ paired” subsample mean of 22.70 (SD = 10.00) was used (Connor et al., 2000). This method of analysis has been used in previously published studies (e.g., Milosevic et al., 2022). 2.4. Data analysis Primary outcomes were analyzed using hierarchical linear modelling (HLM; Raudenbush & Byrk, 2002). HLM was used because it can address missing data at Level-1 (i.e., the outcome variable assessing anxiety and related disorder symptoms) and it is relatively robust to unbalanced designs. The estimation method was restricted maximum likelihood (REML). To determine if cannabis use frequency groups significantly differed in rates of change in anxiety and related disorder symptom severity throughout treatment, an HLM was conducted with time (coded with the unit of measurement as one week) at Level-1 and cannabis use frequency at Level-2 (where non-use was the reference category, and infrequent use and frequent use were incorporated as individually dummy-coded variables). Follow-up individual one-level HLMs were performed to assess change in symptom severity within each cannabis use category. An additional HLM analysis was completed to determine the effect of cannabis-related problems, as assessed by the CUDIT-R (at Level-2), on change in anxiety and related disorder symptom severity throughout treatment. This analysis was performed in a sample of all individuals who endorsed cannabis use (i.e., both frequent and infrequent) to determine if cannabis use problems had an impact on treatment out­ comes. Effect size for primary analyses is reported as Cohen’s d, to be interpreted as small = 0.20, medium = 0.50, and large = 0.80 (Cohen, 2013). A single (3 cannabis frequency use group X 2 Time) repeatedmeasures ANOVA was used to assess the impact of cannabis use status on improvement in anxiety-related illness intrusiveness from pre-to post-treatment. An intent-to-treat approach was used to maximize sample size and external validity of results. Data were collected weekly from pre-to posttreatment, for a total of 14 time points. Missing symptom data ranged from 0.0% at pre-treatment to a maximum of 49.4% at post-treatment, and the overall level of missing data points in the dataset was 32.4%. These data were estimated using REML. Missing data was not imputed for Level-2 variables, and only individuals who had complete data at Level-2 were used in the analysis. Data was not imputed for the repeated measures ANOVA. The uneven sample sizes across groups, and the relatively low sample sizes for the OCD and PD groups, precluded a meaningful analysis within or across specific disorders. Therefore, z-scores were calculated for each symptom measure to collapse participants across diagnostic groups. The z-score formula is z = (participants symptom-specific measure total score – non-anxious population mean)/non-anxious population’s stan­ dard deviation. Z-scores were calculated using available sample norms from validation studies for each questionnaire. Together, the symptomspecific anxiety and related disorder measures provide a broad overview of core symptoms for some of the most common anxiety and related disorders (Kessler et al., 2012). Due to methodological differences be­ tween validation studies and symptom-specific questionnaires, z-scores were only used for the full-sample analysis, whereas raw scores were used for individual group analyses (i.e., descriptive information). Where 3. Results 3.1. Descriptive statistics Table 1 reports demographics, diagnostics, and baseline CUDIT-R scores. Of the 253 participants, 148 (58.50%) had at least one addi­ tional diagnosis documented. Table 2 reports mean symptom-specific measure scores. Fig. 1 demonstrates participants’ CBT group alloca­ tion and number of participants who completed and terminated CBT early. The CBT retention rate was 77.1% (n = 195), with no difference in early termination or CBT completion across groups, χ2(2) = 2.50, p = .29, V = 0.099, or association with CUDIT-R scores H(1) = 0.04, p = .851, ε2 = 0.000. 