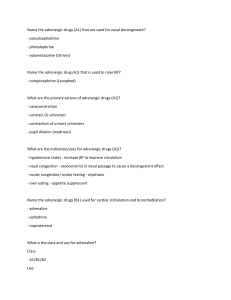
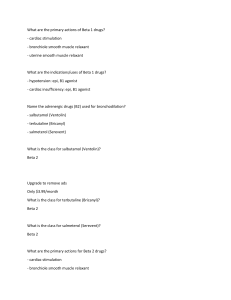
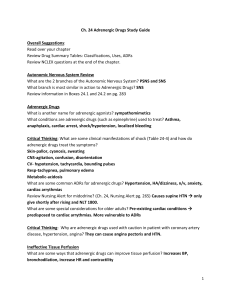
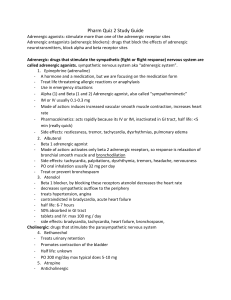
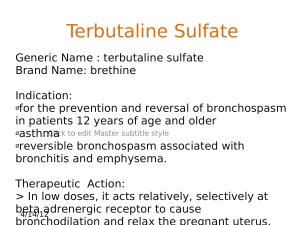
Type Subtype Name Mechanism of action Effect Theraputic use ADR Extra Adrenergic agonist Direct Non-selective Epinephrine α1, α2, β1, β2 Bind to adrenergic receptors SNS activity. CVS: *β1-↑Chronotropic and inotropic effects *β2-vasodilation in muscles. *α1-vasoconstriction. *systolic↑ diastolic ↓. Bronchidialtion(β2) Hyperglycemia: *insulin↓ (α2) *gluconeogenesis(β2) Lipolysis (β3) *Cerebral hemorrhage. *Arrhythmias. *Anxiety. *Tremors. *Headaches. *Pulmonary edema. *Rapid inactivation by COMT & MAO. *Poor penetration to CNS due to polarity. Adrenergic agonist Direct Non-selective Norepinephrine α1, α2, β1 Bind to α1, α2, β1 receptors CVS ↑systolic & diastolic *no β2 for vasodilation. * β1↑intropic effect. *α1↑peripheral resistance. *Anaphylectic shock. *Cardiac errest. *Stop bleeding. (vasoconstriction) *Prolong anesthesia. *Open eye glaucoma (α1 ↓aqueous humor production through vasoconstriction of ciliary body blood vessels). *Hypotension. *Septic shock. *Arrhythmias. *↑BP *Tissue necrosis. *Vasospasms. *Rapid inactivation by COMT & MAO. *Poor penetration to CNS due to polarity. Adrenergic agonist Direct Non-selective Isoproterenol β1, β2 Bind to β1, β2 receptors. CVS:↑diastolic & systolic moderately. *β1-↑Chronotropic and inotropic effects. *β2-vasodilation in muscles. Bronchidialtion(β2) *Bradycardia. *AV block. *Asthma (rare). Adrenergic agonist Direct Selective α2 Apraclonidine Bind to α2 receptors (imidazole type). Act on ocular α2 receptors (inhibit ciliary epithelium aqueous humor production↓) Glaucoma *Cerebral hemorrhage. *Arrhythmias. *Anxiety. *Tremors. *Headaches. *Pulmonary edema. negligible Adrenergic agonist Direct Selective β2 -Terbutaline -Salmeterol -Albuterol Bind to β2 receptors. Bronchodilation T&A: Acute bronchospasm & COPD. S: nocturnal bronchospasm. *Hyperglycemia. *Tremor & anxiety. *Tachycardia & arrhythmias (can also stimulate a bit of β1). *Not inactivated by COMT and poor inactivation by MAO. *Penetrate to CNS due lipophilicity. *Administration: topical ocular *Doesn’t penetrate BBB. T&A: oral/SC/inhalation,rapi d onset, last for 3-6 hours. S: powder inhalation, longer onset, long duration (more than 12 hours). Type Subtype Name Mechanism of action Effect Theraputic use ADR Extra Adrenergic agonist Direct Selective α2 Clonidine Bind to α2 receptors (imidazole type). *CNS: bind to locus ceruleus ↓BP. *SNS: ↓ NE release from postganglionic sympathetic nerves. *PNS: ↑ tone. Direct Selective β1 Dobutamine Bind to β1 receptors. ↑ Chronotropic and inotropic effects. *Hypotension. *Dry mouth. *Sedation. *Sexual dysfunction. *Bradycardia. *Withdrawal (after long use). *Arrhythmias. *Do not metabolize