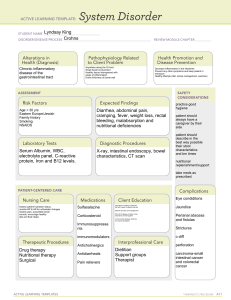
Diarrhea – 3 or more stools per day ● Acute – less than 14 days ● Chronic – more than 30 days ● C. diff – hospital acquired ○ Wash your hands ○ Spores can survive for up to 70 days ○ Contact precautions – gown, gloves ○ Lactobacillus probiotic used as preventative ○ Oral vancomycin for 10 days is drug of choice ● E.coli – bloody diarrhea ● Giardia lamblia – intestinal parasite Irritable Bowel Syndrome ● Disorder of functional motility - digestion moving too fast or too slow ● S/S ○ Pain, bloating, distention of abdomen ● Diagnosis ○ Abdominal pain or discomfort 1 day per week for 3 months + two of these: ■ Related to defecation ■ Change in frequency of bowel mvts ■ Change in form ● Medications ○ IBS-D ■ Alosetran – women – watch for severe constipation, ischemic colitis ■ Loperamide ■ Dicyclomine – antispasmodic – will decrease motility ○ IBS-C ■ Lubiprostone - women ■ Linaclotide ● Pt teaching ○ Eat a well balanced diet, high fiber ○ Increase fluids, but NOT WITH MEALS Appendicitis ● Inflammation of the appendix (right lower quadrant) ● McBurney’s point ○ Halfway between umbilicus and right iliac crest ● S/S ○ Early: dull, periumbilical pain, anorexia, N/V ○ Later: Persistent pain at MB’s point, fever, rebound tenderness, rigidity, guarding ● Nursing Care: prevent fluid volume deficit, relieve pain, prevent complications ○ IV fluids, antibiotics, analgesics ○ Surgery → appendectomy to avoid rupture Diverticular Disease ● Diverticula - one pouch ● Diverticulosis - multiple pouches, typically asymptomatic ● Diverticulitis - inflamed pouches ● Mainly caused by low fiber diet, sedentary lifestyle, obesity, excess alcohol and NSAID use ● S/S ○ LLQ abdominal pain ○ Fever, N/V ○ Bowel freq/form change ● Diagnosis ○ CT scan with oral contrast ○ Sigmoidoscopy or colonoscopy ● Management ○ Pt will have decreased/absent abdominal sounds ○ Prevention: high-fiber, reduced red meat and fat ○ Acute diverticulitis – bowel rest to reduce inflammation, clear liquids, bed rest, analgesia ■ No barium enema – risk of perforation ○ Severe – hospitalization, NG tube, IV fluids and antibiotics, monitor for abscess and peritonitis ○ No morphine for pain – will increase intraluminal pressure Peritonitis ● Inflammation of the peritoneum ● Primary peritonitis → blood-borne pathogen enters peritoneal cavity ○ Cirrhosis with ascites ○ Genital tract organisms ● Secondary peritonitis → perforation of abdominal organs ○ Ruptured appendix** ○ Peritoneal dialysis ○ Perforated gastric/duodenal ulcer ○ Gunshot or knife wounds ● S/S ○ Diffuse abdominal pain at first, but then becomes more local and intense pain ○ Tenderness over the area that is involved** ● Complication ○ Hypovolemic shock** ○ Sepsis ● Care ○ Antibiotics ○ IV fluids ○ NG suction – decompress gastric area, decrease distention ○ Analgesics ○ Monitor I/Os and electrolytes ○ Position pt with knees flexed for comfort Colorectal Cancer ● Risk factor: red meat, smoking, alcohol ● Adenocarcinoma – most common type of carcinoma involved with colorectal cancer ● Insidious onset ● Right sided lesions – diarrhea, bleeding (unrecognized, early sign of anemia) ● Left sided lesions – present with bowel obstruction, hematochezia (fresh blood in stool) ● Complications: obstruction, bleeding, perforation, peritonitis, fistula formation ● Tenesmus – cramping rectal pain, feels like have not completely pooped ● Colonoscopy is gold standard ○ Starting at 45 until 75, every 10 years ○ High-risk, start at 40 and every 5 years ● Stages ○ 0 – NOT grown beyond mucosal layer ○ 1 – grown into submucosa ○ 2 – grown into muscle ○ 3 – lymph node involvement ○ 4 – spread to other organs Inflammatory Bowel Disease – Chronic, inflammation of GI tract characterized by periods of remission are interspersed with periods of exacerbation ● Two types: ○ Crohn’s Disease ■ Anywhere in the GI tract, mouth to anus ■ Skip lesions – reas of normal tissue, areas of inflamed tissue ■ All layers of bowel wall ● Cobblestone appearance from deep ulcerations ■ Rectal bleeding ■ Diarrhea, cramping ■ Fistulas are common ○ Ulcerative Colitis ■ Only in the colon – starts in rectum, spreads to cecum ■ Bloody diarrhea ■ Mucosal (inner) layer ● Electrolyte loss – can’t absorb through inflamed tissue ■ Pseudopolyps – tongue-like projections into bowel ● Complications ○ Perforations with possible peritonitis ● Management ○ High-calorie, high protein, high-vitamin diet ● Drugs ○ 5-ASA (sulfasalazine, mesalamine) and steroids (prednisone) – Decrease inflammation ○ Antimicrobials – Prevent or treat infection ○ Immunosuppressants – Suppress immune response