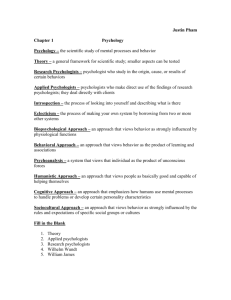
Review Paper a) Treatment combined modalities for individuals with Nicotine Addiction At present, Tobacco use is a global pandemic that is nonnegligible. With 5 million tobaccorelated deaths annually, which are mainly caused by lung cancer, stroke, coronary heart disease, and chronic obstructive pulmonary disease (Casella et al., 2010). The modalities for treating nicotine addiction in tobacco users includes numerous methods such as pharmacotherapy (Nicotine Replacement therapy, Bupropion, and Varenicline) and evidencebased recommendation such as cognitive-behavioral therapy (CBT), or a combination of both methods. A study conducted by Evins et al., (2014) showed that the combined modality treatment for nicotine addiction patients including maintenance pharmacotherapy with varenicline and cognitive behavioral therapy is effective in improving prolonged tobacco abstinence rates. As a result, researchers found that participants who involved in the combination of maintenance therapy and cognitive behavioral therapy for one year showed a less relapse rate of 35% after the termination of a 12-week intervention, suggesting that this approach is effective and feasible in patients with nicotine addiction (Evins et al., 2014). Other than that, another study conducted by Pachas et al., (2012) showed a result that the combination of varenicline and cognitive behavioral therapy had an observed significant improvement from baseline to week 12 or early termination in terms of nicotine withdrawal symptoms (individual subscales of urge to smoke, anxiety, depression, irritability, and concentration). Moreover, according to Fouz-Rosón and colleagues (2017), their study showed that a high intensity cognitive behavioral therapy is believed to significantly contribute to the success of the pharmacologic therapy with varenicline in balancing the efficacy and low adherence rates effectively. Another recent study conducted by Arslan et al., (2021) found a significantly high number and percentage of quitting smoking rate in participants who received combined treatment of varenicline and CBT. Although many recent studies showed the effectiveness of combined modality treatment for treating nicotine addiction including varenicline and cognitive behavioral therapy, a study conducted by Laude and colleagues (2017) has underpinned the controversy. Results of the study showed that there was a lack of effectiveness of extended-CBT treatment combined with varenicline in a smoking cessation program for patients with nicotine addiction. It might be due to the intensive, regular, in-person CBT over six months produced treatment fatigue and declined returns of the on-going treatment (Laude et al., 2017). Laude and colleagues (2017) were then concluded that CBT treatment which combined with pharmacologic treatment such as varenicline exceeded 26 weeks does not escalate long-term abstinence rates, could be explicated by declined commitment caused by treatment fatigue. Similarly, Windle et al., (2016) reviewed that higher-intensity CBT (i.e., individual, group, or telephone therapy) do not improve the abstinence in individuals prescribed varenicline as compared to minimal clinical intervention. Hence, the researchers did not find strong evidence that CBT is necessary to attach with pharmacotherapy (Windle et al., 2016). Nonetheless, García-Gómez et al., (2019) concluded that combined treatment for smoking cessation might be quite effective in the short term, but the abstinence rates are disappointing in the following year. b) Prescription privileges to clinical psychologists Ever since psychology became a scientific profession, it continues to evolve and grow. Over the past decade, arguments exist in the clinician's community regarding the prescription privileges of clinical psychologists (Whitaker, 2016). The researcher stated that if clinical psychologists were given the privileges in prescribing medications, the behavioral problems of patients will be less overlooked, and physicians would also benefit by prescribing fewer psychoactive medications that they are not adequately trained to prescribe (Whitaker, 2016). Other than that, a comparison review by Muse and McGrath (2010) stated that pharmacologically trained psychologists are better prepared than practitioners in other prescribing professions, which could benefit the clients or patients as pharmacologically trained psychologists would handle their patients with all the behavioral, mental, and emotional conditions. Similarly, McGrath (2010) also stated that prescriptive authority for clinical psychologists could increase access to appropriate care for the patients. Moreover, evidence that prescribing clinical psychologists tend to prescribe medication at a low rate than physicians do, in a way, reducing the chances of overmedication and polypharmacy (McGrath, 2010). A study result from Linda and McGrath (2017) indicated that prescriptive privilege of clinical psychologists is offering benefits both in the field of psychology and the patients as the prescribing psychologists reported increased services to patients of minority background, lower socioeconomic status, and patients from the rural area, which psychiatric service is scarce. In contrast, there are also controversies against the prescriptive privilege of clinical psychologists over the debate. The major concern of the argument is that the combination of psychotherapy medications would have harmed the patients (Whitaker, 2016). As a result, patients might be very dependent on medications, and it could reduce patients' ability to obtain effective adaptive behavioral and thinking patterns which they could access through psychotherapy (Whitaker, 2016). To support the argument, the American Psychiatric Association is concerning the patient's safety in providing prescriptive privileges for clinical psychologists who did not go through proper training to prescribe medicine (Levin, 2017). Furthermore, to protect patients' safety, prescribing law of the United State of America restricted psychologists' scope of practice (Moran, 2014). Due to the lack of relevant educational background in prescribing medications, psychologists