Body Temperature & Thermoregulation: Physiology & Control
advertisement

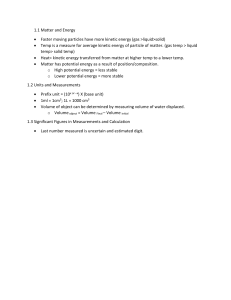
NLOA LT1 CHAPTER 30: Vital Signs BODY TEMPERATURE/THERMOREGULATION PHYSIOLOGY - Body Temperature: difference between the amount of heat produced and the amount of heat lost - Core temp: temperature of the deep tissues o Despite extremes in environmental conditions, the temp control mechanisms of humans keep the body’s core temp constant - Average body temp: 36-38C (96.8-100.4F), but no single temp is normal for all people. - Healthy young adults: average oral temp is 37C (98.6F) - Elderly: average core temp ranges from 35C to 36.1C (95-97F) - Lowest body temperature: 6AM - Highest body temperature: 4PM Body Temperature Regulation - Thermoregulation: balance between heat lost and heat produced - Neural and vascular control o Hypothalamus: controls body temperature o Anterior hypothalamus – controls heat loss Mechanisms of heat loss include sweating, vasodilation, and inhibition of heat production o Posterior hypothalamus – controls heat production Heat-conserving mechanisms include vasoconstriction. When vasoconstriction is ineffective, shivering begins. o Disease or trauma to the hypothalamus or the spinal cord causes serious alterations in temp control Heat Production - Temp regulation depends on the normal heat production processes. - Heat produced by the body is a by-product off metabolism. - As metabolism increases, additional heat is produced and when it decreases, less heat is lost. - Heat production occurs during rest, voluntary movements, involuntary shivering, and non shivering thermogenesis. - Basal metabolism o Defn: Heat produced by the body at absolute rest Average basal metabolic rate (BMR) depends on the body’s surface area o Thyroid hormones and testosterone also affect the BMR by increasing it. - Voluntary movements o Metabolic rate increases during activity, sometimes causing heat production to increase up to 50x normal. - Shivering o Defn: an involuntary body response to temp differences in the body. o The skeletal muscle movement during shivering requires significant energy. o Shivering sometimes increases heat production 4-5x greater than normal. - No shivering thermogenesis o Occurs in neonates. o Because they cannot shiver, a limited amount of vascular brown tissue present at birth is metabolized for heat production. Heat Loss - Heat loss and heat production occur simultaneously. - Radiation o Defn: the transfer of heat from the surface of one object to another without direct contact between the two. o 85% of the surface area of the human body radiates heat to the environment. o Radiation increases as the temp difference between the object increases. o Radiation heat loss happens during surgery when the pt’s skin is exposed to cool environment. o If the environment is warmer, the body absorbs heat thru radiation. o The pt’s position enhances radiation loss (e.g. standing – exposes greater radiating surface area, lying in a fetal position – minimizes heat radiation). o Nsg interventions: Help promote heat loss - Removing clothing or blankets Help decrease the amount of heat lost from radiation Cover the body with dark, closely woven clothing - Conduction o Defn: transfer of heat from one object to another with direct contact. o ♡ Ishbel 2. Person’s ability to sense feeling comfortable or uncomfortable, 3. Thought process or emotions, and 4. Person’s mobility or ability to remove or add clothes o o - - - It normally accounts for a small amount of heat loss. The body gains heat by conduction when it makes contact with materials warmer than skin temp. o Nsg interventions: Increase conductive heat loss – applying ice pack or bathe the pt with a cool cloth Reduce conductive loss – apply several layers of clothing Convection o Defn: transfer of heat away by air movement. o A fan promotes heat loss thru convection o The rate of heat loss increases when moistened skin comes into contact with slightly moving air. Evaporation o Defn: transfer of heat energy when a liquid is changed to gas. o The body continuously loses heat by evaporation. o Approx. 