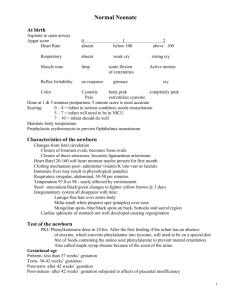
NUR 161 NEWBORN NURSING ASSESSMENT GUIDE OBSERVATION Vital Signs A. Respiration "NORMALS" Rate-normally 30-50/minute; quite shallow, irregular. Breathing usually abdominal or diaphragmatic. Transient tachypnea. Breath sound may be difficult to localize - clear to rales & rhonchi. B. Pulse Beat heard 5th intercostal space. May hear murmurs first or second day which may be physiologic. After this time, notify physician. 120-150 beats/min (if asleep, 80-90/min; if crying, up to 180/min). HOW TO ELICIT Observe first, while infant is quiet. Check for quality and quantity. Count for at least 30 seconds. Check breath sounds for rales & rhonchi. Auscultate with stethoscope while infant quiet. Note quality and position, rate and rhythm. Auscultate for one full minute. DEVIATIONS Less than 35 or +50 (tachypnea) when at rest, dyspnea or cyanosis. Grunting. "Periodic breathing" of more than 10 seconds without a respiration is classified as apnea. Respiratory Distress Symptoms are retractions, grunting nasal flaring. Less than 100-bradycardia, would indicate More than 150-trachycardia, distress Trends are as important as any single finding. Note a shift in placement of heart sounds. (could be due to tension pneumothorax.) Weak pulse Arrhythmia May be regular or irregular, strong, pulses equal C. Blood Pressure D. Temperature Normal average 80/40 at birth to 100/50 by 10 days; depends on age and weight of infant. Difficult to obtain diastolic pressure with standard sphygmomanometer - Blood pressures not routinely done on normal newborns - only those who are premature, in distress or suspected of having an anomaly. Rectal 36.5-37.2o C(97.7-99oF) Axillary 36.537.2o C(97.7-98.6oF) Temperature stabilizes within 8-12 hours after delivery. Check strength and equality of apical femoral, and brachial pulses. Doppler method. Decreased or absent femoral pulses indicate coarctation of aorta. Rectal temperature initially and axillary temperatures the remaining time. Swings of more than 2oF from one reading to next. Hypothermia extremely stressful and dangerous in newborn. Skin temperature is an earlier and more sensitive indicator of thermal state than core temperature. 1 Low blood pressure (shock, hypovolemia) Weight Average birth weight about 7 pounds 8 oz. (3405 Gm) Males usually weigh slightly more than females, white babies more than non-white, second more than first. Average physiologic weight loss about 5-10% of birth weight. Warmed, padded accurate safe scale optimal. Daily comparisons of weight. Length Average-50 cm (20 inches) both sexes grow 1 inch per month for the first 6 months. 4. Head Large in comparison to rest of body; 1/4 of body size. Circumference about 33-35 cm. and is approximately 2 cm greater than chest circumference, (although the first day they may equal due to molding) Asymmetrical due to molding (result of pressure during birth) May see bruising due to trauma of delivery; -Caput succedaneum-swelling or edema of scalp near presenting portion; crosses suture lines -Cephalhematoma-soft mass of irreductible blood accumulating, between periosteum and flat skull bone-absorbed in 2-3 weeks, does not cross suture lines. Place flat on back and extend to fullest. Use disposable paper tape measure. For accurate measurement paper measuring tape is placed over the most prominent part of the occiput and brought to just above the eyebrows. 2 Overheating may cause hyperventilation and stress and apnea. Hypothermia may indicate sepsis, chilling. Less than 2500 grams - Low birth weight (not premature). Using the "Newborn Classification and Neonatal Mortality Risk" chart (Lubchenco), infants classed as large for Gestational Age, appropriate for Gestational Age, or Small for Gestational Age (IGA, AGA, SGA) by plotting their birthweight against their gestational age. Infants of Diabetic mothers are classically large for Gestational Age. Cradle cap Microcephaly - mental deficiency. Hydrocephalus - increased cerebral spinal fluid from various causes - yields increased intracranial pressure Macrocephaly may be a sign. Craniostenosis - premature closure of the cranial sutures before or shortly after birth. A. Fontanels (openings at the points of union of the skull bones) 1. Anterior 2. Posterior B. Scalp/hair C. Face provides examiner an opportunity to indicate unusual facies. D. Eyes E. Ears Feel soft Useful indicator of infant's condition. May pulsate with heartbeat Overriding