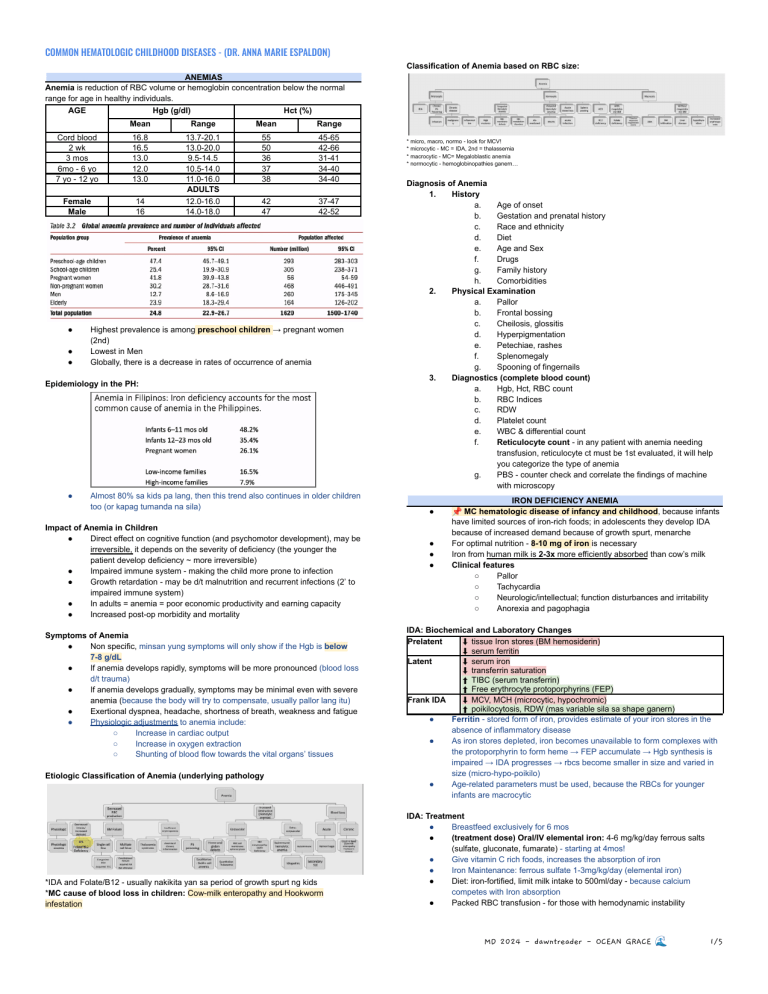
COMMON HEMATOLOGIC CHILDHOOD DISEASES - (DR. ANNA MARIE ESPALDON) Classification of Anemia based on RBC size: ANEMIAS Anemia is reduction of RBC volume or hemoglobin concentration below the normal range for age in healthy individuals. AGE Hgb (g/dl) Hct (%) Mean Range Mean Range Cord blood 2 wk 3 mos 6mo - 6 yo 7 yo - 12 yo 16.8 16.5 13.0 12.0 13.0 55 50 36 37 38 45-65 42-66 31-41 34-40 34-40 Female Male 14 16 13.7-20.1 13.0-20.0 9.5-14.5 10.5-14.0 11.0-16.0 ADULTS 12.0-16.0 14.0-18.0 42 47 37-47 42-52 ● ● ● Highest prevalence is among preschool children → pregnant women (2nd) Lowest in Men Globally, there is a decrease in rates of occurrence of anemia Epidemiology in the PH: ● Almost 80% sa kids pa lang, then this trend also continues in older children too (or kapag tumanda na sila) Impact of Anemia in Children ● Direct effect on cognitive function (and psychomotor development), may be irreversible, it depends on the severity of deficiency (the younger the patient develop deficiency ~ more irreversible) ● Impaired immune system - making the child more prone to infection ● Growth retardation - may be d/t malnutrition and recurrent infections (2’ to impaired immune system) ● In adults = anemia = poor economic productivity and earning capacity ● Increased post-op morbidity and mortality Symptoms of Anemia ● Non specific, minsan yung symptoms will only show if the Hgb is below 7-8 g/dL ● If anemia develops rapidly, symptoms will be more pronounced (blood loss d/t trauma) ● If anemia develops gradually, symptoms may be minimal even with severe anemia (because the body will try to compensate, usually pallor lang itu) ● Exertional dyspnea, headache, shortness of breath, weakness and fatigue ● Physiologic adjustments to anemia include: ○ Increase in cardiac output ○ Increase in oxygen extraction ○ Shunting of blood flow towards the vital organs’ tissues Etiologic Classification of Anemia (underlying pathology *IDA and Folate/B12 - usually nakikita yan sa period of growth spurt ng kids *MC cause of blood loss in children: Cow-milk enteropathy and Hookworm infestation * micro, macro, normo - look for MCV! * microcytic - MC = IDA, 2nd = thalassemia * macrocytic - MC= Megaloblastic anemia * normocytic - hemoglobinopathies ganern… Diagnosis of Anemia 1. History a. Age of onset b. Gestation and prenatal history c. Race and ethnicity d. Diet e. Age and Sex f. Drugs g. Family history h. Comorbidities 2. Physical Examination a. Pallor b. Frontal bossing c. Cheilosis, glossitis d. Hyperpigmentation e. Petechiae, rashes f. Splenomegaly g. Spooning of fingernails 3. Diagnostics (complete blood count) a. Hgb, Hct, RBC count b. RBC Indices c. RDW d. Platelet count e. WBC & differential count f. Reticulocyte count - in any patient with anemia needing transfusion, reticulocyte ct must be 1st evaluated, it will help you categorize the type of anemia g. PBS - counter check and correlate the findings of machine with microscopy 📌 MC hematologic disease of infancy and childhood, because infants IRON DEFICIENCY ANEMIA ● ● ● ● have limited sources of iron-rich foods; in adolescents they develop IDA because of increased demand because of growth spurt, menarche For optimal nutrition - 8-10 mg of iron is necessary Iron from