CVP Measurement Guide: Indications, Procedure, & Nursing Care
advertisement

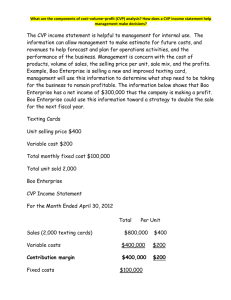
N - 112 MS 1 RLE CENTRAL VENOUS PRESSURE MEASUREMENT Meaning and Purposes • It is the pressure within the right atrium Purposes 1. Determine the pressure in the right atrium 2. Assess the preload of the right side of the heart 3. Guide to fluid replacement 4. Estimate the circulating blood volume Indications of CVP For patients with: 1. Congestive heart failure 2. Decrease in myocardial contractility 3. Renal failure 4. Tension Pneumothorax 5. Pleural effusion 6. Hypovolemia or Hypervolemia 7. Decrease in myocardial contractility 8. Decreased cardiac output Interpretation of CVP • An increase above normal or elevated CVP results indicate weakening or failure of the right side of the heart or excessive fluid blood volume • A pressure below normal reflects an intravascular blood volume deficits or drug-induced excessive vasodilation • CVP measurement must not be interpreted on their own, but viewed alongside the patient’s full clinical picture (BP, respiratory patter, color, temperature) Normal Value and Catheter Placement • Normal CVP ranges from 4 to 12 mm Hg (ref. Brunner) or 5 – 10 cm H2O Veins Sites for Catheter Placement 1.Cephalic or basilic 2.Subclavian 3.External or internal jugular Materials Needed for CVP Measurement 1.Sterile bag of fluid – normal saline solution (isotonic) 2.Administration set 3.IV extension set 4.CVP Manometer 5.Stopcock Nursing Care of CVP 1. Hand hygiene 2. Sterile technique when changing the central line dressing 3. Change gauze every 48 hours; transparent dressing every 7 days 4. Wearing clean gloves before accessing the line port 5. Performing a 15 – 30 second “hub scrub” using friction in a twisting motion 6. Antiseptic-containing port protectors to cover connectors 7. Assess catheter site Skill 9: CVP Measurement 1.Informs patient of the procedure. 2.Washes hands 3.Provides for client’s privacy 4.Places the client in supine position (if contraindicated, adjusts the position). 5.Places the manometer at zero level adjacent to the 5th ICS midaxillary line. 6.Opens the CVP and IV port and closes patient's Port 11.Makes sure no air has entered the IV line during reading. Closes the CVP line and opens the IV line to allow fluid to flow to the patient's line for flushing. 12.Reattaches ventilator if the patient is on ventilator. Repositions patient. 13.Regulates IV fluid as previously ordered. 14.Washes hands. 15.Documents the CVP reading, condition and position of client when CVP reading was obtained. 7. Allows IV solution to flow to the CVP line to about 20 - 25 cm. level at the manometer 8.Closes the IV line and opens CVP line and patient's line. 9.Instructs patient to take a deep breath and observes for fluid fluctuation (In case intubated and conscious, detaches patient from the ventilator temporarily and asks patient to take a deep breath; if intubated and unable to follow commands, observes fluid fluctuation at the end of inspiration). 10.Notes the level where the fluctuation stabilizes.