3.2. Symptom change over time as a function of cannabis use Table 3 presents the full results for all HLM models for the primary analysis assessing the effect of cannabis use frequency or cannabisrelated problem severity on the trajectory of change in anxiety and related disorder symptom severity throughout CBT. There was a sig­ nificant effect of frequent cannabis use on change in symptoms over time (b = 0.04, SE = 0.02, t = 2.72, df = 250, p = .007, d = 0.17) but not infrequent use (b = 0.02, SE = 0.01, t = 1.52, df = 250, p = .129, d = 0.10), relative to non-use. Individuals who use infrequently demon­ strated a non-significant effect when compared against individuals who use frequently (b = − 0.17, SE = 0.02, t = − 0.89, df = 250, p = .376, d = − 0.06). These results indicate that frequent cannabis use was associated with less improvement in anxiety and related disorder symptom severity throughout treatment compared to non-use, albeit with a small effect (Fig. 2). Individual one-level HLMs confirmed that the non-use (b = − 0.13, SE = 0.01, t = − 13.73, df = 135, p < .001, d = − 1.18), infrequent use (b = − 0.10, SE = 0.01, t = − 8.59, df = 44, p < .001, d = − 1.28), and frequent use (b = − 0.09, SE = 0.01, t = − 7.42, df = 71, p < .001, d = − 0.87) groups demonstrated significant reductions in symptom severity throughout CBT. Therefore, although all three groups experienced sig­ nificant improvements in anxiety and related disorder symptoms from pre-to post-treatment, the rate of change was significantly slower in individuals who use cannabis frequently compared to those who do not use cannabis. Notably, when examining end-of-treatment symptomspecific measure raw score means, two diagnostic groups had mean scores representing subclinical symptoms and three groups had means above clinical cut offs. Therefore, overall the sample was considered as “improved but not recovered” as per Jacobson et al. (1999). Z scores at each timepoint are reported in Table 4. Cannabis-related problem severity, as per the CUDIT-R, did not significantly predict anxiety and related disorder symptom change in the 692 Downloaded for Anonymous User (n/a) at Pontifical Catholic University of Chile from ClinicalKey.com by Elsevier on February 21, 2023. For personal use only. No other uses without permission. Copyright ©2023. Elsevier Inc. All rights reserved. M.J. Ouellette et al. Journal of Psychiatric Research 156 (2022) 690–697 Table 1 Demographics. Table 1 (continued ) Non-Use (n = 135) Infrequent Use (n = 45) Frequent Use (n = 73) Variable Age (years) Mean (SD) Gender 36.56 (12.71) 32.49 (12.22) 35.42 (9.41) Male Female Transgender Relationship status 22.2% 76.3% 1.5% 26.7% 71.1% 2.2% 30.1% 67.1% 2.7% Single In a relationship Education 41.5% 57.8% 33.3% 62.2% 42.5% 57.5% Some or completed high school Some or completed post-secondary education Some or completed graduate school Ethnicity 18.5% White Indigenous Black/AfroCaribbean/African Asian Biracial/Multiracial Other Principal Diagnosis 84.4% 0.7% 0.0% 88.9% 2.2% 0.0% 84.9% 1.4% 1.4% 3.0% 3.7% 0.7% 2.2% 2.2% 0.0% 0.0% 0.0% 1.4% Generalized Anxiety Disorder Social Anxiety Disorder Posttraumatic Stress Disorder Panic Disorder/ Agoraphobia Other (e.g., anxiety and related disorders, mood disorders, personality disorders) Additional Diagnosis Major Depressive Disorder Persistent Depressive Disorder Generalized Anxiety Disorder Social Anxiety Disorder Panic Disorder/ Agoraphobia Cannabis Use Disorder Other (e.g., anxiety and related disorders, mood disorders, personality disorders) 28.9% n = 39 17.8% n = 24 13.3% n = 18 8.9% n = 12 8.9% n = 12 8.9% 23.3% 65.9% 73.3% 65.8% 8.9% 13.3% 6.9% Non-Use (n = 135) Comparisons 20.0% n = 9 6.7% n = 3 4.4% n = 2 17.8% n = 13 21.9% n = 16 16.4% n = 12 4.1% n = 3 12.3% n =9 24.4% 17.8% 28.77% 8.15% 11.1% 23.29% 19.26% 15.6% 20.55% 18.52% 17.8% 20.55% 13.3% 6.7% 20.55% 0.0% 4.44% 10.96% 29.6% 40.0% 52.1% Frequent Use (n = 73) Number of additional diagnoses H(2) = 4.94 p = .085, ε2 = .020 Mean (SD) Baseline CUDIT-R scores Mean (SD) χ2(4) = 2.18, 2.01 (1.04) Range p = .70, V = .07 2.04 (1.20) 2.52 (1.64) 3.71 (2.96) 11.03 (5.69) 3 to 27 1 to 12 Comparisons H(2) = 1.89, p = .388, ε2 = .013 Note. Principal diagnosis = A mental health condition that is the patient’s most pressing concern; Additional diagnosis = Mental health conditions secondary to the principal diagnosis; Diagnostic data for principal diagnoses were available for 74% (n = 188) of individuals. χ2(2) = .76, p = .68, V = .06 Table 2 Baseline means (SD) for symptom-specific measures matching participants’ CBT group. χ2(4) = 4.70, p = .32, V = .10 OCI-R PCL-5 PDSS PSWQ SPIN 30.00 (8.63) 55.47 (10.81) 15.30 (4.37) 67.54 (8.42) 46.27 (8.45) sample of individuals who use cannabis only (b = − 0.09, SE = 0.00, t = 0.15, df = 115, p = .879, d = 0.02). Cannabis-related problems did not appear to have