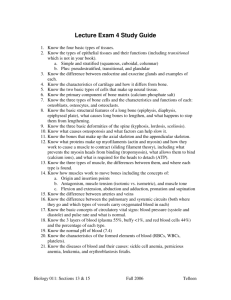
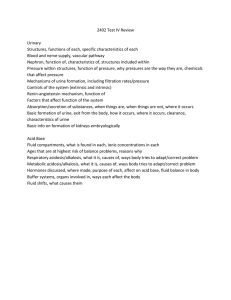
Module 1 Etiology- etiology of a disease defines the cause of the disease. Pathogenesis- the manner of development of a disease. Clinical manifestations- can be either objective (observed by physician) or subjective (described by patient) Treatment implications- the clinical and medical relevance of a specific treatment. Name Plasma membrane Memorable phrase Description Separates the interior Cell’s fortification of the cell from the outside environment Fluid part enclosed by Cytoplasm Cell’s environment the membrane, contains organelles Contains most of the Nucleus Cell’s brain genetic material, in the form of DNA System of metabolic Endoplasmic Reticulum processes (smooth Cell’s pipe system ER), protein manufacturing ribosomes (rough ER) It tags vesicles and Golgi apparatus Cell’s delivery center proteins to help them get carried to their correct destinations Organizes and produces the Centrosome Cell’s anchor microtubules of the cell’s cytoskeleton Produce energy for the cell, break down Mitochondria Cell’s powerplant carbohydrates and some Durations lipids to form molecule ATP Ribosome Cell’s factories Translate RNA into proteins Vesicles filled with digestive proteins, can Lysosome Cell’s stomach absorb something and break it down into recyclable pieces Vesicles that defend Peroxisome Cell’s firemen (or neutralize) the cell from free radicals It modifies the cell’s Cytoskeleton Cell’s shapeshifter shape and ensures mechanical resistance to deformation Enclosed storage Vacuole Cell ‘s compartments vessels which are filled with water containing inorganic and organic molecules Basic Cell Function- Cells-combine to form specialized tissue Tissues- preform organs with precise purpose à Organs- form systems that maintain and perform complex actions to meet the bodies needs systems Differentiation- process by which cells become specialized by type, function, structure, and cell cycle. Energy production- Cells can obtain energy from two main sources: the breakdown of glucose (a type of carbohydrate) and the breakdown of triglycerides (a type of fat). When these sources are not readily available, cells can turn to protein for energy. What is Homeostasis? - A state of equilibrium or balance within the organism to maintain usual function. (Can be maintained by separate organs or by the entire body at once.) Fluid Balance- Water carries nutrients into the cells, waste produces out of cells, enzymes in digestive secretions, and blood cells around the body. (Fluid help to facilitate the movement of body parts, e.g., joints, lung, and heart) Signs & Symptoms of Fluid Overload- Edema (feet and ankles), Difficulty breathing while lying down, Crackles, High BP, Jugular vein distension, cough, dyspnea, and Strong rapid pulse. Signs & Symptoms of Fluid Volume Deficit- lethargy, wight loss, poor skin turgor, low urine output, sunken eyes, dark yellow urine, confusion/mental changes, weakness, lack of sweat, Low BP, rapid heart rate, abnormal labs/electrolytes. Causes of Fluid Loss- hemorrhage, excessive perspiration, polyuria, abdominal surgery, vomiting/diarrhea, excessive use of laxatives, nasogastric drainage, excessive GI suctioning, fistulas. How does fluid move- Fluid movement between compartments is primarily accomplished through osmosis, the movement of fluid (specifically water) across a semipermeable membrane from an area of lower concentration to an area of higher concentration Selective Permeability- allows the cells to maintain homeostasis (Some have free passage in and out of the cell) Cellular Permeability- is the ability of the cell to allow passage of some substances through the membranes, and not others. Diffusion- the movement of solutes from an area of Higher concentration to an area of Lower concentration. Osmosis- A process by which molecules of a solvent tend to pass through a semipermeable membrane from a less concentrated solution into a more concentrated one, thus equalizing the concentrations on each side of the membrane. Facilitated Diffusion- The movement of substances from an area of higher concentration to an area of lower concentration with the assistance of a carrier molecule (Example: Insulin transports glucose into the cells using this method) Intracellular Fluid (ICF): Fluid found inside the cells (rich in potassium (K+), magnesium (mg), phosphates (PO3), and proteins.) 1. Extracellular Fluid (ECF): Is further divided into (ECF is rich in sodium (Na), chloride (Cl), and bicarbonate (HCO3−)) 1. Intravascular Fluid (IVF): Inside the blood vessels 2. Interstitial Fluid (ISF): Between the cells 3. Transcellular Fluid (TCF): A third compartment where fluid is found 4. Fluid in the peritoneal, pleural, and pericardial cavities 5. Cerebrospinal fluid 6. Fluid in the joint spaces, lymph system, eyes, and gastrointestinal tract Hyponatremia: Low sodium levels. Water shifts into cells. Brain cells are especially susceptible to this cellular swelling, which causes cerebral edema and death. You will see this with Cushing syndrome and corticosteroids Hypernatremia: Can be seen with Addison's disease HYPERkalemia- high levels of Potassium. Causes: Cellular movement of K, Adrenal insufficiency, Renal failure, Excessive K+ intake, Drugs. S&S: Muscle weakness, Urine output little to none, Respiratory failure, Weak pulse or low HR, muscle twitches/cramps, Rhythm changes (tall T waves, long PR interval) HYPOkalemia- Low levels of Potassium. Causes: Drugs (loop diuretics), Inadequate consumption of K+, high water intake, Cushing’s Syndrome, Heavy fluid loss. S&S: Lethargy, Low shallow respirations, Lethal cardiac dysrhythmias, Loss of urine, Leg cramps, Limp muscles, Low BP. Hypocalcemia- Low calcium levels. Two signs specific to hypocalcemia may be present—the Trousseau and Chvostek signs. (To test for the Chvostek sign, tap the patient’s facial nerve in front of the ear. A spasm or brief contraction of the corner of the mouth, nose, eye, and muscles in the cheek is considered a positive sign and indicates increased neuromuscular