Obstetrics Study Guide: Teratogens, Fetal Assessment, Preeclampsia
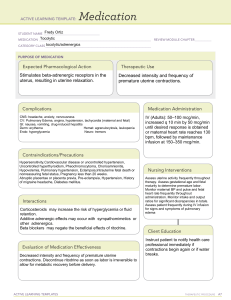
advertisement
Chapter 3: Teratogens A. Teratogens are drugs, viruses, infections or other exposures that have the potential to cause embryonic/fetal developmental abnormality B. Fetus is most vulnerable to effects of teratogens during organogenesis (first 8 weeks gestation), exposure during this time will cause structural defects C. Exposure after 13 weeks gestation may cause fetal growth restriction or reduced organ size D. Medications a. ACE inhibitors (end in -pril) b. Carbamazepines (anticonvulsant) c. Cocaine d. Warfarin (coumadin); heparin is the anticoagulant of choice safe for pregnancy E. Infections/viruses (TORCH) a. Toxoplasmosis (avoid cleaning litter box and eating rare beef or lamb) b. Other (Syphilis, varicella zoster, parvovirus, and listeria) c. Rubella d. Cytomegalovirus e. Herpes varicella Chapter 3: FDA 5 Categories of Safety A. In 1979, the FDA established five letter risk categories - A, B, C, D or X - to indicate the potential of a drug to cause birth defects if used during pregnancy. The categories were determined by assessing the reliability of documentation and the risk to benefit ratio. B. A (least risk) to X (most risk) Chapter 6: BPP A. Screening test done to determine fetal well-being, done via U/S and FHR reactivity B. The fetus responds to central hypoxia by alterations in movement, muscle tone, breathing, and heart rate patterns C. Each BPP category is assigned a score of 2, 1 or 0 D. Categories a. Fetal breathing movement b. Fetal movement of body/limbs c. Fetal tone (extension/flexion) d. Amniotic fluid volume e. NST (reactive) E. Results a. 8-10, normal b. 6, should be reassessed in 6 hrs c. <4, delivery should occur without delay Chapter 6: NST A. Uses fetal monitoring to assess fetal well being by using ultrasound for the fetal heart rate and a toco on the fundus of the uterus B. The NST is based on the premise that a normal fetus moves at various intervals and that the CNS and myocardium respond to this movement C. Accelerations in FHR should be visible on the strip D. Results a. Reactive, accelerations of the FHR with fetal movement felt by the mother ensures adequate oxygenation and an intact CNS b. Non-reactive, no accelerations of FHR; additional testing required i. May need vibro acoustic stimulation Chapter 7: Preeclampsia A. Hypertension accompanied by proteinuria after the 20th week gestation B. Decreased placental perfusion and placental hypoxia C. Multisystem hypertensive disease a. Blood pressure ≥ 160/110 b. Visual problems c. Pulmonary edema d. Epigastric pain e. Low platelet f. Proteinuria g. Elevated AST/ALT D. HELLP a. Serious compilation of preeclampsia b. Hemolysis c. Elevated liver enzymes d. Low platelets <100,000 E. Clonus assessment a. Clonus response is often a precursor to seizure activity and warrants immediate provider notification b. Rhythmic oscillations between dorsiflexion and plantar flexion=clonus F. Medical management of preeclampsia a. Control blood pressure, prevent seizure activity, and prevent cerebral hemorrhage b. Antihypertensive drugs and intravenous magnesium sulfate to prevent seizures c. MgSO4 i. Loading dose is 4-6g administered over 15-20 minutes ii. Continuous infusion 2g/hr iii. Dosage is titrated to maintain therapeutic level (4-8 mg/dL) iv. Infusion should continue 24 hrs after delivery v. Measure serum magnesium Q4-6hr (normal 1.5-2) vi. Antidote is calcium gluconate Chapter 7: Induction/Tocolytic medications A. Indications of induction a. Must be at least 39 weeks gestation b. Medically indicated when the condition or safety of woman or fetus will be improved by birth B. Oxytocin a. Establish uterine contraction patterns that promote dilation of about 1 cm/hr once in active labor C. Cervidil and misoprostol a. Cervical ripening agents if not quite ready for oxytocin induction D. Mechanical a. Dilators placed in the cervix promote cervical ripening by stimulating release of prostaglandins b. Typically done by using an inflated foley catheter balloon