a significant effect on the trajectory of change in anxiety and related disorder symptom severity throughout CBT. χ2(10) = 8.73, 22.2% n = 10 13.3% n = 6 Infrequent Use (n = 45) p = .56, V = .14 3.3. Changes in illness intrusiveness across frequency of cannabis use groups Complete pre- and post-treatment data for the IIRS were only available for 126 participants (see Table 5). We assessed whether the IIRS total score improved significantly from pre-to post-treatment across the non-use, infrequent use, and frequent use groups. There was a sig­ nificant main effect of Time [F(1,123) = 27.20, p < .001, η2p = .18], but the main effect of Group [F(2,123) = 0.72, p = .488, η2p = .01] and the Group X Time interaction [F(2,123) = 2.00, p = .140, η2p = .03] were non-significant. These results indicate that changes in anxiety-related illness intrusiveness from pre-to post-treatment were unrelated to cannabis use frequency. Differences in IIRS at pre- [F(2,250) = 1.61, p = .201, η2 = 0.01] and post-treatment F(2,123) = 1.72, p = .183, η2 = 0.03] were non-significant. χ2(8) = 7.78, p = .456, V = .144 4. Discussion This study adds to the sparse literature examining cannabis use’s impact on CBT outcomes for anxiety and related disorders. Consistent with our first hypothesis, frequent cannabis use (2–3 times per week or more) was associated with less anxiety and related disorder symptom reduction from pre-to post-CBT compared to non-use. This is inconsis­ tent with results using brief CBT where cannabis use did not impact outcomes (Bricker et al., 2007; Ruglass et al., 2017), however, the cur­ rent study used a standard 12-session CBT protocol for anxiety and related disorders and did not exclude severe cannabis use presentations, which may partially explain the contrasting findings. On the other hand, this finding is consistent with research suggesting that cannabis use moderates treatment outcomes. Buckner et al. (2021) compared MET-CBT and integrated cannabis and anxiety reduction treatment (ICART). They found that ICART led to better outcomes than MET-CBT for those who used more baseline cannabis use while MET-CBT led to better outcomes than ICART for those with low levels of baseline cannabis use (Buckner et al., 2021). Although our study and Buckner et al.‘s study differed in type of treatment offered, both suggest that 693 Downloaded for Anonymous User (n/a) at Pontifical Catholic University of Chile from ClinicalKey.com by Elsevier on February 21, 2023. For personal use only. No other uses without permission. Copyright ©2023. Elsevier Inc. All rights reserved. M.J. Ouellette et al. Journal of Psychiatric Research 156 (2022) 690–697 Fig. 1. Participant CBT group allocation, completion, and early termination. impact on treatment outcomes. This is consistent with research on combined CBT and pharmacotherapy for anxiety and depressive symp­ toms where low cannabis use frequency did not impact outcomes (Bricker et al., 2007). Inconsistent with our hypothesis, cannabis-related problem severity was not associated with dampened CBT outcomes for anxiety and related disorders, adding to the nuances of investigating the potential impact of cannabis use and misuse within CBT. It is possible that our sample did not present with a broad enough severity range to see meaningful relationships between cannabis-related problems and CBT outcomes, as most participants did not have a CUD diagnosis and the mean CUDIT-R score for the frequent use group was below the CUDIT-R total cut off score (Adamson et al., 2010). Higher CUD rates might reveal a relationship between cannabis-related problem severity and CBT outcomes, however the current study’s CUD rates are representative of a naturalistic sample of individuals seeking anxiety treatment. It may be that cannabis-related problems are less important than cannabis use frequency in affecting CBT outcomes in this population. There are multiple ways that frequent cannabis use might interfere with CBT outcomes for anxiety and related disorders. For example, negative cognitive impacts of cannabis use (e.g., memory, attention; Broyd et al., 2016) or associated amotivation (e.g., Meier and White, 2018) may make it more difficult for participants to engage in CBT, and thus affect outcomes. In fact, some research suggests that there are biological changes involved in the cognitive and amotivation effects of Table 3 Results of hierarchical linear modelling assessing