suture lines due to molding and will disappear when molding disappears Diamond shaped, average diameter 1.5-2.5 cm. Closes at about one year of age. Triangular shape; may be nearly closed at birth Measured in centimeters Bulging fontanele - a clue to increased palpated gently intracranial pressure Examine when infant at rest. Depressed fontanele - indicates dehydration. Junction of 2 parietal and 2 frontal bones. Located between occipital and parietal bones. Small, minute "pin-prick" in scalp due to internal Palpate gently. fetal monitor scalp electrode varying amounts of Note color, amount & hair. texture. Note placement and symmetry of eyes, ears & During cry, note symmetry grimace with cry. of facial muscles. Chin recessed. Usually blue or slate blue-gray in color. Will open spontaneously. Sclera may have bluish tint. Subconjunctival hemorrhage not uncommon. Iris color may change up to 3 months. Pupils reactive to light and equal. Tearing not established until 1-3 months. Incoordinate movements normal. Transient strabismus due to poor neuromuscular control of eye muscles. Eyelids edema due to instillation of silver nitrate in eyes--chemical conjunctivitis 1-2 hours after instillation; disappears in 1-2 days. Can discriminate patterns, brightness; will track moving objects to midline. Epicanthal folds in oriental babies. Have well formed cartilage (one determinant of gestational age). Pinna inserted on head on horizontal plane to outer canthus of eye. Place infant in vertical position away from light. Check for pupil size, reaction of pupils to light, blink reflex to light, and edema and inflammation of eyelids. Note shape of eyes. Note color of eyes and sclera. Check vision Note eye ball movement Check eyelids Should return quickly when folded over. Inspect shape, size and position, and evaluate hearing by his 3 May have abrasions or bruising with instrument deliveries. Asymmetry may be due to nerve damage. Chromosomal anomalies. Lacerations to cheek – especially in C section Babies or Forceps Delivery Retrolental Fibroplasia may result from hyperoxemia; Opacities on pupil (sign of congenital cataract). Setting sun sign - may indicate increased intracranial pressure if persists. Report immediately to prevent eye damage. Infectious conjunctivitis - same symptoms as chemical conjunctivitis, but caused by staph or gram negative rods. Onset usually after 2nd day. Requires treatment. Epicanthal folds (Down's syndrome) Pupils not reactive and/or equal. Misplacement may indicate chromosomal problem (low set ears). Malformation may indicate associated renal problems. Can hear immediately after birth. response to loud noises. F. Nose Small and narrow, symmetrical. Infants obligatory nose breathers. Sneezing normal. Milia Patent nares bilaterally. Does not open mouth to breath. G. Mouth Fat pads on cheeks. Sucking callouses on lips for a few weeks. Lips should be pink. Precocious teeth will be pulled, especially if loose to prevent aspiration. Inclusion cysts (gray-white lesions) Epstein's Pearls (white cysts that are hard); disappear in a few weeks. Tongue proportional to mouth. Assess for mucus obstructions. Pass soft catheter (not to be done by student RN's) OR Gently cover infants mouth and occlude one nare at a time & observe if infant has any signs of respiratory distress. Check by inserting gloved finger or by stimulating infant to cry. 5. Neck Short and creased with deep moist folds. Posterior neck lacks loose extra folds of skin. Observe crying, sucking. Palpate carefully. Passive range of motion. Clavicles straight and intact. 4 Pressure necrosis. Preauricular skin tags - usually tied off and allowed to slough off. Choanal atresia. Nasal flaring - indicates distress. Drooling-suspect tracheo-esophageal fistula. Cleft palate, cleft lip Macroglossia (large tongue) Thrush-white curd type deposits; difficult to remove, bleed when disrupted-caused by candida albicans. Frenum linguae - "tongue tied" ridge of frenulum tissue attached to underside of tongue, causing a heartshape at tip of tongue. Clipping of tongue no longer done due to danger of infection. Nerve paralysis from birth trauma-asymmetrical mouth movements. Fracture clavicle Swelling or masses Rigidity of neck may indicate sternocleidomastoid injury. Torticollis or wry neck (head held at angle). Webbing Abnormally short neck. Arching of neck. 6. Chest 7. Abdomen 8. Extremities A. Arms and hands Cylindrical shape, circumference No intracostal, subcostal