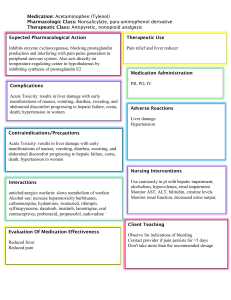
1391 Management of Primary Liver Sarcomas Jürgen Weitz, MD1 David S. Klimstra, MD2 Karina Cymes, MD2 William R. Jarnagin, MD1 Michael D’Angelica, MD1 Michael P. La Quaglia, MD1 Yuman Fong, MD1 Murray F. Brennan, MD1 Leslie H. Blumgart, MD1 Ronald P. DeMatteo, MD1* BACKGROUND. Primary hepatic sarcoma is a rare entity. The objectives of the study were to define treatment and long-term outcome and to identify prognostic factors. METHODS. Between January 1981 and December 2004, 30 patients with primary sarcoma of the liver and 5 patients with primary carcinosarcoma of the liver were treated. Patient demographics, tumor characteristics, treatment, and actuarial survival were analyzed. RESULTS. Of the 30 patients with primary hepatic sarcoma (10 epithelioid hemangioendothelioma, 5 embryonal sarcoma, 5 angiosarcoma, 3 solitary fibrous tumor, and 7 other types), 11 underwent R0-resection and had a 5-year diseasespecific survival of 64%. Of these 11 patients, 4 had low-grade sarcoma and have Department of Surgery, Memorial Sloan-Kettering Cancer Center, New York, New York. not developed tumor recurrence. In the group of 7 patients with high-grade sar- 2 within 11 months, whereas the 5 patients with embryonal sarcoma had a 5-year 1 Department of Pathology, Memorial Sloan-Kettering Cancer Center, New York, New York. comas who underwent R0-resection, both patients with angiosarcoma died disease-free and disease-specific survival of 80%. Six of the 10 patients with an epithelioid hemangioendothelioma were managed without surgery, as they had diffuse, slowly progressing, or stable lesions; these patients had a 5-year diseasespecific survival of 67%. Of the remaining 13 patients in whom R0-resection was not performed, there were no 3-year survivors. The prognosis for patients with primary carcinosarcoma of the liver was poor, with all but 1 patient dying within a year and no 3-year survivors. CONCLUSIONS. The outcome of patients with primary hepatic sarcoma depends primarily on tumor histology and the ability to achieve complete tumor resection. Improvements in outcome will require the development of more effective systemic therapies. Cancer 2007;109:1391–6. 2007 American Cancer Society. KEYWORDS: liver, sarcoma, therapy, surgery. P Current address for J. Weitz: Department of Surgery, University of Heidelberg, Heidelberg, Germany. Address for reprints: Ronald P. DeMatteo, MD, Memorial Sloan-Kettering Cancer Center, Box 203, 1275 York Ave., New York, NY 10021; Fax: (212) 639-4031; E-mail: dematter@mskcc.org Received October 16, 2006; revision received December 4, 2006; accepted December 21, 2006. ª 2007 American Cancer Society rimary sarcomas of the liver are very rare tumors, representing less than 1% of all hepatic malignancies. Some of the more common hepatic sarcomas are angiosarcoma,1,2 embryonal sarcoma,3,4 leiomyosarcoma,5,6 epithelioid hemangioendothelioma,7,8 fibrosarcoma,9 and malignant fibrous histiocytoma.10,11 Other sarcomas, such as malignant solitary fibrous tumor and follicular dendritic cell sarcoma, have also been found to arise in the liver.12 In infants and children, additional types such as rhabdomyosarcoma have been described, although these were excluded from the present report.13,14 In immunocompromised individuals smooth muscle tumors of uncertain malignant potential have been described that are Epstein-Barr virus (EBV)-driven.15 Primary soft-tissue sarcomas most commonly originate in the extremities and due to their prevalence the prognostic factors for these patients have been well documented.16–20 We previously reported our experience with sarcoma metastatic to the liver.21 Due to the rarity of primary hepatic sarcomas, the natural history, prognostic factors, and optimal management are poorly characterized. Further complicating the study of primary hepatic sar- DOI 