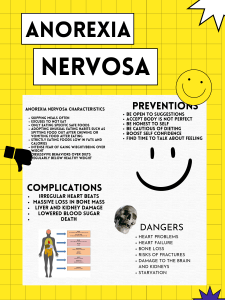
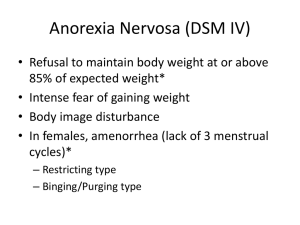
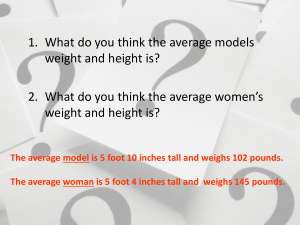
EATING DISORDERS OVERVIEW Gross disturbance in eating behaviors Very common in adolescent females Age of Onset: Anorexia Nervosa - typically begins between 14 to 18 years old Bulimia Nervosa – typically begins between 18 to 19 years old Etiology: Disorder Anorexia Nervosa Biologic Obesity; Dieting at an early age Bulimia Nervosa Obesity; Dieting; Possible serotonin & norepinephrine disturbances; Chromosome 1 susceptibility Developmental Issues of developing autonomy & having control over self & environment; develop a unique identity; dissatisfaction with body image Self-perceptions of being overweight, fat, unattractive, & desirable; Dissatisfaction with body image Family Family lacks emotion nal support; parental maltreatment; can’t deal with conflict Chaotic family with loose boundaries; parental maltreatment including possible physical or sexual abuse Socio-Cultural Cultural ideal of being thin; Media focus on beauty, thinness, fitness; Preoccupation with achieving the ideal body Same as above; weight-related teasing TYPES OF EATING DISORDERS Anorexia Nervosa A life-threatening eating disorder characterized by the client’s Refusal or inability to maintain a minimally normal body weight Intense fear of gaining weight or becoming fat Significantly disturbed perception of the shape or size of the body Steadfast inability or refusal to acknowledge the seriousness of the problem or even that one exists Symptoms: Body image disturbance – occurs when there is an extreme discrepancy between one’s body image & the perceptions of others & extreme dissatisfaction with one’s body image Amenorrhea Alexithymia – difficulty in identifying & expressing feelings Depressive symptoms such as depressed mood, social withdrawal, irritability & insomnia Preoccupation with thoughts of food (grocery shopping, collecting recipes or cookbooks, counting calories, creating fat-free meals, cooking family meals) Feelings of ineffectiveness Inflexible thinking Strong need to control environment Limited spontaneity & overly restrained emotional expression Engage in unusual or ritualistic food behaviors (refusing to eat around others, cutting food in minute pieces, not allowing food to touch their lips) Complaints of constipation & abdominal pain Cold intolerance Lethargy Emaciation Hypotension, hypothermia & bradycardia Electrolyte imbalances Leukopenia & mild anemia Treatment: Medical Management Focuses on weight restoration, nutritional rehabilitation, rehydration, correction of electrolyte imbalances Access to bathroom is supervised to prevent purging Psychopharmacology Amitriptyline (Elavil) in high doses (up to 28mg/day) can promote weight gain Olanzapine (Zyprexa) for antipsychotic effect (for bizarre body image distortions) & associated weight gain Fluoxetine (Prozac) shows some effectiveness in preventing relapse Psychotherapy Family Therapy Individual Therapy Bulimia Nervosa Characterized by recurrent episodes (at least twice a week for 3 months) of binge eating followed by inappropriate compensatory behaviors to avoid weight gain such as purging Binge Eating – consuming large amount of food (far greater than most people eat at one time) in a discrete period usually 2 hours or less Purging – the compensatory behaviors designed to eliminate food by means of selfinduced vomiting or misuse of laxatives, enemas & diuretics Binging or purging episodes are often precipitated by strong emotions & followed by guilt, remorse, shame or self-contempt Clients are aware that their eating behavior is pathologic & go to great lengths to hide it from others Symptoms: Self-evaluation overly influenced by body shape & weight Usually within normal weight range, possible underweight or overweight Restrict of total calorie consumption between binges, selecting low-calorie foods while avoiding foods perceived to be fattening or likely to trigger a binge Depressive & anxiety symptoms Possible substance use involving alcohol or stimulants Loss of dental enamel Chipped, ragged appearance of teeth Increased dental caries Menstrual irregularities Dependence on laxatives Esophageal tears F&E abnormalities Metabolic alkalosis (vomiting) or metabolic acidosis (diarrhea) Treatment: Cognitive-Behavioral Therapy Found to be the most effective treatment for bulimia Strategies are designed to change the client’s thinking (cognition) & actions (behavior) about food & focus on interrupting the cycle of dieting, binging & purging & altering dysfunctional thoughts & beliefs about food, weight, body image & overall self-concept Psychopharmacology Antidepressants such as Tofranil, Elavil, Parnate, Nardil, Prozac effective in reducing binge eating; also improves moods & reduces preoccupation with shape & weight; however, most of the positive results are short-term in nature NURSING INTERVENTIONS Establishing nutritional eating patterns Sit with the client during meals & snacks Offer liquid protein supplement if unable to complete a meal Adhere to treatment program guidelines regarding restrictions Observe client following meals & snacks for 1 to 2 hours Weigh client daily in uniform clothing Be alert for attempts to hide or discard food or inflate weight Helping the client identify emotions & develop non-food coping strategies Ask the client to identify feelings Self-monitoring using a journal Relaxation techniques Distractions Helping client deal with body image issues Recognize benefits of a more near-normal weight Assist to view self in ways not related to body image Identify personal strengths, interests, talents Providing client & family education Client: Basic nutritional needs Harmful effects of restrictive eating, dieting, purging Realistic goals for eating Acceptance of healthy body image Family & Friends: Provide emotional support Express concern about client’s health Encourage client to seek professional help Avoid talking only about weight, food intake, calories Become informed about eating disorders It is not possible for family & friends to force the client to eat; the client needs professional help from a therapist or a psychiatrist