or suprasternal retractions. Small bell stethoscope. Individual stethoscope at each bedside. Funnel check (lower sternum depressed), Pigeon breast (prominent sternum and costal cartilage). Diaphragm and abdominal muscles perform most of breathing. Xiphoid cartilage - protrusion at lower end of sternum. Breast tissue diameter 5 cm. or more at term. Engorged breasts: "witchs' milk" Extra or supernumerary nipples-below and medial to true nipples. Cylindrical with some protrusion. Distention after feeding common. Umbilical cord stumpWhartons jelly. (2 arteries, 1 vein) Nontender. No cyanosis and few, if any, blood vessels, should be seen. Circumference Bowel sounds heard shortly after birth. Bladder 1-4 cm above symphysis; empties about 3 hours after birth; urine mild odor. Measure circumference. Measure breast tissue. Palpate xiphoid. Observe respiratory effort. Respiratory Distress symptoms: - retractions - grunting - nasal flaring Asymmetry of chest may indicate pneumothorax. Gently palpate all 4 quadrants. Check contour. Check for masses, distention. Check for bladder distention. Check for any hernias. Check vessels in cord. Check abdominal tension Listen for bowel sounds Arms are abducted, flexed and internally rotated. Movement symmetrical. Hands are normally clenched into fists. Full range of motion possible. Five fingers - each hand & separate. Note symmetry of movement Open hands and examine each finger separately; count them. Passive range of motion to all joints. Meconium or yellow stained cord-evidence of fetal distress. Single umbilical artery - associated anomalies (renal). Diaphragmatic hernia - abdomen flat and scaphoid. Congenital tumors - do not palpate abdomen. Omphalocele Urachal fistula Umbilical hernia, infections Atonic bladder myelomeningocele-crade Distention not associated with feeding (may be first sign of many GI abnormalities). Foul smelling drainage from umbilicus; bleeding from umbilicus, inflammation. Absence of bowel sounds. Unusual position may be caused by fracture (humerus, elbow). Poor muscle tone may be due to cerebral injury, narcosis, shock, anoxia. Syndactyly (webbing). Polydactyly (excess digits) Simian crease-s single palmar crease (frequently present in infants with Down's 5 Syndrome.) Brachial Palsy-paralysis of portions of arm trauma to brachial plexus during delivery. Erb-Duchenne paralysis-arm lies limply at side; elbow in extension with forearm B. Legs and feet 9. Back 10. Genital (Assess last) A. Male Legs of equal length and symmetrical thigh and gluteal skin folds. Legs flexed, in partial abduction. Femoral and pedal pulses present. No resistance to hip abduction. Hips abduct to more than 60o. Legs shorter than arms at birth. Creases on soles of feet. Foot is in straight line. Positional clubfootbased on position in utero. 5 toes each foot, separate Spine is straight and flat. Coccygeal dimple - note if hair present or appears very deep. Dimple common finding resulting from maldevelopment of caudal ligament. At least 1/2 of back devoid of lanugo. Urine of either may be brick red in color due to uric acid crystals. Diaper will hematest negative. Phimosis (opening of prepuce is narrowed and foreskin cannot be retraced over gland); normal size varies. Testicles descended at 40 weeks; not consistently found in scrotum. Meatus is at tip of penis. Scrotal edema/discoloration common in breech deliveries. Hydrocele-very common in newborns Circumcision - optional. Passive range of motion to all joints. Check symmetry, thigh folds. Check amount of sole creases Place infant in prone position and separate buttocks to expose coccygeal area. Check vertebral alignment. Palpate scrotal sac. Examine penis for placement of meatus. Assess scrotal rugae Palpate testes 6 pronated. Moro reflex can't be elicited on affected side (5th and 6th cervical nerve palsy). Unilateral or bilateral dislocated hips. Absence of pulses in lower extremities, classic sign of coarctation of aorta. Syndactyly and polydactyly Genu recurvatum-knee bends backwards. Clubfoot (talipes equinovarus). Meningomyelocele, spina bifida. Dermal sinus tract - site of potential contamination of cerebral spinal fluid Pilonidal cysts. Curvatures of vertebral column. Hypospadias. Epispadias Hernia Abrasions resulting from breech presentation Specific Gravity normally 1.003-1.012 Undescended testicles. B. Female 1. Anus 2. Skin A. Color Labia majora covers labia minora (an indicator of gestational age). May