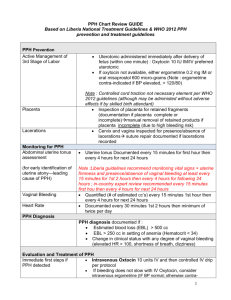
DOI: 10.1111/j.1471-0528.2006.01235.x General obstetrics www.blackwellpublishing.com/bjog Internal iliac artery ligation for arresting postpartum haemorrhage VM Joshi, SR Otiv, R Majumder, YA Nikam, M Shrivastava KEM Hospital, Pune, India Correspondence: Dr VM Joshi, A-47, Tulshibagwale Colony, Sahakarnagar, Parvati, Pune 411009, Maharashtra, India. Email drvivek_joshi@yahoo.co.in; s_otiv@vsnl.com Accepted 29 November 2006. Published OnlineEarly 25 January 2007. Objective To study the role of internal iliac artery ligation (IIAL) in arresting and preventing postpartum haemorrhage (PPH). Design Retrospective chart review of women undergoing therapeutic IIAL for PPH or prophylactic IIAL for risk of PPH. Setting Tertiary care hospital in Pune, India. Sample Women admitted to King Edward Memorial (KEM) Hospital, Pune, India, who underwent IIAL to control or prevent PPH. Methods Bilateral IIAL was performed in all women. Main outcome measures Need for re-laparotomy or hysterectomy to control haemorrhage, complications of the procedure. Results Out of 110 women who underwent IIAL, 88 had therapeutic IIAL for PPH from atony (36), genital tract injury (23), placenta praevia (21), placental abruption (4), uterine inversion (3) or coagulopathy (1). Hysterectomy was performed after IIAL failed to arrest haemorrhage in 33 (39.3%) of 84 women (excluding 4 with vaginal lacerations). Hysterectomy was more likely with uterine rupture (79%) than with nontraumatic PPH (up to 27%). Failure to control haemorrhage by IIAL was evident immediately, and bleeding arrested by IIAL did not recur to require later laparotomy in any woman. Out of 22 women at high risk for PPH undergoing prophylactic IIAL at caesarean section, none had subsequent haemorrhage. One woman had an iliac vein injury that was repaired with no further morbidity. There were no ischaemic complications either during inpatient stay or up to 6 weeks. Conclusions IIAL is useful in the treatment and prevention of PPH from any cause. Early resort to IIAL effectively prevents hysterectomy in women with atonic PPH. In traumatic PPH, IIAL facilitates hysterectomy or repair as indicated and prevents reactionary haemorrhage. Keywords Internal iliac artery ligation, PPH. Please cite this paper as: Joshi V, Otiv S, Majumder R, Nikam Y, Shrivastava M. Internal iliac artery ligation for arresting postpartum haemorrhage. BJOG 2007;114:356–361. Introduction Postpartum haemorrhage (PPH) is a major cause of worldwide maternal mortality ranging from 13% in developed countries to 34% in developing countries.1 It is reportedly responsible for over 125 000 maternal deaths each year and is associated with morbidity in 20 million women per year.2 Major PPH or loss of over 1000 ml of blood occurs in 1–5% of deliveries. Uterine atony is the common cause of PPH that accounts for 80% of cases.3 Other causes include retained placental fragments, lower genital tract lacerations and uterine rupture. Known risk factors for occurrence of atonic PPH include a history of PPH, history of retained placenta, placental abruption, placenta praevia, uterine fibroids, hydramnios, multiple pregnancies, augmentation of labour, prolonged labour and instrumental delivery. Although an 356 assessment of risk factors is important, PPH typically occurs unpredictably and no parturient is exempt from the risk of PPH. When PPH continues despite aggressive medical treatment, early consideration should be given to surgical intervention. The choice of procedure will depend on the parity of the women and her desire for childbearing, the extent of haemorrhage and, most importantly, the experience and judgement of the surgeon. In most catastrophic situations, hysterectomy is preferred in order to arrest further blood loss and compromise with certainty. Although a life-saving procedure, it may not be appropriate for women who need to preserve their reproductive potential. Haemostatic procedures that preserve the uterus include uterine cavity tamponade, selective uterine artery embolisation, uterine artery ligation and uterine brace sutures. ª 2007 The Authors Journal compilation ª RCOG 2007 BJOG An International Journal of Obstetrics and Gynaecology Internal iliac artery ligation Internal iliac artery ligation (IIAL) has been advocated as an effective means of controlling intractable PPH and preventing maternal death. The