600-900ml a day evaporates from the skin and lungs, resulting in water and heat loss. Diaphoresis o Defn: visible perspiration primarily occurring on the forehead and upper thorax, although you can see it in other places on the body. o Excessive evaporation causes skin scaling and itching and drying of the nares and pharynx. Skin in Temperature Regulation - The skin regulates thru insulation of the body, vasoconstriction, and temperature sensation. - The skin, subcutaneous tissue, and fat keep heat inside the body. - People with more fat have more natural insulation than slim and muscular people. - The degree of vasoconstriction determines the amount of blood flow and heat loss to the skin. - If the core temp is too high, the anterior hypothalamus inhibits vasoconstriction and initiates vasodilation. If core temp is too low, the posterior hypothalamus initiates vasoconstriction. Behavioral control - The ability of a person to control body temp depends on: 1. Degree of temperature extreme, FACTORS AFFECTING BODY TEMPERATURE Age - An infant’s temperature greatly responds to changes in the environment. A newborn loses up to 30% of body heat through the head. Average newborn body temp: 35.5-37.5C (95.9-99.5F). Nsg interventions: Provide adequate clothing and avoid exposing infants to temperature extremes. Temp regulation is unstable until children reach puberty. The usual temp range gradually drops as people approach older adulthood. Average older adult body temp: 35-36.1C (95-97F). Older adults are more sensitive to temp extremes because of deterioration of control mechanisms (e.g. poor vasomotor control, reduced amounts of subcutaneous tissue, reduces sweat gland activity, & reduced metabolism). Exercise - Any form on exercise increases metabolism and heat production and thus body temp. - Prolonged strenuous exercise raises body temp. Hormone level - Women experience greater fluctuations in body temp than men. - The menstrual cycle causes body temp fluctuations due to hormonal variations such as the rise and fall of progesterone levels. Circadian Rhythm Body temp normally changes 0.5 to 1C (0.9-1.8F). Stress - Physical and emotional stress increase body temp thru hormonal and neural stimulation. - A pt who is anxious often has a higher normal temp Environment ♡ Ishbel - When pt is placed in a warm environment, he may be unable to regulate body temp by heat-loss mechanisms & the body temp increases. When pt is placed in a cold environment without warm clothing, body temp is low d/t extensive radiant and conductive heat loss. Affects infants and older adults more often because their temp-regulating mechanisms are less efficient. Temperature Alterations - Changes in body temp outside the usual range are r/t excessive production, excessive heat loss, minimal heat production, minimal heat loss, or any combination of these alterations - Fever/Pyrexia o Occurs because heat-loss mechanisms are unable to keep pace with excessive heat production resulting in an abnormal rise in body temp. o Not harmful if temp stay below 39C in adults or below 40C in children. o Pyrogens such as bacteria and viruses elevate body temp o Phases of a fever: Chill phase pt experiences chills, shivers, and feels cold Resolves when the new set point (higher temp) is achieved Plateau phase chills subsides, pt feels warm & dry Febrile skin becomes warm & flushed d/t vasodilation Diaphoresis assists in evaporative heat loss When the fever “breaks”, the pt becomes afebrile o Fever patterns: Sustained: a constant body temp continuously above 38C that has little fluctuation. Intermittent: fever spikes interspersed with usual temp levels (temp returns to acceptable value atleast once in 24hrs). Remittent: fever spikes and falls without a return to acceptable temp levels. - - Relapsing: periods of febrile episodes and period with acceptable temp values (febrile eps & periods of normothermia are often longer than 24hrs). o Fever of Undetermined cause (FUO) o If the body cannot meet the demand for additional O2, cellular hypoxia occurs. o Myocardial hypoxia causes angina, cerebral hypoxia produces confusion. o Dehydration is a serious problem for older adults & children with