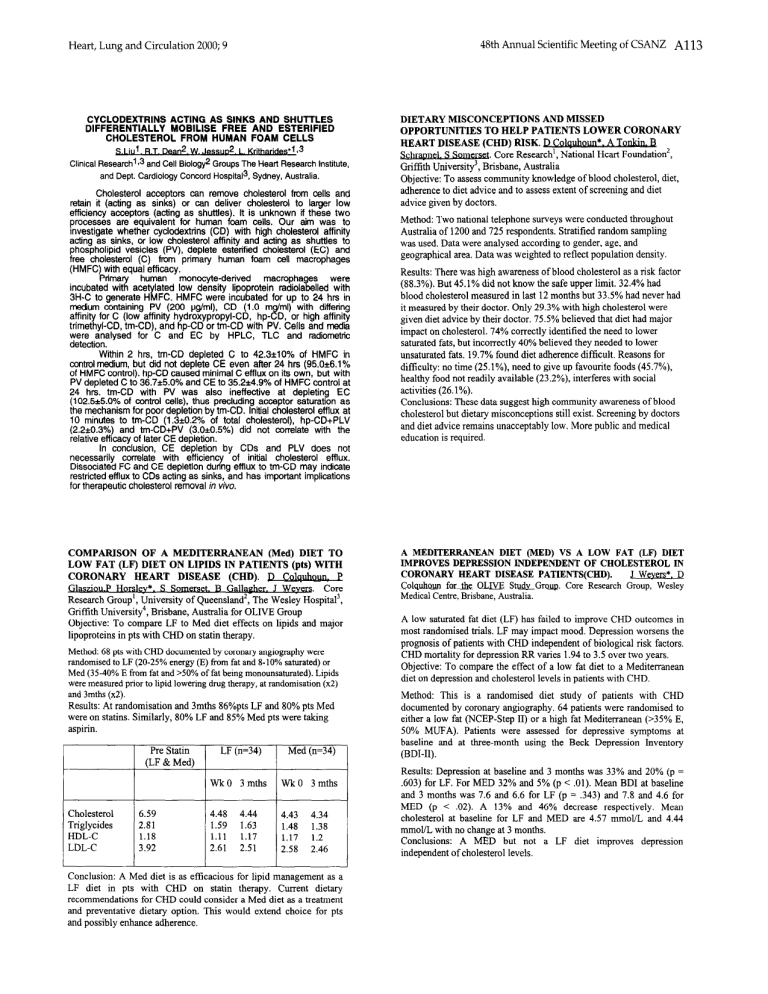
Heart, Lung and Circulation 48th Annual 2000; 9 CYCLODEXTRINS ACTING AS SINKS AND SHUTTLES DIFFERENTIALLY MOBILISE FREE AND ESTERIFIED CHOLESTEROL FROM HUMAN FOAM CELLS S LIU . R.T. Dean2. W. Jessuo2. L. Kritharides’l s3 Clinical Fteseaicii13 and Cell Biology2 Groups The Heart Research Institute, and Dept. Cardiology Concord Hospita13, Sydney, Australia. Cholesterol acceptors can remove cholesterol from cells and retain it (acting as sinks) or can deliver cholesterol to larger low efficiency acceptors (acting as shuttles). It is unknown if these two processes are equivalent for human foam cells. Our aim was to investigate whether cyclodextrfns (CD) with high cholesterol affinity acting as sinks, or low cholesterol affinity and acting as shuttles to phospholipid vesicles (PV), deplete esterified cholesterol (EC) and free cholesterol (C) from primary human foam cell macrophages (HMFC) with equal efficacy. Primary human monocyte-derived macropha es were incubated with acetylated low density lipoprotein radiola L lled with 3H-C to generate HMFC. HMFC were incubated for up to 24 hrs in medium containing PV (200 pg/ml), CD (1.0 m f ml) with diffenng :. affinity for C (low affinity hydroxypropyl-CD, hp- D, or hrgh afflnlty trimethyl-CD, tm-CD), and hp-CD or tm-CD with PV. Cells and media were analysed for C and EC by HPLC, TLC and radiometric detection. Within 2 hrs, tm-CD depleted C to 42.3*10% of HMFC in control medium, but did not deplete CE even after 24 hrs (95.0+6.1% of HMFC control). ho-CD caused minimal C efflux on its own. but with PV depleted C td 36.7*5.0% and CE to 35.2*4.9% of HMFC’control at 24 hrs. tm-CD with PV was also ineffective at depleting EC (102.5&.0% of control cells), thus precluding acceptor saturation as the mechanism for poor depletion by tm-CD. Initial cholesterol efflux at IO minutes to tm-CD (1.3*0.2% of total cholesterol), hp-CD+PLV (2.2&0.3%) and tm-CD+PV (3.&0.5%) did not correlate with the relative efficacy of later CE depletion. In conclusion, CE depletion by CDs and PLV does not necessarily correlate with efficiency of initial cholesterol efflux. Dissociated FC and CE depletion during efflux to tm-CD may indicate restricted efflux to CDs acting as sinks, and has important implications for therapeutic cholesterol removal in vivo. COMPARISON OF A MEDITERRANEAN @led) DIET TO LOW FAT (LF) DIET ON LIPIDS IN PATIENTS (pts) WITH CORONARY HEART DISEASE (CHD). D et. B Gallag-. Core Research Group’, University of Queensland’, The Wesley Hospita13, GriMith University4, Brisbane, Australia for OLIVE Group Objective: To comuare LF to Med diet effects on liuids and maior lipoproteins in pts with CHD on statin therapy. Method: 68 pts with CHD documented by coronary angiography were randomised to LF (20-25% energy (E) from fat and 8-10% saturated) or Med (35-40% E from fat and >50% of fat being monounsahuated). Lipids were measured prior to lipid lowering drug therapy, at randomisation (x2) and 3mths (x2). Results: At randomisation and 3mths 86%pts LF and 80% pts Med were on statins. Similarly, 80% LF and 85% Med pts were taking Pre Statin CLF & Med) 6.59 2.81 1.18 3.92 LF (n=34) Med (n=34) WkO 3 mths WkO 3 mths 4.48 1.59 4.44 1.63 1.11 2.61 1.17 2.51 4.43 1.48 1.17 2.58 4.34 1.38 