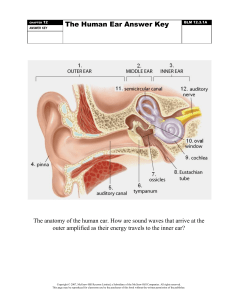
What is the main function of the ear? Your ears have two main functions: hearing and balance. • Hearing: ➢ When sound waves enter ear canal, tympanic membrane (eardrum) vibrates. ➢ This vibration passes on to three tiny bones (ossicles) in middle ear. The ossicles amplify and transmit these sound waves to the inner ear. ➢ Once the sound waves reach inner ear, tiny hair cells called stereocilia transform the vibrations into electrical energy and send it along nerve fibers to brain. What is the main function of the ear? • Balance: ➢ Inner ear contains semicircular canals filled with fluid and hair-like sensors. ➢When move head, the fluid inside these loop-shaped canals sloshes around and moves the hairs. ➢The hairs transmit this information along the vestibular nerve to brain. ➢Finally, brain sends signals to muscles to help stay balanced. What are the parts of the ear? • The three main parts of ear include ➢ the outer ear, ➢ middle ear ➢ inner ear. • tympanic membrane (eardrum) separates outer ear and middle ear. Middle ear ➢ Middle ear begins on the other side of tympanic membrane (eardrum). ➢ There are three tiny bones in this area — the malleus, incus and stapes. (ossicles) ➢ They transfer sound vibrations from eardrum to inner ear. ➢ Middle ears also house the eustachian tubes, which help equalize the air pressure in the ears. Otitis media ➢ Otitis media is the most common disease of the middle ear. Otitis media is a general term for inflammation of the middle ear, mastoid, and eustachian tube. ➢ Inflammation of the nasopharynx causes most cases of otitis media. As inflammation occurs, the nasopharyngeal mucosa becomes edematous and discharge is produced. ➢When fluid, pus, or air builds up in the middle ear, the eustachian tube becomes blocked, and this impairs middle ear ventilation. Types of otitis media There are several types of otitis media in which inflammation can occur alone, with infective drainage, or with noninfective drainage. Types of otitis media The first type of otitis media is otitis media without effusion. This is an inflammation of the middle ear mucosa without drainage. Types of otitis media The second type of otitis media occurs when there is a bacterial infection of the middle ear mucosa. This is called acute otitis media, suppurative otitis media, or purulent otitis media. The infected fluid becomes trapped in the middle ear. If the infection continues longer than 3 months, chronic otitis media results. Types of otitis media The third type of otitis media is otitis media with effusion. Other names include serous otitis media, nonsuppurative otitis media, and glue ear. With this type of otitis media, noninfective fluid accumulates within the middle ear. SIGNS AND SYMPTOMS • Acute otitis media commonly follows an upper respiratory infection. • A fever, earache, and feeling of fullness in the affected ear are common symptoms. • As purulent drainage forms, pain and, conductive hearing loss occur. SIGNS AND SYMPTOMS •Nausea and vomiting may also be present. • Purulent drainage may be evident in the external ear canal if the tympanic membrane ruptures. • Mastoid tenderness indicates that the infection may have spread to the mastoid area. SIGNS AND SYMPTOMS • Otoscopic examination reveals a reddened, bulging tympanic membrane. • Symptoms of otitis media with effusion may go undetected in adults because there are no signs of infection. • The patient may report fullness, bubbling, or crackling in the ear. The patient may have a slight conductive hearing loss or allergies or be a mouth breather. COMPLICATIONS • A perforation may occur with an acute or chronic infection. • Buildup of fluid and pressure in the middle ear can cause a spontaneous perforation of the tympanic membrane. • The patient usually experiences pain before the rupture and relief of pain after the rupture. • The fluid in the middle ear moves through the perforation into the ear canal, relieving the pressure and pain. • A tympanic membrane perforation causes hearing loss. The location and size of the perforation determine the extent of hearing loss. COMPLICATIONS • Cholesteatoma • Repeated infections in the middle ear or mastoid can cause a cholesteatoma, which is an epithelial cystlike sac that fills with debris such as degenerated skin and sebaceous material. The cholesteatoma starts in the external ear canal and spreads to the middle ear through a perforation in the tympanic membrane. Damage occurs in the middle ear structures as a result of pressure necrosis. Cholesteatoma causes conductive hearing loss. As the disease progresses, facial paralysis and vertigo may occur. COMPLICATIONS •Tympanosclerosis is another complication of repeated middle ear infections. •Tympanosclerosis consists of deposits of collagen and calcium on the tympanic membrane. •The condition can slowly progress over time to the area around the middle ear ossicles. •These deposits appear as chalky white plaques on the tympanic membrane and contribute to conductive hearing loss. COMPLICATIONS •Mastoiditis can occur if acute otitis media is not treated. •The infection spreads to the mastoid area, causing pain. •The use of antibiotics has resulted in acute mastoiditis becoming relatively uncommon. •Chronic