Respiratory System: Gas Exchange & Transport Presentation
advertisement
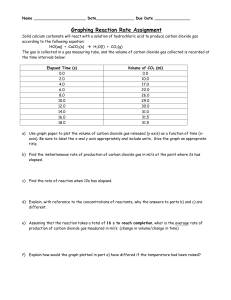
The Respiratory System Gas Exchange and Transport Presented by: Shannel Morgan, Marie Rene, JC Rodriguez Pulmonary Gas Exchange Pulmonary Gas Exchange Pulmonary gas exchange or external respiration is the process of removing CO2 from blood and replenishing oxygen supply. It occurs between alveoli and the blood of lungs. Pulmonary gas exchange occurs by diffusion and depends on pressure gradient. Inspired air consists of a mixture of gases including oxygen and carbon dioxide with individual pressures called pressure gradient. Pulmonary Gas Exchange Differences in the partial pressures between the gases in the alveoli and blood create a pressure gradient across the respiratory membrane. When the partial pressures of O2 and CO2 are different gas exchange occurs. Diffusion occurs as the freshly inspired air in the alveoli is high in O2, the O2 diffuses across the respiratory membrane into the blood where the concentration of O2 is low. This blood is now ‘oxygenated’ and is sent to the tissues of the body for use. Figure 1: Oxygen from the inhaled air diffuses through the walls of the alveoli and the capillaries into the red blood cells, which carry it through the blood to the body tissues. Carbon dioxide produced by the body’s tissues returns to the alveoli via the blood. It then diffuses across the capillary and respiratory membranes into the air space to be removed by expiration Systemic Gas Exchange Systemic Gas Exchange The exchange of gases between blood in systemic capillaries and body cells is called internal respiration. Oxygen molecules move rapidly out of the blood through the systemic capillary membrane into the interstitial fluid and cell tissues. Carbon dioxide molecules leave cells , diffuse through the interstitial fluid then enters systemic capillaries eventually transported to lungs for elimination from the body. Systemic Gas Exchange Diffusion results in the movement of oxygen from an area of high partial pressure (Po2, 100 mm Hg) to lower partial pressure ( Po2, 40 mm Hg) in cells where it’s needed. Diffusion is also responsible for movement of carbon dioxide from an area of high partial pressure (Pco2, 46 mm Hg) to lower partial pressure ( Pco2,43 mm Hg) in the systemic capillaries. Systemic Gas Exchange Figure 2: Oxygen diffuses out of the capillary and into cells, whereas carbon dioxide diffuses out of cells and into the capillary. Figure 3 Blood Transportation of Gases Blood Transportation of Gases Blood transports the respiratory gases, oxygen and carbon dioxide in both dissolved or combined states with other chemicals. Respiratory gases dissolve in the plasma , and rapidly form a chemical union with hemoglobin or water. Once gas molecules bound to another molecule, their plasma concentration decreases, and more gas can diffuse into the plasma. Transport of Oxygen Transport of Oxygen The total amount of oxygen that blood can transport is 20.4 ml in 100ml of blood, only about 1.3 ml is dissolved. Oxygen combines with blood to form oxyhemoglobin (Hb02) so that it can be carried to the tissues. Oxygenated blood is found in the systemic arteries and pulmonary veins. Transport of Oxygen The difference in oxygen saturation results from the release of oxygen from oxyhemoglobin to supply body cells. In summary, oxygen travels in two forms, as dissolved O2 in the plasma and as a combination of O2 and hemoglobin (oxyhemoglobin). Oxyhemoglobin carries vast majority of the total oxygen transported TRANSPORT Of CARBON DIOXIDE Transport of Carbon Dioxide Carbon dioxide is a by-product of cellular metabolism and plays a vital role in regulating pH of body fluids. If carbon dioxide accumulates in the body beyond normal limits, it can quickly become toxic. Elimination of excess Co2 from the body occurs when it enters the alveoli and expelled during expiration. Transport of Carbon Dioxide Co2 must be transported in the blood in one of three forms, carbon dioxide, carbaminohemoglobin and bicarbonate. Approximately, 10% of the total amount of carbon dioxide in blood is carried in the dissolved form. This dissolved Co2 produces Pco2 of the blood plasma. Transport of Carbon Dioxide About 20% of the total CO2 transported in the blood is in the form of carbaheminoglobin ( HbCO2). Carbaheminoglobin is formed by the union of carbon dioxide and hemoglobin. When Co2 dissolves in water, some of the Co2 molecules associate with water (H20) to form carbonic acid. Transport of Carbon Dioxide • Once formed some of the carbonic acid molecules dissociate to form hydrogen and bicarbonate ions. • The rate of this process is increases dramatically within red blood cells because the presence of an enzyme called carbonic anhydrase. Quick Check Question 1: What is Internal Respiration? Answer: The exchange of gases that occurs between blood in systemic capillaries and the body cells is called internal respiration Question 2: In what form does most oxygen travel in the blood? Answer: Oxygen combines with the hemoglobin in the blood to form oxyhemoglobin (HbO2) so that it can be carried to the tissues and used by the body cells. Question 3: In what three forms does carbon dioxide travel in the blood? Answer: Carbon dioxide is transported in the blood to the lungs in one of three forms: • 1. As dissolved carbon dioxide (CO2) • 2. As carbaminohemoglobin (HbCO2) • 3. As bicarbonate ions (HCO3−). THANK YOU