by COMT long action. *Oral / IV. Adrenergic agonist *Hypertension. *Rehab from opoids (act on receptors which produce morphine-like effects). *Cardiogenic shock. *Acute HF. Adrenergic agonist Direct Selective α1 Phenylephrine Bind to α1 receptors. *↑ peripherial resistance, DBP, SBP may induce reflax bradycardia. *Mucous vasoconstriction. *Hypotension. *Supraventricul ar tachycardia. *↓ Nasal& ocular congestion. *Cause mydriasis. *Hypertension. *Stroke. *HF. *Mixed acting (direct + indirect) *Non-selective (D1&D2 >β>α) Dopamine Small: SBP ↑ (DBP no change). Medium: ↑HR Large: constriction of BV ↑ peripheral resistance. *cardiogenic & septic & hypovolemic shocks (dopamine has also receptors in the kidney cause vasodilation don’t damage it) *Hypertension. *Arrhythmia. *Nausea. Adrenergic agonist Small dose (D&β2): renal vasodilation. Medium dose (D&β): ↑ Chronotropic and inotropic effects. Large dose (D&β&α1): vasoconstriction. ↑ NE release from adrenergic neurons. *Doesn’t metabolize by COMT, only by MAO & in the liver longer life span. Type Subtype Name Mechanism of action Effect Theraputic use ADR Extra Adrenergic agonist *Mixed acting (direct + indirect) *Non-selective Ephedrine Activate adrenergic receptors. *↑SNS. *Constrict BV and ↑HR DBP&SBP ↑ *Bronchodilation. *Slight stimulation of CNS (↑vigorous) *Tachycardia. *BP ↑. *Insomenia. *Urinary retention. Lipid soluble penetrate the CNS and absorbed well in the intestine. Adrenergic agonist Indirect – releasing agent Amphetamine *Stimulate intracellular secretion of catecholamines from vesicles. *Competitive inhibitor of catecholamine reuptake by DAT & NET. ↑ Cateocholamis in the synaptic cleft. Replace stored catecholamines. *CNS stimulation. *Vadoconstriction ↑BP. *↑ HR. *Bladder sphincter constriction. *Pseudoephedri ne – mixture for nasal, sinus and eustachian congestion. *Methampheta mine (illegal) *ADD *Urinary incintinence. *Anorexiant. *Narcolepsy. ↑BP Non *Hypertension. *Arrhythmia. *Stroke. *Drug of abuse – addiction. *Seizures. *Mucous ischemia and necrosis. *Hypertension. *Arrhythmia. Adrenergic agonist Indirect – releasing agent Tyramine Adrenergic agonist Indirect – reuptake inhibitor Cocaine Block NET&DAT no reuptake of dopamine & NE. *Vasoconstriction. *↑BP. *Local anesthesia. Adrenergic antagonist Inhibitor of adrenergic transmission Metyrosine Competitive inhibitor of tyrosine hydroxylase ↓ production of catecholamines. ↓ production of catecholamines. *Pheochromacy toma. *Control dyskinesia. *Hypertension. *Addictive. *Aggression. *Paranoia. *Act mainly in the CNS. *Oral / parental *Inactivated by MAO in the GIT & Liver. *Tyramine is found in foods: cheese, banana & Chianti red wine. Type Subtype Name Mechanism of action Effect Theraputic use ADR Adrenergic antagonist Inhibitor of adrenergic transmission Reserpine Inhibit VMAT irreversibly catecholamines