human milk is 2-3x more efficiently absorbed than cow’s milk Clinical features ○ Pallor ○ Tachycardia ○ Neurologic/intellectual; function disturbances and irritability ○ Anorexia and pagophagia IDA: Biochemical and Laboratory Changes Prelatent ⬇ tissue Iron stores (BM hemosiderin) ⬇ serum ferritin Latent ⬇ serum iron ⬇ transferrin saturation ⬆ TIBC (serum transferrin) ⬆ Free erythrocyte protoporphyrins (FEP) Frank IDA ⬇ MCV, MCH (microcytic, hypochromic) ⬆ poikilocytosis, RDW (mas variable sila sa shape ganern) ● Ferritin - stored form of iron, provides estimate of your iron stores in the absence of inflammatory disease ● As iron stores depleted, iron becomes unavailable to form complexes with the protoporphyrin to form heme → FEP accumulate → Hgb synthesis is impaired → IDA progresses → rbcs become smaller in size and varied in size (micro-hypo-poikilo) ● Age-related parameters must be used, because the RBCs for younger infants are macrocytic IDA: Treatment ● Breastfeed exclusively for 6 mos ● (treatment dose) Oral/IV elemental iron: 4-6 mg/kg/day ferrous salts (sulfate, gluconate, fumarate) - starting at 4mos! ● Give vitamin C rich foods, increases the absorption of iron ● Iron Maintenance: ferrous sulfate 1-3mg/kg/day (elemental iron) ● Diet: iron-fortified, limit milk intake to 500ml/day - because calcium competes with Iron absorption ● Packed RBC transfusion - for those with hemodynamic instability MD 2024 - dawntreader - OCEAN GRACE 🌊 1/5 COMMON HEMATOLOGIC CHILDHOOD DISEASES - (DR. ANNA MARIE ESPALDON) Thalassemia: Diagnosis ● Sa CBC - Low MCV, low Hgb, high RBC ct, give iron for 1 month - if hindi mag normalize consider Thalassemia ● Hemoglobin electrophoresis - first diagnostic test; measures fraction of HB A, A2, F, H, E and other variants ● Iron Studies - Serum ferritin (N/↑), TIBC, serum Iron, red cell folate ● ß and α globin gene mapping Consequences of Thalassemia 😅 Lucky Iron Fish: Mechanism of Action ● Quick and easy to cook with, simply drop it in boiling liquid for 10 mins; reusable for 5yrs, no A/E ● Releases 6-8 mg of absorbable iron 📌 THALASSEMIA The Thalassemia Belt * yung sa Cambodia chika ni doc ~ thalassemia talaga yung underlying cause nila ● Inherited defect in the rate of globin chain synthesis ● Alterations in the amounts of HbA2 and HbF are seen Pakitandaan po yung mga charts sa baba, lalo na yung table, tnx! * Hb Barts - not compatible with life, hydrops fetalis ● B-thalassemia - decrease in beta-globin chains causing a relative excess of alpha globin chains, this will also manifest as RBC inclusions ● Alpha-thalassemia - there is excess of beta and gamma chains, which are seen in the fetal life, these are non-functional hgb that have high affinity for oxygen Thalassemia: Genetics ● Autosomal recessive pattern ○ 25% - risk of having major thalassemia ○ 25% - no thalassemia ○ 50% - risks of having minor thalassemia ● Genetic counseling is advised Thalassemia Major: Clinical Features Etiology: there is increased sequestration of your RBCs at the spleen ● Chipmunk facies - because the bones that are not supposed to produce rbcs are producing rbcs; there is hair-on-end appearance because of widening of diploic spaces, tapos may mga fractures din ● Severe hemolytic anemia ● Progressive splenomegaly ● Progressive