irritability.) Hypercalcemia- Common causes (not a complete list): Antacids with Ca in them, Thiazide diuretics, Kidney dysfunction RAAS system-The Renin-Angiotensin-Aldosterone System (RAAS) is a hormone system within the body that is essential for the regulation of blood pressure and fluid balance (Renin, Angiotensin II, and Aldosterone) RAAS & Hypotension1. The kidneys signal the Juxta-Glomerular Cells to produce Prorenin (hypotension is the main stimulation to convert Prorenin into renin) 2. Renin is an enzyme that acts on Angiotensinogen (Angio = vessels, Tensinogen = vasoconstriction) Angiotensin is a plasma protein that is synthetized in the liver 3. Renin converts angiotensinogen into angiotensinogen 1 4. Next step takes place in the lungs- Where angiotensin converting enzyme (ACE) converts angiotensin 1 into angiotensin 2 (Angiotensin 2 is a powerful vasoconstrictor to the blood vessels. Arteries = Total peripheral resistance; Veins = increase in venous return.) Constriction of both the veins and arteries increase the blood pressure. Angiotensin 2’s effects on the kidneys- Angiotensin 2 effects the kidneys in two ways the Direct way and Indirect way. Direct: The GFR is proportional to the blood flow of the blood to the kidneys. - ANG 2 enters the glomerulus through the blood flow and vasoconstricts the blood flow, this decreases the GFR of the kidney, thus decreasing the blood flow Indirect: ANG 2 acts on the adrenal gland and releases aldosterone, aldosterone acts on the kidney and increases sodium and water reabsorption. Module 2 Han Selye described body changes with stress and called this protective stress response as the general adaptation syndrome (GAS). The body releases epinephrine during the alarm stage. Resulting in the release of catecholamines and cortisol (fight or flight syndrome). HR and BP elevated, pupils and bronchial dilate The resistance stage is when the body chooses the most effective and advantageous defense and Cortisol levels and the sympathetic nervous system return to normal. This stage is activated if the stressor is prolonged or overwhelms the body-Exhaustion Stage Steps in carcinogenesis: 1. Initiation: introduction of the agent 2. Promotion: initiation of uncontrolled growth 3. Progression: permanent malignant changes 4. Metastasis: Moves to other sites Inflammatory Response-Release of Histamine, Bradykinin, Prostaglandins Antigens- a toxin or other foreign substance in the body. Antigens are recognized by the lymphocytes T cells: cell-mediated immunity. They become sensitized to the disease. They learn to recognize the disease and fight it off B cells: humoral immunity Macrophages – Engulf foreign substances Blood is formed in the bone marrow Active Immunity- by having a disease and or by vaccinations. Passive Immunity- receiving antibodies: mother to baby, breastfeeding, and immunoglobulin. Innate: Provides immediate protection, nonspecific (providing protection against all invaders) Adaptive or acquired: Can take up to 7 to 10 days to provide protection specific to the antigen The FIVE CARDINAL SIGNS OF INFLAMMATION: Pain, heat, redness, swelling, and loss of function. Mast cells play an important role in how the immune system responds to certain bacteria and parasites and they help control other types of immune responses. They contain chemicals such as histamine, heparin, cytokines, and growth factors. Commom lab test to test inflammation: Erythrocytes Sedimentation Rate (ESR). Systemic Lupus Erythematosus (SLE) is an autoimmune disorder characterized by antibodies to nuclear and cytoplasmic antigens, multisystem inflammation, protean clinical manifestations, and a relapsing and remitting course. SLE is a chronic inflammatory disease that can affect almost any organ system, although it mainly involves the skin, joints, kidneys, blood cells, and nervous system. Its presentation and course are highly variable, ranging from indolent to fulminant. S/S Malar rash (butterfly rash on the face), polyarthritis, muscle pain, inflammation in the kidneys, lungs, and heart C: Changes in bowel or bladder habits A: A sore that does not heal U: Unusual bleeding or discharge T: Thickening or lump in the breast or elsewhere I: Indigestion or difficulty swallowing O: Obvious change in a wart or mole N: Nagging cough or hoarseness Cachexia- a generalized wasting syndrome in which the person appears emaciated, often occurs due to malnutrition. Fatigue, or feeling of weakness, results from the parasitic nature of a tumor, anemia, malnutrition, stress, anxiety, and chemotherapy. Benign-Slow, progressive, localized, well defined, resembles host (more differentiated), grows by expansion, does not usually cause death, causes less damage to host – adenoma, papilloma Malignant-Rapid growing, spreads (metastasis) quickly, fatal, highly undifferentiated. Sarcoma, Carcinoma Steps in carcinogenesis: 1. Initiation: introduction of the agent 2. Promotion: initiation of uncontrolled growth 3. Progression: permanent malignant changes 4. Metastasis: Moves to other sites Module 3 Normal ABG Levels pH- Hydrogen- 7.35-7.45 (determines if Acidotic or Alkalotic) PaCO2- Carbon dioxide- 35-45 mmHg (Respiratory) HCO3- Bicarbonate -22-26 mmol/L (Metabolic) Respiratory: The PaCo2 will be out of the normal range Metabolic: The HCO3 will be abnormal PaCO2 compensated or Uncompensated Compensation= The bodies attempt at correcting the imbalance Acidosis, we look at what HCO3 is doing Alkalosis, we look at what PaCO2 is doing If these levels are within normal range, the issues are (non)un-compensated If the opposing component has gone outside of the normal range, we know it is trying to correct the problem or compensate To assess how well the body is compensating, we need to look at the pH If the pH is not within or close to the normal range, then it is a partial compensation If the pH is within the normal range, then it is fully compensated Metabolic Acidosis- when acid accumulates in the body or when bicarbonate is lost from the body fluid, a bicarbonate deficit results, and metabolic acidosis occurs. Causes: Ketoacidosis, shock, severe diarrhea, impaired kidney function. S&S: Headache, lethargy, anorexia, deep rapid respirations, nausea, diarrhea, abdominal discomfort, coma/ dangerous dysrhythmias Metabolic Alkalosis-occurs when digestive issues disrupt the blood’s acid-base balance. Not life-threatening. Causes: loss of stomach acids (most common cause), excess of antacids, diuretics, potassium deficiency, reduced volume of blood in the arteries, heart/liver or kidney failure, genetic causes. S&S: confusion, hand tremors, lightheadedness, muscle twitching, nausea/vomiting, numbness/tingling in hands, feet or face. Respiratory Acidosis- A condition that occurs when the lungs cannot remove all the carbon dioxide the body produces. Causes: COPD, emphysema, asthma, pneumonia, conditions that affect rate of breathing, muscle weakness that affects taking deep breaths/breathing, obstructed airways, overuse of drugs (opioids) that affect the central nervous system. S&S: Hyperventilating, shortness of breath, fatigue, chronic exhaustion, headaches, drowsiness, confusion, sweating. Respiratory Alkalosis: A condition marked by low level of carbon dioxide in the blood due to rapid breathing. Causes: Anxiety/panic attack, fever, pregnancy, pain, tumor, trauma, severe anemia, liver disease. S&S: hyperventilation, tachycardia, low or normal BP, hypokalemia, numbness/tingling of extremities, seizures, high anxiety & irritability, hyper reflexes and muscle cramping. The integumentary system protects the body from a. Pathogens b. Regulates temperature c. Senses environmental changes d. Maintains water balance -Made up of: Skin, nails, hair, mucous membranes, glands Layers of the Skin: Epidermis- the outermost layer (squamous epithelia) Dermis- the middle layer (dense irregular connective tissue, hair follicles, nerves, smooth muscle) Hypodermis- the bottom layer (Subcutaneous tissue, soft fatty tissue, blood vessels, nerves and immune cells) Café-au-lait (macule)- brown/coffee colored mark on a baby’s back or legs Mongolian Spots- Dark, bruise-like spots on the back and upper butt area of a baby Port wine Stain- Red/wine colored smooth stain usually on face. Albinism- Genetic mutation that affects the amount of melanin produced resulting in light skin tone, eye color and hair color. (Impairs optic nerve development causing vision problems) Sign- A sign is something that can be observed externally (Noted by physician) Symptom- is felt internally (Reported by patient) Inflammatory Integumentary Disorders Contact Dermatitis- An acute inflammatory reaction triggered by direct exposure to an irritant or allergen-producing substance (metals, chemicals, adhesives, cosmetics & plants) - Typically, manifestations of allergic contact dermatitis include pruritus, erythema, and edema at the site, but small vesicles may also be present. Atopic Dermatitis (Eczema)- Chronic inflammatory condition, cause is unknown. May result from an immune system malfunction, similar to hypersensitivity (an elevated level of immunoglobulin E is usually present) - Inherited tendency and may be accompanied by asthma/ allergic rhinitis Signs and symptoms: - Red to brownish-gray colored skin patches - Pruritus, which may be severe, especially at night - Vesicles - Thickened (lichenified), cracked, or scaly skin - Irritated, sensitive skin from scratching Urticaria (Hives)- Consists of raised erythematous skin lesions all over the body. Lesions are a result of a type I hypersensitivity reaction. It occurs when histamine release is initiated. Psoriasis- Described as silver, scaly skin. A common chronic inflammatory condition that affects the life cycle of the skin cells, specifically keratinocytes. Cellular proliferation is significantly increased in this disorder, such that cells build up too rapidly on the skin’s surface. can be a result of an autoimmune process in which the body—specifically T lymphocytes— mistakes normal skin cells as foreign. Infectious Integumentary Disorders o Staphylococcus and Streptococcus generally are the common culprits in integumentary infections o BACTERIAL INFECTIONS -Folliculitis: infections involving the hair follicles (Hot tubs, pools, shaving) -Furuncles: infections that begin in the hair follicles and then spread into the surrounding dermis. Presents as a firm red painful nodule, that may be filled with a purulent exudate. -Impetigo: a common and highly contagious skin infection. -Cellulitis: an infection deep in the dermis and subcutaneous tissue. Cellulitis appears as a swollen, warm, tender area of erythema o Erythema and warmth is D/T the increased blood flow to the area -Necrotizing Fasciitis: is a serious infection that is generally rare, although its incidence rates are rising. One out of four people who develop this infection will die from the disease. Also known as “flesh-eating bacteria,” necrotizing fasciitis can aggressively destroy skin, fat, muscle, and other tissue Viral Infections Herpes Simplex type 1- Above the waist. A cold sore, is a viral infection typically affecting the lips, mouth and face. Herpes Simplex type 2- Below the waist. Thought to stay in the genitalia region. Herpes Zoster (Shingles)- caused by the varicella-zoster virus. This condition usually appears in the adulthood years after a primary infection with varicella (chickenpox) has occurred in childhood. Follows dermatomes. Verrucae (Warts)- are caused by a number of human papillomaviruses (HPVs). These skin lesions can develop at any age and often resolve spontaneously. - Condyloma acuminatum- Genital warts Molluscum contagiosum- a poxvirus infection that is characterized by clusters of pink, coneshaped, smooth, waxy, or pearly papules 2 to 5 mm in diameter Parasitic Infections Tinea- Tinea typically manifests as a circular, erythematous rash, which is usually associated with pruritus and burning. These fungi typically grow in warm moist places. Scabies- Mite infestation. Female mites burrow into the epidermis. This burrowing appears as small light brown streaks on the skin Pediculosis (Lice) – lice infestation, lice bite and suck the host’s blood