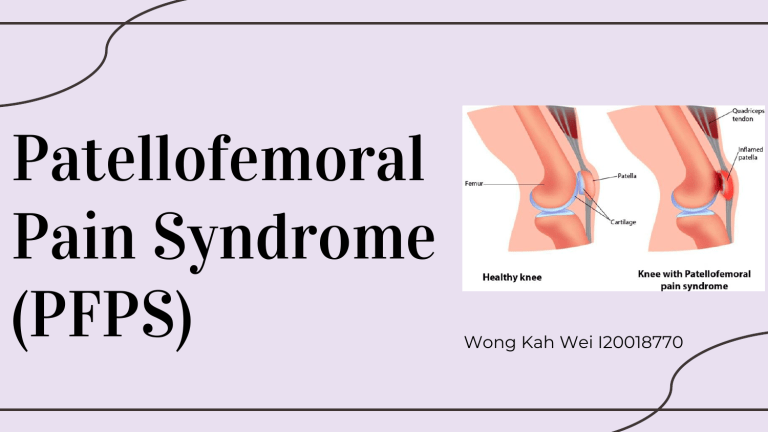
Patellofemoral Pain Syndrome (PFPS) Wong Kah Wei I20018770 Introduction to PFPS - Patellofemoral joint is the most heavily loaded joint and its articular cartilage is the thickest - Also known as Runner’s Knee, PFPS is a one of the most common causes of anterior knee pain located behind (retropatellar) or around the patella (peripatellar) - The onset of knee pain can be gradual or sudden with worsening of pain by loading a flexed knee joint, such as running, walking up or down stairs, prolonged sitting, jumping, or squatting (Kooiker, Van De Port, Weir, & Moen, 2014) - Symptoms can cause participation restriction in physical activity, sports, and work, as well as recur and persist for years (Willy et al., 2019) (Bump & Lewis, 2022) (Kooiker, Van De Port, Weir, & Moen, 2014) Pathophysiology - Multifactorial: overactivity and overload of patellofemoral joint as well as muscle and tissue imbalances (hip abductor weakness), results in improper tracking of patella in trochlear groove (malalignment- increased hip adduction angles) in knee flexion and extension as well as increased stress at the patellofemoral joint. - Microdamage, inflammation and pain at the cartilage and subchondral bone occurs - Heino Brechther and Powers (2002) proved that patients with PFPS have increased patellofemoral joint stress which causes increased cartilage and subchondral bone stress, eventually leading to damage and pain over time. - Other causes: Direct or indirect injuries to the patellar area (lateral retinaculum, synovium, medial patellofemoral ligament), acute and chronic subluxation/ dislocation of patella (patellar instability) (Bump & Lewis, 2022) Clinical Features 01 03 05 Dull, aching pain at the anterior knee, especially when walking stairs, kneeling, squatting or prolonged sitting w/ bent knee Reduced patellar mobility Increased quadriceps angle 02 Patellofemoral crepitation 04 Squinting patella (patella pointing inwards) 06 Lateral and medial retinacular tenderness (Bump & Lewis, 2022) Risk factors (DIXIT, DIFIORI, BURTON, & MINES, 2007b) Differential Diagnosis - Patellofemoral OA - Osgood Schlatter's disease - Plica - Bursitis (prepatellar or Hoffa's) - Saphenous neuritis - Quadriceps tendinopathy - Patellar tendinopathy - Referred pain from hip or back (Bump & Lewis, 2022) Epidemiology - In active individuals, it may account for 25% to 40% of all knee problems - According to studies, PFPS affects women more than men at a ratio of close to 2:1 - Age of occurrence is typically seen in adolescents (Prevalence> 20%) and adults in 20s and 30s. (Bump & Lewis, 2022) Case Study Demographic Data - Name: Ms S - Age: 42 - Gender: Female - Race: Indonesian - Occupation: School Cleaner - Dr Diagnosis: PFPS - Dr Mx: Conservative (Refer to PT) - Date of Ax: 27/2/2023 - Date of Referral: 27/2/2023 Subjective Ax - Chief complaint: pt c/o pain at the front knee on the Rt side - Current Hx: pt has pain at the anterior knee since 3/52. She feels pain when sitting up from bed and bending knee even after putting ointment. After prolonged walking, she feels pain and heard crepitus sound. She visited Dr today, previously she is just enduring pain. - Past Hx: pt has been admitted to hospital in Dec 2022 d/t mini stroke - Medical Hx: High cholesterol, DM, HPT - Medications: For High cholesterol, DM, HPT - Surgical Hx: NIL Subjective Ax - Family Hx: NIL - Investigation: NIL - Environmental Hx: - - Need to use sit toilet at home d/t difficulty in squatting - Need to walk 3 flight of stairs at school, walk