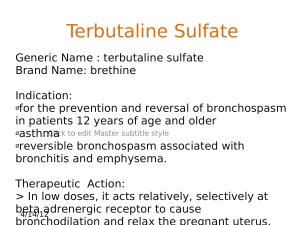
. Objectives Adrenergic and Antiadrenergic Drugs Dr. Anusha Vohra PHOD, Pharmacology The students should be able to • Classify Adrenergic and Anti-adrenergic drugs. • Describe mechanism of action, types, doses, side effects, indications and contraindications of adrenergic drugs • Describe mechanism of action, types, doses, side effects, indications and contraindications of anti-adrenergic drugs • NT: NA- most of the sites Drugs acting on Adrenergic neurons s • 1. Di-Hydroxy-Phenylalanine (DOPA) by tyrosine hydroxylase- metyrosine – Pheochromocytoma • 2. Reserpine, tetrabenazine, valbenazine - DA-(dopamine beta hydroxylase)-NA [disulfiram] • Noradrenaline is converted to adrenaline in adrenal medulla by phenylethanolamine-N- methyltransferase • Sympathetic neurons lack this enzyme 1 . Directly acting sympathomimetics Classification of adrenergic drugs based on action • Pressor agents: Noradrenaline, Ephedrine, Dopamine, Phenylnephrine, Methoxamine, Mephentermine • Cardiac Stimulants: Adrenaline, Isoprenaline, Dobutamine • Bronchodilators: -SA: Salbutamol, Terbutaline -LA: Salmeterol, Formoterol -Very LA: Indacaterol, Vilanterol • Nasal Decongestants: Phenylnephrine, Xylometazoline, Oxymetazoline, Naphazoline, Pseudoephedrine, Phenylpropanolamine (PPA) • CNS stimulants: Amphetamine, Dexamphetamine, Methamphetamine • Anorectics: Fenfluramine, Dexfenfluramine, Sibutramine • Uterine Relaxants and vasodilators : Ritodrine, Isoxsuprine Sympathomimetics uses Non catecholamines Catecholamines • Adrenaline is a drug of choice for Anaphylactic shock -0.5 ML 1:1000 solution i.m. injection • It prolong the duration of action and decrease systemic toxicity of local anesthetic • It is also used in cardiac arrest preferred route is iv followed by Intra osseus and endotracheal • Dopamine is the drug of choice for cardiogenic shock with oliguric renal failure • agonists: as nasal decongestant -can result in after congestion and atrophic rhinitis • As Mydriatic • As Vasopressors • agonist: Clonidine and Alpha methyldopa (prodrug)- in hypertension, Diabetic diarrhoea, prophylaxis of migraine, management of withdrawal symptoms, epidurally with opioids for pain relief, ADHD and Tourette's syndrome -Apraclonidine and brimonidine used topically in glaucoma -Dexmeditomidine: (sedation) as preanesthetic medication -Tizanidine muscle relaxant Indirectly acting sympathomimetics • Beta one agonists: Prenalterol: in reversing beta blockade • Beta two agonist: Salbutamol-in bronchial asthma -Ritodrine, Isoxsuprine: Preterm labor • Beta three agonist: Mirabegron: overactive bladder �Tachyphylaxis ( rapid development of tolerance) �Tyramine- cheese reaction with MAO inhibiters �Methylphenidate, Amphetamine -ADHD �Modafinil- narcolepsy, in shift workers, to relieve fatigue in multiple sclerosis, as an adjunct in obstructive sleep apnea Mixed action sympathomimetics Ephedrine and pseudoephedrine: nasal decongestant, as bronchodilator in bronchial asthma, as vasopressor of choice in pregnancy 2 . Uses of Adrenergic Drugs ?? Antiadrenergic drugs Alpha blockers Cont- -Nonselective Alpha blockers Phenoxybenzamine: Irreversible antagonist Sympatholytic drugs Selective A1 blockers Phentolamine and tolazoline: Reversible blockers • Prazosin, terazosin, doxazosin and alfuzosin �Decrease in blood pressure with lesser tachycardia �favorable effect on lipid profile �drug of choice for patients with hypertension and benign hyperplasia of prostate (BHP) �Tamsulosin and silodosin: Selectively inhibit