Burns First degree burn- (Superficial) burns affect only the epidermis. These burns cause pain, erythema, and edema. Second degree burn- (partial- thickness) burns affect the epidermis and dermis. These burns cause pain erythema, edema and blistering. Deep partial thickness burns involve hair follicles and scarring is common. Third-degree burn – (Full thickness) burns extend into deeper tissues. These burns cause white or blackened, charred skin that may be numb. - Burn treatment is complex and varies depending on the location and severity of the injury. Ulcer Staging Stage 1- Skin is unbroken but inflamed Stage 2- Skin is broken to epidermis or dermis Stage 3- Ulcer extends to subcutaneous fat layer Stage 4- Ulcer extends to muscle or bone, Undermining is likely How do we screen for melanoma? - Asymmetry, Border, Color, Diameter Disorders of the Musculoskeletal System Bone- is a living, metabolically active tissue. This is the site of fat and mineral storage (especially calcium) as well as Hematopoiesis. o Osteoblasts: Build bone through collagen o Osteoclasts: Enable the matrix to be absorbed; assist with the release of calcium and phosphate o Osteocytes: Mature cells that help maintain the bone matrix; also play a major role in the release of calcium into blood Muscles: Motion requires a skeleton with moveable joints and muscles acting on the bones. - 3 types of muscle, Skeletal (connect to bone), Smooth and Cardiac Kyphosis- excessive outward curvature of the spine, causing hunching of the back. (Upper, shoulder area) Lordosis- excessive inward curvature of the lumbar spine. (Lower back) Scoliosis- a sideways curvature of the spine Edema Grading Scale 1+: 2mm depression, barely detectable. Immediate rebound 2+: 4mm deep pit, A few seconds to rebound 3+: 6mm deep pit, 10-12 seconds to rebound 4+: 8mm very deep pit, >20 seconds to rebound Types of Fractures -Simple fracture-a fracture with a single break in the bone and in which bone ends maintain their alignment and position A-Transverse fracture-a fracture straight across the bone shaft B-Oblique fracture-a fracture at an angle to the bone shaft C-Spiral fracture-a fracture that twists around the bone shaft D-Comminuted fracture-a fracture characterized by multiple fracture lines and bone pieces E-Greenstick fracture-an incomplete fracture in which the bone is bent and only the outer curve of the bend is broken; commonly occurs in children because of minimal calcification and often heals quickly F-Compression fracture-a fracture in which the bone is crushed or collapses into small pieces 5 P’s of Compartment Syndrome -Paresthesia -Pallor -Pain -Paralysis -Pulselessness Osteoarthritis: (WEAR+ TEAR) develops gradually & intermittently over several months when bone rubs against bone. Common sites are Hips, Knees, Lower back, Neck, Feet, and finger tips. S&S: Stiffness in the morning that goes away after a few minutes of activity, stiffness after resting for an hour or more. Rheumatoid Arthritis: (INFLAMMATORY condition) Immune system attacks the tissues in your joints causing pain and stiffness that worsen over time. Common Sites: Any joint, mostly seen in Hands, wrists and Feet. S+S: morning stiffness that improves after an hour or longer. Occasionally prolonged joint stiffness in the morning is the first symp. Of RA. Osteoporosis: causes bones to become weak and brittle, decrease in osteoblast activity and increase in osteoclast activity. Bones can be so weak and brittle that a fall or mild stresses (bending over, stepping off a curb, sneezing, and or coughing) can cause a fracture. Common Sites: Hip, wrist and spine. Module 4, 5, and 6 Peritonitis-Inflammation of the Peritoneum-Inflammation and abdominal wall is spasming What will mechanical obstructions: FECAL IMPACTION What can cause Hiatal hernia? The stomach moves up because of a weaken of the diaphragm, causes are coughing, vomiting, pregnancy, obesity, straining to defecate. Why does a person experience diarrhea when taking an antibiotic? Because it also kills good bacteria (Flora) The most common cause of PUD is NSAIDs and H. pylori. What two most common inflammatory bowel diseases are? Crohn’s disease and Ulcerative colitis. What is the main cause of chronic pancreatitis? Alcohol What is it called when the intestine telescopes into an adjacent portion of the intestine? Intussusception Heartburns are most likely to happen when the esophageal spams. A Child that presents a cleft lip/plate is caused by a congenital birth defect. The most common cause of Acute Gastritis is Gallstones. Which hepatitis is most transmitted by fecal to oral? Hepatitis A A patient comes in with Right Lower abdominal pain, fever, nausea, and with rebound tenderness. What do they mostly have? Appendicitis What is a serious complication of GERD? Esophageal Cancer A patient that is sent home with untreated diarrhea, what can happen to them? Unbalanced electrolytes and dehydration. What will you see in a patient that has gallstones that were obstructing the bile duct? Pain the RIGHT upper Quadrant. What does dysphagia mean? Difficulty swallowing. If a patient has chronic gastritis, what will they present? Dull epigastric pain, a sensation of fullness with minimal intake. Patient starts to get pain 30 mins to an hour after a meal, what does the patient most likely have? GASTRIC Ulcers (NOT common but DEADLY) Duodenal Ulcers pain is relieved by a meal, it’s the most common but NOT Deadly. What is true about ulcerative colitis? Ulcers penetrate the inner lining of the abdomen ONLY. What is the clinic manifestation of portal hypertension? Vomiting blood from esophageal varices. What is expected to see in ACUTE gastritis? Vomiting, epigastric pain, and cachexia What is an early sign of stress ulcer? Hemorrhage (vomiting blood) If you have a patient that has chronic bleeding from a gastritis ulcer, what do you expect to see? Blood in the stool Where's the topical site of pain from diverticulitis? In the LOWER LEFT quadrant. What is an early sign of cancer in the ascending colon? Occult blood in the stool. If your patient is presenting