Tranexamic Acid Misadventures: Anesthesia Safety Commentary
advertisement

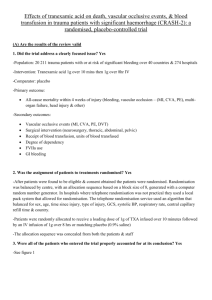
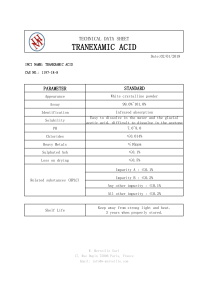
[Downloaded free from http://www.joacc.com on Saturday, August 6, 2022, IP: 14.186.209.12] Commentary Tranexamic Acid: Beware of Anaesthetic Misadventures Abstract Tranexamic acid (TXA) is an antifibrinolytic agent that is commonly used in cardiac, gynecologic, and obstetric surgeries. Inadvertent intrathecal injection of the TXA may lead to serious side effects, including back pain, myoclonus, seizure, and ventricular fibrillation that can be attributed to similar appearance of ampoules, location of ampoules, and incorrect labeling of prefilled syringes and can be avoided by vigilance, correct labeling of syringes and ampoules, double checking medications prior to administration, and preventing manufacturing of vials of different drugs with similar appearance. Treatment of intrathecal injection of the TXA includes administration of the anticonvulsants, general anaesthetics, MgSO4, along with intensive haemodynamic monitoring, scalp electroencephalography monitoring guided burst suppression with thiopentone infusion and cerebrospinal fluid lavage. Sunanda Gupta, Anil K. Bhiwal, Karuna Sharma Department of Anesthesiology, Geetanjali Medical College and Hospital, Udaipur, Rajasthan, India Keywords: Cerebrospinal fluid lavage, electroencephalography, intrathecal injection, seizure, spinal anaesthesia, tranexamic acid Introduction Medication errors during anaesthesia vary from <1% of anaesthetics to >5% of medication administrations.[1‑3] The absolute incidence of drug administration errors in the neuraxial compartment during obstetric procedures cannot be known from published case reports as reporting bias, medicolegal implications, and lack of an established critical incident reporting system in our country tend to limit publications. Thus, many errors go unreported and what are reported likely represent just the tip of the iceberg. Moreover, these are infrequent events difficult to study and require long periods of data collection, with potential risks of introduction of confounding variables. Failure to acknowledge human factors and system weaknesses along with the lack of accountability in anaesthesia has led to perioperative drug mishandling. We have been pioneers in sensitizing the world to our patient safety efforts with phenomenal efforts invested in making our equipment safer for anaesthesia. Yet, despite mounting evidence, we have not developed or implemented tamper‑proof interventions to improve medication safety during anaesthesia to prevent medication errors. Brittle strategies such as “provider vigilance” and This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercialShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms. For reprints contact: reprints@medknow.com “reading the label” are the only safeguards practiced worldwide, especially in low‑resource countries. Thus, unintentional intrathecal/epidural administration of intravenous (IV) medications continues with occasionally devastating consequences leading to death.[4] The World Health Organization (WHO) recently included tranexamic acid (TXA) in its “Model List of Essential Medicines” with a strong recommendation for early use of IV TXA (within 3 h of birth), in addition to standard care for women with clinically diagnosed postpartum haemorrhage, following vaginal birth or cesarean section.[5] It should be given at a fixed dose of 1 g (100 mg/ml) intravenously at 1 ml/min (i.e., given over 10 min), with a second dose of 1 g intravenously if bleeding continues after 30 min, or if bleeding restarts within 24 h of completing the first dose. Thus, TXA is advocated as a life‑saving intervention that should be made readily available for the management of postpartum haemorrhage wherever emergency obstetric care is provided.