the effect of cannabis use status (non-use, infrequent use and frequent use) and cannabis-related problem severity (CUDIT-R) on trajectory of change in symptom severity (z-score) over the course of treatment. Full Sample z-score Effect df p d Initial z-score (Intercept) 1.47 0.09 15.83 Infrequent Use − 0.03 0.19 − 0.14 Frequent Use 0.24 0.16 1.49 z-score Over Time (Slope) − 0.13 0.01 − 14.74 Infrequent Use 0.02 0.02 1.31 Frequent Use 0.04 0.02 2.68 CUDIT-R in Individuals Who Use Cannabis Only (n = 118) b SE t 250 250 250 250 250 250 <.001 .886 .137 <.001 .190 .008 − 0.01 0.09 − 0.93 0.08 0.17 Effect b SE t df p d Initial z-score (Intercept) CUDIT-R z-score Over Time (Slope) CUDIT-R 1.60 0.02 − 0.09 0.00 0.10 0.02 0.01 0.00 16.15 1.43 − 10.86 .15 116 116 116 116 <.001 .157 <.001 .879 0.13 − 1.00 0.01 cannabis use may be associated with poorer outcomes with certain treatments. Additionally, the present findings indicate that cannabis use frequency appears to impact treatment outcomes, as unlike frequent cannabis use, infrequent cannabis use was not found to have a negative Fig. 2. Change in symptom severity (z-score) across levels of cannabis use (non-use, infrequent use, and frequent use). Note. Individuals who used frequently experienced a statistically significant slower reduction in anxiety symptoms throughout CBT compared to the non-use group. The unit of time is coded as one week, and treatment occurs over the course of 12 weeks, adding pre- and post-treatment for a total of 14 time points. See data analysis section for detail on how z-scores were calculated for each diagnostic measure. 694 Downloaded for Anonymous User (n/a) at Pontifical Catholic University of Chile from ClinicalKey.com by Elsevier on February 21, 2023. For personal use only. No other uses without permission. Copyright ©2023. Elsevier Inc. All rights reserved. M.J. Ouellette et al. Journal of Psychiatric Research 156 (2022) 690–697 Table 4 Mean z scores throughout CBT with ANOVA and Tuckey HSD comparisons between cannabis use groups. Week Mean Z score Non-use Infrequent use Frequent use F df p η2 Tuckey HSD Comparisons PreCBT 1 2 3 4 5 6 1.72 1.72 1.9 .96 2, 250 ns .008 1.21 1.26 1.63 2.07 2, 156 ns .026 1.18 1.00 1.30 .79 2, 195 ns .008 .99 1.10 1.32 1.47 2, 198 ns .015 .97 .95 1.35 2.00 2, 196 ns .020 .75 .87 1.35 3.89 2, 182 .022 .041 Frequent use > Non-use 7 8 9 10 11 12 PostCBT .65 .64 1.22 3.67 2, 184 .41 .66 1.30 7.08 2, 171 .26 .38 .87 3.24 2, 163 .23 .13 1.00 5.17 2, 153 .001 .076 Frequent use > Nonuse .042 .038 Frequent use > Nonuse .007 .063 Frequent use > Non-use & Infrequent use .11 − .29 .55 2.67 2, 135 ns .038 − .04 − .15 1.11 7.65 2, 96 .027 .038 Frequent use > Nonuse .14 .30 .69 2.10 2, 148 ns .028 .53 .39 .77 .82 2, 125 ns .013 outcomes, however this is an important area of future research. The current sample was predominantly White and cis-gender and therefore the results may not generalize to diverse groups who report differences in motives and cannabis use patterns (Buckner et al., 2016; Wu et al., 2016). This is an area for future research. Finally, the current study relied on self-report measures which are subjective and thus, may lead to biased reporting. The current results are preliminary and require replication with consideration for the limitations. With this in mind, our findings suggest that cannabis use is not necessarily detrimental to CBT outcomes given that all groups, including the frequent use group, experienced significant improvement in anxiety and related disorder symptoms from pre-to post-treatment. However, it may be worth screening for cannabis use frequency in patients seeking CBT for anxiety and related disorders. Clinicians may recommend that individuals who use cannabis frequently attempt to reduce their use prior to CBT to maximize outcomes. It may also be helpful for clinicians to closely monitor the timing of use for individuals who use cannabis frequently throughout CBT and help pa­ tients experiment with small shifts in when and how they use rather than how much they use. For example, avoiding cannabis use right before a therapy session may increase the patient’s ability to focus and retain information learned in CBT. However, the current results suggest that frequent cannabis use should not warrant unilateral exclusion from CBT for anxiety and related disorders as patients generally benefit from CBT despite their cannabis use. In fact, successful CBT may have