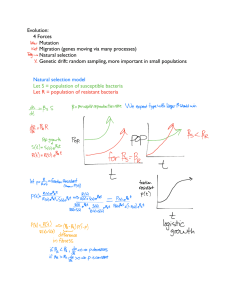
Notes Questions Antibiotics Videos Home Podcast Medicine Books Flashcards Infectious Disease More Antibiotics The Zero to Finals Medical Revision Podcast Antibiotics 00:00 | 09:51 Antibiotics are used to treat bacterial infections. They work in various ways to either stop the reproduction and growth of bacteria (bacteriostatic) or kill the bacteria directly (bactericidal). Antibiotics need to be used carefully as overuse or inappropriate use can lead to resistance of bacteria to those antibiotics and increasing di!culty in treating infections. Local Resistance and Guidelines The bacteria in di#erent populations develop resistance to di#erent antibiotics. For example the e. coli in one area of the country might be particularly resistant to trimethoprim whereas in another area of the country they may be resistant to nitrofurantoin but sensitive to trimethoprim. Therefore it is necessary to have local policies that guide what antibiotics to use in di#erent scenarios. TOM TIP: In your OSCEs questions about treating infections can always be answered with “treat with antibiotics as per the local antibiotic policy”. Mechanism of Action Antibiotics That Inhibit Cell Wall Synthesis Antibiotics with a beta-lactam ring Penicillin Carbapenems such as meropenem Cephalosporins Antibiotics without a beta-lactam ring Vancomycin Teicoplanin Antibiotics that Inhibit Folic Acid Metabolism Bacteria produce their own folic acid in a series of steps. This chain starts with para-aminobenzoic acid (PABA), which is directly absorbed in to the cell across the cell membrane. PABA is then converted to dihydrofolic acid (DHFA), then tetrahydrofolic acid (THFA) and finally folic acid. Antibiotics can be used to disrupt steps along this chain: Sulfamethoxazole blocks the conversion of PABA to DHFA Trimethoprim blocks the conversion of DHFA to THFA Co-trimoxazole is a combination of sulfamethoxazole and trimethoprim Metronidazole The reduction of metronidazole into its active form only occurs in anaerobic cells. When partially reduced metronidazole inhibits nucleic acid synthesis. This is why metronidazole is e#ective against anaerobes and not aerobes. Antibiotics that inhibit protein synthesis by targeting the ribosome Macrolides such as erythromycin, clarithromycin and azithromycin Clindamycin Tetracyclines such as doxycycline Gentamicin Chloramphenicol Penicillin Allergy “Penicillin allergy” is very common. True penicillin allergy can lead to anaphylaxis and death so should not be taken lightly. The problem is that true allergy is much more rare than reported allergy and being labelled as penicillin allergic stops patients from getting many potentially life saving antibiotics. Around 10% of patients report penicillin allergy however only around 10% of patients that report penicillin allergy have a true allergy to penicillin. It is often believed that 10% of patients with penicillin allergy will have a reaction to cephalosporins and carbapenems. In reality this is closer to 1%. TOM TIP: When taking an allergy history always ask what reaction patients have had to become labelled allergic. If they report diarrhoea for example, this is a side e!ect rather than an allergy and means if necessary (for example in life threatening sepsis) they can still receive that medication. Antibiotic coverage Use this table to think about how you could treat di#erent presentations of patients with infections. For example, think about what antibiotics would be appropriate for a patient with a chest infection and why. This table is not exactly accurate and should not be used for treating patients, but is helpful to gain an understanding of the general patterns of antibiotic coverage. When learning antibiotic coverage I used this stepwise process of escalating antibiotic treatment in a hospital patient to remember what antibiotics covered what bacteria: Start with amoxicillin which covers streptococcus, listeria and enterococcus Switch to co-amoxiclav to additionally cover staphylococcus, haemophilus and e. coli Switch to tazocin to additionally cover pseudomonas Switch to meropenem to additionally cover ESBLs Add teicoplanin or vancomycin to cover MRSA Add clarithromycin or doxycycline to cover atypical bacteria Last updated February 2019 Copyright 2016-2023 - Zero to Finals - All Rights Reserved