[6] Drug administration errors with TXA attributed to wrong drug drawn up from incorrect ampoule in error and administered in the neuraxial space are alarming case reports increasingly appearing in the literature. The actual number of intrathecal Address for correspondence: Dr. Anil Kumar Bhiwal, Department of Anesthesiology, Geetanjali Medical College and Hospital, Udaipur ‑ 313 001, Rajasthan, India. E‑mail: anilbhiwal@yahoo.co.in Access this article online Website: www.joacc.com DOI: 10.4103/joacc.JOACC_12_18 Quick Response Code: How to cite this article: Gupta S, Bhiwal AK, Sharma K. Tranexamic acid: Beware of anaesthetic misadventures. J Obstet Anaesth Crit Care 2018;8:1-6. © 2018 Journal of Obstetric Anaesthesia and Critical Care | Published by Wolters Kluwer - Medknow 1 [Downloaded free from http://www.joacc.com on Saturday, August 6, 2022, IP: 14.186.209.12] Gupta, et al.: Accidental Intrathecal tranexamic acid medication errors are vastly understated and the main goal of this review is to increase awareness among anaesthesia care providers regarding prevention strategies and treatment recommendations resulting in a positive outcome. Our literature search yielded 17 case reports[7-23] which have been summarised with drug dose, surgical procedure, signs and symptoms, management, sequelae of errors, and final outcome in Table 1. Inadvertent intrathecal injection of the TXA instead of hyperbaric bupivacaine was given in all these case reports because of the similarity of appearance of both the ampoules. The most commonly reported neurological complications were failure of intended sensory and motor block, severe back pain radiating to the gluteal region and lower extremities, and involuntary motor activity, such as a “jerking” of the lower extremities (referred to as myoclonic movements). These abnormal movements rapidly progressed to generalised tonic–clonic seizures. Myoclonic movements may serve as a warning sign of impending seizures.[8,14] Hypertension, tachycardia, refractory ventricular arrhythmias, cardiovascular collapse, and death occurred in nearly eight of these reports. Common side effects reported with parenteral administration of TXA are headache, backache, nasal sinus congestion, abdominal pain, diarrhea, fatigue, anaemia, and rarely pulmonary embolism, deep vein thrombosis, anaphylaxis, visual disturbances, and seizures.[24] It has been reported that IV injection with 1 g TXA results in a concentration of 5–20 mg/l in the plasma and 2–5 mg/l in the cerebrospinal fluid (CSF). Assuming that the drug was thoroughly diluted within the thecal space containing 500 ml of CSF, 500 mg TXA would produce a concentration of 1,000 mg/l in the CSF, which is 500 times greater than the therapeutic level (2–5 mg/l).[25] Proposed Mechanism Severe pain in back and gluteal region Gamma‑aminobutyric acid (GABA) and glycine are co‑released by spinal dorsal horn neurons and are important in regulating sensory processing. In addition, GABA and glycine receptors are abundant in the spinal cord, and antagonism of these receptors produces pain phenomena, such as allodynia and hyperalgesia. Indeed, several clinical studies have reported that patients to whom TXA was accidentally injected intrathecally immediately complained of severe back pain.[8,11,14,26] Thus, it seems TXA directly inhibits GABA and glycine receptors located on postsynaptic sites of the recorded substantia gelatinosa (SG) neurons and also inhibits GABA‑A and glycine receptors located on postsynaptic sites on excitatory interneurons. This leads to increased glutamate release from the excitatory interneurons to the recorded SG neurons located postsynaptically, resulting in increased spontaneous activity [Figure 1].[27] 2 Figure 1: Model circuit for underlying mechanism of TXA induced pain in the spinal dorsal horn circuit Seizures The diagnosis of TXA‑associated seizures may be facilitated by EEG monitoring and that could also help distinguish between TXA‑associated seizures, shivering, myoclonic movements, and thereby prevent a misdiagnosis. It may also detect subclinical seizures that are not apparent by observing sedated patients.[19,28] Triggering of seizures may be explained by suppression of the inhibitory GABA‑A receptors in the cerebral cortex or by direct cerebral ischaemia as a result of reduced cerebral blood flow. Blockade of GABA‑A receptor by the TXA leads to lower threshold for neuronal depolarization and enhanced neurotoxicity. The proconvulsant properties of TXA likely result from direct effects on the central nervous system, as application of TXA to the cortex or injection into the cisterna magna in experimental animals causes systemic as well as intracranial hypertension and seizures. Epileptic property of TXA is directly proportional to the concentration of the drug and area of the exposed cortex.