Chapter 7: Gestational diabetes A. Carbohydrate intolerance leading to hyperglycemia first discovered in pregnancy B. Blood glucose self-monitoring, diet, and exercise are the interventions used to manage GDM C. If treated by diet and exercise (A1); if oral medications or insulin is needed (A2) D. All pregnant women are screened for GDM between 24-28 weeks with a glucola screening; if this is failed they must return for a oral glucose tolerance test Chapter 7: Hyperemesis gravidarum A. Severe nausea and vomiting usually during the first trimester of pregnancy that can lead to dehydration B. Women with HG are at risk for fluid and electrolyte imbalances, weight loss, and IUGR C. Management for mild cases a. Rest b. Avoid triggers c. Small frequent meals d. Crackers/high protein snack D. Medications a. Ginger capsules b. Pyridoxine c. Promethazine d. Metoclopramide Chapter 7: Placenta abruption/Placenta Previa A. Placenta previa a. Occurs when the placenta attaches to the lower uterine segment or near or over the cervical os instead of the fundus b. Vaginal exam is contraindicated c. Signs and symptoms i. Painless bright-red bleeding ii. Soft and relaxed uterus iii. Hemorrhage, shock and uterine rupture can occur and result in maternal and fetal mortality/morbidity iv. Usually and indicated cesarean delivery v. Potential emergency hysterectomy is bleeding does not stop after delivery B. Placental abruption a. Occurs with premature separation of the normally implanted placenta after 20 weeks gestation b. Results in hemorrhage, requires urgent action to prevent fetal loss and further hemorrhage c. Vaginal exam is contraindicated d. Signs and symptoms i. Bleeding associated with severe abdominal pain (location dependent) ii. Uterine tenderness with boardlike abdomen and no bleeding (location dependent) iii. Fetal compromise iv. Fetal demise Chapter 7: Chorio A. Most often associated with prolonged labor (membranes that have been ruptured for longer than 24hrs) B. Assess for signs of infection a. Maternal or fetal tachycardia b. Maternal fever >100.4 c. Uterine tenderness d. Malodorous fluid or discharge C. Treatment is IV ampicillin or erythromycin Chapter 7: Ectopic pregnancy A. Implantation of the fertilized egg in a site other than the lining of the uterus, most frequently the fallopian tubes B. Causes a. PID b. Previous tubal surgery c. Endometriosis d. IUD C. Signs and symptoms a. Rupture and bleeding into abdominal cavity b. Sharp one sided pain that may refer to the shoulder D. Diagnosis a. hCG level decreased b. U/S E. Treatment a. Surgery if >3.5cm b. Methotrexate if >3.5cm Chapter 8: Labor exams/definition of labor A. Labor a. Definition of labor is progressive dilation and effacement of the cervix b. Uterine contractions occur at regular intervals and increase with intensity as labor progresses c. 5 P’s of labor will ensure labor progression i. Powers; uterine contractions ii. Passage; pelvis shape iii. Passenger; fetal lie and presentation iv. Psyche; response of women v. Position; maternal positioning B. Labor exams a. Dilation i. Assessment of opening and enlargement of the cervix expressed in centimeters diameter on a scale of 1cm-10cm ii. Once the cervix is fully dilated it can no longer be palpated b. Effacement i. Assessment of shortening and thinning of the cervix expressed as a percentage (0%-100%) related to the length of the cervical canal c. Station i. Assessment of the position of the fetal head in relation to the pelvis expressed by a -5 to 5 with positive station being at the pelvic outlet Chapter 8: Epidural/Spinal A. Epidural a. Lumbar epidural is most commonly used method of analgesia during labor b. Injection of opioid into epidural space provides pain relief from uterine contractions while still maintaining alertness during labor and birth c. Disadvantages are maternal hypotension, spinal headache, loss of bladder control, and lower back pain i. An IV bolus may be given to correct hypotension d. Current CBC with platelets and informed consent e. RN can monitor but not manage epidural anesthesia B. Spinal a. Used for