10.1002/cncr.22530 Published online 21 February 2007 in Wiley InterScience (www.interscience.wiley.com). CANCER April 1, 2007 / Volume 109 / Number 7 coma is the diversity of histologic subtypes. In this study we analyzed our experience over the last 2 decades with primary hepatic sarcoma in order to define outcome and prognostic factors. MATERIALS AND METHODS Patients Thirty patients with primary sarcoma of the liver who were evaluated at Memorial Sloan-Kettering Cancer Center between January 1981 and December 2004 were identified from the prospective Hepatobiliary and Sarcoma databases. Patients with sarcoma metastatic to the liver or direct invasion of the liver by a retroperitoneal sarcoma were not included in this study. Five other patients with primary carcinosarcoma of the liver were also identified. All pathologic diagnoses were recently reconfirmed. Patients underwent routine staging using preoperative CT scanning of the chest, abdomen, and pelvis. Further imaging, such as magnetic resonance imaging (MRI), positron emission tomography (PET) scan, or angiography as well as percutaneous biopsy were performed at the discretion of the treating physician. Radiologic studies were reviewed at a multidisciplinary case management conference held twice weekly. Patients underwent surgical exploration if all disease was judged to be completely resectable and if the medical condition of the patient permitted liver resection. Criteria for inoperability were extrahepatic tumor spread, diffuse intrahepatic tumor making the patient not a candidate for complete tumor removal, and impaired liver function precluding the planned hepatic resection. No special liver function tests were used in the context of this study. Some patients with borderline resectablity by preoperative imaging also underwent surgical exploration. The use of neoadjuvant, adjuvant, or palliative chemotherapy was left to the discretion of the treating physician, taking into account patient preferences, tu- mor histology, patient comorbidities, and extent of the tumor. Patient demographics, tumor characteristics, treatment, and postoperative course were analyzed. The completeness of tumor resection (R0-resection [negative microscopic margins], R1-resection [positive microscopic margin], or R2-resection [gross residual disease]) was recorded. Statistical Analysis Statistical computations were performed with the software package JMP (Cary, NC). The length of follow-up was calculated from the date of hepatectomy or, in the case of nonoperative management, from the initial diagnosis at our institution. Survival was estimated according to the Kaplan-Meier method and compared using the log-rank test. Statistical significance was defined as P < .05. RESULTS Patients With Primary Liver Sarcoma (n = 30) Demographic and clinical data Of the 30 patients with primary liver sarcomas, 16 were (53%) females. The median age was 52 (range, 6–81) years. Five patients were under the age of 18 (6, 9, 9, 10, and 16 years old). The majority of patients (n ¼ 24, 80%) were Caucasian. None of the patients had known risk factors for the development of a hepatic sarcoma. The most common symptom at diagnosis was pain, which occurred in 19 patients (63%). Five patients had nonspecific symptoms such as dyspnea or abdominal discomfort and 6 patients were asymptomatic. Pathologic factors The median tumor diameter was 10.5 (range, 2–20) cm. The median tumor number was 1 (range, 1–13). Twelve patients (40%) presented with multifocal tumors. A median of 4.5 (range, 1–8) liver segments were involved. The TABLE 1 Primary Sarcomas of the Liver Histology No. Low-grade High-grade Laparotomy R0 Laparotomy R1/R2 No laparotomy Angiosarcoma Embryonal sarcoma Epithelioid hemangioendothelioma Hemangiopericytoma Leiomyosarcoma Pleomorphic MFH Smooth muscle tumor* Solitary fibrous tumor 5 5 10 1 2 1 3 3 1 0 10 1 1 0 3 3 4 5 0 0 1 1 0 0 2 5 2 0 0 0 1 1 1 0 2 0 1 1 0 0 2 0 6 1 1 0 2 2 R0 indicates R0 resection; R1/R2, R1 or R2 resection; MFH, malignant fibrous histiocytomas. *Uncertain malignant potential. 