low body weight. o Interventions: O2 therapy Maintain optimum fluid volume status Hyperthermia o Defn: an elevated body temp related to the inability of the body to promote heat loss or reduce heat production o Any disease or trauma to the hypothalamus impairs heat-loss mechanisms o Malignant hyperthermia – a hereditary condition of uncontrolled heat production that occurs when susceptible people receive certain anesthetic drugs. Heatstroke o Defn: body temp of 40C or more o Heat depresses hypothalamus function o It is a dangerous heat emergency with a high mortality rate o Pts at risk: very young & very old; have cardiovascular disease, hypothyroidism, diabetes, or alcoholism; people who take medications that decrease the body’s ability to lose heat (e.g. phenothiazines, anticholinergics, diuretics, amphetamines, betaadrenergic receptor antagonists); people who exercise/work strenuously. o S/sx: Hot, dry skin; giddiness; confusion; delirium; excess thirst; nausea; muscle cramps; visual disturbances; incontinence. V/S shows body temp sometimes > 45C, increased HR, lower BP Severe heatstroke: pt becomes unconscious, with fixed, nonreactive pupils. ♡ Ishbel - - Permanent neurological damage occurs unless cooling measures are rapidly started. Heat exhaustion o Occurs when profuse diaphoresis results in excess water & electrolyte loss o Caused by environmental heat exposure o Pt shows s/sx of deficient fluid volume o First-aid mgt: Transporting pt to a cooler environment Restricting fluid & electrolyte balance Hypothermia o Caused by heat loss during prolonged exposure to cold, which overwhelms the body’s ability to produce heat. o Classifications: Mild – 34 to 36C Moderate – 30 to 34C Severe - <30C o It is sometimes unintentional (falling into a frozen lake), but sometimes induced (during surgical/emergency procedures). o S/sx: uncontrolled shivering; loss of memory; depression; poor judgement; HR, RR, & BP fall; skin becomes cyanotic; cardiac dysrhythmias, loss of consciousness, unresponsive ness to painful stimuli. o S/sx of severe hypothermia: similar to those of death (e.g. lack of stimuli & extremely slow RR & PR). o Ax of core temp is critical. o Frostbite: occurs when the body is exposed to subnormal temps Areas susceptible to frostbite are the earlobes, tip of the nose, fingers & toes. S/sx: white, waxy, & firm to the touch; pt loses sensation in the affected area Interventions: gradual warming measures, analgesia, protection of the injured tissue. ASSESSMENT - When possible, select the temp site preferred by the pt. - Include the pt’s preferences when selecting non pharmacological interventions for hyperthermia (e.g. cooling blankets, tepid baths, etc.) - - Sites: o Core & surface body temp ICU: pulmonary artery, esophagus, & urinary bladder o Axillary temp Not recommended in adults because they are inaccurate & poorly reflect core temp. However, they are reliable as rectal temp measurement in infants. o Oral, rectal, & skin temp Rely on effective blood circulation @ the measurement site. o Tympanic temp Relies on the radiation of body heat to an infrared sensor. o The temp varies depending on the site used, but it is usually between 36 – 38C. o Rectal temp is usually 0.5C higher than oral temp o If possible, use the same site when repeated measurements are necessary. Thermometers: o Electronic Thermometers Provides 2 modes of operation: a 4-second predictive temp & a 3-minute standard temp. Forms: Tympanic temp - an otoscope-like speculum with infrared sensor tip; it detects heat from the tympanic membrane Superficial temporal artery temp – a handheld scanner with infrared sensor tip; detects temp of cutaneous blood flow by sweeping the sensor across the forehead & just behind the ear. Greatest advantage of electronic thermometers: Readings appear within seconds & are easy to read. o Disposable Thermometers Readily available for use in the home setting. Are useful for temp screening but are not as accurate as non disposable electronic thermometers. o Chemical Dot Thermometers Single-use or reusable ♡ Ishbel Thin strips of plastic with temperature sensor at one end. Celsius ver: 50 dots, each dot