helpful downstream effects on cannabis use for those who use as a form of avoidance. In summary, this study is one of the first to examine the relationship between cannabis use and CBT outcomes for anxiety and related disor­ ders. Results indicated that individuals who use cannabis frequently experienced significant symptom improvement, but dampened CBT outcomes compared to non-use. Future research should attempt to replicate the findings and continue to consider the most impactful ways of measuring and understanding cannabis use and disuse. Table 5 Means and standard deviations of IIRS from pre-to post-treatment across groups. Variable IIRS Total Score Non-Use Infrequent Use Frequent Use IIRS Total Score Non/Infrequent Use Use N 98 28 Pre-Treatment Post-Treatment Mean SD Mean SD 57.30 56.71 57.25 15.35 12.56 11.82 48.99 45.29 53.82 16.83 15.18 17.75 57.15 57.25 14.66 11.81 48.08 53.82 16.45 17.75 <.001 .137 Frequent use > Non-use & Infrequent use Note. IIRS = Illness Intrusiveness Rating Scale. cannabis, such as reduced dopamine associated with heavy cannabis use (Ferland and Hurd, 2020). If participants who use cannabis frequently are experiencing these negative effects of cannabis use, they may struggle to learn or practice the CBT skills more than individuals who use cannabis infrequently or do not use. Engaging in homework (i.e., practicing CBT skills outside of the therapy context) enhances CBT outcomes (Kazantzis et al., 2010) and therefore if individuals who use cannabis frequently struggle to engage in homework, it is plausible that they would experience dampened outcomes. Research is needed to specifically investigate these hypotheses. High cannabis use frequency may also serve as a subtle avoidance strategy, which may be harder to target in CBT protocols where overt avoidance is a core treatment target. Future studies should measure cannabis use throughout treatment to investigate the temporal relationship between fluctuations in cannabis use and symptom change in CBT. There are several limitations to consider when interpreting the cur­ rent results. First, there is no standardized method of categorizing cannabis use patterns. Differing cannabis use definitions across studies complicates comparisons of results between them. The current study used cannabis use frequency and cannabis-related problem severity to attempt to gain a more specific understanding of the impact of cannabis use on treatment outcomes. Ideally, the field would standardize frequent vs. infrequent use and studies would further capture various factors involved in cannabis use (e.g., product, amount consumed) to identify variables that contribute most of the variance in CBT outcomes, and which are negligible. Given the lack of comprehensive cannabis use measures, future studies should attempt to develop improved cannabis use measures to examine the effects of these variables on treatment outcomes. Additionally, the impact of cannabis on CBT outcomes was not compared between diagnostic groups due to small sub-sample sizes. Given differing reported frequencies of use across anxiety disorder groups in the current study (e.g., higher use in SAD), the impact of use on CBT outcomes may be more or less prominent with different pre­ senting concerns. Further, there were too few individuals with likely CUD as per the CUDIT-R or diagnosed CUD to examine the effect on CBT Role of funding source The study has received funding from the Michael G. DeGroote Centre for Medicinal Cannabis Research but the sponsors had no other role in the study. Grant reference: McCabe, R.E., Rowa, K., Pawluk, E., Phung, N., & Soreni, N. Cannabis Use and Anxiety Disorders. Seed grant received October 2018 from the Michael G. DeGroote Centre for Medicinal Cannabis Research. CRediT authorship contribution statement Mélise J. Ouellette: Conceptualization, Methodology, Formal analysis, Writing – original draft, Writing – review & editing. Karen 695 Downloaded for Anonymous User (n/a) at Pontifical Catholic University of Chile from ClinicalKey.com by Elsevier on February 21, 2023. For personal use only. No other uses without permission. Copyright ©2023. Elsevier Inc. All rights reserved. M.J. Ouellette et al. Journal of Psychiatric Research 156 (2022) 690–697 Rowa: Conceptualization, Methodology, Supervision, Writing – review & editing. Duncan H. Cameron: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing. Ashleigh Elcock: Data curation. Noam Soreni: Conceptualization, Writing – review & editing. Elizabeth J. Pawluk: Conceptualization, Methodology, Writing – review & editing. Randi E. McCabe: Conceptualization, Methodology, Supervision, Writing – review & editing, Resources. Ferland, J.N., Hurd, Y.L., 2020. Deconstructing the neurobiology of cannabis use disorder. Nat. Neurosci. 