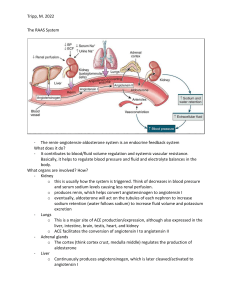
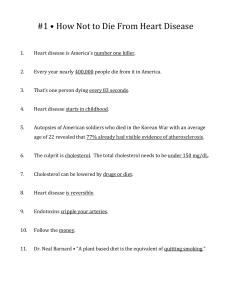
Dobutamine – Positive inotropic agent = Increased contractility and cardiac output, but not heart rate (decreased chance of irregular heartbeat; no change in peripheral resistance. ONLY for ACUTE HF; Chronic HF = Increased doses = Increased HR = Increased workload of heart = Greater HF Furosemide – Loop diuretic = Induce fluid loss = Decrease blood volume Digitalis – Positive inotropic agent = Increased contractility Brain Natriuretic Peptide – Increased and released by the ventricles in response to pressure and volume overload – Biomarker for heart failure; Drugs that increase BNP = promotion of diuresis, natriuresis, and vasodilation of systemic and pulmonary vascular, and reduce circulating levels of endothelin and aldosterone Atrial Natriuretic Peptide – Increased excretion of Na+ and water (decreased blood volume), promotes vasodilation, inhibit renin secretion (Inhibit angiotensinogen to angiotensin I conversion = reduced formation of angiotensin II = vasodilation; NORMAL: Angiotensinogen -> *Renin* -> Angiotensin I -> *ACE* -> Angiotensin II: Cardiac and vascular hypertrophy, Systemic Vasoconstriction, Increased thirst = increased blood volume, Stimulate Adrenal Cortex release of Aldosterone = Renal sodium and fluid retention, Simulate Pituitary release of ADH = Renal sodium and fluid retention), Antagonizes the effects of angiotensin II and ADH Sulfa Drugs = Antibiotics Primaquine = Antimalarials Aspirin = Antipyretics Statins – Inhibition of cholesterol synthesis by competitively binding to HMG CoA Synthase (Ratelimiting) PCSK9 Inhibitors = Increased LDLR (inhibits degradation of LDLR); Monoc. Ab against PCSK9 = inactivate Bile Acid Binding Drugs (Cholestyramine) – Reduces reuptake of bile acids in terminal ileum and the liver uses free cholesterol to synthesize bile acids = increased hepatic LDLR synthesis because cytosolic free cholesterol levels are lower than normal Ezetimibe – Inhibits intestinal cholesterol transporter Verapamil – Calcium Channel Blocker = Negative Inotrope Propranolol – Beta Receptor Blocker = Negative Inotrope; decreases HR (chronotrope) and decreased conduction velocity Warfarin – Blocks Vitamin K Epoxide Reductase = Decreased regeneration of active Vitamin K – Prothrombin (F2), F7, F9, F10 and Protein C+S required Vitamin K as a cofactor/coenzyme Heparin – Activates antithrombin 3 (inhibits F10 of common pathway) and inactivates thrombin Streptokinase/Urokinase – Thrombolytic agent, plasminogen activator – Converts plasminogen to plasmin enabling dissolution of clots Tissue Plasminogen Activator – Dissolves thrombus Digoxin – Treat HF, controls ventricular rate in atrial fibrillation; class of glycosides; Positive inotropic and negative chronotropic activity -> Digoxin inhibits Na-K ATPase – Increased Calcium = Increased contraction Prazosin