represents a temp increment of 0.1C, over a range of 35.5 - 40.4C. Fahrenheit ver: 45 dots with increments of 0.2F & a range of 96 – 104.8F Chemical dots on the thermometer change color to reflect temp reading, usually 60 seconds. Are usually for oral temps. Can also be used for rectal temps when covered by a plastic sheath & placed for 3mins. Useful for screening temps especially in infants, young children, & intubated pts. - Convert Celsius to Fahrenheit C = (F - 32) x 5/9 Example: 40C = (104F – 32) x 5/9 Convert Fahrenheit to Celsius F = (9/5 x C) + 32 Example: 104F = (9/5 x 40C) +32 - NSG DIAGNOSIS - Risk for imbalanced body temp - Hyperthermia - Hypothermia - Ineffective thermoregulation - Risk for hypothermia IMPLEMENTATION Health Promotion - Teach pts to avoid strenuous exercise in hot, humid weather; Drink fluids such as water or clear fruity juices before, during, & after exercise; Wear light, loose-fitting, light-colored clothes - Teach pts to avoid exercising in areas with poor ventilation, weary a protective covering over the head when outdoors, & expose themselves to hot climates gradually. Fever - The choice of interventions depends on the cause; adverse effects & the strength, intensity, and duration of the temp elevation. - - - If caused by pyrogens: isolate the causative pyrogen o obtain culture specimens (e.g. urine, blood, sputum, & wound sites) o Administer antibiotic medications ordered If caused by a viral origin (common in children): o Children between 6 mos & 3 yrs are prone to dehydration & febrile seizures during the rising of temp o Children have a risk for fluid volume deficit because they can quickly lose large amounts of fluids in proportion to their body weight. o Nsg Interventions: Maintain accurate I/O records Weigh the pt daily Encourage fluids Provide regular mouth/oral care If fever is caused by a hypersensitivity response to a drug: o Treatment: Withdrawing the medication Treating any skin integrity impairment Educating pt & family about the allergy Medication of choice: Antipyretics o Acetaminophen & NSAIDs (ibuprofen, salicylate, indomethacin) Corticosteroids: reduces heat production by interfering with the hypothalamic response o Pts taking steroids need to be monitored closely especially if they have a risk for infection bc steroids mask the s/sx of infection. Meperidine or butorphanol: reduces shivering Nonpharmalogical mgt: o TBS, bathing with alcohol-water solns, applying ice packs to axillary & groin areas, cooling fans — avoid these because they lead to shivering (according sa book) o Blankets cooled by water – placing a bath blanket between the pt and hypothermia blanket & wrapping distal extremities reduces the risk of injury to the skin & tissues. o Wrap pt’s extremities – reduces incidence & intensity of shivering Heatstroke - Emergency situation - First-aid: o moving pt to a cooler environment ♡ Ishbel - o removing excess body clothing o placing cool, wet towels over the skin o using oscillating fans Emergency treatment: o IV fluids o irrigating the stomach lower bowel with cool solns o hypothermia blankets - Hypothermia - priority treatment: prevent a further decrease in body temp - Removing wet clothes & replacing them with dry ones - Wrapping pts in blankets - Emergency away from a health care setting: o Have pt lie under blankets next to a warm person o If pt is conscious: offer hot liquids such as soup and avoid alcohol & caffeinated drinks o Keep head covered o Place pt near a fire or a warm room, or place heating pads next to areas of the body that lose heat the quickest. Restorative & Continuing Care - Educate pt about the importance of taking & continuing any antibiotics as directed until the course of treatment is completed. - Especially for children & older adults: identify preferred fluids and encouraging oral fluid intake - Radial & Apical: most common site for PR assessment. Use radial pulse to teach pts how to monitor their own HRs. Assess the apical pulse if: o If the radial pulse is abnormal or intermittent resulting from dysrhythmias or if it is inaccessible d/t a cast or dressing. o When a pt takes meds that affect the HR – it provides