[29,30] Furtmuller et al. first showed that TXA is a competitive antagonist of GABA‑A receptors and that it inhibits recombinant GABA‑A receptors (a1b2c2) with a half‑maximal inhibitory concentration (IC50) of 7 mM. GABA‑A receptors generate two distinct forms of inhibition, synaptic and tonic, which could exhibit different sensitivities to TXA. Synaptic currents are fast transient events that are activated by near saturating concentrations of agonist. In contrast, tonic currents are generated by low, ambient concentrations of transmitter.[31] TXA competitively inhibits glycine because TXA is a structural analog of glycine receptors and this action contributes to seizures, which is supported by other glycine receptor antagonists, such as strychnine, and cause myoclonic movements and twitching, particularly in the lower limbs, as well as muscle spasms and convulsions similar to the pattern of the proconvulsant effects of TXA. Similar to GABA‑A receptors, glycine receptors generate Journal of Obstetric Anaesthesia and Critical Care | Volume 8 | Issue 1 | January-June 2018 [Downloaded free from http://www.joacc.com on Saturday, August 6, 2022, IP: 14.186.209.12] Gupta, et al.: Accidental Intrathecal tranexamic acid Author Table 1: Summary of published case reports of inadvertent intrathecal injection of tranexamic acid Wong et al, 1988[7] De Leede‑van der Maarl et al, 1999[8] Yeh et al., 2003[9] Sabzi et al., 2009[10] Dose of TXA/ surgery 75 mg TXA appendicectomy 150 mg TXA 500 mg in 10 ml saline Indwelling intrathecal catheter for chronic pain relief 500 mg elective cesarean section Signs & symptoms Management Sequelae Persistent motor sensory block both lower extremities, Urinary incontinence Statusepilepticus Diazepam Myoclonus, generalized seizure , Hyperthermia, recovered Diazepam, phenytoin and thiopental Diazepam, DC shock Survived with bilateral peroneal palsy Generalized convulsions, cardiovascular collapse, and refractory ventricular fibrillation Severe pain in the back and gluteal region, myoclonus lower extremities, Hypertension, tachycardia Myoclonus, generalized seizure refractory ventricular fibrillation General anaesthesia, diazepam Death after 1.5 h Myoclonus, generalized seizure refractory ventricular fibrillation. GA, propofol infusion, phenytoin, sodium valproate, dexamethasone, General anaesthesia, lidocainesedative drugs and mechanically ventilated. Death Myoclonus, tonic clonic convulsions, recovered fully on sixth postoperative day Tachyarrhythmia, nystagmus, , seizure, ventricular tachycardia, fibrillation.death Mohseni K et al., 2009[11] Orthopedic surgery Perianal burning, hypertension, tachycardia, Veisi F et al., 2010[12] Emergency caesarean section Kaabachi et al., 2011[13] 90 mg TXA Tossing and turning, severe sharp pain in lower extremities, dysphoric, dizziness. No sensory or motor block. Severe pain in the back and gluteal region, myoclonus lower extremities, Hypertension, tachycardia Butala BP et al., 2012[14] 300 mg TXA cystolithotripsy Severe burning pain in both lower limbs, back and gluteal region, irritable. Myoclonus lower limbs Mahmoud K et al., 2012[15] 300 mg TXA lower‑limb skin grafting Severe pain in the back and gluteal region, no sensory motor block, hypertension, tachycardia Srivastava et al. 2012[16] 350 mg TXA cholecystectomy GA, Diazepam, symptomatic management Raghu et al., 2013[17] TXA 250 mg Caesarean section Severe pain back radiating to lower limbs, restless, Hypertension, tachycardia, myoclonic movement of feet Back pain, gluteal region, lower limb pain, myoclonus, Antwi‑kusi et al., 2013[18] 200 mg TXA Elective Caesarean section General anaesthesia Goyal G et al., 2014[19] 250 mgTXA herniorrhaphy No sensory block, Myoclonus lower extremity, hypertension Pain in the back, lower limbs, generalized tonic‑clonic seizures., Hypertension, tachycardia GA, Clonazepam, phenobarbital and sodium thiopental infusion Midazolam, propofol, sodium thiopentone, phenytoin, dexamethasone, sodium valproate, levetiracetam and mannitol. CSF lavage with 20 ml NS GA, Propofol, propranolol, amiodarone, lidocaine, and mannitol General anaesthesia GA, lorazepam, phenytoin, clobazampropofol infusion, EEG, induced coma with thiopentone infusion, Recurrent attacks of polymyoclonus and