jaundice, what disease might they have? Liver Disease If you had a patient that dysphagia, what does you expect to see? Weight LOST You have a patient that is anorexic, has abdominal pain, rigid abdominal wall, and fever of 101.0, what do you think is happening? What causes pyelonephritis? UTIs What electrolyte imbalance can cause fatal cardiac arrest? Potassium Why do patients get dialysis? To remove waste and fluids. What can cause obstruction in the renal system? Tumor or enlargement of the prostate. What is the order of filtration through the kidneys? Glomerulus, Proximal Convoluted tubules, loop of Helene, and into the Collecting ducts. Stress incontinence is due to increased abdominal pressure under stress. Urge Incontinence due to involuntary contraction of the bladder muscles. Overflow Incontinence is due to a blockage of the urethra. Neurogenic Incontinence is due to impaired functioning of the nervous system. What can cause post-renal injury? Obstruction What causes a pre-renal injury? Interruption the blood flow. What is the function of the urinary system? Remove water and waste, regulate the PH, production of erythropoietin, renin for the blood pressure regulation. What is nephrolithiasis? Kidney Stone. What risk increases the incidences for UTI’s in men over 50 y/o? Enlarged prostrate Cystitis refers to infection in the bladder UTI’s are most often caused by: Direct bacterial invasion of the lower urinary tract Women are at an increased risk for UTI D/T the opening of the urethra is close to the anus What group of people have the highest risk of UTI’s: Sexually active women Ways to prevent cystitis caused by infection: Flushing effects of voiding, low pH in urine, high urine osmolarity. Clinical manifestation: Dysuria, increase in voiding, odor, changes in the color and clarity of the urine. If left untreated it may lead to bacteremia, sepsis What is pyelonephritis? Inflammation of the kidneys. Occurs as a result of an ascending urinary tract infection. What is the clinic manifestation of pyelonephritis? Fever, flank pain, N/V, burning with urination, increase frequency and urgency. What are the two main conditions associated with kidney disease? High blood pressure and diabetes mellitus. Out of ALL the kidney disease, which one is caused by a genetic mutation? Polycystic kidney disease. Prerenal Kidney Injury- decrease blood flow and can also cause EXTREMELY low BP. Intrarenal (Intrinsic)- reaction to certain nephrotoxic medications or substances Postrenal-Kidney Injury- can cause obstruction of the ureter and the bladder; EX. Tumors,H, Nerve innervation disruption. What are the most common bacteria that are seen? E. Coli Who is at greater risk for postrenal acute kidney injury? An Elderly pt with hypertrophy of the prostrate. What is Glomerulonephritis? Inflammation of the glomeruli. Protein in the urine. What is the clinic manifestation of post-streptococcal glomerulonephritis? Dark Urine What is the clinic manifestation of glomerulonephritis? Proteinuria (Protein in the urine) If the patient was in the oliguric stage, the patient would have decreased in urine output. Hematuria- Blood in the urine. Bladder cancer-patient will have blood in the urine but no pain. What causes a post renal injury? Bilateral Kidney Stones A patient that is in end stage renal failure what medication would you give? Erythropoietin What might you see in the urine of a patient with kidney stones? Hematuria When would you call the provider quickly if the patient has a urethral colic? Fever and chills What would you tell a gentleman that has BPH? Weak Stream, nocturia, difficulty starting stream Patient presents with dull achy pain with a mass on the costovertebral angle what might it be? Renal Cancer Increase in pressure to intrabdominal muscles causes what kind of incontinence? Stress Incontinence What is a predisposed factor to bladder cancer? Exposure to chemicals and smoking. What type of incontinence is caused by neurological damage? Reflex Incontinence Why do men over 50 tend to develop UTIs? Prostatitis (E. coli) Who is at the highest risk of UTI? Sexually active Women Mechanisms of defense against urinary pathogens in men? Which does not defend ALKALINE urine Is urge incontinence a normal part of aging? NO What is the most common clinical manifestation of patients with cystitis? Dysuria Where is the urinary meatus located hypospadias? Under the penis If urinary meatus is located on top of the penis, what is called? Epispadias Main concern of HPV-Cervical Cancer What is the common organism that causes PID? Neisseria Gonorrhea If a newborn is born vaginal and is contaminated with chlamydia- Neonatal Conjunctive If a woman has cessation of her menstrual cycle, what is it called? Decrease in estrogen What causes syphilis? T-pallidum Female with extra hair, no period, and is unable to get pregnant what does she have? Polycystic Ovarian Syndrome What is the correct medical term if a part of the bladder prolapses into the vaginal canal? Cystocele A male patient has a tender prostate and painful to urinate what does he have? Prostatitis What if you have a pregnant lady who has hypertension, what are the symptoms? Weight gain and proteinuria A sexually active male has unilateral pain in the scrotum, its red, tender, and swollen what does he have? Epididymitis What if the head or glans of the penis is inflamed? Balanitis Which of the following is a medical emergency? Testicular torsion What causes diabetes insipidus? Insufficient ADH What is the most common form of hypothyroidism? Hashimoto’s Adrenocortical insufficiency such as Addison's disease is because there is an insufficient amount of what? Cortisol Out of the following which explains the etiology of dwarfism? Lack of growth hormone What is the name of the condition that is caused by a benign tumor of the adrenal medulla that secretes epinephrine and norepinephrine? Pheochromocytoma Hypercalcemia would occur in which of the following? Hyperparathyroidism What is the hormone that increases blood glucose to maintain homeostasis? Glucagon If a patient has a head injury