step by step and holding the rails - Need to stop work if she feels pain/ tired Social Hx: - Married, has 4 kids - Non-smoker, doesn’t drink - Hobby: jogging (4-5 rounds/ day, but stop jogging recently d/t anterior knee pain) - Fall Hx: NIL - Expected outcome: - To reduce pain - To get back to work w/o pain Pain Ax - Side & site: Rt side anterior knee - Onset: 3/52 ago, sudden - Type: Pin-prick sensation - Radiation: Pain radiates to Rt buttocks & toes - Aggravating factor: Knee flexion - Relieving factor: Ointment - 24 Hrs: Throughout the day - VAS: Current 6, Aggravating 8, Relieving 4 - Irritability: High - Severity: High - Associated symptom: NIL Objective Ax General observation - A middle-aged woman walks in independently w/o walking aids but w/ antalgic gait - Body built: Mesomorph - External appliances: NIL - Deformity: NIL - Posture: - Lateral view: Rounded shoulder, Anteriorly tilted pelvis, Forward head posture - Anterior view: Knock knee - Posterior view: Normal Objective Ax Local observation - Skin changes: No signs of inflammation - Scar: NIL - Muscle palpation: - G1 tenderness at Rt quadriceps - No swelling - No warmth - Muscle tightness: Rt gluteus medius & piriformis - Swelling measurement: NIL - Gait: pt walks w/ antalgic gait d/t pain at Rt anterior knee, loss of heel strike and knee flexion at Rt foot Objective Ax Examination-ROM ROM Left End Feel AROM PROM Knee flexion 0-131 0-135 Knee extension 131-0 - Right End Feel AROM PROM Firm 0-121 0-123 Hard 121-0 - Empty Hip flexion Hip extension AFROM Firm AFROM Firm Objective Ax Examination-ROM ROM Left AROM Ankle dorsiflexion Ankle plantarflexion End Feel PROM AFROM Right AROM Firm End Feel PROM AFROM Firm Objective Ax Examination- MMT Left Right Knee flexorHamstring G5 G5 but w/ pain Knee extensionQuadriceps G5 G5 Objective Ax Examination- Special Test - +ve Clarke Test on Rt side: pain at base of patella - +ve Ober’s Test on Rt side: ITB tightness on Rt side - +ve Patella Tilt Test on Rt side: pain w/ crepitus when gliding patella superiorly and inferiorly Examination- Special Test - Balance: Good (able to hold more than 5 seconds in single leg stance test) Analysis Impairments - Pain at the Rt anterior knee d/t knee movt (flexion and extension) - Reduced AROM of Rt knee flexion d/t pain at the Rt anterior knee Activity limitation - Difficulty in bending the knee - Difficulty in prolonged walking - Difficulty in sitting up from bed - Difficulty in squatting Analysis Participation Restriction - Difficulty in walking stairs in school during work - Difficulty in jogging for 4-5 rounds/day - Difficulty in praying STG - To reduce pain at Rt anterior knee from 6/10 to 3/10 *3/7 - To increase AROM of Rt knee flexion by 5 degrees *3/7 Analysis LTG - Improve gait pattern w/ proper heel strike and knee flexion * 1/12 - Improve ability to do school work w/o knee pain & tiredness * 2/12 - Improve ability to sit up from bed w/o pain * 2/12 PT’s impression: PFPS on Rt side d/t pain at Rt anterior knee & limited Rt knee flexion AROM Plan of Tx - Pain Mx - Stretching exs - Myofascial release - Strengthening exs - Gait training - Posture correction - Trunk stability exs - HEP - Pt’s education (Petersen et al., 2013) Precautions & contraindications Precautions - Monitor the BP level throughout the treatment session - Always ask for patient’s consent prior to any intervention - Maintain a comfortable environment free from any obstruction and distraction - Consider the risk of fall/ injury during treatment - Check patient’s sensation before applying