10970142, 2007, 7, Downloaded from https://acsjournals.onlinelibrary.wiley.com/doi/10.1002/cncr.22530 by Iraq Hinari NPL, Wiley Online Library on [03/04/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License 1392 1393 FIGURE 1. Treatment strategy for 30 patients with primary hepatic sarcomas. EHE indicates epithelioid hemangioendothelioma; *1 patient also received radiotherapy, § 5 patients received adjuvant chemotherapy, &2 FIGURE 2. Disease-specific survival of patients with primary hepatic sarcoma (n ¼ 30) stratified according to treatment. EHE indicates epithelioid patients received chemotherapy. hemangioendothelioma. distribution of histologic subtypes is shown in Table 1. There were 19 (63%) low-grade tumors. time of last follow-up, 5 patients (17%) had no evidence of disease, 7 (23%) were alive with disease, 13 (44%) had died of disease, 4 patients (13%) had died of causes unrelated to their malignant disease, and 1 patient (3%) was lost to follow-up. The 15 patients under the age of 50 had a significantly better 5-year disease-specific survival (67% vs 0% for older patients, P ¼ .005). For the 11 patients who underwent R0-resection, the 5-year disease-specific survival was 64%. For the 6 patients with epithelioid hemangioendothelioma who were managed conservatively, the 5-year disease-specific survival was 67%. In contrast, actuarial 3-year disease-specific survival was 0% for the other 13 patients in whom complete resection of the tumor was not possible or not attempted (P ¼ .0003, Fig. 2). There were 10 patients with epithelioid hemangioendothelioma and their 5-year disease-specific survival was 58%. Six of them were managed conservatively with a 5-year disease-specific survival of 67%. Four patients underwent laparotomy; however, only 2 patients underwent R0-resection and both died without evidence of tumor recurrence. One patient underwent R1-resection and died of disease 14 months postoperatively; 1 patient underwent R2resection and was alive with disease 24 months postoperatively. Treatment Figure 1 and Table 1 summarize the treatment of the 30 patients. In 14 (47%) patients, surgical exploration was not attempted, either due to the extent of the tumor or patient comorbidities (n ¼ 8) or as the patients had diffuse, slow-growing epithelioid hemangioendothelioma (n ¼ 6). Sixteen (53%) patients with primary hepatic sarcoma underwent surgical exploration with the intention of complete tumor resection. The following surgical procedures were performed: 7 patients underwent a left or right hepatectomy, 4 patients an extended right hepatectomy, 1 patient a bisegmentectomy, and 4 patients a laparotomy with tumor biopsy. Median blood loss was 1160 mL (interquartile range [IQR] 300–2200). The median length of hospital stay was 11.5 days (IQR 7–15); 7 of 16 (44%) patients developed postoperative complications, and the 30-day mortality was 0%. An R0-resection was achieved in 11 of the 16 patients explored, of whom 2 had received chemotherapy before surgery and 5 patients were given adjuvant chemotherapy. One patient with an epithelioid hemangioendothelioma underwent complete macroscopic tumor resection (right hepatectomy); however, pathologic workup demonstrated a positive microscopic surgical margin (R1-resection). Outcome The median follow-up for the 30 patients with primary hepatic sarcoma was 20 months (IQR 7–41 months), whereas the median follow-up for surviving patients was 39 months (IQR 25–66 months). At the Long-term outcome of patients undergoing R0-resection (n = 11) The median follow-up for the 11 patients undergoing R0-resection was 35 months (IQR 11–63 months), whereas the median follow-up for surviving patients