are restricted in prescribing medicines unless they completing minimum educational and training requirements. Prescribing psychologists are also required to collaborate with a physician in treating patients with mental illness (Moran, 2014). c) Personal stance on prescription privilege of clinical psychologists As for my stance towards the prescription privilege of clinical psychologists, I am supporting this issue as it may aid in treating patients from minority backgrounds where psychiatric service is meager and insufficient. Like a shred of evidence, few studies reported the reduction of psychiatrists when patients are desperate to seek psychoactive medication consultants (McGrath, 2010; Linda & McGrath, 2017; Shafron, 2014). Other than that, I think that clinical psychologists should be providing prescriptive privilege if they were completing relevant educational and training requirements regarding pharmacology. It is believed that pharmacologic training and didactic materials are sufficient for clinical psychologists to gain the prescriptive privilege. To support the statement, the result of a comparison review by Muse and McGrath (2010) showed that pharmacologically trained psychologists are exposed to an intensive pedagogic material that is relevant to the incorporation of pharmacotherapy in the clinical treatment of mental, behavioral, and emotional conditions. Hence, the researchers think that there is nothing to prevent a clinical psychologist with well-trained in pharmacology to prescribe psychoactive medications. However, clinical psychologists could obtain prescriptive privileges with conditions, such as completing the doctorate program. This is to ensure and beneficiating the treatment process of the patients. Research questions 1. Is combined modalities treatment effective in treating patients with nicotine addiction in the Malaysian context? 2. What are the advantages and disadvantages of the prescriptive privilege of clinical psychologists in Malaysia? 3. Is Malaysia's clinical psychology education requirements sufficient for the practitioners to obtain prescriptive privilege? Conclusion To summarize this assignment, it is a review paper discussing the effectiveness of combined modality treatment in treating nicotine addiction patients. As studies reported, combined therapy is effective to treat patients with nicotine addiction as compared to pharmacologic and evidence-based treatment alone. However, in my humble opinion, I think that we should consider the uniqueness of different patients before the treatment plans can be written out. As therapies are not a one-size-fits-all theory, we should be more aware of the different conditions of the patients. Lastly, this review paper also discussed the controversies of the prescriptive privilege of clinical psychologists in pharmacotherapy. Psychologists need to receive appropriate training and educational study before even talked about the prescriptive privilege. The authorities should be more careful in the decision-making as it will be affecting the effectiveness of patients' treatment process. References Arslan, Y., Öcal, N., Çağın, A., Doğan, D., & Taşçı, C. (2021). The success of smoking cessation treatments: The Gulhane experience. Addicta: The Turkish Journal on Addictions, 8(1), 8-15. doi: 10.5152/ADDICTA.2021.21041 Evins, A. E., Cather, C., Pratt, S. A., Pachas, G. N., Hoeppner, S. S., Goff, D. C., Achtyes, E. D., Ayer, D., & Schoenfeld, D. A. (2014). Maintenance treatment with varenicline for smoking cessation in patients with schizophrenia and bipolar disorder. JAMA, 311(2), 145-154. doi: 10.1001/jama.2013.285113 Fouz-Rosón, N., Montemayor-Rubio, T., Almadana-Pacheco, V., Montserrat-García, S., Gómez-Bastero, A. P., Romero-Muñoz, C., & Polo-Padillo, J. (2017). Effect of 0.5 mg versus 1 mg varenicline for smoking cessation: a randomized controlled trial. Addiction, 112(9), 1610–1619. doi:10.1111/add.13855 García-Gómez, L., Hernández-Pérez, A., Noé-Díaz, V., Riesco-Miranda, J. A., & JiménezRuiz, C. (2019). Smoking cessation treatment: Current psychological and pharmacological options. Rev Invest Clin, 71, 7-16. Heiby, E. M. (2010). Concerns about substandard training for prescription privileges for psychologists. Journal of Clinical Psychology, 66(1), 104-111. doi:10.1002/jclp.20650 Laude, J. R., Bailey, S. R., Crew, E., Varady, A., Lembke, A., McFall, D., … David, S. P. (2017). Extended treatment for cigarette smoking cessation: a randomized control trial. Addiction, 112(8), 1451–1459. doi:10.1111/add.13806 Levin, A. (2017). Psychologist prescribing bills defeated in many states. Psychiatric News. https://doi.org/10.1176/appi.pn.2017.8a2 Linda, W. P., & McGrath, R. E. (2017). The current status of prescribing psychologists: Practice patterns and medical professional evaluations. Professional Psychology: Research and Practice, 48(1), 38-45. http://dx.doi.org/10.1037/pro000011838 McGrath, R. E. (2010). Prescriptive authority for psychologists. Annual Review of Clinical Psychology, 6(1), 21–47. doi:10.1146/annurev-clinpsy-090209-151448 Moran, M. (2014). Prescribing law tightly restricts psychologists’ scope of practice. Psychiatric News. https://doi.org/10.1176/appi.pn.2014.8a2 Muse, M., & McGrath, R. E. (2010). Training comparison among three professions prescribing psychoactive medications: psychiatric nurse practitioners, physicians, and pharmacologically trained psychologists. Journal of Clinical Psychology, 66(1), 96103. doi:10.1002/jclp.20623 Pachas, G. N., Cather, C., Pratt, S. I., Hoeppner, B., Nino, J., Carlini, S. V., … Evins, A. E. (2012). Varenicline for smoking cessation in schizophrenia: Safety and effectiveness in a 12-week open-label trial. Journal of Dual Diagnosis, 8(2), 117– 125. doi:10.1080/15504263.2012.663675 Shafron, G. R. (2014). Prescription privileges and the ethics code: A modern look into the right to prescribe among applied psychologists. Graduate Student Journal of Psychology, 15, 95-102. Windle, S. B., Filion, K. B., Mancini, J. G., Adye-White, L., Joseph, L., Gore, G. C., … Eisenberg, M. J. (2016). Combination therapies for smoking cessation. American Journal of Preventive Medicine, 51(6), 1060–1071. doi:10.1016/j.amepre.2016.07.0