hot pack as patient has diabetes Contraindications - Stop exercise if patient c/o dizziness or worsening pain - Don't apply hot pack if patient has open wound, dermatitis, deep vein thrombosis etc. Intervention: Myofascial release (MFR) - Aim: To release tightness and pain throughout the myofascial tissues in order to eliminate pain and improve motion - pt position: Side and supine lying - Procedure: PT uses elbow to release Rt gluteus medius and piriformis (in side lying) and Rt quadriceps (in supine lying) for 10 minutes - In combine with exercise therapy (stretching and strengthening exercises for the lower extremity), MFR has demonstrated superior improvement demonstrating in reducing pain and improving functional activity in patients with patellofemoral pain syndrome by releasing the interconnected fascia that corrects lower extremity kinematics. (De Souza & Kumar G., 2020) Intervention: Hot pack - Aim: To reduce pain and muscle tightness over the Rt anterior knee - pt position: supine lying - Procedure: Hot pack is placed over the Rt anterior knee for 10 minutes - According to Malanga, Yan, & Stark, 2015, the physiological effects of heat therapy include pain relief and increases in blood flow, metabolism, and elasticity of connective tissues, thus provides short-term reductions in pain and disability and significant pain relief Intervention: Stretching exs - Aim: To improve the muscle flexibility of the tight muscles - pt position: prone & supine lying - Procedure: - Rt Quadriceps: In prone lying, PT supports pt’s Rt leg and bend the knee to full range for 15 seconds hold, 4 repetitions and 3 sets/ day - Rt Hamstring: In supine lying, pt’s knee is straight and Rt leg is lift to full range for 15 seconds hold, 4 repetitions and 3 sets/ day - In patients with PFPS who have inflexible hamstrings, dynamic hamstring stretching with strengthening exercises was superior for improving muscle activation time compared with static hamstring stretching with strengthening exercises. (Lee, Jang, Kim, Rhim, & Kim, 2020) - Stretching exercises for the muscles of the knee and hip also improved the function, pain and range of motion of PFPS patients. (Alba-Martín et al., 2015) Intervention: HEP - Aim: To educate patient on exercise that can be done at home - pt position: standing & supine lying - Procedure: - Rt Quadriceps: In standing, pt bends the Rt knee to the buttocks and bring the leg backward with body straight for 15 seconds hold, 4 repetitions and 3 sets/ day - Rt Hamstring: In supine lying, pt’s knee is straight and Rt leg is lift as high as possible with a pull of a towel at the Rt ankle for 15 seconds hold, 4 repetitions and 3 sets/ day - In a 12-week home exercise therapy program, Pain and function improved significantly after a home exercise therapy program in patients with patellofemoral pain syndrome. In addition, patients with a delayed onset or reduced activity of the vastus medialis compared to the vastus lateralis experienced a reduction in this imbalance. (Kölle, Alt, & Wagner, 2020) Intervention: pt education - Reduce any activity that has hurt the knees in the past - Maintain a healthy body weight to avoid overstressing the knees - Take rest in between knee movements such as walking stairs and prolonged walking (Patellofemoral Pain Syndrome - OrthoInfo - AAOS, 2020) Evaluation - VAS is reduced from 6/10 to 2/10 - Increased AROM of Rt knee flexion ROM Left End Feel AROM PROM Knee flexion 0-131 0-135 Knee extension 131-0 - Right AROM End Feel PROM Firm Hard Firm AFROM Hard Hip flexion Hip