pallor ● Jaundice ● Skeletal abnormalities ● Growth retardation ● Amenorrhea ● Thalassemia patients would require blood transfusion every month → accumulation of iron → Treatment Related Iron Overload Thalassemia: Treatment ● Hypertransfusion in Childhood ○ Maintain 10-12 g/dl ○ Pretransfusion Hb is not <10g/dL, kasi may BM expansion already - yung facies ng thalassemia patient will manifest (chipmunk) ○ Advantages of Hypertransfusion ■ Permits normal growth of physical activities ■ Suppresses erythropoiesis and extramedullary erythropoiesis ■ Prevents skeletal damage ■ Prevents GI absorption of iron ■ Iron overload is no more than low transfusion ○ Hgb levels falls 1g/week - kaya ka nagbibigay ng transfusion almost monthly ● NO IRON SUPPLEMENTATION - contraindicated - this will only lead to iron deposition ● Folic acid supplementation - for nuclear maturation (iron is for rbc membrane maturation) ● Iron chelation therapy for iron overload (Ferritin >1000ug/dl) ○ To bind free extracellular iron ○ To remove excess intracellular iron ○ To attain a negative iron balance (ex: iron excretion>iron input) ○ Target: Ferritin ≤ 1000ng/ml; monitored every 3-6 months ○ Deferoxamine - 40-60 mg/kg/day, subcutaneously, 8-10h nightly, CONS: not available - Local: in patient - 4 days ○ Oral Iron chelators: deferasirox and deferiprone - expensive ● Bone marrow transplant ● Recent advances: 5-Azacytidine, gene therapy 📌 MC enzymatic disorder of RBCs G6PD DEFICIENCY ● ● ● ● X-linked disorder Free radical mediated oxidative damage to RBCs = hemolysis Diagnosis: direct or indirect demonstration of reduced G6PD in the RBCs ○ Diagnosed early because of NBS Pathophysiology * children with G6PD - usually asymptomatic unless ma-expose sa trigger * mainly supportive and management * yung mga rbcs with heinz bodies - once they pass through the spleen, magiging bite cells sila to remove the heinz bodies MD 2024 - dawntreader - OCEAN GRACE 🌊 2/5 COMMON HEMATOLOGIC CHILDHOOD DISEASES - (DR. ANNA MARIE ESPALDON) Clinical Signs and Symptoms ● Anemia ● Jaundice ● Splenomegaly ● Dark urine - hemoglobinuria ● Reticulocytosis - because of increased erythropoiesis ● Decreased haptoglobin 2 Main Phases: 1. Primary Hemostasis Involves the binding of the platelet on to the exposed collagen of the subendothelium of the blood vessel Target: Platelet plug 2. Secondary Hemostasis Target: Blood clot Laboratory tests ● CBC - anemia ● PBS - Heinz bodied ● G6PD level determination ● G6PD gene mutation Evaluation of Hemostasis ● History: Family hx and Bleeding hx ● Physical Examination ○ Mucocutaneous bleed (more likely superficial) ○ Deep bleed ● Venous thrombosis ○ Swollen, warm extremities, unexplained dyspnea, varicosities ● Arterial thrombosis ○ Precipitous impairment of organ function (stroke, AMI, acute limb), cold, pulseless, pain Treatment ● Avoidance of triggers ● Mainly supportive ● ● ● ● ● PANCYTOPENIA All 3 cell lines are affected (RBC, WBC and Platelets), BM microscopy is needed Categories based on Marrow Cellularity Hypocellular Marrow - constitutional marrow failure syndromes, acquired aplastic anemia (MC in children), hypoplastic MDS ○ What you see the BM - empty with a lot of fat Cellular Marrow - in primary BM diseases (acute leukemia, MDS), severe infections