was 63 months (IQR 38–160 months). At the time of the last follow-up, 5 (46%) patients had no evidence 10970142, 2007, 7, Downloaded from https://acsjournals.onlinelibrary.wiley.com/doi/10.1002/cncr.22530 by Iraq Hinari NPL, Wiley Online Library on [03/04/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License Primary Liver Sarcoma/Weitz et al. CANCER April 1, 2007 / Volume 109 / Number 7 years, with the other patients surviving less than 1 year. The median disease-specific survival for all patients with carcinosarcoma was 8 months. DISCUSSION FIGURE 3. Disease-free survival after R0-resection of hepatic sarcoma (n ¼ 11) stratified according to histology. of disease, 3 (27%) had died of disease, and 3 (27%) patients had died of causes unrelated to their malignant disease. The actuarial 5-year disease-free survival of the 11 patients undergoing complete tumor resection was 70% and the median has not been reached. None of the 4 patients with a low-grade tumor developed a tumor recurrence (5-year diseasefree survival 100%) compared with a 5-year diseasefree survival of 57% in patients with a high-grade sarcoma. The patients with primary angiosarcoma had a particularly poor prognosis, with both patients developing recurrence and dying within 11 months (Fig. 3). The actuarial 5-year disease-specific survival of the 11 patients undergoing complete tumor resection was 64% and the median has not been reached. Patients with embryonal sarcomas had a 5-year disease-specific survival (and also disease-free survival) of 80% despite having high-grade tumors. Patients With Carcinosarcoma of the Liver (n = 5) Carcinosarcomas were included because their sarcomatoid components may be nearly indistinguishable from true sarcomas, and they clearly fall in the histologic differential diagnosis of primary liver sarcomas. Because carcinosarcomas are fundamentally of epithelial origin, they were analyzed separately from the 30 primary sarcomas of the liver. Of the 5 patients with primary carcinosarcoma of the liver, there were 3 female and 2 male patients with a median age of 67 (range, 34–70). One of the patients had underlying liver cirrhosis. Four patients underwent laparotomy with the intention of tumor resection. R0-resection was achieved in only 1 patient and this patient died of disease 8 months later. Only 1 patient with carcinosarcoma survived for almost 3 In this study we evaluated the outcome and prognostic factors of patients presenting with primary hepatic sarcomas. There are only a few series in the literature regarding the management of primary hepatic sarcomas in a mainly adult patient population.22–25 The rarity of this disease is evident by the existence of only 30 patients with primary hepatic sarcoma managed at our institution between 1981 and 2004, compared with 331 patients with liver metastases from sarcoma admitted to our institution during a similar time period.21 In our 30 patients with primary hepatic sarcoma, we were able to define 3 distinct groups of patients: patients with complete tumor resection (R0-resection), patients in whom complete resection was not possible or not attempted, and patients with epithelioid hemangioendothelioma who were managed conservatively because they had diffuse and indolent disease. Long-term (>3 years) survival was only possible if R0-resection was achieved, except for patients with epithelioid hemangioendothelioma. Surgical resection therefore seems to be the only potentially curative treatment. In 5 of 16 patients (31%) undergoing surgical exploration a complete tumor resection (R0-resection) could not be achieved. One might view this as a high R1/R2-resection rate. However, it is our policy to offer surgical exploration to all patients without obvious criteria of irresectability or medical problems precluding major resection. This aggressive approach is based on the importance of