and damaged the antidiuretic hormone-producing cell what would the diagnosis be? Diabetes Insipidus Which would cause hyperparathyroidism? Thyroid tumor For patients with type one diabetes that are under severe stress, what would you expect their blood sugar to be? Higher blood sugar Anterior pituitary gland releases which of these? Growth hormone, TSH, ACTH, LH, FSH, and prolactin. What is true acromegaly? Growth hormone secreting pituitary adenoma What would you see in someone who has myxedema? Non-pitting edema What is the name of the mechanism that controls hormone release and regulation? Negative feedback loop. Module 7 If a parent gave you information about their child and said they had irreversible brain damage that was caused before, during, and after birth, what condition do they have? Cerebral Palsy A patient comes in that was in an MVA and it is suspected that there is a spinal cord injury, we know which of the following maybe have caused this injury to occur? Twisting of the neck. Meningitis is inflammation of what? Meninges Risk factors for Meningitis include Nuchal rigidity, photopia, and headache What is the etiology of a CVA? Lack of blood flows to part of the brain. A patient is in an MVA, and we want to prevent more damage to the spinal cord, what is done to the patient? Stabilization is necessary to prevent further trauma to the spinal cord. How would you describe a TIA (Transient Ischemic Attach)? It is a temporary episode of cerebral ischemia, causing impaired neurologic functioning caused by inadequate blood flow to a portion of the brain. What is the difference between hemorrhagic strokes and Embolic strokes? Hemorrhagic strokes result in bleeding in or around the brain and it is the deadliest form of stroke. a-fib, rheumatic heart diagnosed, and valvular prosthetics are risk factors for Embolic stroke. How would you describe cerebral aneurysm? An out pouching or dilation of a portion of a blood vessel. If someone tells you that your patient is having a transient neurological event of paroxysmal abnormal, or excessive cortical discharges, what do you think is going on? Seizure Generalized seizure is caused by abnormal neuronal activity in both hemispheres of the brain. Atonic seizure is a sudden loss of muscle tone, lasting for seconds, and followed by postictal confusion. Generalized tonic-clonic Seizure is stiffening of the muscles of the arms and legs, F/B the immediate loss of consciousness, and jerking of all extremities. Autonomic Hyperreflexia is a sympathetic response that can cause HA, HTN, tachycardia, or bradycardia, diaphoresis, blurred vision, cold clammy skin, seizures, stroke, and death. Glasgow Coma Scale is used to determine a patient’s level of consciousness. Chronic Traumatic Encephalopathy is a type of damage caused by multiple mild TBI (Think Aaron Hernandez) An early symptoms of ALS muscle twitching. Module 8 The excruciating pain that radiates along the side of your face, is induced by chewing while eating. What disorder do you suspect? Trigeminal Neuralgia Clinical manifestations of Parkison’s disease? Muscle tremors, pill-rolling, postural abnormalities. What is often the cause of pulmonary embolism? Blood clot to lungs. What causes the appearance of the barrel chest in a patient with emphysema? Air trapped in the alveoli Which of the following will describe the pathophysiology of exercise induced asthma? Bronchospasm after exercise. Patient with tension pneumothorax and we need to do a needle thoracostomy and/or a chest tube placement. What is patho of that condition? A large accumulation of trapped air in a plural space affecting both the ones in the heart. How do people transmit TB to each other? Airborne droplets in inhaled to the lungs. Which patient do you think is at the highest risk for pneumonia? Someone who is hospitalized and is immunocompromised. Risk factors for respiratory disorder are bedrest, asthma, and smoking. What type of pneumonia causes a foreign substance such as food, saliva, liquid, or vomit that gets inside the lungs? Viral bacterial aspiration What condition is caused by the escape of air into the plural cavity? Pneumothorax How would you differentiate asthma from COPD? Asthma is reversible and COPD is irreversible. If you had someone with a pH of 7.3 and PCO2 of 55. What is the acid-base in balance? Respiratory acidosis. Which two diseases could result in COPD? Emphysema and Chronic Bronchitis Which mechanism in the lung paronychia allows pneumonia to develop? Inflammation What effect would hemoglobin amount (how many red blood cells you have) how would that affect oxygenation? Decreased hemoglobin decreases oxygen Which of the following activities is going to most likely trigger exercise-induced asthma? Running Which one accurately describes the pathophysiology of COPD? Inflammation leads to lung fibrosis and a loss of elasticity. Which is the most common cause of bacterial pneumonia? Streptococcus pneumonia What would you see in hypercapnia? Respiratory Acidosis How does severe hypoxia develop with pneumonia? Oxygen diffusion is impaired by congestion. Patient with acute respiratory failure what would you expect to find? Hypoxemia and hypercapnia. What would you expect to see of an elderly immunocompromised person? Severe hypoxemia (low oxygen) What would you expect to find in a person with asthma? Wheezing, coughing, and dyspnea. What would you expect from your patient that has COPD? Dyspnea on exertion. What would you expect from a patient with cystic fibrosis? Excessive mucous secretion. What would you expect to see from a patient hypo-ventilating? Increased CO2 Patient comes in with sudden shortness of breath, absent on the right side. What is it? Spontaneous pneumonia You walk into your patient's room, and they are in respiratory distress. The trachea deviates to the right side, what do you think they have? Attention pneumonia What is orthopnea? Difficulty breathing when lying down. What would you think of the signs and symptoms of epiglottis? Fever, sore throat, and drooling. You have a healthy patient that has pneumonia? What