rationale for this is based on the haemodynamic studies of Burchell,4 which showed that IIAL reduced pelvic blood flow by 49% and pulse pressure by 85%, resulting in venous pressures in the arterial circuit thus promoting haemostasis. However, the reported success rate of IIAL varies from 40 to 100%,5 and the procedure averts hysterectomy in only 50% of cases.6 Failures were more evident in atonic PPH than in other causes of PPH.7 IIAL is thought to be technically difficult, and although much quicker than a hysterectomy, it is seldom attempted. We present a case series of IIAL performed over 13 years at our institution and define the role of IIAL for various indications in obstetrics. Methods The study was carried out from April 1993 to April 2006 in King Edward Memorial (KEM) Hospital, Pune, India, which is a tertiary care centre for high-risk obstetrics. Most operative procedures were performed by Consultant Obstetricians (V.M.J., S.R.O., R.M.), whereas some were performed by lecturers (Y.A.N., M.S.) with more than 2 years experience after qualifying, supervised by the principal author (V.M.J.). All the Consultants were experienced with Gynaecologic cancer surgery. Therapeutic IIAL was performed in women with PPH either at caesarean section or at laparotomy performed at a variable time after vaginal or caesarean delivery. IIAL was also performed prophylactically at caesarean section in women with a high-risk factor for developing PPH, such as coagulopathy, placenta praevia or placental abruption, in the absence of any evident haemorrhage. Women with atonic PPH at vaginal delivery or caesarean section were initially treated with massage and uterotonics such as oxytocin infusion and carboprost injections 250 mcg at appropriate intervals. Failure to restore the uterine tone and arrest the blood loss despite these measures led to the decision to do IIAL. During caesarean section for placenta praevia, failure to control bleeding from the placental bed by pressure or by under running the bleeding sites with absorbable sutures led to the decision to do IIAL. All the four women with placental abruption had undergone caesarean section and developed atonic PPH that failed to respond to uterotonics and hence were subjected to IIAL. Three women with uterine inversion were referred from other hospitals. After repositioning the uteri at laparotomy, they developed atonic PPH that failed to respond to uterotonics and were subjected to IIAL. One woman with HELLP (haemolysis, elevated liver enzymes and low platelet count) syndrome developed atonic PPH after a forceps delivery. As the bleeding did not respond to uterotonics and fresh frozen plasma transfusions, she underwent IIAL but even that could not halt the bleeding and required hysterectomy. At caesarean section in women with placental abruption (eight), placenta praevia (four), HELLP (eight), ITP (one) and acute hepatitis with coagulopathy (one), a prophylactic IIAL was performed in the absence of any significant uterine bleeding. The women were placed in the semi-lithotomy position as it permitted assessment of vaginal bleeding. When quick access was required in high-risk situations like rupture uterus or shock, a midline infraumbilical incision was preferred, otherwise a Pfannenstiel incision was used. The uterus was pulled out of the abdominal incision and bowels were packed away. On the left side, it was sometimes necessary to incise the sigmoid mesocolon and mobilise the sigmoid colon medially in order to expose adequately the area overlying the iliac vessels. After identifying the ureter at the pelvic brim, the peritoneum was incised starting from a point just proximal to the bifurcation of the common iliac artery proceeding caudally along the external iliac artery for a length of about 8 cm. Using gentle finger dissection, the ureter was retracted medially exposing the retroperitoneal anatomy. Using a long haemostat, the fascia around the internal iliac artery was dissected completely to free the artery from its adjacent structures and to clarify the anatomical relationship of the internal iliac artery with the iliac veins (Figure 1). A right-angled clamp was passed beneath the internal iliac artery from lateral to medial side about 4 cm distal to its origin (Figure 2). As the posterior division usually branches off proximal to this, no attempt was made to locate it. Using a nonabsorbable suture (linen), the