complete tumor resection in order to reach cure for the patient and the lack of effective alternative therapies. The development of more accurate imaging methods may improve patient selection. Hepatic resection was safe for these patients, with no 30-day mortality and an acceptable complication rate. As we and others have reported recently, hepatic resection has become a safe treatment modality for patients with hepatic tumors.26 Age and completeness of resection were significant prognostic factors regarding disease-specific survival, which is consistent with prognostic factors defined for primary soft-tissue sarcomas of other locations, such as the extremity or retroperitoneum.17–20 Interestingly, grade did not appear to be a significant prognostic factor in our analysis, but the numbers are too small for definitive conclusion. This is in contrast to other studies regarding primary hepatic sarcoma and to the find- 10970142, 2007, 7, Downloaded from https://acsjournals.onlinelibrary.wiley.com/doi/10.1002/cncr.22530 by Iraq Hinari NPL, Wiley Online Library on [03/04/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License 1394 ings in primary soft-tissue sarcoma that arise in other locations.19,20,23,27 When looking at the patients in our series who underwent R0-resection, however, it becomes clear that no patient with a low-grade sarcoma experienced a tumor recurrence, underlining the relevance of tumor grade in determining the prognosis of the patient. Patients with high-grade sarcomas who underwent R0-resection either had angiosarcoma or embryonal sarcoma. Prognosis for patients with angiosarcoma was dismal, which is in accordance with a previous report.28 Patients with embryonal sarcoma, however, seem to have a particularly favorable outcome, with a 5-year disease-specific survival of 80% in our series. Embryonal sarcomas usually occur in patients 6 to 10 years of age and are only uncommon in adults.4,29 In our series 3 of the 5 patients with embryonal sarcoma fell into the expected age distribution; however, 2 patients presented at the age of 16 and 18. All 5 of our patients with embryonal sarcoma underwent R0resection followed by systemic chemotherapy. The 5year disease-specific survival of 80% for patients with embryonal sarcoma is better than that previously reported, even though other studies have reported favorable outcomes after resection in combination with postoperative chemotherapy.29,30 Complete resection followed by systemic chemotherapy might therefore be the optimal treatment for these patients. Epithelioid hemangioendothelioma is a distinctive vascular neoplasm that usually arises in liver, lung, or bone and can be regarded as a type of low-grade angiosarcoma. Ten patients with epithelioid hemangioendothelioma were included in our series, with a 5year disease-specific survival of 58%. Of note, 6 patients were managed conservatively and they had a 5-year disease-specific survival of 67%. Our results are consistent with those of others—hepatic epithelioid hemangioendothelioma is a malignant tumor with a favorable, yet unpredictable clinical course in the majority of patients. Treatment options include liver transplantation, resection, or nonsurgical management, and depend on tumor extent, tumor progression, and patient comorbidities.7,8,31 We treated 5 patients with carcinosarcoma. As these tumors are fundamentally epithelial tumors in which the sarcomatoid elements are thought to arise via transdifferentiation, we analyzed them separately. In the literature, only a few primary carcinosarcomas of the liver have been reported.32,33 Whereas the majority of patients previously reported were men with liver cirrhosis or fibrosis, 3 of the 5 patients in this report were female patients, and only 1 patient had underlying liver cirrhosis. Consistent with these other reports, we found that the prognosis for