and secondary systemic diseases (SLE and storage diseases) ○ Kapag uniformed yung itsura - usually primary yarn - leukemia BM infiltration - metastatic solid tumors (neuroblastoma ~ rosettes), myelofibrosis and HLH Acquired Aplastic Anemia - because of cytotoxic effects, immune-mediated sya usually - management by immunosuppression ● Drug-induced: chemotherapeutic drugs, antibiotics (chloramphenicol), insecticides, chemicals (benzene), anticonvulsants, NSAIDs, recreational drugs (ecstasy) ● Chemicals: insecticide ● Virus: CMV, EBV, HIV, Hepa B & C, seronegative hepatitis, mumps, rubella ● Pregnancy ● Marrow replacement: leukemia, metastasis, MDS, MF ● Clinical findings: ○ Anemia ○ Leukopenia ○ Thrombocytopenia ○ HSM/LAD - only in infiltrative marrow failures ● Laboratory Findings: ○ Pancytopenia (normo or macrocytic) ○ Reticulocytopenia - automatic dapat na nagccompensate ito sa Anemia ○ Fetal Hgb - may be elevated ○ BM - replaced by fatty tissue ○ Chromosomal breakage assay: normal (to R/O Fanconi Anemia) ● Treatment: ○ HSCT - if with HLA matched family donor = 90% long term survival ○ Immunosuppression with ATG and cyclosporine, methylprednisolone ○ Supportive care: GCSF, blood component therapy Defect Hemorrhage Bleeding Labs Timing of bleeding Primary Platelet or blood vessel Microhemorrhages (petechiae, purpura) Mucosal bleeding (gum bleeding, epistaxis) Increased BT, low platelet ct. Immediately after trauma Secondary Coagulation factors Large palpable ecchymoses Deep tissue bleeding (hematoma, hemarthrosis) Normal BT and Platelet ct.; increased PT and/or PTT Bleeding minutes to hours after trauma HEMOSTASIS Major Components of Hemostasis Five main components 1. Vessel wall 2. Platelets 3. Clotting factors 4. Anti-coagulation factors 5. Fibrinolytic factors MD 2024 - dawntreader - OCEAN GRACE 🌊 3/5 COMMON HEMATOLOGIC CHILDHOOD DISEASES - (DR. ANNA MARIE ESPALDON) HEREDITARY CLOTTING FACTOR DEFICIENCIES Hemophilia ● MC congenital clotting factor deficiency ○ FVIII - Hemophilia A ○ FIX - Hemophilia B ● X-linked recessive inheritance ● May nangyayaring clotting, pero very slow and unstable, delayed formation of fibrin clot and if it forms - it is very friable Hemophilia: Management 1. Clotting factor replacement: F VIII Expected response 1 IU/kg = 2% rise Half-life 8-12 h 2. 3. 4. F IX 1 IU/kg = 1-1.5% rise 16-24 h Supportive care: RICE (rest ice compress elevate) Blood component therapy - not done anymore unless walang factor concentrate na available Antifibrinolytic therapy - if may mild deficiencies Treatment of acute bleeds ● The earlier the better ● When in doubt, treat and treat quickly ● A shot in time saves VIII or IX ● ● ● ● THROMBOCYTOPENIA Platelet count less than 150 x 109/L Decreased production - acquired or congenital Increased destruction Sequestration in an enlarged organ Immune Thrombocytopenia ● MC acute onset thrombocytopenia in an otherwise healthy child ● Peaks at 1-4 yo, affects 1:20,000 children ● In 50-60% of cases, it is associated with history of viral illness, 3-4 wks prior to presentation of symptoms ● Resolves spontaneously within 6 mos in 70-80% of cases ● 20% - progresses to Chronic ITP ● Microscopy: if nakakita ka ng medium-large or giant platelets - clue na yern for ITP, more likely immune; nakikita