seizures, ventricular tachycardia recovered within 4 days without any neurologic sequelae Discharged on 7th day without any neurological sequelae Generalized myoclonic seizures, ventricular fibrillation, fully recovered without any neurologic sequelae Generalized convulsions, complete CVS collapse, multifocal PVC on ECG, Death after 6hrs ventricular arrhythmias, Cardiovascular collapse, death Seizures, ventricular tachycardia fibrillation, death Recurrent generalized tonic clonic seizures, refractory status epilepticus, discharged after 7 days without any neurological deficit Contd... Journal of Obstetric Anaesthesia and Critical Care | Volume 8 | Issue 1 | January-June 2018 3 [Downloaded free from http://www.joacc.com on Saturday, August 6, 2022, IP: 14.186.209.12] Gupta, et al.: Accidental Intrathecal tranexamic acid Author Roy A et al., 2015[20] Dose of TXA/surgery 200 mg caesarean section Narra GR 2015[21] 250 mg TXA Prostatectomy Hatch DM et al., 2015[22] Cesarean delivery Elkhateeb R et al., 2017[23] Elective caesarean section Table 1: Contd... Signs & symptoms Myoclonic seizures of lower extremity followed by generalized convulsion, cardiac arrest Severe pain back, gluteal region, pereneal burning radiating to lower limbs, agitation, forceful urination, severe myoclonus lower extremity and mild in upper limbs, hyperthermia, hypertension, tachycardia Severe pain back, gluteal region, lower extremity spasms, hypertension, tachycardia Management Midazolam, Phenytoin, Thiopentone General anaesthesia Sequelae Recovered in 5 days GA, dexamethasone, mannitol, Sodium valproate, CSF lavage with normal saline, thiopental infusion Polymyoclonus, Recovered with no neurological deficit on sixth day GA, amiodarone, mannitol, fentanyl, Magnesiumsulphate Refractory status epilepticus, ventricular arrhythmias Burning sensation at the site of injection, back and gluteal pain, restlessness GA, Propofol infusion, Thiopental infusion, Clonazepam, phenobarbital, DC shock Recovering but died due to interrupted Oxygen supply Recurrentpolymyoclonus and seizures, tachyarrhythmis, ventricular fibrillation death both synaptic currents and tonic inhibitory currents.[32] It is postulated that high doses of the drug would lead to massive sympathetic surge, which results in systemic hypertension and ventricular fibrillation.[19] Several general anaesthetics, including the inhalational agents as isoflurane, sevoflurane, and desflurane and the IV anaesthetic such as propofol, act as positive allosteric modulators of glycine receptors that fully reversed TXA inhibition of tonic glycine current, which may prove to be effective for either treating or preventing TXA‑associated seizures.[33,34] Prevention Drug errors may be minimised by the following procedures: (1) infrequently used emergency medications stored in a distinctive location; (2) a standardised layout of drugs which is safest in the operating room helps create a mental model that makes mistakes less likely; (3) a team‑based approach with reading aloud the drug label prior to drawing up the drug; (4) confusing medications should have different (size, color, shape) drug labels and vials; (5) continuous review of medication errors in hospitals to identify causative associated factors and systematic interventions for prevention.[4,35] Local institutions should be vigilant and aggressive in collecting data not only about negative outcomes but also about errors and near misses. A trend toward data sharing and transparency along with accessible electronic mechanisms to capture errors, mandatory critical incident reporting with a reinforcing culture can all lead to a decrease in medication errors in the future. 4 Management Currently, there are no recommended treatments for TXA‑induced seizures, however, understanding the cause of TXA‑associated seizures, recognizing the early warning signs of impending seizures, and using anaesthetic agents may reduce the incidence and severity of seizures and lead to better patient outcomes. The above case reports advocate administration of anticonvulsants including MgSO4, IV, and inhalational general anaesthetic agents, intensive haemodynamic monitoring, and CSF lavage. Continuous infusion of thiopentone to induce burst suppression pattern has been used in a patient who had refractory status epilepticus as shown on EEG.