patients 1395 with primary carcinosarcoma of the liver is poor. The sarcomatoid regions of carcinosarcomas may be very difficult to distinguish from true sarcomas, especially on the basis of a small biopsy specimen. Our data underscore the importance of tumor histology and complete tumor resection in the treatment of primary hepatic sarcoma. However, we and others have shown that recurrence is common.23 Although randomized trials have shown that radiotherapy decreases the local recurrence rate but does not improve survival for extremity sarcoma,34,35 the use of radiotherapy is constrained in the liver due to potential toxicity. Whether adjuvant chemotherapy improves overall survival in soft-tissue sarcoma remains debatable, although 1 meta-analysis demonstrated a small benefit.36 Without surgery, chemotherapy can only rarely cure patients with sarcoma.37 As indicated above, adjuvant chemotherapy might have a role in the treatment of patients with embryonal sarcoma of the liver. New combination regimens might improve efficacy and decrease side effects, but whether they improve survival has not been firmly established.38 We conclude that the outcome of patients with primary hepatic sarcoma depends primarily on tumor histology and the ability to achieve complete tumor resection. Overall, in order to improve the outcome for these patients, more effective systemic therapies are needed. REFERENCES 1. El-Domeiri AA, Huvos AG, Goldsmith HS, Foote FW. Primary malignant tumors of the liver. Cancer. 1971;27:7–11. 2. Alrenga DP. Primary angiosarcoma of the liver: review article. Int Surg. 1975;60:198. 3. Walker NI, Horn MJ, Strong RW, et al. Undifferentiated (embryonal) sarcoma of the liver. Cancer. 1992;69:52–59. 4. Stocker JT, Ishak KG. Undifferentiated (embryonal) sarcoma of the liver. Cancer. 1978;42:336–348. 5. Bloustein PA. Hepatic leiomyosarcoma. Ultrastructural study and review of the differential diagnosis. Hum Pathol. 1978;9:713–715. 6. Gates LK, Cameron A, Nagorney DM, Goellner JR, Farley DR. Primary leiomyosarcoma of the liver mimicking liver abscess. AJG. 1995;90:649–652. 7. Ishak KG, Sesterhenn IA, Goodman MZD, Rabin L, Strohmeyer FW. Epithelioid hemangioendothelioma of the liver. A clinicopathologic and follow-up study of 32 cases. Hum Pathol. 1984;15:839–852. 8. Makhlouf HR, Ishak KG, Goodman ZD. Epithelioid hemangioendothelioma of the liver: a clinicopathologic study of 137 cases. Cancer. 1999;85:562–582. 9. Alrenga DP. Primary fibrosarcoma of the liver. Case report and review of the literature. Cancer. 1975;36:446–449. 10. Arends JW, Willebrand D, Blaauw AMM, Bosman FT. Primary malignant fibrous histiocytoma of the liver. A case report with immunocytochemical observations. Histopathology. 1987;11:427–431. 10970142, 2007, 7, Downloaded from https://acsjournals.onlinelibrary.wiley.com/doi/10.1002/cncr.22530 by Iraq Hinari NPL, Wiley Online Library on [03/04/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License Primary Liver Sarcoma/Weitz et al. CANCER April 1, 2007 / Volume 109 / Number 7 11. Fujita S, Lauwers GY. Primary hepatic malignant fibrous histiocytoma: report of a case and review of the literature. Pathol Int. 1998;48:225–229. 12. Torres U, Hawkins WG, Antonescu C, DeMatteo R. Hepatic follicular dendritic cell sarcoma without Epstein-Barr virus expression. Arch Pathol Lab Med. 2005;129:1480–1483. 13. Horowitz ME, Etcubanas E, Webber BL, et al. Hepatic undifferentiated (embryonal) sarcoma and rhabdomyosarcoma in children. Results of therapy. Cancer. 1987;59:396– 402. 14. Hadley GP, Govender D, Landers G. Primary tumours of the liver in children: an African perspective. Pediatr Surg Int. 2004;20:314–318. 15. Lee ES, Locker J, Nalesnik M, et al. The association of Epstein-Barr virus with smooth-muscle tumors occurring after organ transplantation. N Engl J Med. 1995;332:19–25. 