mastoiditis is still seen with repeated middle ear infections. DIAGNOSTIC TESTS •An elevated WBC count may be seen • Cultures on ear drainage identify the specific infective organism. • Conductive hearing loss is usually present on audiometric studies and Rinne, Weber, and whisper voice tests. •Imaging studies may be done to diagnose infection. THERAPEUTIC MEASURES • Bacterial infections are treated with topical and systemic antibiotics. •Topical antibiotics may contain steroids to help with inflammation. •Oral analgesics are given to control pain. THERAPEUTIC MEASURES •A modified Politzer ear device can be used to help equalize pressure in the middle ear and aid fluid drainage. The device, also known as the ear popper, emits a stream of air into the nasal cavity that gently opens the eustachian tubes. This relieves negative pressure and allows pressure to equalize and fluid to drain. THERAPEUTIC MEASURES Surgical intervention includes several techniques. • Paracentesis may be performed with a needle and syringe. The tympanic membrane is punctured with the needle, and the fluid is drained from the middle ear. • A myringotomy may also be performed. During this procedure, an incision is made in the tympanic membrane and fluid is allowed to drain out or is suctioned out of the middle ear. THERAPEUTIC MEASURES • Another technique is laser-assisted myringotomy, which vaporizes the tympanic membrane. • Various types of transtympanic tubes may be inserted to keep the incision open. The transtympanic tube keeps the incision in the tympanic membrane open, equalizes pressure, and prevents further fluid formation and buildup. The transtympanic tubes are left in place until the infection is cured. THERAPEUTIC MEASURES • Reconstructive repair of a perforated tympanic membrane is called a myringoplasty. One technique involves placing Gelfoam over the perforation. A graft from the temporal muscle behind the ear or tissue from the external ear is then placed over the perforation and Gelfoam. The Gelfoam is absorbed, and the graft repairs the perforation. THERAPEUTIC MEASURES •A mastoidectomy involves incision, drainage, and surgical removal of the mastoid process if the infection has spread to the mastoid area. Nursing Process for the Patient With Middle Ear Disorders: • DATA COLLECTION. • reviews the subjective data that should be collected. • The external ear should be inspected and palpated to obtain objective data. • Pain with palpation is indicative of external ear problems, not middle ear problems. • Pain over the mastoid area can indicate a mastoid problem. Nursing Process for the Patient With Middle Ear Disorders: • DATA COLLECTION. • The middle ear and mastoid cavity cannot be visualized directly. • The tympanic membrane is the only middle ear structure that can be directly visualized with an otoscope. • Objective assessment also includes vital signs, noting any elevation in temperature. • Any drainage from the ear should be noted and described. • Hearing acuity is screened with the whisper voice, Rinne, and Weber tests. Nursing Process for the Patient With Middle Ear Disorders: NURSING DIAGNOSES, PLANNING, AND IMPLEMENTATION. • Risk for Infection related to broken skin, pressure necrosis, chronic disease, or surgical procedure • EXPECTED OUTCOME: The patient will have no signs of infection (no drainage from ear, no tenderness over mastoid, negative culture, and afebrile). • Explain to the patient not to blow nose by pinching off nares to prevent spread of upper respiratory infections up the eustachian tube. • Teach patient not to insert anything into ear canal to prevent ear damage. • Teach patient how to correctly remove cerumen from ear to prevent infection or damage. Nursing Process for the Patient With Middle Ear Disorders: NURSING DIAGNOSES, PLANNING, AND IMPLEMENTATION. • Acute Pain related to fluid accumulation, inflammation, or infection • EXPECTED OUTCOME: The patient will indicate pain is decreased or absent as evidenced by a lower rating on a pain scale. • Monitor pain using a pain scale, and determine optimum analgesic schedule with patient to maximize pain control. • Use nonpharmacological measures such as heat, distraction, and relaxation techniques for pain reduction. • Teach patient how to administer eardrops or ear ointment to help resolve infection and decrease pain. • Instruct patient to take all prescribed antibiotics, even after symptoms are relieved, to ensure that infection is completely resolved. Nursing Process for the Patient With Middle Ear Disorders: NURSING DIAGNOSES, PLANNING, AND IMPLEMENTATION. • Deficient Knowledge Regarding Hearing Loss and Lack of Information or Surgery related to lack of exposure to information due to no prior experience • EXPECTED OUTCOME: The patient will state an understanding of methods for preventing problems in the middle ear, tympanic membrane, and mastoid process or impending surgery. • Teach patient to avoid trauma to the ear, loud noise exposure, and environmental or occupational conditions to prevent damage to the ear. • Teach patient to yawn or perform jaw-thrust maneuver (opening mouth wide and moving jaw) to equalize ear pressure, which helps maintain ear health. • Teach patient methods of effective communication to compensate for hearing loss.