23, 600–610. https://doi.org/10.1038/s41593-020-0611-0. Foa, E.B., Huppert, J.D., Leiberg, S., Langner, R., Kichic, R., Hajcak, G., Salkovskis, P.M., 2002. The Obsessive-Compulsive Inventory: development and validation of a short version. Psychol. Assess. 14 (4), 485–496. https://doi.org/10.1037/10403590.14.4.485. Fresco, D.M., Mennin, D.S., Heimberg, R.G., Turk, C.L., 2003. Using the Penn State Worry Questionnaire to identify individuals with generalized anxiety disorder: a receiver operating characteristic analysis. J. Behav. Ther. Exp. Psychiatr. 34 (3), 283–291. https://doi.org/10.1016/j.jbtep.2003.09.001. Furukawa, T.A., Shear, M.K., Barlow, D.H., Gorman, J.M., Woods, S.W., Money, R., Etschel, E., Engel, R.R., Leucht, S., 2009. Evidence-based guidelines for interpretation of the panic disorder severity scale. Depress. Anxiety 26 (10), 922–929. https://doi.org/10.1002/da.20532. Henry, E.A., Kaye, J.T., Bryan, A.D., Hutchison, K.E., Ito, T.A., 2014. Cannabis cue reactivity and craving among never, infrequent and heavy cannabis users. Neuropsychopharmacology 39 (5), 1214–1221. https://doi.org/10.1038/ npp.2013.324. Jacobson, N.S., Roberts, L.J., Berns, S.B., McGlinchey, J.B., 1999. Methods for defining and determining the clinical significance of treatment effects: description, application, and alternatives. J. Consult. Clin. Psychol. 67 (3), 300–307. https://doi. org/10.1037/0022-006X.67.3.300. Kazantzis, N., Whittington, C., Dattilio, F., 2010. Meta-analysis of homework effects in cognitive and behavioral therapy: a replication and extension. Clin. Psychol. Sci. Pract. 17 (2), 144–156. https://doi.org/10.1111/j.1468-2850.2010.01204.x. Kessler, R.C., Petukhova, M., Sampson, N.A., Zaslavsky, A.M., Wittchen, H.-U., 2012. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int. J. Methods Psychiatr. Res. 21 (3), 169–184. https://doi.org/10.1002/mpr.1359. McCabe, R.E., Milosevic, I., Rowa, K., Shnaider, P., Key, B., Antony, M.M., 2017. Diagnostic Assessment Research Tool (DART). St. Joseph’s Healthcare/McMaster University, Hamilton, ON. McManus, F., Sacadura, C., Clark, D.M., 2008. Why social anxiety persists: an experimental investigation of the role of safety behaviours as a maintaining factor. J. Behav. Ther. Exp. Psychiatr. 39 (2), 147–161. https://doi.org/10.1016/j. jbtep.2006.12.002. Meier, M.H., White, M., 2018. Do young-adult cannabis users show amotivation? An analysis of informant reports. Translat. Issue. Psychol. Sci. 4 (1), 99–107. https:// doi.org/10.1037/tps0000150. Meyer, T.J., Miller, M.L., Metzger, R.L., Borkovec, T.D., 1990. Development and validation of the penn state worry questionnaire. Behav. Res. Ther. 28 (6), 487–495. https://doi.org/10.1016/0005-7967(90)90135-6. Milosevic, I., Cameron, D.H., Milanovic, M., McCabe, R.E., Rowa, K., 2022. Face-to-face versus video teleconference group cognitive behavioural therapy for anxiety and related disorders: a preliminary comparison. Can. J. Psychiatr. 67 (5), 391–402. https://doi.org/10.1177/07067437211027319. Moscovitch, D.A., Gavric, D.L., Merrifield, C., Bielak, T., Moscovitch, M., 2011. Retrieval properties of negative vs. positive mental images and autobiographical memories in social anxiety: outcomes with a new measure. Behav. Res. Ther. 49 (8), 505–517. https://doi.org/10.1016/j.brat.2011.05.009. Moser, J.S., Hajcak, G., Foa, E.B., Simons, R.F., 2008. Interpretation bias in social anxiety as detected by event-related brain potentials. Emotion 8 (5), 693–700. https://doi. org/10.1037/a0013173. Otte, C., 2011. Cognitive behavioral therapy in anxiety disorders: current state of the evidence. Dialogues Clin. Neurosci. 13 (4), 413–421. https://doi.org/10.31887/ DCNS.2011.13.4/cotte. Ouellette, M.J., Puccinelli, C., Rowa, K., Elcock, A., McCabe, R.E., 2019. Cannabis use in patients seeking therapy for anxiety and related disorders: a descriptive study. Can. J. Addict. 