internal iliac artery was ligated singly. Pulsations of the femoral artery and dorsalis pedis were identified after tying the ligature. In cases of nontraumatic haemorrhage, Figure 1. Retroperitoneal anatomy showing right psoas major, external iliac artery and vein, internal iliac artery and vein and ureter. ª 2007 The Authors Journal compilation ª RCOG 2007 BJOG An International Journal of Obstetrics and Gynaecology 357 Joshi et al. Table 1. Indications for IIAL (n = 110) Indication Number of women (%) Uterine atony Placenta praevia Genital tract injury Placental abruption Coagulopathy Uterine inversion Total 36 (32.7) 25 (22.7) 23* (20.9) 12 (10.9) 11 (10) 3 (2.7) 110 (100) *Out of 23 women, 4 had traumatic PPH from vaginal lacerations. Figure 2. Safe method of passing right-angled clamp from lateral to medial side below the internal iliac artery. once IIAL was performed, the control of haemorrhage was confirmed by improvement in vital signs as well as decrease in amount of vaginal bleeding. If bleeding continued unabated, decision for hysterectomy was taken. In uterine rupture, IIAL was performed at the outset. Following this, decision to repair the trauma or resort to hysterectomy was influenced by the extent and location of injury as well as by control of haemorrhage. In extensive vaginal lacerations, suturing was performed after IIAL. Results Over a period of 13 years from April 1993 to April 2006, 110 women underwent IIAL at KEM Hospital, Pune, India. Eighty-eight women had IIAL for PPH after vaginal or caesarean delivery in the KEM hospital or in other referring hospitals. In addition, prophylactic IIAL was performed in 22 women at high risk of PPH during caesarean section at KEM hospital. Uterine atony was the common indication for therapeutic IIAL (32.7%). Other indications were placenta praevia, traumatic PPH, placental abruption and uterine inversion (Table 1). Out of 11 women with coagulopathy, 9 had HELLP syndrome and 1 each had ITP and acute liver disease. Out of 23 women with genital tract injury, 19 had uterine rupture and 4 had extensive vaginal lacerations. In cases of uterine rupture, early IIAL as well as the extent and location of damage determined the feasibility of conservation of uterus. Out of 19 women who had uterine rupture, the uterus could be repaired in only 4 women and the others underwent hysterectomy. However, IIAL performed at the outset helped in repairing the uterus or doing the hysterectomy. In four women with vaginal laceration, direct suturing of the lacerated and friable walls provoked further bleeding. IIAL arrested the blood loss and facilitated suturing of the tissues properly. 358 In women with PPH, whether IIAL was performed primarily at caesarean section or at an interval after delivery, once haemostasis was achieved and the abdomen closed, haemorrhage did not recur. After successful control of haemorrhage with IIAL, no woman had delayed haemorrhage requiring re-laparotomy. However, failure of IIAL to arrest uterine bleeding was evident immediately before closure of the abdomen, enabling a timely decision to proceed to hysterectomy. Out of 106 (excluding 4 women who had traumatic PPH from vaginal lacerations) women where IIAL was performed, 33 women required hysterectomy, giving an overall uterine salvage rate of 68.8%. The uterine salvage rate in women where therapeutic ligation of internal iliac artery (n = 84) was performed was 60.7% (Table 2). Among 19 women with uterine rupture who underwent IIAL, 15 required hysterectomy, giving a uterine salvage rate of 21%. Women with nontraumatic PPH (n = 65), who had IIAL fared better with only 18 requiring hysterectomy to control uterine bleeding, giving a uterine salvage rate of 73%. Prophylactic ligation was performed in 22 women, and none of these women required hysterectomy (Table 3). Table 2. Hysterectomy in women undergoing IIAL for uterine haemorrhage (n = 84*) Indication Uterine atony Placenta praevia Uterine rupture Placental abruption Uterine inversion HELLP syndrome Total Total number of women Hysterectomy carried out, n (%) Uterine salvage rate (%) 36 21 19 4 3 1 84 13 (36.2) 3 (14.3) 15 (79) 0 (0) 1 (33.3) 1 (100) 33 (39.3) 63.8 85.7 21 100 66.6 0 60.7 *Out of 88 women who underwent therapeutic IIAL, 4 had traumatic PPH from vaginal lacerations. ª 2007 The Authors Journal compilation ª RCOG 2007 BJOG An International Journal of Obstetrics and