extension AFROM Firm AFROM Firm Review - TCA: 6/3/2023 2pm - Check calf tightness - Quadriceps strengthening - Outcome Measure: Knee injury and Osteoarthritis Outcome Score Patellofemoral subscale (KOOS-PF) Follow up- 6/3/2023 2pm - Chief complaint: pt c/o knee pain at the outer part of the patella since 2/7, but pain is lesser (VAS 4/10) - Current Hx: Pain felt when squatting, knee flexion at the mid range from knee extension (pop sound is heard) and rotating body to the Rt - AROM on the Rt knee has improved ROM Left AROM Knee flexion Knee extension End feel PROM Right AROM PROM Firm AFROM Hard End feel Firm AFROM Hard Follow up- 6/3/2023 2pm (cont’d) - Muscle power still remain constant - Rt vastus lateralis, gluteus medius and piriformis are tight Intervention: hot pack, myofascial release, stretching, strengthening Intervention: Myofascial release (MFR) - Aim: To release tightness and pain throughout the myofascial tissues in order to eliminate pain and improve motion - pt position: Side and supine lying - Procedure: PT uses elbow to release Rt gluteus medius and piriformis (in side lying) and Rt quadriceps (in supine lying) for 10 minutes - In combine with exercise therapy (stretching and strengthening exercises for the lower extremity), MFR has demonstrated superior improvement demonstrating in reducing pain and improving functional activity in patients with patellofemoral pain syndrome by releasing the interconnected fascia that corrects lower extremity kinematics. (De Souza & Kumar G., 2020) Intervention: Hot pack - Aim: To reduce pain and muscle tightness over the Rt anterior knee - pt position: supine lying - Procedure: Hot pack is placed over the Rt anterior knee for 10 minutes - According to Malanga, Yan, & Stark, 2015, the physiological effects of heat therapy include pain relief and increases in blood flow, metabolism, and elasticity of connective tissues, thus provides short-term reductions in pain and disability and significant pain relief Intervention: Stretching - Quadriceps - In standing, pt bends the Rt knee to the buttocks and bring the leg backward with body straight for 15 seconds hold, 4 repetitions and 3 sets/ day - Calf - In standing, pt’s hands are on the wall and Rt leg backwards, then lean the body towards the wall for 15 seconds hold, 4 repetitions and 3 sets/ day - Gluteus maximus - In supine, pt bends the Rt hip and knee maximally towards the chest for 15 seconds hold, 4 repetitions and 3 sets/ day Intervention: Stretching - Gluteus medius - In supine, pt bends the Rt hip and knee maximally towards the Lt shoulder for 15 seconds hold, 4 repetitions and 3 sets/ day - Piriformis - In sitting, pt bend the Rt leg to Lt leg above the knee, hold it w/ both hands and bend body forward for 15 seconds hold, 4 repetitions and 3 sets/ day Intervention: Strengthening - Aim: To strengthen the lower limb muscles, especially the quadriceps to eliminate pain and improve function - pt’s position: crook lying and sitting - Procedure: - Pelvic bridging: In a crook lying position, pt engage the abdominal and gluteal muscles and lift the hips until the knees are aligned with the shoulders for 10 seconds hold, 10 times and 3 sets/day - VMO strengthening: In a sitting position, pt place a ball between the thighs and squeeze the ball to activate VMO for for 10 seconds hold, 10 times and 3 sets/day - According to Kooiker, Van De Port, Weir, and Moen (2014), isolated quadriceps strengthening (non–weight bearing and weight bearing, general versus selective VMO training) for 3 times per week is proven to