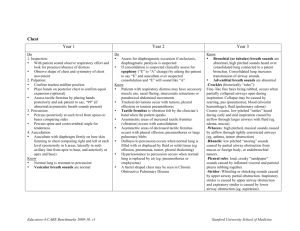
Script for NCM 101 (Thorax and Lungs) Greet C.I (Good morning, Doc Cy, I am Mary Anne Taylor and I will be demonstrating Assessment of Thorax and Lungs. Examination of the thorax and lungs gives the medical provider information about the movement of air and gas exchange. The purpose of this assessment is – that once we perform a comprehensive respiratory assessment it can detect problems before they become emergencies. then proceed… - Prior going to the patient’s room make sure you review the patient’s medical record, and prepared all the necessary equipment needed for this assessment. (Stethoscope, skin marker/pencil, centimeter ruler) - Don’t forget to do hand hygiene, you can use alcohol as a sanitizer to prevent cross contamination. - Make sure knock first prior entering the patient’s room. (Knock-knock) - Greet the patient (Good morning, Ma’am, my name is Mary Anne, I will be your student nurse for today from 7am till 3pm. How are you feeling? --- I am here to do an assessment of your Thorax and Lungs. May I ask for your permission when I need to touch your chest and back area during the procedure? I will be needing your full cooperation in this assessment to help us give you proper medical intervention if needed --- Rest assured that all of the data conducted here is fully confidential. -Locate the hospital name tag of the patient to see patient’s name and date of birth as a patient identifier and to know that you are with the correct patient. (Can you tell me your name and DOB please) - Always provide privacy by drawing the curtain and create a proper environment by making sure its well-lit, quiet and right room temperature. (Are you comfortable?) Okey, let’s start, I have some few questions… Do you have any family history illness, cancer, allergies, tuberculosis? Lifestyle habits such as smoking and occupational hazards (ex: inhaling fumes) Medications Current problems (ex: swellings, coughs, wheezing, and pain) POSTERIOR THRAX 9. Inspect the shape and symmetry of the thorax from posterior and lateral views. Compare the anteroposterior diameter to the transverse diameter. - I observed that the anteroposterior to transverse diameter in ratio of 1-2, Chest symmetric ABNORMAL: Barrel chest, increased anteroposterior to transverse diameter, chest asymmetric 10. Inspect the spinal alignment for deformities if the client can stand. From a lateral position, observe the three normal curvatures: cervical, thoracic, and lumbar. - I observed that spine is vertically aligned ABNORMAL: exaggerated spinal curvatures(kyphosis, lordosis) To assess for lateral deviation of spine (scoliosis), observe the standing client from the rear. Have the client bend forward at the waist and observe from behind. -I observed that spinal column is straight, right and left shoulders and hips are at the same height. ABNORMAL: Spinal column deviates to one side, often accentuated when bending over. Shoulders or hips not even 11. Palpate the posterior thorax. For clients who have no respiratory complaints, rapidly assess the temperature and integrity of all chest skin. - Skin is intact and uniform in temperature ABNORMAL: Visible skin lesions and areas of hyperthermia For clients who have respiratory complaints, palpate all thorax areas for bulges, tenderness, or abnormal movements. Avoid deep palpation for painful areas, especially if a fractured rib is suspected. In such a case, deep palpation could lead to displacement of the bone fragment against the lungs. -Chest wall is intact, no tenderness nor masses ABNORMAL: lumps, bulges, depressions, areas of tenderness, movable structures such as ribs 12. Palpate the posterior thorax for respiratory excursion (thoracic expansion). Place the palms of both your hands over the lower thorax with your thumbs adjacent to the spine and your fingers stretched laterally. Ask the client to take a deep breath while you observe the movement of your hands and any lag in movement (I am going to place my hand on your midback, and I am going to ask you to take a deep breath) -full and symmetric chest expansion (ex: when the client takes a deep breath, your thumbs should move apart an equal distance and at the same time, normally the thumbs separate 3 to 5cm (1 ½ to2 inches) during deep inspiration) ABNORMAL: asymmetric and/or decreased chest expansion 13. Palpate the thorax for vocal (tactile) fremitus, the faintly perceptible vibration felt through the chest wall when the client speaks. -Bilateral symmetry of vocal fremitus. Fremitus is heard most clearly at the apex of the lungs ABNORMAL: Decreased or absent of fremitus (associated with pneumothorax) Increased fremitus (associated with consolidated lung tissue as in pneumonia) ● Place the palmar surfaces of your fingertips or the ulnar aspect of your hand or closed fist on the posterior thorax, starting near the apex of the lungs -Low-pitched voices of males are more readily palpated than higher pitched voices of females ● Ask the client to repeat such words as “blue moon” or “one, two, three.” ● Repeat the two steps, moving your hands sequentially to the base of the lungs. ● Compare the fremitus on both lungs and between the apex and the base of each lung, using either one hand and moving it from one side of the client to the corresponding area on the other side or using two hands that are placed simultaneously on the corresponding areas of each side of the thorax. 