would you assess? Check respiratory rate. The immune system responds to the presence of allergen by causing which of the symptoms in intrinsic asthma? Broncho constriction Which of the following symptoms is NOT associated with acute bronchitis? Decrease mucous production What is associated with bronchiolitis? Thick tenacious mucus, wheezing, crackles, tachycardia. Which one is true of hypoventilation? The PaCo2 exceeds 45 What do you expect from an older client who is 40 years old and has a history of smoking, smokes 1 to 2 packs a day? Chronic bronchitis. If you had a patient who had laryngotracheobronchitis would they have? Hoarse voice and barking If you had a patient that is trying to compensate for metabolic acidosis, how would they compensate? Increase ventilation. Module 9 Hematopoiesis: is the process of blood formation Lymphocytes are produced in the lymph system (spleen, lymph nodes, and thymus) Monocytes are produced in the liver, spleen, lymp Erythropoiesis refers to hematopoiesis of the RBCs. The kidneys secrete a hormone called erythropoietin to increase RBS production There are 3 steps in the process that help the wound heal and stop bleeding. 1. Vasospasm 2. Platelet Plug 3. Coagulation. Vasospasm: Is a brief reflex in which the blood vessel narrows to decrease the blood flow to the injury and increase the blood pressure Platelet plug formation involves the activation, aggregation, and adherence of plts into a plug that serves as a barrier against blood flowing out of the vessel Coagulation or also known as Clotting- Changes liquid to a gel through a complex clotting cascade. Leukocytes: are a diverse group of cells that trigger the inflammatory process and combat infection(s) Leukocytosis: Describes an increase in WBCs and can indicate an infection Leukocytopenia: A decrease in WBCs, and can indicate an immune deficiency state (bone marrow suppression) What disease is known as Kissing disease? Mononucleosis “Mono” Lymphomas are cancer that develops from the lymphatic cells in the lymphatic system. What type of cancer has Reed Sternberg cells? Hodgkin’s Lymphoma Risk factors for non-Hodgkin's lymphoma: auto immune disorder, exposure to environmental irritants, history of solid organ transplants. NO household cleaning products or pesticides. Leukemia is a cancer of what? Leukocytes Acute lymphoblastic leukemia (ALL)-Most common (75% of all cases), affecting mostly children. Chronic myeloid leukemia (CML) Characterized by a malignant granulocyte that carry a unique chromosomal abnormality Clinical manifestations of leukemia? Weight loss, easy bruising, and recurrent infections. Cancer of the plasma cell that most often affects an older adult? Multiple Myeloma What can cause anemia? Decrease in the production of red blood cells? Yes. Hereditary causes? Yes. Increased red blood cell destruction? Yes. Increase in the clotting cascade? NO Manifestations of anemia are weakness, fatigue, pallor, syncope, dyspnea, and tachycardia. The goal in treating anemia? Improve tissue oxygenation. If you have iron-deficiency anemia. What would you see? Irritability in your patient, delayed healing, memory loss, NO geographical tongue. What type of anemia is caused by deficiency of vitamin B 12? Pernicious Anemia Pernicious anemia is characterized by? Large Macrocytic immature erythrocytes. Sign and symptoms of Aplastic Anemia? Pallor, Dyspnea, and Petechiae Pancytopenia is a lack of: Erythrocytes, leukocytes, and platelets Why are patients with leukemia at risk for infections? Nonfunctional immature leukocytes. Acute chest pain syndrome that is potentially life-threatening and presents with pain coughing and dyspnea and fever what disorder will you see that in? Sickle Cell The patient is experiencing a sickle cell crisis. What would you expect to see? Bone pain and dyspnea. Polycythemia is a disorder where the bone marrow produces too many erythrocytes (RBCs). Polycythemia Vera is caused by an overproduction of erythrocytes? True Thrombocytosis: increased platelets (this condition can cause thrombosis). Thrombocytopenia: decrease in platelets (can cause a risk of bleeding and infections). Hemophilia A is classic hemophilia and is caused by what factor? Factor VIII deficiency Hemophilia B is also known as Christmas hemophilia and is associated with what factor? Factor IX deficiency What type of inherited blood disorder causes a decrease in coagulation? Hemophilia Teaching patient about hemophilia and your patient says to you wow so I've been diagnosed with hemophilia I must've contracted that by using the same washcloth. What's your best response to that patient? This is a genetic mutation caused by X chromosome. A life-threatening condition that happens when tissue factor is exposed to blood? DIC Disseminated Intravascular Coagulation DIC can be a severe complication from sepsis//Complications that could cause DIC? Emphysema sepsis Characteristic of DIC is: Simultaneous clotting and bleeding Typical first signs of DIC (disseminated intravascular coagulation)? Petechiae on the skin and mucous membrane The patient has plastic anemia (one that needs a bone marrow transplant) what are the risks? Toxins, medications, autoimmune disorders. Bleeding Pt and platelets within the bloodstream start to aggregate to prevent further blood loss. What would you call that? Hemostasis tries to bring the body back to normal. Epstein Barr virus. What would you see? Malaysia, chills, sore throat, NOT nausea, and vomiting. Patient has Epstein-Barr virus and mononucleosis do you think they need further teaching if they say: I should be able to go play football in a couple of days. Clinical manifestations of anemia include all the following except which: Chest pain Clinical manifestation of ITP (immune thrombocytopenic purpura): produces a vesicular rash. Which condition is characterized by malignant granulocytes that carry a unique chromosome abnormality? Chronic myeloid leukemia Patient with Thrombocytopenia. What would you expect to see? A decreased platelet cell count. Patient has back pain, reduced bone density, he's got compression