1.2 2.46 Conclusion: A Med diet is as efficacious for lipid management as a LF diet in pts with CHD on statin therapy. Current dietary recommendations for CHD could consider a Med diet as a treatment and preventative dietary option. This would extend choice for pts and possibly enhance adherence. Scientific Meeting of CSANZ A113 DIETARY MISCONCEPTIONS AND MISSED OPPORTUNITIES TO HELP PATIENTS LOWER CORONARY HEART DISEASE (CHD) RISK. D_Colauholm * . A Tonkin. v. Core Research’, National Heart Foundation’, Griffith University3, Brisbane, Australia Objective: To assess community knowledge of blood cholesterol, diet, adherence to diet advice and to assess extent of screening and diet advice given by doctors. Method: Two national telephone surveys were conducted throughout Australia of 1200 and 725 respondents. Stratified random sampling was used. Data were analysed according to gender, age, and geographical area. Data was weighted to reflect population density. Results: There was high awareness of blood cholesterol as a risk factor (88.3%). But 45.1% did not know the safe upper limit. 32.4% had blood cholesterol measured in last 12 months but 33.5% had never had it measured by their doctor. Only 29.3% with high cholesterol were given diet advice by their doctor. 75.5% believed that diet had major impact on cholesterol. 74% correctly identified the need to lower saturated fats, but incorrectly 40% believed they needed to lower unsaturated fats. 19.7% found diet adherence difficult. Reasons for difficulty: no time (25.1%), need to give up favourite foods (45.7%), healthy food not readily available (23.2%), interferes with social activities (26.1%). Conclusions: These data suggest high community awareness of blood cholesterol but dietary misconceptions still exist. Screening by doctors and diet advice remains unacceptably low. More public and medical education is required. A MEDITERRANEAN DIET (MED) VS A LOW FAT (LF) DIET IMPROVES DEPRESSION INDEPENDENT OF CHOLESTEROL IN CORONARY HEART DISEASE PATIENTS(CHD). ,I Weyers*. D Core Research Group, Wesley Medical Centre, Brisbane, Australia. A low saturated fat diet (LF) has failed to improve CHD outcomes in most randomised trials. LF may impact mood. Depression worsens the prognosis of patients with CHD independent of biological risk factors. CHD mortality for depression RR varies 1.94 to 3.5 over two years. Objective: To compare the effect of a low fat diet to a Mediterranean diet on depression and cholesterol levels in patients with CHD. Method: This is a randomised diet study of patients with CHD documented by coronary angiography. 64 patients were randomised to either a low fat (NCEP-Step II) or a high fat Mediterranean (~35% E, 50% MUFA). Patients were assessed for depressive symptoms at baseline and at three-month using the Beck Depression Inventory (BDI-II). Results: Depression at baseline and 3 months was 33% and 20% (p = ,603) for LF. For MED 32% and 5% (p < .Ol). Mean BDI at baseline and 3 months was 7.6 and 6.6 for LF (p = ,343) and 7.8 and 4.6 for MED (p < .02). A 13% and 46% decrease respectively. Mean cholesterol at baseline for LF and MED are 4.57 mmol/L and 4.44 mmoVL with no change at 3 months. Conclusions: A MED but not a LF diet improves depression independent of cholesterol levels.