more accurate assessment of heart function. Best site for infants or younger children: brachial & apical CHARACTER OF THE PULSE - Radial pulse: measure the rate, rhythm, strength, & equality - Apical pulse: assess rate & rhythm Rate - - Before measuring a pulse, review the pt’s baseline rate Age Heart Rate (bpm) Infant 120-160 Toddler 90-140 Preschooler 80-110 School-age child 75-100 Adolescent 60-90 Adult 60-100 Positions: sitting, standing, & lying When assessing the pulse, consider the ff factors that influence the PR: PULSE The palpable bounding of blood flow in a peripheral artery. The pulse is an indirect indicator of circulatory status. PHYSIOLOGY & REGULATION - Cardiac output: the volume of blood pumped by the heart during 1 min, it is the product of HR & SV of the ventricle. - An adult heart pumps 5000 mL of blood/min ASSESSMENT OF PULSE - Carotid site: recommended for quickly finding & assessing the pulse. ♡ Ishbel - Identify the first & second heart sounds o S1: low pitched and dull; “lub” o S2: higher pitchers & shorter; “dub” - Two common abnormalities in PR: o Tachycardia: abnormally elevated HR (>100 bpm) o Bradycardia: slow rate (<60 bpm) - Pulse deficit: the difference between the apical & radial pulse o an inefficient contraction of the heart that fails to transmit a pulse wave to the peripheral pulse site creates a pulse deficit. Rhythm Normally there is an interval between each pulse or heartbeat. - Dysrhythmias or abnormal rhythm: an interval interrupted by an early/late beat or a missed beat o It threatens the ability of the heart to provide adequate cardiac output, particularly if it occurs repetitively. o Assessing for dysrhythmias: palpate an interruption in successive pulse waves or auscultating an interruption between heart sounds. o Documentation: ECG: records electrical activity of the heart for a 12-sec interval. Holter monitor: records and stores 24hrs of electrical activity. Telemetry monitor: continuous observation of the heart rhythm during all of the patient’s daily activities. Strength - Depends on the volume of blood ejected against the arterial wall with each heart contraction & the condition of the arterial vascular system leading to the pulse site. - Documenting pulse strength: o Bounding (4) o Full or strong (3) o Normal and expected (2) o Diminished or barely palpable (1) o Absent (0) Equality - Assess all symmetrical pulses simultaneously except for the carotid pulse because excessive pressure occluded blood supply to the brain. NSG DIAGNOSIS (interventions depends on the diagnosis of the pt) - Activity intolerance - Anxiety - Decreased cardiac output - Deficient fluid volume - Impaired gas exchange - Acute pain - Ineffective peripheral tissue perfusion BLOOD PRESSURE - The force exerted on the walls of the artery by the pulsing blood under pressure from the heart. Systematic or arterial BP: BP in the system of arteries in the body o Is a good indicator of cardiovascular health Systolic pressure: peak of maximum pressure when ejection occurs Diastolic pressure: the minimal pressure exerted against the arterial walls at all times. Standard unit for measuring BP: mercury (mmHg) Pulse pressure: difference between systolic & diastolic BP PHYSIOLOGY Cardiac Output - Increased cardiac output: more blood is pumped against the arterial walls, causing the BP to rise o Sx: Increase in HR, greater heart muscle contractability, or an increase in blood volume - A rapid or significant increase in HR decreases the filling time of the heart, resulting to decreased BP. Peripheral Resistance - The size of arteries & arterioles changes to adjust blood flow to the needs of the local tissues. - Ex: when the heart needs more blood, the peripheral arteries constrict decreasing their supply of blood. More blood becomes available to the heart bc of resistance change in the periphery. ♡ Ishbel - Normal arteries & arterioles remain partially constricted to maintain constant flow of blood. Peripheral vascular resistance: the resistance to blood flow determined by the tone of vascular musculature & diameter of blood vessels. Rising resistance: BP rises; vessels dilate: BP drops Blood Volume - Most adults have a circulating blood volume of 5000 mL. Normally this stays constant. - Increase in volume: exerts more pressure against arterial walls - Ex: rapid, uncontrolled infusion of IV fluids elevates BP; when a pt’s circulating blood volume falls (e.g. hemorrhage or dehydration), BP drops. Viscosity - When hematocrit rises & blood flow slows: arterial BP increases Elasticity - Increasing pressure in the arteries: diameter of vessel walls increases to accommodate pressure change. - Arterial distensibility prevents wide fluctuations in BP - In some diseases such as arterioscleroses, the vessel wall loses its elasticity & results in greater resistance to blood flow. FACTORS INFLUENCING BP Age Average Optimal BP for Age Classification BP (mmHg) Newborn 1 month 1 year 6 yrs 40 (mean) 85/54 95/65 105/65 7 yrs 10-13 yrs 14-17 yrs 18 yrs & older 87 to 117/48 to 64 110/65 119/75 <120/<80 Category Systolic (mmHg) Normal Prehypertension Stage hypertension Stage hypertension Diastolic (mmHg) <80 80-89 1 <120 120-139 or >140 or >90 2 >160 or >90 Stress - Anxiety, fear, pain, & emotional stress result in sympathetic stimulation, which increases HR, cardiac output, & vascular resistance. It’s effect increases BP. - Anxiety raises BP up to 30 mmHg. Ethnicity - African-Americans are have a higher risk for severe hypertension at an earlier age & have twice the complications such as stroke & heart attack. Gender - After puberty, males tend to have higher BP readings - Menopause women have higher BP levels than men of similar age. Daily Variation - When the pt sleeps (Between midnight & 3AM): lower BP - Between 3AM & 6AM: slow & steady rise in BP - When pt awakens: early-morning surge - Between 10AM & 6PM: highest BP of the day Medications Classification for BP for Adults Ages 18 & Older ♡ Ishbel o Activity & Weight - A period of exercise can reduce BP for several hrs afterwards. - Inadequate exercise contributes to weight gain, & obesity is a risk factor of hypertension. Smoking - It results to vasoconstriction. - BP rises when a person smokes & returns to baseline about 15mins after stopping smoking. HYPERTENSION - The most common alteration in BP. - Are often asymptomatic - Diastolic: >90 mmHg; Systolic: >140 mmHg - Associated with loss of elasticity in the arterial walls. - People with fam hx of hypertension are at significant risk - Modifiable risk factors: o Obesity o Cigarette smoking o Heavy alcohol consumption o High sodium intake o Sedentary lifestyle o Continued exposure to stress o Diabetes o Age o African-americans - Nsg Interventions for pts diagnosed with hypertension: o Educate pt about BP values, long-term follow-up care & therapy The usual lack of sx (that it cannot be felt) Ability of therapy to control but not cure it Consistently followed treatment plan that ensures a relatively normal lifestyle. HYPOTENSION - Systolic: <90 mmHg - Occurs bc of the dilation of the arteries in the vascular bed, the loss of substantial amount of blood vol., or the failure of the heart muscle to pump blood adequately. - Sx of pallor, skin mottling, clamminess, confusion, increased HR, or decreased urine output is life threatening & to be reported to the HC provider immediately. - Orthostatic hypotension/ Postural hypotension: when a normotensive person develops sx & a drop in systolic BP by atleast 20mmHg or a drop in diastolic pressure by atleast 20mmHg within 3mins of rising to an upright position. o Risk factors: pts who are dehydrated, anemic, or have experienced prolonged bed rest or recent blood loss o Ax: obtain BP and pulse in sequence with the pt supine, sitting, & standing. Obtain readings within 3mins after pt changes position. Observe for fainting, weakness, blurred vision, or lightheadedness. o Orthostatic hypotension is a risk factor for falls, especially among elderly pts. MEASUREMENT OF BP BP Equipment - Sphygmomanometer: includes a pressure manometer, an occlusive cuff that encloses and inflatable rubber bladder, & a pressure bulb with a release valve that inflates the bladder. - Aneroid manometer: has a glass-enclosed circular gauge containing a needle that registers mm calibrations. Before