fractures of the vertebra, his serum calcium levels are elevated. What do you think he has? Myeloma Module 10 What causes Atherosclerotic plaque to form in the body? Injury to the epithelium What is not modifiable for people with hypertension? Age Risk factor for Hypertension? Smoking What is the cause of Cardiogenic shock? Myocardial Infarction When arterial blood pressure declines your kidneys secrete a hormone that increases your blood pressure and peripheral resistance. Renin What causes heart tissue damage or cardiac tissue damage when someone's having an MI? Blockage of oxygen? Which type of cardiomyopathy causes thickened hyperkinetic ventricle heart muscle? Hypertrophy What type of cardiomyopathy causes enlarged floppy ventricle heart muscles? Dilated Cardiac tamponade, a condition where there's a large amount of fluid that accumulates around the heart and it impedes what? Stretching and filling in the heart during diastole What condition is poorly understood because Weald or decades can go by between the exposure of the infectious agent and the development of symptoms? Myocarditis Chronic Inflammation and pericardium become thick and fibrous? Constrictive Pericarditis Loss of sympathetic tone in the smooth muscle of the arteries and veins secondary to the spinal cord damage which causes massive vasodilation causes what type of shot? Neurogenic Shock Endocarditis is an infection of what? Endocardium or heart valves Valve Stenosis results in the following alterations and blood flow through the heart. It's unable to flow easily out of the valves because the valves don't fully open. This condition is because fat-containing substances are deposited on the coronary artery lumens, and this causes the artery to narrow. Coronary Artery Disease What type of shock would occur after a severe MI? Cardio decline. Massive blood loss or dehydration what type of shock would you expect to see? Hypovolemic Pt diagnosed with hypertension and there is no identifiable cause. Primary Pt comes in with hypertension, they have chronic renal failure and diabetes. Secondary Pt has right sided heart failure. What would you see? Pulmonary edema? Pt has coronary artery disease. What would you see? Insufficient delivery of oxygen to the heart S/S of a Traditional pt coming in within an MI? Chest pain that radiates to the arm and the jaw. Stable Angina? Predictable and consistent pain that occurs on exertion and is relieved by rest and/or nitroglycerin. Unstable Angina? Chest pain that occurs while a person is at rest and not exerting. A common finding with forms of heart failure? Reduced cardiac output. What happens with septic shock? Decreased cardiac output. because they are overwhelmed by infection. Blood pressure drops. Not much cardiac output. Pt with BP 136/85. What stage hypertension do they have? Stage 1 Pt with BP 165/94. What stage hypertension do they have? Stage 2 Which of the following is a typical manifestation of decreased cardiac output? Fluid accumulation. Pt had an anaphylactic shock. What would you see? Insufficient delivery of oxygen to the heart. S/S of a Traditional pt coming in within an MI? Chest pain that radiates to the arm and the jaw. Pt has shock and an accumulation of lactic acid in the body. What would it cause? Tissue hypoxia. Chest pain with exertion? Angina pectoris. Pt has increased dyspnea (shortness of breath) and are feeling anxious, and they've noticed that their feet and ankles are swelling. What do you think they have? Congestive heart failure. Pt in ER bed is pale, cold, clammy, they have a rapid weak pulse, tachycardia, and they have an altered level of consciousness. What do you think is happening? Shock Pt in the hallway has a pulsating mass on his abdomen. What do you think his issue is? Aortic pulmonaria. Pt complains when it gets cold out, her fingers, hands, and feet become painful, sometimes numb, and sometimes they discolor. What is it? Rennard's. Proximal nocturia? Shortness of breath at night when laying down. Pt has a heart rate of 54. Bradycardic Which of the following can lead to impaired neurological function in a patient with increased intracranial pressure? Compression of the brain? Yes. Inflammation of the brain tissue? Yes. Decreased perfusion of the brain tissue? Yes, they're not getting enough oxygen; it absolutely can impair their neurological function. The ability of tissue to auto-regulate pressure. No. Pt in shock. Which of the following examples would you expect to be present? Expect them to have an altered level of consciousness? Yes. Hypotension? Yes. Increased mental clarity? No. Tachycardia? Yes. Hypertension? No. With left-sided heart failure. What would you expect to see? Jugular vein distension? No. Cough with frothy sputum? Yes. Hear crackles? Yes. Complaining of nocturnal dyspnea? Yes. True regarding syphilis? Caused by a spirochete's corkscrews. Can cause problems with cardiovascular and aortic necrosis. Can cause damage to the central nervous system and cause blindness paresthesia in mental deterioration. Patient shows up with cystitis. What would you expect to see? Dysuria or burning when you pee? Yes. urinary frequency? Yes. A fever? No. Pain in the super pubic area? Yes. Hypotension? No. Your patient is at risk for neutropenia. What could cause neutropenia? Chemo? Yes. Smoking? No. Excessive exercise? No. Congenital condition? Yes. Infection? No CHEMO & CONGENITAL CONDITIONS Clinical manifestations of pernicious anemia? Anorexia? Yes. Stomatitis? Yes. Paresthesia of the hands and feet? Yes. Pt comes in with DKA (diabetic ketoacidosis). Would they have low blood sugar? No. Would they have deep and fast respirations? Yes. They are blowing off lactic acid and CO2. Are they lethargic? Yes. Will they have an increase in energy? No For someone who has ARDS. What would you expect them to be? Hypoxic? Yes. Would they have changes to the AV diameter changes? Yes. Injury to the pulmonary circulation? Yes. Injury through the alveoli? Yes. Increase lung compliance? No Epicardium- Outer Protective Layer Myocardium- Muscular Middle Layer Endocardium- Thin Inner Layer