[19] Hatch et al. (2015) used magnesium sulfate as bolus dose, followed by infusion along with phenytoin which was helpful in terminating the seizure activity.[22] If the use of propofol or other anaesthetics is deemed to be unsafe or if these drugs are unavailable, alternative therapies can be considered. A second‑line treatment for TXA‑associated seizures includes compounds that increase GABA‑A receptor activity, which may compensate for a reduction in glycinergic inhibition. Benzodiazepines (lorazepam, midazolam, diazepam, and clonazepam), which do not modify glycine receptors but rather upregulate GABA‑A receptor function, have been used to treat seizures following inadvertent intrathecal injection of TXA.[36] Cerebrospinal fluid lavage After intrathecal injection of a wrong drug, immediate CSF drainage and early irrigation has been reported with good Journal of Obstetric Anaesthesia and Critical Care | Volume 8 | Issue 1 | January-June 2018 [Downloaded free from http://www.joacc.com on Saturday, August 6, 2022, IP: 14.186.209.12] Gupta, et al.: Accidental Intrathecal tranexamic acid outcomes as CSF lavage removes and dilutes the injected drug and limits the neuronal toxic damage. To avoid a higher spread of the wrong drug, maintain a head‑up position, and first aspirate CSF (with a 22 G needle), from a lower space, and then infuse crystalloids several times into the intrathecal compartment from a higher space.[14,37] 12. 13. Conclusion Recognizing the early warning signs of impending seizures, and using anaesthetics, administration of the anticonvulsants, intensive haemodynamic monitoring, scalp electroencephalography monitoring, magnesium sulfate, and CSF lavage may reduce the incidence and severity of seizures and lead to better patient outcomes. Development and promulgation of a formal protocol by every institution to prevent wrong route drug administration could further contribute to prevention of iatrogenic drug administration errors. 14. 15. 16. 17. 18. Financial support and sponsorship Nil. 19. Conflicts of interest There are no conflicts of interest. 20. References 1. Cooper L, Nossaman B. Medication errors in anaesthesia: A review. Int Anesthesiol Clin 2013;51:1‑12. 2. Wahr JA, Abernathy JH 3rd, Lazarra EH, Keebler JR, Wall MH, Lynch I, et al. Medication safety in operating room: Literature and expert‑based recommendations. Br J Anaesth 2017;118:32‑43. 3. Nanji KC, Patel A, Shaikh S, Seger DL, Bates DW. Evaluation of perioperative medication errors and adverse drug events. Anesthesiology 2016;124:25‑34. 4. Grigg EB, Roesler A. Anesthesia medication handling needs a new vision. Anesth Analg 2018;126:346‑50. 5. Roberts I, Kawahara T. Proposal for the inclusion of tranexamic acid (anti‑fibrinolytic‑lysine analogue) in the WHO model list of essential medicines. Geneva, Switzerland: World Health Organization; 2010. 6. Vogel JP, Oladapo OT, Dowswell T, Gülmezoglu AM. Updated WHO recommendation on intravenous tranexamic acid for the treatment of post‑partum haemorrhage. Lancet Glob Health 2018;6:e18‑9. 7. Wong JO, Yang SF, Tsai MH. Accidental injection of tranexamic acid (Transamin) during spinal anesthesia. Ma Zui Xue Za Zhi 1988;26:249e252. 8. De Leede‑van der Maarl MG, Hilkens P, Bosch F. The epileptogenic effect of tranexamic acid. J Neurol 1999; 246:843. 9. Yeh HM, Lau HP, Lin PL, Sun WZ, Mok MS. Convulsion and refractory ventricular fibrillation after intrathecal administration of a massive dose of tranexamic acid. Anesthesiology 2003;98:270‑2. 10. Sabzi F, Teimouri H, Zokai A. Myoclonus, seizure, and ventricular fibrillation after intrathecal injection of tranexamic acid. J Tehran Univ Heart Cent 2009;4:253‑5. 11. Mohseni K, Jafari A, Nobahar MR, Arami A. Polymyoclonus 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. seizures resulting from accidental injection of tranexamic acid in spinal anesthesia. Anaesth Analg 2009;108:1984‑6. Veisi F, Salimi B, Mohseni G, Golfam P, Kolyaei A. Accidental intra‑thecal injection of tranexamic acid for caesarean section: A fatal medication error. Anaesthesia Patient Safety Foundation Journal. Newsletter 2010;25:9. Kaabachi O, Eddhif M, Rais K, Zaabar MA. Inadvertent intrathecal injection of tranexamic acid. Saudi J Anaesth 2011;5:90‑2. Butala BP, Shah VR, Bhosale GP, Shah RB. Medication error: Subarachnoid injection of tranexamic