have hymenal tag-disappears in several weeks. May have blood or white discharge pseudomenses Edema and bruising in breech delivery. Patent Passage of meconium usually within 24 hours. Normal stool cycle; Meconium stool-black, sticky, odorless Transitational stool - green/black Breast/bottle stool - yellow Frequency of stools depend on method of feeding (breast vs. bottle) Pink and warm to the touch, red when crying. Acrocyanosis (blue extremities) common in first 24 hours of life. Blood supply returns quickly when skin blanched with a finger. Mottling-common with chilling; can be sign of distress. Common skin manifestations: Milia-tiny pearl white bumps occurring around nose, check, forehead. Mongolian spots - hyper-pigmented brownbluish spots over lower back. Usually found in dark skinned races. "Stork's" beak mark-reddish areas on eyelids & occiput caused by dilatation of superficial blood vessels. Erythema Toxicum-newborn rash "flea-bite" -areas of redness varying in diameter with small raised yellowish white wheal. Peak incidence: 24-48o of life. Forcep marks. Recto-vaginal fistual, recto-anthral. Check patency by observing Imperforate anus passing of meconium or soft Rectal stress catheter inserted gently. No stool after 24o of life. Check color and consistency of stools Blanch tip of nose or gum line to assess jaundice. Check capillary refill on palm. Examine skin on nose, back & buttocks. 7 Acrocyanosis persisting beyond 24-48 hours of life. Circumoral cyanosis (blue around mouth). Mottling. Meconium stained skin indicates fetal distress pre- or intra- partum. Observe for jaundice (1/2 of all newborn within first 3 days of life). Jaundice in the first 24 hours is not normal. Ecchymosis (bruises) may cause an elevated bilirubin as they resolve. "Bronze baby syndrome"-seen rarely if phototherapy is used with an obstructive type jaundice. "Physiologic" jaundice may appear from day 3-7. Plethora after the initial period may indicate polycythemia. Watch any laceration (especially C-section or fetal scalp electrode) for bleeding, infection. Pallor B. Texture C. Turgor 13. Reflexes A. Grasp B. Root Soft; may have dry & peeling hands & feet Vernix caseosa (cheesy white substance and lanugo (fine, downy hair) disappear after a few days. First day - may be slight edematous. Subcutaneous fat. Both hands and feet. Strong enough in hands to enable infant to be lifted (carefully) off bed. Turns head toward stimuli and attempts sucking. C. Suck Tongue should not be up while feeding-prevent flow of milk. D. Startle or Moro Arms and legs extend upward with any disturbance in equilibrium. "C" shape in fingers. Present at birth. E. Tonic Neck Fencing position - when on back with head turned to side, tends to flex arm and legs and extend arm and leg looking toward. Hyperextension of all toes when one side of sole is stroked from heel upward across ball of foot. F. Babinski G. Stepping General Activity/Appearance Check creases for vernix Large amounts of lanugo (premature) Generalized cracked or peeling skin (postmaturity). Gently pinch up skin over abdomen. If skin returns promptly to surface, turgor is elastic. If feels doughy and stays pinched up, tenting is present. Pressure against palm or sole of foot. Touch against cheek or chin. Do when hungry. Stimulus to lips. Poor turgor may indicate dehydration. Decreased serum protein will cause edema. Sclerema (hardening of subcutaneous tissue) poor prognostic sign. Low birth weight or postmature baby may lack subcutaneous tissue. Asymmetry of response. Loud noise, grasp both hands, lift until arms fully extended and suddenly release. Postural relax. Poor sucking or easily fatigued. Suck and swallow not coordinated before 34 weeks gestation. Excessive drooling may indicate TEF. Sudden or startling behavior may indicate neurological symptoms. Asymmetry of body response. Absence of Moro. Asymmetry. Stroke bottom of foot. Absence. When held upright and one foot touching a flat surface, will step alternately. Asymmetry. Cry strong and lusty. Sleeps in fetal position. Responds to stimulation Alternate periods of excitability and quietness. Cries vary in length from 3-7 minutes after Cry-weak or high pitched, shrill or absent cry. Abnormal movements (seizures) Lethargic, limp Hypertonic Floppy baby 8 consoling measures are used. Cry strong. Symmetrical movement and strength in all extremities May be jerky or have brief twitching. Head lag not over 45o Tremors Revised 1/16 9