Gynaecology Internal iliac artery ligation Table 3. Hysterectomy in women who underwent prophylactic IIAL (n = 22) Indication Placental abruption Placenta praevia Coagulopathy Total Number of women Hysterectomy Uterine salvage rate (%) 8 4 10 22 0 0 0 0 100 100 100 100 The time interval between the onset of haemorrhage from uterine atony and IIAL influenced the uterine salvage rate (Table 4). Injury to the internal iliac vein that occurred in one woman was repaired by passing a figure of ‘8’ black silk 3-0 gauge suture around the defect in the vein and then incorporating adventitia of the internal iliac artery in the same suture. There were no ischaemic complications like gluteal muscle ischaemia or bladder ischaemia in the postoperative period either during inpatient stay or up to 6 weeks. There were three maternal deaths unrelated to PPH; two women with fulminant hepatitis succumbed to hepatic failure after the seventh postoperative day and one had HELLP syndrome and died of hepatorenal failure on postoperative day 25. Six women conceived after IIAL. These pregnancies continued till term, with no evidence of fetal growth restriction. Discussion PPH can cause exsanguination rapid enough to be fatal in spite of the immediate availability of blood products. One of the reasons for this could be the delay in resorting to surgical techniques once conservative measures have failed.8,9 The authors believe that the life-saving technique of IIAL is underutilised in the management of PPH, probably due to fear of injury to iliac veins. Thorough knowledge of retroper- itoneal anatomy and meticulous operative technique can minimise these complications. Since the internal iliac vein lies directly posterior to the internal iliac artery, passing the rightangled clamp in a controlled manner in close proximity to the posterior wall of the artery prevents perforating the underlying internal iliac vein. It is imperative to dissect the internal iliac artery completely from the surrounding fascia for the passage of the right-angled clamp without resistance. Resistance to the passage of the right-angled clamp implies inadequate dissection around the internal iliac artery. Forceful passage of the clamp in such a situation incurs the risk of injury to the adjacent vein. It is safer to withdraw the clamp, complete the dissection of fascia around the artery and then pass the clamp under the artery. Some authors have advised the use of Babcock forceps to elevate the internal iliac artery to facilitate the passage of right-angled clamp.10 However, the Babcock forceps itself may obstruct surgeon’s operative field. While passing the right-angled clamp beneath the internal iliac artery, the operator has better control at the point of entry than at the point of exit. Hence, we believe that passing the clamp from lateral to medial side is safer. If the clamp is passed from medial to lateral side, the tip of the clamp may injure the laterally located external iliac vein (Figure 3). Ideally, the internal iliac arteries should be ligated distal to the posterior division to get optimum decrease in pulse pressure in the uterine circulation. However, in emergency situations, it is not advisable to try locating the posterior division as this could be time consuming and may injure the internal iliac vein. Since the posterior division is given off within 3 cm from the bifurcation, most of the times what is ligated beyond 3 cm from bifurcation is the anterior division of internal iliac artery. Selective arterial embolisation is an option in managing PPH if the women is haemodynamically stable. Current indications include haemorrhage due to vaginal or cervical Table 4. Timing of IIAL and uterine salvage in uterine atony (n = 36) Timing of IIAL At caesarean section Laparotomy after vaginal delivery Re-laparotomy after caesarean section Number of women Hysterectomy Uterine salvage rate (%) 20 14 3 8 85 43 2 1 50 Figure 3. Tip of right-angled clamp passed from medial to lateral side may injure the external iliac vein. ª 2007 The Authors Journal compilation ª RCOG 2007 BJOG An International Journal of Obstetrics and Gynaecology 359 Joshi et al. lacerations or persistent bleeding after hysterectomy. Round the clock, availability of a skilled interventional radiologist and the radiologic set-up in proximity is a prerequisite. Complications like post-procedure fever, uterine and bladder necrosis,11,12 