are not being kept in vesicles degradation by MAO. ↓ SNS tone *Hypertension. Severe depression. Adrenergic antagonist Inhibitor of adrenergic transmission Guanethidine Displace with NE inside vesicles NE depletion (only in neuron terminals, and not in all CNS) destroy adrenergic neurons. *↓Vasoconstriction. *↓ HR Hypertension *Hypotension. *Sexual dysfunctions. *Diarrhea. *Nasal congestion. Adrenergic antagonist Non-selective α blockers Phentolamine Competitive antagonist of α receptor. ↓ Vasoconstriction ↓ BP. *Pheochromacy toma. *Antidote for α agonists. *Reflex tachycardia (↓ α2 also). *Postural hypotension. *Sexual dysfunction. *Vertigo. Adrenergic antagonist Non-selective α blockers Phenoxybenzami ne Irreversible (covalent) binding to α receptor. ↓ Vasoconstriction ↓ BP. *Pheochromacy toma. *Raynaud’s phenomenon (arterial spasms) *Reflex tachycardia (↓ α2 also). *Postural hypotension. *Sexual dysfunction. *Vertigo. Adrenergic antagonist Non-selective β blockers Propranolol Competitive antagonist of β receptor. *↓ Chronotropic and inotropic effects O2 demend ↓. *BP ↓ *↓ Renin secretion. *Hypertension. *Thyrotoxicosis (cause high BP) *Angina pectoris. *Pheochromacy toma. *Acute MI. *Tremor. *Anxiety. *Migraine. *Glaucoma *Angina pectoris. *Hypertension. *Migraine. *Bronchospasm. *Sexual impairment. *CNS sedation. *AV block. *HF. *Cold hands. *Fatigue. Adrenergic antagonist Non-selective β blockers Timolol Competitive antagonist of β receptor. *↓ Chonotropic and intropic effects O2 demend ↓. *↓ Renin secretion. *↓ IOP *AV block. *HF. *CNS sedation. *Bronchospasms. *Cold hands. Extra *Oral / topical. *2 hours half life (short). *Oral/IV *Half-life: 4 hours. Type Subtype Name Mechanism of action Effect Theraputic use ADR Extra *Fatigue. *Bradyarrhythmia. *Hypotension. *Fatigue. *oral *5-8 hours effect *Low lipid soluble. Adrenergic antagonist Selective β1 blockers Atenolol Competitive antagonist of β1 receptor. *↓ Chronotropic and inotropic effects O2 demand ↓. *BP ↓ *Angina pectoris. *Acute MI. *Hypertension. Adrenergic antagonist Selective β1 blockers Esmolol Competitive antagonist of β1 receptor. *↓ Chronotropic and inotropic effects O2 demand ↓. *BP ↓. *Thyrotoxic crisis. *Acute supraventricular tachycardia. *Bradyarrhythmia. *Hypotension. *Fatigue. Adrenergic antagonist Non selective α&β blockers Labetalol Competitive antagonist of α&β receptor. ↓ in BP: *Vasodilation. *↓ Chronotropic and inotropic effects. ↓ in BP: *Vasodilation. *↓ Chronotropic and inotropic effects. ↑ CO (in HF patients). *Hypertensive emergencies. *Hypotension. *Bronchoconstriction. *Hepatic injury. Adrenergic antagonist Non selective α&β blockers Carvediol Competitive antagonist of α&β1 receptor. *Hypertension. *HF. *Bradyarrhythmia. *Hypotension. *Fatigue. *IV *Low lipid soluble. *Very fast onset. Oral / IV *Oral *Very short half life (10 min)