cesarean section delivery b. Single local anesthetic or combined with fentanyl inserted into the subarachnoid space c. At risk for maternal hypotension, decreased placental perfusion, and ineffective breathing Chapter 9: Early/Variable/Late decelerations A. Early decelerations a. Mirror the contraction, are usually tolerated by the fetus b. Cause is fetal head compression c. No treatment necessary unless bradycardia occurs B. Variable decelerations a. Variable in onset, frequency, duration, and intensity b. Cause is umbilical cord compression c. Consider an amnioinfusion, tocolytics, or delivery d. Nursing actions i. Notify provider ii. Oxygen via facemask 10L iii. Change position iv. Decrease/DC oxytocin v. Consider more invasive monitoring (FSE) vi. Modify pushing C. Late decelerations a. Begin around the peak of the contraction b. Cause is uteroplacental insufficiency c. Nursing actions i. Notify provider STAT ii. Oxygen via facemask 10L iii. IV bolus 500mL iv. Decrease/DC oxytocin v. Consider tocolytics/delivery Chapter 9: Amnioinfusion/IUPC A. Normal saline infused through an intrauterine pressure catheter to increase amniotic fluid and cushion the umbilical cord to reduce compressor B. Often used as an intervention for variable decelerations C. Usually a bolus, can also have a continuous infusion D. IUPC is able to measure strength of uterine contractions E. Careful monitoring and documentation of fluid intake and output is important to avoid overload Chapter 10: Hematoma/Shoulder dystocia/Vacuum/Forceps A. Hematoma a. Complication of vacuum and forcep deliveries b. Increased risk of cephalohematoma and neonatal jaundice from a vacuum delivery c. Increased risk of maternal perineal trauma and hematoma from forcep delivery B. Assisted deliveries a. Fetal head must be engaged and cervix must be dilated b. Often used in situations of maternal exhaustion, epidural anesthesia, fetal distress, or need to rotate the fetal head c. Cesarean birth should proceed if assistive delivery is not successful d. Vacuum i. Maximum of three attempts for a 15 minute period, nurse should document the beginning time and count each attempt ii. Note fetal hematoma risk e. Forceps i. Note maternal hematoma risk ii. May need cold perineal pad to soothe area C. Shoulder dystocia a. Unpredictable and unpreventable OB emergency b. Failure of the fetus to descend through the pelvic canal causing the anterior shoulder to become lodged and failure to deliver the rest of the body c. Often first suspected by the turtle sign; a crowning head will retreat back into the birth canal after a contraction d. Once the head is delivered it is important to mark the exact time; more than a 5minute delay in head to body interval may result in hypoxia e. McRobert’s manuver and supra pubic pressure are interventions done by the RN during a shoulder dystocia delivery i. McRobert’s; legs are brought back as far as the woman can tolerate to widen the pelvis ii. Supra pubic pressure; have a stool at the bedside and push the anterior shoulder downward to facilitate delivery Chapter 10: Umbilical Cord Prolapse A. Partial or total occlusion of the umbilical cord with fetal deterioration B. Obstetric emergency, stat initiation of measures to relieve cord compression is critical C. Nursing action a. Elevation of the presenting part off the umbilical cord, hands remain in vagina lifting the part off the cord until cesarean delivery D. Variable decelerations a. May be present on the FHR strip indicating umbilical cord compression Chapter 11: Post-op Cesarean A. Patient will be stabilized in the PACU after cesarean delivery B. PACU a. Stabilize vital signs, bleeding, and pain (1hr) b. One to one ratio c. Monitor I&O d. Discharge criteria met prior to transfer to the unit e. Initiate skin to skin once mother is stable C. Nursing care a. Facilitate bonding b. Monitor fundus and lochia c. Assess incision site/dressing d. TCDB/incentive spirometer e. SCD hose f. Pain control g. Advance diet slowly Chapter 12: OCPs contraindications/warning signs to report A. Initial exam for hormonal BC a. Through history