10 (3), 30–37. https://doi.org/10.1097/CXA.0000000000000060. Raudenbush, S.W., Bryk, A.S., 2002. Hierarchical Linear Models: Applications and Data Analysis Methods, second ed. Sage Publications Inc, Thousand Oaks, CA. Resick, P.A., Monson, C.M., Chard, K.M., 2016. Cognitive Processing Therapy for PTSD: A Comprehensive Manual. Guilford Publications. Riccardi, C.J., Korte, K.J., Schmidt, N.B., 2017. False Safety Behavior Elimination Therapy: a randomized study of a brief individual transdiagnostic treatment for anxiety disorders. J. Anxiety Disord. 46, 35–45. https://doi.org/10.1016/j. janxdis.2016.06.003. Rowa, K., Chudzik, S., LeMoult, J., Aiken, A., Pawluk, E., 2019. Cognitive Behavioural Therapy Manual for Anxiety. Unpublished manual. Ruglass, L.M., Shevorykin, A., Radoncic, V., Smith, K.M.Z., Smith, P.H., Galatzer-Levy, I. R., Papini, S., Hien, D.A., 2017. Impact of cannabis use on treatment outcomes among adults receiving cognitive-behavioral treatment for PTSD and substance use disorders. J. Clin. Med. 6 (2), 1–15. https://doi.org/10.3390/jcm6020014. Salkovskis, P.M., Clark, D.M., Hackmann, A., Wells, A., Gelder, M.G., 1999. An experimental investigation of the role of safety-seeking behaviours in the maintenance of panic disorder with agoraphobia. Behav. Res. Ther. 37 (6), 559–574. https://doi.org/10.1016/S0005-7967(98)00153-3. Schneider, L.H., Pawluk, E.J., Milosevic, I., Shnaider, P., Rowa, K., Antony, M.M., Musielak, N., McCabe, R.E., 2021. The Diagnostic Assessment Research Tool in action: a preliminary evaluation of a semistructured diagnostic interview for DSM-5 disorders. Psychol. Assess. 34 (1), 21–29. https://doi.org/10.1037/pas0001059. Shear, M.K., Brown, T.A., Barlow, D.H., Money, R., Sholomskas, D.E., Woods, S.W., Gorman, J.M., Papp, L.A., 1997. Multicenter collaborative panic disorder severity scale. Am. J. Psychiatr. 154 (11), 1571–1575. https://doi.org/10.1176/ ajp.154.11.1571. Declaration of competing interest No conflicts of interests to declare. References Adamson, S.J., Kay-Lambkin, F.J., Baker, A.L., Lewin, T.J., Thornton, L., Kelly, B.J., Sellman, J.D., 2010. An improved brief measure of cannabis misuse: the Cannabis Use Disorders Identification Test-Revised (CUDIT-R). Drug Alcohol Depend. 110 (1), 137–143. https://doi.org/10.1016/j.drugalcdep.2010.02.017. Aderka, I.M., McLean, C.P., Huppert, J.D., Davidson, J.R.T., Foa, E.B., 2013. Fear, avoidance and physiological symptoms during cognitive-behavioral therapy for social anxiety disorder. Behav. Res. Ther. 51 (7), 352–358. https://doi.org/10.1016/ j.brat.2013.03.007. American Psychiatric Association, 2013. Diagnostic and Statistical Manual of Mental Disorders, fifth ed. Author, Washington, DC. Beck, A.T., 1993. Cognitive therapy: past, present, and future. J. Consult. Clin. Psychol. 61 (2), 194–198. Bovin, M.J., Marx, B.P., Weathers, F.W., Gallagher, M.W., Rodriguez, P., Schnurr, P.P., Keane, T.M., 2016. Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders–fifth edition (PCL-5) in veterans. Psychol. Assess. 28 (11), 1379–1391. https://doi.org/10.1037/pas0000254. Brady, K.T., Haynes, L.F., Hartwell, K.J., Killeen, T.K., 2013. Substance use disorders and anxiety: a treatment challenge for social workers. Soc. Work. Publ. Health 28 (3–4), 407–423. https://doi.org/10.1080/19371918.2013.774675. Bricker, J.B., Russo, J., Stein, M.B., Sherbourne, C., Craske, M., Schraufnagel, T.J., RoyByrne, P., 2007. Does occasional cannabis use impact anxiety and depression treatment outcomes?: results from a randomized effectiveness trial. Depress. Anxiety 24 (6), 392–398. https://doi.org/10.1002/da.20248. Broyd, S.J., van Hell, H.H., Beale, C., Yücel, M., Solowij, N., 2016. Acute and chronic effects of cannabinoids on human cognition—a systematic review. Biol. Psychiatr. 79 (7), 557–567. https://doi.org/10.1016/j.biopsych.2015.12.002. Buckner, J.D., Carroll, K.M., 2010. Effect of anxiety on treatment presentation and outcome: results from the marijuana treatment project. Psychiatr. Res. 178 (3), 493–500. https://doi.org/10.1016/j.psychres.2009.10.010. Buckner, J.D., Schmidt, N.B., 2008. Marijuana effect expectancies: relations to social anxiety and marijuana use problems. Addict. Behav. 33 (11), 1477–1483. https:// doi.org/10.1016/j.addbeh.2008.06.017. Buckner, J.D., Crosby, R.D., Wonderlich, S.A., Schmidt, N.B., 2012. Social anxiety and cannabis use: an analysis from ecological momentary assessment. J. Anxiety Disord. 26 (2), 297–304. https://doi.org/10.1016/j.janxdis.2011.12.006. Buckner, J.D., Zvolensky, M.J., Farris, S.G., Hogan, J., 2014. Social anxiety and coping motives for cannabis use: the impact of experiential avoidance. Psychol. Addict. Behav.: J. Soc. Psychol. Addict. Behav. 