using, make sure that the ♡ Ishbel needle point to zero & is correctly calibrated. It requires calibration every 6 mos. - Occlusive cuff: comes in different sizes; ideally the width of the cuff is 40% of the circumference of the midpoint of the limb. The inflatable bladder encircles atleast 80% of the upper arm in adults & the entire arm in children. Auscultation - For best results, do this in a quiet room & comfortable temp. - The pts position during BP taking should be the same during each measurement. - Before taking BP: control factors responsible for high readings (e.g. anxiety, pain, exertion) - During initial ax: obtain & record BP in both arms. - During subsequent ax: measure BP in the arm with the higher pressure. Pressure differences greater than 10mmHg indicate vascular problems. - Korotkoff (1905): o 1st sound – onset of systolic pressure: clear rhythmical tapping; PR is gradually increasing in intensity o 2nd sound – a blowing or swishing sound o 3rd sound – crisper & more intense tapping o 4th sound – muffled & low pitched; is the diastolic pressure for children o 5th sound – diastolic pressure (adolescents & adults): disappearance of the sound Ax in Children - Children 3yo & above need to have their BP checked annually. - Readings are difficult to obtain in restless or anxious infants & children. o Allow atleast 15mins for them to recover from recent activities o Different arm size requires careful & appropriate cuff size. o The child’s cooperation is increased If a parent have prepared him/her for the usual sensation of the BP cuff (ex: “tight hug on your arm”). o Do not press stethoscope too firmly on the antecubital fossa to prevent errors in auscultation. Sounds are difficult to hear in children bc of low frequency & amplitude. Use a pediatric bell if necessary. Ultrasonic Stethoscope - When unable to auscultate sounds d/t weakened arterial pulse, use an ultrasonic stet. - It allows you to hear low-frequency systolic sounds. - It is frequently used in measuring BP of infants & children and low BP in adults. Palpation - Useful for pts whose arterial pulsations are too weak to create sounds. - Can be used along with auscultation. Lower-extremity BP - Used if pt has dressings, casts, IV catheters, or AV fistulas or shunts in the upper extremities - Site for auscultation: popliteal artery - Best position: prone; if impossible, ask pt to flex the knee slightly for easier access to the artery. - The systolic pressure in the legs is usually higher by 10-40mmHg than the brachial artery, but the diastolic pressure stays the same. Electronic BP Devices - Rely on electronic sensor to detect the vibrations caused by the rush of blood through an artery. - Is used for pts who are critically ill or unstable, during or after procedures, or when therapies require frequent monitoring. - Pt conditions not appropriate for electronic BP mgt: o Irregular HR o Peripheral vascular obstruction o Shivering o Seizures o Excessive tremors o Inability to cooperate o BP <90 mmHg systolic o Experienced trauma - Advantages: o Ease of use & efficiency when repeated or frequent measurements are indicated. Self-measurement of BP - Aneroid sphygmomanometer & electronic digital readout devices that do not require stet. Benefits: o Elevated BP is detected previously unaware of the problem ♡ Ishbel o - - People with prehypertension provide information about the pattern of Bp values to their HC provider. o Pts with hypertension adhere to their treatment through selfmonitoring. Disadvantages: o Improper use of the device o Risk of inaccurate readings o Some pts get alarmed with one elevated reading or get overly conscious and inappropriately self-adjust meds. Nsg interventions: o Advice pts of possible inaccuracies in the BP devices o help them understand the meaning & implications of readings o Teach them proper measurement techniques. o Encourage them to record the date of their BP readings NSG DIAGNOSIS (interventions depends on the diagnosis of the pt) - Activity intolerance - Anxiety - Decreased cardiac output - Deficient/excess fluid volume - Risk for injury - Acute pain - Ineffective peripheral tissue perfusion ♡ Ishbel