ischaemic nerve injury,13 vascular perforation and infection have been reported. Uterine artery ligation is a promising technique in the management of PPH as occlusion of the uterine artery reduces 90% of the blood flow. It is useful in uterine atony, but in uterine trauma, when the avulsed uterine artery retracts into the broad ligament forming a haematoma, it is difficult to do a uterine artery ligation and salvage the uterus. IIAL in such situations is helpful as the pressure and flow of circulation decrease distal to the ligation and enabling one to readily locate the bleeder and ligate it securely. Similarly, in cases of deep forniceal tears and haematomas, uterine artery ligation or even hysterectomy does not stop the haemorrhage. In such cases, blood loss could be arrested after IIAL as vaginal artery is a direct branch of anterior division of internal iliac artery. In complete placenta praevia, the placental site receives a significant proportion of its arterial blood supply from the descending cervical and vaginal arteries. These arteries continue to perfuse the lower segment even after uterine artery ligation, which fails to control haemorrhage.14 In these circumstances, IIAL is more effective by diminishing the blood flow in the uterine, cervical and vaginal vessels. The technique of stepwise devascularisation of uterus, which includes bilateral uterine and ovarian artery ligation, is effective in decreasing the blood loss, but uterine ischaemia followed by synechiae formation, premature ovarian failure and secondary amenorrhoea has been reported subsequent to this procedure.15 The B-Lynch suture has been reported to successfully control refractory uterine bleeding in several case series. The suture envelops and compresses the uterus, producing a result similar to manual compression, but failures can occur16 for various technical reasons,17,18 with severe uterine atony and in the presence of coagulopathy.19 Delayed ischaemic necrosis of the myometrium has been recently reported even after applying the sutures correctly.20 The uterine brace compression sutures can be used only for achieving haemostasis in atonic PPH and are less useful in placenta praevia. It has no application in uterine rupture or bleeding from vaginal lacerations. IIAL not only contributes to the prevention of hysterectomy but also in cases where hysterectomy cannot be prevented, it facilitates hysterectomy as in cases of uterine trauma.14 IIAL performed at the outset decreases the bleeding, clears the operative field and thus enables the surgeon to avoid blindly clamping and ligating tissues submerged in a pool of blood. This is particularly helpful in reducing the risk of ureteric injury. IIAL also facilitates repair of vaginal 360 lacerations that bleed profusely with each suture through the vaginal wall. Although IIAL is not a substitute for meticulous repair of vaginal lacerations, in four women with extensive vaginal lacerations where suturing was not possible, IIAL arrested the bleeding and enabled suturing. We observed that some women having high-risk factors for PPH like placenta praevia, placental abruption, HELLP syndrome, ITP and infective hepatitis undergoing caesarean section required a laparotomy for reactionary haemorrhage in the immediate postoperative period. A re-laparotomy in such compromised situations not only exposed the women to the risks of anaesthesia and emergency surgery but almost always culminated in a hysterectomy as a definitive treatment. Hence, we subsequently started doing prophylactic IIAL at caesarean section in all women with these high-risk factors. With this protocol re-laparotomy was averted in all such cases. Since the morbidity of IIAL in experienced hands is less than that of a re-laparotomy, we believe that such a concurrent prophylactic ligation of internal iliac arteries is justified when one is doing a caesarean section for women with highrisk factors for PPH. The injuries that can occur to the iliac veins are due to perforation either by haemostat during dissection of fascia around the internal iliac artery or by the tip of right-angled clamp that is passed beneath the internal iliac artery. In the event of such an injury, suction and good illumination with the use of fibreoptic light source facilitate location of these injuries. These venous perforations can be sealed by passing a figure of 8 suture around the defect in the