16. Lewis JJ, Leung DH, Heslin MJ, Woodruff J, Brennan MF. Association of local recurrence with subsequent survival in extremity soft tissue sarcoma. J Clin Oncol. 1997;15:646– 652. 17. Pisters PWT, Leung DH, Woodruff J, Shi W, Brennan MF. Analysis of prognostic factors in 1041 patients with localized soft tissue sarcomas of the extremities. J Clin Oncol. 1996;14:1679–1689. 18. Stojadinovic A, Leung DH, Hoos A, Jaques DP, Lewis JJ, Brennan MF. Analysis of the prognostic significance of microscopic margins in 2,084 localized primary adult soft tissue sarcomas. Ann Surg. 2002;235:424–434. 19. Weitz J, Antonescu C, Brennan M. Localized extremity soft tissue sarcoma: improved knowledge with unchanged survival over time. J Clin Oncol. 2003;21:2719–2725. 20. Kattan MW, Leung DH, Brennan MF. Postoperative nomogram for 12-year sarcoma specific death. J Clin Oncol. 2002;20:791–796. 21. DeMatteo RP, Shah A, Fong Y, Jarnagin WR, Blumgart LH, Brennan MF. Results of hepatic resection for sarcoma metastatic to the liver. Ann Surg. 2001;234:540–548. 22. Almogy G, Lieberman S, Gips M, et al. Clinical outcomes of surgical resection for primary liver sarcoma in adults: results from a single centre. Eur J Surg Oncol. 2004;30:421– 427. 23. Poggio JL, Nagorney DM, Nascimento AG, et al. Surgical treatment of adult primary hepatic sarcoma. Br J Surg. 2000;87:1500–1505. 24. Zornig C, Kremer B, Henne-Bruns D, Weh HJ, Schroder S, Brolsch CE. Primary sarcoma of the liver in the adult. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. Report of five surgically treated patients. Hepatogastroenterology. 1992;39:319–321. Forbes A, Portmann B, Johnson P, Williams R. Hepatic sarcomas in adults: a review of 25 cases. Gut. 1987;28:668–674. Jarnagin WR, Gonen M, Fong Y, et al. Improvement in perioperative outcome after hepatic resection. Ann Surg. 2002;236:397–407. Lewis JJ, Leung D, Woodruff JM, Brennan MF. Retroperitoneal soft-tissue sarcoma. Ann Surg. 1998;228:355–365. Vennarecci G, Ismail T, Gunson B, McMaster P. Primary angiosarcoma of the liver. Minerva Chir. 1997;52:1141– 1146. Johnson J, White J, Thompson A. Undifferentiated (embryonal) sarcoma of the liver in adults. Am Surg. 1995;61:285– 287. Kim DY, Kim KH, Jung SE, Lee SC, Park KW, Kim WK. Undifferentiated (embryonal) sarcoma of the liver: combination treatment by surgery and chemotherapy. J Pediatr Surg. 2002;37:1419–1423. Mehrabi A, Kashfi A, Schemmer P, et al. Surgical treatment of primary hepatic epithelioid hemangioendothelioma. Transplantation. 2005;80:S109–112. Freeman AJ, Bullpitt P, Keogh GW. Primary hepatic carcinosarcoma. ANZ J Surg. 2004;74:1021–1023. Nomura K, Aizawa S, Ushigome S. Carcinosarcoma of the liver. Arch Pathol Lab Med. 2000;124:888–890. Pisters PWT, Harrison LB, Leung DH, Woodruff J, Casper ES, Brennan MF. Long-term results of a prospective randomized trial of adjuvant brachytherapy on soft tissue sarcoma. J Clin Oncol. 1996;14:859–868. Yang JC, Chang AE, Baker AR, et al. Randomized prospective study of the benefit of adjuvant radiation therapy in the treatment of soft tissue sarcomas of the extremity. J Clin Oncol. 1998;16:197–203. Tierney JF, Steward LA, Parmar MKB. Adjuvant chemotherapy for localised resectable soft-tissue sarcoma of adults: meta-analysis of individual data. Lancet. 1997;350:1647– 1654. Blay JY, van Glabbeke M, Verweij J, et al. Advanced soft tissue sarcoma: a disease that is potentially curable for a subset of patients treated with chemotherapy. Eur J Cancer. 2003;39:64–69. Siehl JM, Thiel E, Schmittel A, et al. Ifosfamide/liposomal daunorubicin is a well tolerated and active first-line chemotherapy regimen for advanced soft tissue sarcoma. Cancer. 2005;104:611–617. 10970142, 2007, 7, Downloaded from https://acsjournals.onlinelibrary.wiley.com/doi/10.1002/cncr.22530 by Iraq Hinari NPL, Wiley Online Library on [03/04/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License 1396