28 (2), 568–574. https://doi.org/10.1037/ a0034545. Buckner, J.D., Shah, S.M., Dean, K.E., Zvolensky, M.J., 2016. Cannabis use frequency and use-related impairment among African-American and White users: the impact of cannabis use motives. Ethn. Health 21 (3), 318–331. https://doi.org/10.1080/ 13557858.2015.1065311. Buckner, J.D., Zvolensky, M.J., Ecker, A.H., Schmidt, N.B., Lewis, E.M., Paulus, D.J., Lopez-Gamundi, P., Crapanzano, K.A., Bakhshaie, J., 2019. Integrated cognitive behavioral therapy for comorbid cannabis use and anxiety disorders: a pilot randomized controlled trial. Behav. Res. Ther. 115, 38–45. https://doi.org/10.1016/ j.brat.2018.10.014. Buckner, J.D., Morris, P.E., Zvolensky, M.J., 2021. Integrated cognitive-behavioral therapy for comorbid cannabis use and anxiety disorders: the impact of severity of cannabis use. Exp. Clin. Psychopharmacol 29 (3), 272–278 https://doi.org.libaccess. lib.mcmaster.ca/10.1037/pha0000456. Cohen, J., 2013. Statistical Power Analysis for the Behavioral Sciences. Academic Press. Connor, K.M., Davidson, J.R.T., Churchill, L.E., Sherwood, A., Weisler, R.H., Foa, E., 2000. Psychometric properties of the social Phobia inventory (SPIN): new self-rating scale. Br. J. Psychiatry 176 (4), 379–386. https://doi.org/10.1192/bjp.176.4.379. Cornelius, J.R., Chung, T., Martin, C., Wood, D.S., Clark, D.B., 2008. Cannabis withdrawal is common among treatment-seeking adolescents with cannabis dependence and major depression, and is associated with rapid relapse to dependence. Addict. Behav. 33 (11), 1500–1505. https://doi.org/10.1016/j. addbeh.2008.02.001. Devins, G.M., 2010. Using the Illness Intrusiveness Ratings Scale to understand healthrelated quality of life in chronic disease. J. Psychosom. Res. 68 (6), 591–602. https://doi.org/10.1016/j.jpsychores.2009.05.006. Devins, G.M., Binik, Y.M., Hutchinson, T.A., Hollomby, D.J., Barre, P.E., Guttmann, R.D., 1983. The emotional impact of end-stage renal disease: importance of patients perceptions of illness and control. Int. J. Psychiatr. Med. 13, 327–343. https://doi. org/10.2190/5DCP-25BV-U1G9-9G7C. 696 Downloaded for Anonymous User (n/a) at Pontifical Catholic University of Chile from ClinicalKey.com by Elsevier on February 21, 2023. For personal use only. No other uses without permission. Copyright ©2023. Elsevier Inc. All rights reserved. M.J. Ouellette et al. Journal of Psychiatric Research 156 (2022) 690–697 Shear, M.K., Rucci, P., Williams, J., Frank, E., Grochocinski, V., Vander Bilt, J., Houck, P., Wang, T., 2001. Reliability and validity of the panic disorder severity scale: replication and extension. J. Psychiatr. Res. 35 (5), 293–296. https://doi.org/ 10.1016/S0022-3956(01)00028-0. Simons, J., Correia, C.J., Carey, K.B., Borsari, B.E., 1998. Validating a five-factor marijuana motives measure: relations with use, problems, and alcohol motives. J. Counsel. Psychol. 45 (3), 265–273. https://doi.org/10.1037/0022-0167.45.3.265. Skalisky, J., Wielgus, M.D., Aldrich, J.T., Mezulis, A.H., 2019. Motives for and impairment associated with alcohol and marijuana use among college students. Addict. Behav. 88, 137–143. https://doi.org/10.1016/j.addbeh.2018.08.028. Skinner, W., O’Grady, C., Bartha, C., Parker, C., 2004. Concurrent Substance Use and Mental Health Disorders. Centre for Addiction and Mental Health, Toronto. Stewart, S.H., Conrod, P.J. (Eds.), 2008. Anxiety and Substance Use Disorders: the Vicious Cycle of Comorbidity. Springer. Stöber, J., Bittencourt, J., 1998. Weekly assessment of worry: an adaptation of the Penn State Worry Questionnaire for monitoring changes during treatment. Behav. Res. Ther. 36 (6), 645–656. https://doi.org/10.1016/S0005-7967(98)00031-X. Weathers, F.W., Litz, B.T., Keane, T.M., Palmieri, P.A., Marx, B.P., Schnurr, P.P., 2013. The PTSD Checklist for DSM-5 (PCL-5) 10 (4), 206. Scale available from: the National Center for PTSD at. www.ptsd.va.gov. Wu, L.-T., Zhu, H., Swartz, M.S., 2016. Trends in cannabis use disorders among racial/ ethnic population groups in the United States. Drug Alcohol Depend. 165, 181–190. https://doi.org/10.1016/j.drugalcdep.2016.06.002. 697 Downloaded for Anonymous User (n/a) at Pontifical Catholic University of Chile from ClinicalKey.com by Elsevier on February 21, 2023. For personal use only. No other uses without permission. Copyright ©2023. Elsevier Inc. All rights reserved.