din ito sa dengue Hemophilia: Clinical Manifestations ● Musculoskeletal Bleed ○ Hemarthrosis - bleeding into joint space, hall-mark of Hemophilia ○ Muscle bleed ○ Iliopsoas bleed ● Life threatening Hemorrhages ○ CNS bleed ○ Bleeding around the airway ○ Exsanguinating hemorrhages ● Miscellaneous: Oral, Mucosal, Genitourinary ITP: Pathophysiology ● Spleen - there is increase platelet clearance ○ CD4 Th cells - Ag presentation ○ B cells - platelet reactive plasma cells, produce autoantibodies ○ CD8 Tc cells - directly lyse platelets ● Blood - Tc and plasma cells further induce autoimmune response ● BM - Tc and plasma cells target megakaryocytes Onset of symptoms: 1. Initially: tingling warmth, increasing pain, decreased joint motion 2. Feeling of vague pain on motion, increased circumference of affected limb, pseudotumor formation 3. Vague symptoms of lower abdominal or upper thigh discomfort ○ Gait: hips flexed, inwardly rotated ○ Unable to extend hip (normal internal/external rotation) iliopsoas bleed ○ PE findings: loss of hyperextension of the hip Hemophilia: Laboratory Evaluation 1. Partial thromboplastin Time (PTT) - measures all procoagulant factors except FVII and FXIII Prolonged! 2. Factor Assay Hemostatic level FVIII - 30 U/dL FIX - 25-30 U/dL Mild-moderate FIX deficiency may be missed 3. Inhibitor Assay Inhibitors would consume the clotting factors ~ no response na sa patient Bethesda assay 1 BU = amount of antibody that will inactivate 50% of the factor in 2 hours when the residual factor level is between 25-75 U/dL 4. Genetic Testing Hemophilia A - Gene inversion (45%) Hemophilia B - Missense point mutations (60%) 50% FIX protein is non-functional; others have no FIX protein production at all ITP: Clinical Features ● Petechiae ● Purpura ● Gum bleeding - in an otherwise healthy child MD 2024 - dawntreader - OCEAN GRACE 🌊 4/5 COMMON HEMATOLOGIC CHILDHOOD DISEASES - (DR. ANNA MARIE ESPALDON) ITP: Laboratory findings ● CBC - normal except for thrombocytopenia ● PBS - (+) large platelets ● BMA - normal erythroid and myeloid series; increased megakaryocytes (in compensation ~ liver produces ↑ TPO) ○ Indications: ■ Abnormal WBC diff count ■ Unexplained anemia ■ Hx and PE findings suggestive of bone marrow failure/malignancy ITP: Treatment ● ● ● ● ● ● Plate transfusion is not indicated dahil may presence ka ng anti-platelet antibody - ma-cconsume lang yarn! IVIg muna before prednisone - kasi for leukemia ituu, baka ma-miss mo yung diagnosis nya Safe platelet ct for steroid therapy: >20,000 plt ○ Possible long-term side effects of steroids ■ Growth failure ■ DM ■ Osteoporosis For relapse and recurrent - splenectomy - ONLY on patients diagnosed with Chronic ITP, who are > 5 yo. Those who are younger have higher risk for post splenectomy infections. For B-cells - give Rituximab! Fostamatinib - inhibits platelet; treat thrombocytopenia (less than normal number of platelets) in adults with chronic immune thrombocytopenia (ITP; an ongoing condition that may cause unusual bruising or bleeding due to an abnormally low number of platelets in the blood) who were not helped with another treatment. 45 points - for Hema-Onco ● Read Nelson’s pa din, lalo na for Blood Transfusions! ● Pages 4514 to 4535 MD 2024 - dawntreader - OCEAN GRACE 🌊 5/5