acid. Indian J Anaesth 2012;56:168‑70. Mahmoud K, Ammar A. Accidental intrathecal injection of tranexamic acid. Case Rep Anesthesiol 2012;2012:646028. Srivastava U, Joshi K, Gupta A, Chauchan N, Dupargude A, Saxena A. Accidental injection of tranexamic acid into subarachnoid space leading to fatal outcome. Internet J Anaesth 2012;30. Raghu K, Shrevanni P, Haneef M, Ramyakumar, Chenna Rao M. Accidental intrathecal injection of tranexamic acid in a term gestation. Int J NeuSpi Sci 2013;1:1-3. Antwi‑Kusi A, Sam Awortwi W, Serwaa Hemeng A. Unusual complication following spinal anesthesia for caesarean section. Open J Anesthesiol 2013;3:275‑7. Goyal G, Vajpayee A, Rama Kant, Singh R. Refractory status epilepticus after accidental intrathecal injection of tranexamic acid. J Acute Med 2014;4:92‑4. Roy A, Sarkar S, Thakur SB, Jain PK. Inadvertent intrathecal administration of Tranexamic acid in a case of caesarean section: A report of medication error. Southeast Asian J Case Rep Rev 2015;4:1910‑6. Narra GR. Accidental injection of tranexamic acid into intrathecal space. J Res Anaesthesiol Pain Med 2015;1:12‑4. Hatch DM, Atito‑Narth E, Herschmiller EJ, Olufolabi AJ, Owen MD. Refractory status epilepticus after inadvertent intrathecal injection of tranexamic acid treated by magnesium sulfate. IntJ Obstet Anesth 2015;26:71‑5. Elkhateeb R, Kamel HH. Intrathecal injection of tranexamic acid during caesarean section: Accidental fatal mistake. J Clin Obstet Gynecol Infertil 2017;1:1014. Henry DA, Carless PA, Moxey AJ, O’Connell D, Stokes BJ, McClelland B, et al. Anti‑fibrinolytic use for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst Rev 2007;3:CD001886. Tovi D, Thulin CA. Ability of tranexamic acid to cross the blood‑brain barrier and its use in patients with ruptured intracranial aneurysm. Acta Neurol Scand 1972;48:257. Garcha PS, Mohan CV, Sharma RM. Death after an inadvertent intrathecal injection of tranexamic acid. Anesth Analg 2007;104:241‑2. Ohashi N, Sasaki M, Ohashi M, Kamiya Y, Baba H, Kohno T, Tranexamic acid evokes pain by modulating neuronal excitability in the spinal dorsal horn. Scientific Reports, 2015; 5:13458/DOI 10.1038/13458. Sharma V, Katznelson R, Jerath A, Garrido‑Olivares L, Carroll J, Rao V, et al. The association between tranexamic acid and convulsive seizures after cardiac surgery: A multivariate analysis in 11,529 patients. Anaesthesia 2014;69:124‑30. Schlag MG, Hopf R, Zifko U, Redl H. Epileptic seizures following cortical application of fibrin sealants containing tranexamic acid in rats. Acta Neurochir (Wien) 2002;144:63‑9. Yamaura A, Nakamura T, Makino H, Hagihara Y. Cerebral complication of antifibrinolytic therapy in the treatment of ruptured intracranial aneurysm. Animal experiment and a review Journal of Obstetric Anaesthesia and Critical Care | Volume 8 | Issue 1 | January-June 2018 5 [Downloaded free from http://www.joacc.com on Saturday, August 6, 2022, IP: 14.186.209.12] Gupta, et al.: Accidental Intrathecal tranexamic acid of literature. Eur Neurol 1980;19:77‑84. 31. Furtmuller R, Schlag MG, Berger M, Hopf R, Huck S, Sieghart W, et al. Tranexamic acid, a widely used antifibrinolytic agent, causes convulsions by a gamma‑aminobutyric acid (A) receptor antagonistic effect. J Pharmacol Exp Ther 2002;301:168‑73. 32. Lynch JW. Native glycine receptor subtypes and their physiological roles. Neuropharmacology 2009;56:303‑9. 33. Downie DL, Hall AC, Lieb WR, Franks NP. Effects of inhalational general anaesthetics on native glycine receptors in rat medullary neurons and recombinant glycine receptors in Xenopus oocytes. Br J Pharmacol 1996;118:493‑502. 6 34. Hales TG, Lambert JJ. The actions of propofol on inhibitory amino acid receptors of bovine adrenomedullary chromaffin cells and rodent central neurones. Br J Pharmacol 1991;104:619‑28. 35. Patel S, Loveridge R. Obstetric neuraxial drug administration errors: A quantitative and qualitative analytical review. Anesth Analg 2015;121:1570‑7. 36. Tan KR, Rudolph U, Luscher C. Hooked on benzodiazepines: GABA‑A receptor subtypes and addiction. Trends Neurosci 2011;34:188‑97. 37. Tsui BC, Malherbe S, Koller J, Aronyk K. Reversal of an unintentional spinal anesthetic by cerebrospinal lavage. Anesth Analg 2004;98:434‑6. Journal of Obstetric Anaesthesia and Critical Care | Volume 8 | Issue 1 | January-June 2018