alpha1A subtype present in prostate (BHP) – cause Floppy iris syndrome during cataract surgery �Treatment of scorpion sting �Adverse effect: postural hypotension (first dose effect), inhibition of ejaculation • Phenoxybenzamine used to prevent hypertensive episodes in during operative manipulation of tumor in pheochromocytoma • Phentolamine and Tolazoline:in treatment of hypertensive crisis in Clonidine withdrawal and cheese reaction Selective A2 blocker • Yohimbine • no established clinical role 3 . Beta blockers Effects • nonselective beta blockers (first generation) �Propranolol, timolol, nadolol, pindolol, alprenolol and oxprenolol �Useful in classical angina but contraindicated in variant angina �Decrease in blood pressure • Heart • Blood vessels • Respiratory • Skeletal muscles • Metabolic • CNS • Eye • Local Anaesthetic effect Limitations Contraindications of non-selective Beta blockers • Contraindicated in bronchial asthma • Hypoglycemia in diabetic patients receiving insulin and oral hypoglycemic drugs • Adversely effect serum lipid profile and can cause glucose intolerance • Contraindicated in peripheral vascular disease • Impair exercise capacity • A-Asthma • B-Block (AV) • C-CHF • D-Diabetes Cardio selective / Second generation beta blockers Beta Blockers with intrinsic sympathomimetic activity (ISA) Preferred in patients with DM, BA, PVD or hyperlipidemia • N-Nebivolol (most cardioselective) • B-Betaxolol • B-Bisoprolol • A-Acebutalol • E-Esmolol • A-Atenolol • M-Metoprolol • C-Celiprolol New Beta Blockers Acting Exclusively At MyoCardium �Preferred in patients prone to develop severe bradycardia �Less useful in angina • C-Celiprolol, Oxprenolol • P-Pindolol, Penbutolol • A-Alprenolol • A-Acebutolol �COntain Partial Agonistic Activity 4 . Beta blockers with membrane-stabilizing action Lipid-Insoluble Beta Blockers �Sodium channel blocking (LA) activity �Contribute to antiarrhythmic action �Avoided in glaucoma • P-Propranolol (maximum) • M-Metoprolol • L-Labetalol • A-Acebutolol • P-Pindolol �Possess Membrane stabilizing or Local Anaesthetic Property �Mainly excreted by kidney and CI in Renal Failure �Long duration of Action • N-Nadolol (longest acting) • S-Sotalol • A-Atenolol, Acebutolol (all Activities) • B-Betaxolol, Bisoprolol • C-Celiprolol �Not Soluble ABC Third-Generation Beta-Blockers Indications of beta blockers • Additional Vasodilatory property • Alpha block:-Labetalol, Carvedilol (hypertensive episodes in pheochromocytoma, CHF) • Beta 2 agonism:-Celiprolol, Carteolol, Bopindolol • Release of NO:-Nebivolol, Celiprolol • Opening of Potassium channel:-Tilisolol • Inhibition of Ca2+ channels:- Carvedilol, Betaxolol • Antioxidant activity : Carvedilol Cardiac (beta 1 block) Extracardiac (beta 2 block) Hypertension Pheochromocytoma (after alpha block) Classical Angina Hyperthyroidism Myocardial Infarction Performance anxiety Supraventricular Arrhythmias Tremors Chronic CHF (Carvedilol) Akathisia Hypertrophic Obstructive Cardiomyopathy (DOC) Prophylaxis of Migraine Emergency Management of symptoms of TOF Glaucoma (Timolol and Betaxolol) Mitral valve prolapse Alcohol and Opioid withdrawal Prophylaxis of bleeding in portal hypertension Objectives Self Directed Learning Cycle The students should be able to • Classify adrenergic and antiadrenergic drugs • Describe mechanism of action, types, doses, side effects, indications and contraindications of adrenergic drugs • Describe mechanism of action, types, doses, side effects, indications and contraindications of anti-adrenergic drugs 5