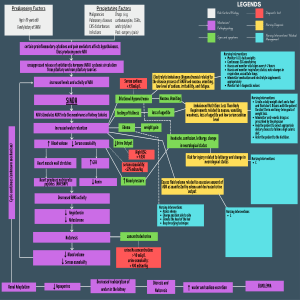
DI vs SIADH: Overview Notes Diabetes Insipidus (DI); DRY Hyposecretion of ADH/Vasopressin secondary to strokes, trauma, idiopathic causes kidney tubules fail to reabsorb water. Diabetes insipidus (DI) is associated with a deficiency (lack) of production or secretion of ADH/Vasopressin or decreased renal response to ADH. Depending on cause, DI may be transient or a chronic lifelong condition. There are three types of DI: Central (Neurogenic) ADH not produced by posterior pituitary, which is most common, nephrogenic (Renal tubules desensitized to effects of ADH, and primary. o Central (Neurogenic)- usually occurs due to severe head trauma, brain or pituitary tumors. Posterior pituitary unable to secrete vasopressin (ADH), leading to inability to concentrate urine DI is characterized by polydipsia and polyuria. If oral fluid intake cannot keep up with urinary losses, severe fluid volume deficit results as manifested by hypotension and hypovolemic shock. The increased urinary output and plasma osmolality can cause severe fluid and electrolyte imbalances. DI is characterized by dilute urine with urine output greater than 200 mL per hour and specific gravity < 1.005 (Dilute). Identification of cause as central neurogenic DI often requires a water deprivation test. For central DI, fluid and hormone therapy is the cornerstone of treatment. Nursing care includes early detection, maintenance of adequate hydration, and patient teaching for long-term management. Assessment Polyuria, 4 to 24 L/day Polydipsia Dehydration Decreased skin turgor, dry mucus membranes Inability to concentrate urine Low urinary specific gravity, below 1.005 Elevated plasma osmolality >295 mOsm/kg (Dry) Decreased urine osmolality <500 mOsm/kg (Dilute) Hypernatremia (Na high = serum dry) Fatigue Muscle pain/weakness Headache Postural hypotension that may progress to vascular collapse Tachycardia Hemo-concentration (electrolyte, etc.) Interventions – Nursing Care Monitor vital signs/cardiovascular/neurological status. Provide safe environment. Monitor electrolyte levels as prescribed (BMP, UA) Strict I&O, foley catheter 1 Monitor for signs dehydration (Decreased urine output, loss of weight, decreased specific gravity, dry skin, dry mucus membranes, lack of tears, if infant, sunken fontanel) Maintain adequate intake of fluids (Volume replacement) Administer chlorpropamide as prescribed for mild DI. Administer vasopressin (ADH) tannate or desmopressin acetate (DDAVP) IV/SQ initially as prescribed for severe or chronic deficiency in ADH. Instruct client in administration of medications as prescribed. Desmopressin acetate (DDAVP) may be administered intranasally, by injection, or orally. Educate client to obtain and wear at all times Medic-Alert bracelet. Syndrome of Inappropriate Antidiuretic Hormone (SIADH) Excess ADH/Vasopressin released, but not in response to bodily need for it. Causes include trauma, stroke, malignancies, especially lungs/pancreas, medications (antineoplastics), stress. Results in hyponatremia. Excessive release of ADH→ decreases urine volume → urine very concentrated → Can progress to water intoxication, cerebral edema and death. Syndrome of inappropriate antidiuretic hormone (SIADH) results from abnormal production or sustained secretion of ADH. The most common cause is a hormone-secreting tumor, such as lung cancer. SIADH is characterized by fluid retention, serum hypoosmolality, dilutional hyponatremia, hypochloremia, concentrated urine in presence of normal or increased intravascular volume, and normal renal function. Treatment is directed at the underlying cause with a goal to restore normal fluid volume and osmolality. Fluid restriction results in gradual, daily weight reductions, progressive rise in serum sodium concentration and osmolality, and symptomatic improvement. With chronic SIADH, patients must learn self-management. Low sodium levels must be normalized very carefully and in a measured manner. The level should not increase by more than 8 to 12 mEq/L in the first 24 hours. Sodium levels of less than 120 mg/dL are considered critical and require the implementation of seizure precautions and hourly neuro checks. Assessment Signs of fluid overload, including bounding pulse, hypertension, distended neck veins, dyspnea, crackles, pitting dependent edema, ascites Weight gain Tachycardia Early signs: Anorexia/nausea/vomiting, HA, Fatigue, Dyspnea Late signs: Decreased LOC, Coma, Seizures Hyponatremia (Na+ <135 mEq/dL) Blood Serum Osmo < 280 mOsmo/kg (Dilute) Very concentrated urine Urine Osmo >500 mOsmo/kg Interventions – Nursing Care Monitor vital signs/cardiac/neurological status. Provide safe environment. Strict I&O 2 Daily weighing, if in hospital. Monitor serum electrolytes, especially sodium. Restrict fluid intake (Free water restriction) Administer diuretics (Loop diuretics; Furosemide, Bumetadine) Administer IV fluids; If severe, 3% saline infusion + diuretic Monitor infusions carefully because of risk of water intoxication. Administer demeclocycline (tetracycline antibiotic): Increases urinary water excretion, Inhibits ADH (ADH release) induced water reabsorption/produces water diuresis Normal Labs Serum Osmolality 285-295 mOsm/kg Sodium 136-145 mEq/L Urine osmolality 500-1200 mOsm/kg Urine specific gravity 1.005-1.030 3