14. Percuss the thorax. Percussion of the thorax is performed to determine whether underlying lung tissue is filled with air, liquid, or solid material and to determine the positions and boundaries of certain organs. Because percussion penetrates to a depth of 5 to 7 cm (2 to 3 in.), it detects superficial rather than deep lesions. ● Ask the client to bend the head and fold the arms forward across the chest. Rationale: This separates the scapula and exposes more lung tissue to percussion. ● Percuss in the intercostal spaces at about 5-cm (2-in.) intervals in a systematic sequence. ● Compare one side of the lung with the other. ● Percuss the lateral thorax every few inches, starting at the axilla and working down to the eighth rib. -percussion notes resonate, except over scapula., lowest point of resonance is at the diaphragm (ex: at the level of 8th to 10th rib posteriorly) Note: percussion on a rib normally elicits dullness ABNORMAL: asymmetry in percussion, areas of dullness or flatness over lung tissue (associated with consolidation of lung tissue or a mass) 15. Auscultate the thorax using the flat-disk diaphragm of the stethoscope.(best for transmitting the high pitched breath sounds) ● Use the systematic zigzag procedure used in percussion. ● Ask the client to take slow, deep breaths through the mouth. Listen at each point to the breath sounds during a complete inspiration and expiration. ● Compare findings at each point with the corresponding point on the opposite side of the thorax. -Vesicular and bronchovesicular breath sounds (definition only: vesicular- soft-intensity, low-pitched, “gentle sighing” sounds created by air moving through smaller airways (bronchioles and alveoli)., bronchovesicular- moderate-intensity and moderate-pitched “blowing” sounds created by air moving through larger airway (bronchi) ABNORMAL: adventitious breath sounds (ex: crackles, gurgles, wheeze, friction rub)., absence of breath sounds. ANTERIOR THORAX 16. Inspect breathing patterns (e.g., respiratory rate and rhythm). -quiet, rhythmic, and effortless respirations-ABNORMAL:-17. Inspect the costal angle (angle formed by the intersection of the costal margins) and the angle at which the ribs enter the spine. -costal angle is less than 90*, and the ribs insert into the spine at approximately a 45* angle ABNORMAL: coastal angle is widened (associated with chronic obstructive pulmonary disease) 18. Palpate the anterior thorax for respiratory excursion. ● Place the palms of both your hands on the lower thorax, with your fingers laterally along the lower rib cage and your thumbs along the costal margins. ● Ask the client to take a deep breath while you observe the movement of your hands. -full symmetric excursion, thumbs normally separate 3 to 5 cm (1 ½ to 2 inches) ABNORMAL: asymmetric and/or decreased respiratory excursion 19. Palpate tactile fremitus in the same manner as for the posterior thorax. If the breasts are large and cannot be retracted adequately for palpation, this part of the examination is usually omitted. -same as posterior vocal fremitus; fremitus is normally decreased over heart and breast tissue. ABNORMAL: same as posterior fremitus 20. Percuss the anterior thorax systematically. Begin above the clavicles in the supraclavicular space, and proceed downward to the diaphragm. Compare the lung on one side to the lung on the other side. Displace female breasts to facilitate percussion of the lungs. - percussion notes resonate down to the 6th rib at the level of the diaphragm but are flat over areas of heavy muscle and bone, dull on areas over the heart and the liver, and tympanic over the underlying stomach. ABNORMAL: asymmetry in percussion notes, areas of dullness or flatness over lung tissue. 21. Auscultate the trachea. -bronchial and tubular breath sounds (definition lang: bronchial(tubular) means high-pitched, loud, “harsh” sounds created by air moving through the trachea ABNORMAL: adventitious breath sounds 22. Auscultate the anterior thorax, beginning over the bronchi between the sternum and the clavicles. -Bronchovesicular and vesicular breath sounds (definition lang: bronchovesicular- moderate-intensity and moderate-pitched “blowing” sounds created by air moving through larger airway (bronchi), vesicular- soft-intensity, low-pitched, “gentle sighing” sounds created by air moving through smaller airways (bronchioles and alveoli) LIFESPAN CONSIDERATION: Infants: to assess tactile fremitus, place the hand over the crying infant’s chest Children: they tend to breathe more abdominally than thoracically up to age 6 Elder: thoracic curvature may be accentuated(kyphosis) because of osteoporosis and changes in cartilage, resulting in collapse in the vertebrae. This can also compromise and decrease normal respiratory effort. - Ok ma’am we are now done with the assessment. I am now going to document all the data in your chart. Thank you for your cooperation. - Do not forget to do a hand hygiene after the assessment.