be effective for PFPS Tx. Evaluation - VAS is reduced from 4/10 to 3/10 - Patient is alert and cooperative - Patient felt muscle soreness during strengthening exercises Review - TCA: 20/3/2023 2pm - More quadriceps strengthening exercises: squat (double leg and single leg), clam exercise - Vastus lateralis and ITB strengthening References Alba-Martín, P., Gallego-Izquierdo, T., Plaza-Manzano, G., Romero-Franco, N., Núñez-Nagy, S., & Pecos-Martín, D. (2015). Effectiveness of therapeutic physical exercise in the treatment of patellofemoral pain syndrome: a systematic review. Journal of Physical Therapy Science, 27(7), 2387–2390. https://doi.org/10.1589/jpts.27.2387 Bump, J. M., & Lewis, L. (2022, February 18). Patellofemoral Syndrome. Retrieved March 5, 2023, from Nih.gov website: https://www.ncbi.nlm.nih.gov/books/NBK557657/ De Souza, I. G., & Kumar G., P. (2020). Effect of Releasing Myofascial Chain in Patients with Patellofemoral Pain Syndrome - A Randomized Clinical Trial. International Journal of Current Research and Review, 12(08), 05-10. https://doi.org/10.31782/ijcrr.2020.12082 DIXIT, S., DIFIORI, J. P., BURTON, M., & MINES, B. (2007). Management of Patellofemoral Pain Syndrome. American Family Physician, 75(2), 194–202. Retrieved from https://www.aafp.org/pubs/afp/issues/2007/0115/p194.html HEINO BRECHTER, J., & POWERS, C. M. (2002). Patellofemoral stress during walking in persons with and without patellofemoral pain. Medicine & Science in Sports & Exercise, 34(10), 1582–1593. https://doi.org/10.1097/00005768-200210000-00009 Kölle, T., Alt, W., & Wagner, D. (2020). Effects of a 12-week home exercise therapy program on pain and neuromuscular activity in patients with patellofemoral pain syndrome. Archives of Orthopaedic and Trauma Surgery, 140(12), 1985–1992. https://doi.org/10.1007/s00402-020-03543-y Kooiker, L., Van De Port, I. G. L., Weir, A., & Moen, M. H. (2014). Effects of Physical Therapist–Guided Quadriceps-Strengthening Exercises for the Treatment of Patellofemoral Pain Syndrome: A Systematic Review. Journal of Orthopaedic & Sports Physical Therapy, 44(6), 391-B1. https://doi.org/10.2519/jospt.2014.4127 Lee, J. H., Jang, K.-M., Kim, E., Rhim, H. C., & Kim, H.-D. (2020). Effects of Static and Dynamic Stretching With Strengthening Exercises in Patients With Patellofemoral Pain Who Have Inflexible Hamstrings: A Randomized Controlled Trial. Sports Health: A Multidisciplinary Approach, 13(1), 49–56. https://doi.org/10.1177/1941738120932911 Malanga, G. A., Yan, N., & Stark, J. (2015). Mechanisms and efficacy of heat and cold therapies for musculoskeletal injury. Postgraduate Medicine, 127(1), 57–65. https://doi.org/10.1080/00325481.2015.992719 Patellofemoral Pain Syndrome - OrthoInfo - AAOS. (2020). Aaos.org. https://orthoinfo.aaos.org/en/diseases--conditions/patellofemoral-pain-syndrome/ Patellofemoral Pain Syndrome | NHS Lanarkshire. (2021). Retrieved March 5, 2023, from Scot.nhs.uk website: https://www.nhslanarkshire.scot.nhs.uk/services/physiotherapy-msk/patellofemoral-pain-syndrome/ Petersen, W., Ellermann, A., Gösele-Koppenburg, A., Best, R., Rembitzki, I. V., Brüggemann, G.-P., & Liebau, C. (2013). Patellofemoral pain syndrome. Knee Surgery, Sports Traumatology, Arthroscopy, 22(10), 2264–2274. https://doi.org/10.1007/s00167-013-2759-6 Willy, R. W., Hoglund, L. T., Barton, C. J., Bolgla, L. A., Scalzitti, D. A., Logerstedt, D. S., … McDonough, C. M. (2019). Patellofemoral Pain. Journal of Orthopaedic & Sports Physical Therapy, 49(9), CPG1–CPG95. https://doi.org/10.2519/jospt.2019.0302