is necessary to rule out contraindications b. Contraindications i. History of pulmonary embolism, deep vein thrombosis, stroke, or coronary artery disease ii. Uncontrolled hypertension iii. Estrogen dependent cancers B. Oral contraceptive pill a. 91% effective b. Lowest dose of estrogen possible, progestins have become safer with fewer side effect c. Only are effective when taken consistently d. Some contain folic acid to reduce risk of neural tube defects in the event of a pregnancy C. Side effects a. Teaching regarding expected side effects will increase compliance b. Scanty periods c. Breakthrough bleeding d. Nausea D. Life threatening side effects a. ACHES, if a women experiences any of these symptoms consult emergency care b. Abdominal pain c. Chest pain or shortness of breath d. Headaches that are sudden or persistent e. Eye problems f. Severe leg pain Chapter 12: Rhogam/Rubella/tDAP A. Rhogam a. Given to Rh-negative women at 28 weeks gestation prenatally b. Rh-negative women who give birth to an Rh-positive baby are screened for antiRh antibodies c. A second injection of Rho immune globulin is given postpartum if the baby is Rh positive d. Prevents production of anti-Rh antibodies e. Dose; 300 mcg IM B. Rubella a. Postpartum patients who are rubella-non-immune should be vaccinated before discharge b. MMR vaccine is usually given and protects against measles, mumps, and rubella C. tDAP a. Vaccine against tetanus, diphtheria, and pertussis b. First dose typically given in adolescence and then every 10 years Chapter 14: Uterine Atony/Postpartum hemorrhage/Oxytocin A. Uterine atony is is the most common cause of postpartum hemorrhage B. Postpartum hemorrhage is >500mL blood loss following a vaginal birth and >1000mL blood loss following a cesarean birth C. Immediately after delivery, initiate fundal massage and administer IV oxytocin to stimulate uterine contractions to decrease risk of postpartum hemorrhage D. Assess uterine tone, uterus should not be boggy or atony E. More than one saturated peripad per hour is indicative of PPH F. Oxytocin a. Is a high-alert medication that needs to be verified by another RN b. Rate and titration is determined by uterine contraction activity during labor and uterine tone and bleeding postpartum, must be on a pump c. Typically administered IV infusion Chapter 19: Mastectomy/Hysterectomy A. Mastectomy a. Surgical removal of one or both breasts, typically done as treatment for breast cancer b. Lymphededma is a complication of mastectomy surgery; lymph fluid is not able to circulate and accumulates in arm, hand, or breast i. Can lead to necrosis c. Post-op nursing care following mastectomy i. Monitor for lymphedema ii. Maintain JP drains iii. No BP, venipuncture, or injections in affected arm iv. Elevate affected arm on pillows B. Hysterectomy a. Pre-operative care i. Admission assessment and health history ii. Laboratory tests iii. EKG iv. NPO v. Consent vi. IV, antibiotics, foley b. Post-operative care i. IV medications for pain ii. Antibiotic therapy for infection risk iii. Slow progression of diet iv. Foley catheter 12-24 hrs post-surgery v. Ambulate early c. Nursing interventions i. Monitor for blood loss ii. Monitor VS iii. Incentive spiromete/TC&DB/splinting iv. Monitor LOC d. Teaching i. Keep incision dry ii. Nutritional information iii. Do not put anything in vagina until advised by surgeon iv. Notify the HCP of increased pain, drainage or bleeding, leg/calf pain, and fever >102.2 Chapter 19: IPV A. A screening test for intimate partner violence should be done at each prenatal visit B. If the partner is with the patient, wait until they are alone to assess for IPV C. Ask the patient whether they feel safe going home and whether they have been hurt physically, emotionally, or sexually by current or previous partner D. IPV is associated with poor outcomes for pregnancy E. Signs and symptoms a. Repeated non-specific complaints b. Overuse of the healthcare system c. Hesitancy, embarrassment, or evasiveness relating to history of injuries F. Documentation and reporting is essential when dealing with IPV