vein with black silk gauge 3-0 and then incorporating adventitia of the internal iliac artery in the same suture to give support to the injured vein. Given the usefulness of IIAL in prevention and treatment of PPH, one could explore other methods of occluding the internal iliac artery (like applying a clip on the vessel) that do not entail dissection around the artery and incur the possibility of venous injury. Fear of vascular injury and recurrence of haemorrhage commonly deter an obstetrician from resorting to IIAL. We observed that once the uterine bleeding was controlled during surgery, it did not recur in the postoperative period in any woman in whom the uterus was conserved. Similarly, there was no reactionary haemorrhage from the pedicles in any woman where hysterectomy was carried out after IIAL. In conclusion, IIAL is a valuable procedure in treatment of PPH and its prevention in high-risk women. Unlike other procedures, it can be reliably used in all causes of PPH. Early resort to IIAL is the key to prevent hysterectomy in women with uterine atony. In traumatic PPH, IIAL facilitates repair or hysterectomy when indicated and prevents reactionary haemorrhage. All obstetricians caring for parturient women should familiarise themselves with this procedure and lower their threshold for its use in emergent situations. j ª 2007 The Authors Journal compilation ª RCOG 2007 BJOG An International Journal of Obstetrics and Gynaecology Internal iliac artery ligation References 1 Khan KS, Wojdyla D, Say L, Gulmezoglu AM, Van Look PF. WHO analysis of causes of maternal death: a systematic review. Lancet 2006;367:1066–74. 2 Selo-Ojeme DO. Primary post partum haemorrhage. J Obstet Gynecol 2002;22:463–9. 3 Arulkumaran S, De Cruze B. Surgical management of severe postpartum haemorrhage. Curr Obstet Gynecol 1999;8:101–5. 4 Burchell RC. Physiology of internal iliac artery ligation. J Obstet Gynaec Brit Cwlth 1968;75:642–51. 5 Vedantham S, Godwin SC, McLucas, Mohr G. Uterine artery embolization: an underused method of controlling haemorrhage. Am J Obstet Gynecol 1997;176:938–48. 6 Gilstrap LC, Ramin SM. Postpartum haemorrhage. Clin Obstet Gynecol 1994;37:824–30. 7 Chattopadhyay SK, Deb Roy B, Edrees YB. Surgical control of obstetric haemorrhage: hypogastric artery ligation or hysterectomy? Int J Obstet Gynaecol 1990;32:345–51. 8 Reich WJ, Nechtow JR. Ligation of internal iliac (internal iliac) arteries: a life saving procedure for uncontrollable gynaecologic and obstetric haemorrhage. J Int Coll Surg 1961;36:157. 9 Reich WJ, Nechtow JR, Keith L. Supplementary report on internal iliac artery ligation in the prophylactic and active treatment of haemorrhage in pelvic surgery. J Int Coll Surgeons (Bull) 1965;44:1. 10 Breen J, Gregori CA, Kindzierski JA. Haemorrhage in Gynaecologic Surgery. Hagerstown, MD: Harper and Row, 1981, p. 438. 11 Porcu G, Roger V, Jacquier A, Mazouni C, Rojat-Habib MC, Girard G, et al. Uterus and bladder necrosis after uterine artery embolization for postpartum haemorrhage. BJOG 2005;112:122–3. 12 Cottier JP, Fignon A. Uterine necrosis after arterial embolization for postpartum haemorrhage. Obstet Gynecol 2002;100:1074–7. 13 Hare W, Holland CJ. Paresis following internal iliac artery embolization. Radiology 1983;146:47–51. 14 Cruishank SH. Management of postpartum and pelvic haemorrhage. Clin Obstet Gynecol 1986;2:213–19. 15 Romans H, Sentilhes L, Cingotti M. Uterine devascularization and subsequent major intrauterine synechiae and ovarian failure. Fertil Steril 2005;83:755–7. 16 Joshi VM, Shrivastava M. Partial ischemic necrosis of the uterus following a uterine brace compression suture. BJOG 2004;111: 279–80. 17 El-Hamamy E. Partial ischemic necrosis of the uterus following a uterine brace compression suture (letter). BJOG 2005;112:126–7. 18 B-Lynch C. Partial ischemic necrosis of the uterus following a uterine brace compression suture (letter). BJOG 2005;112:126–7. 19 B-Lynch CB, Coker A, Lawal AH, Abu J, Cowen MJ. The B-Lynch surgical technique for control of massive postpartum haemorrhage: an alternative to hysterectomy? Five cases reported. Br J Obstet Gynaecol 1997;104:372–6. 20 Treolar EJ, Anderson RS, Andrews HS, Bailey JL. Uterine necrosis following B-Lynch suture for primary postpartum haemorrhage. BJOG 2006;113:486–8 ª 2007 The Authors Journal compilation ª RCOG 2007 BJOG An International Journal of Obstetrics and Gynaecology 361