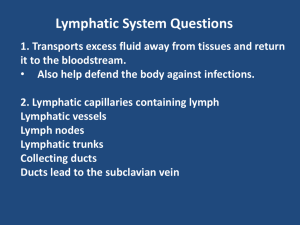
Inflammation and Tissue Healing - Big Ideas Big Ideas Inflammation Non-specific protection Fever o hypothalamus raises body temperature to make the organism inhospitable to pathogens o not always present especially in consideration of: age immunocompromise Initial injury/infection o Brief vasoconstriction o Chemotaxis attracts neutrophils Marginization: Integrin receptors activate and stick to integrins causing neutrophil to stop rolling and accumulate along margins of endothelium Mast cell degranulation: release histamine Cause vasodilation (redness, heat) Endothelial cells contract, causing spaces between cells Fluid and small particles escape from blood vessel into tissue (edema) Neutrophils undergo diapedesis and move into tissue, monocytes that move into tissue are macrophages Bradykinin release causes pain (dolor) Interleukin-1 (of many) is the initial pro-inflammatory chemokine initiating fever and signaling activation of many systemic and cellular activities. o o Cellular response to injury Cell wall contains arachadonic acid which is released in assault (whatever breaks up cell wall - trauma or chemo receptor response) Arachadonic acid creates COX-1 and COX-2 as well as lipoxygenase These stimulate creation of several immune modulating substances, most noteably specific prostaglandins(by COX) and leukotrienes (by lipoxygenase) Different prostglandins have different effects; Some are "constitutional" and considered protective. Some only involved in the inflammation process and are "induced" by that process. Pediatric and Elderly Immaturity of processes per physiologic developmental norms must be considered for infants, children. Less efficient immune response, effects of aging on collagen and chronic disease in either must be considered. 3. CBC with differential WBC (total count) norm per LEWIS appendix C Differential cell types purposes, possible interpretation of high and low Elevation in bands indicates infection of some type (shift to left) 4. Wound healing Factors that improve wound healing o Consistent moisture o Consistent temperature o Consistent pH o Proper nutrition o Vasculature properly functioning - provide protection from ischemia. Factors to assess o REEDA Redness Edema Ecchymoses Drainage Approximation Factors that decrease wound healing o Infection o Abscesses o Hematoma o Decreased blood flow (ischemia) o Aging/children and developmental factors Healthy wound bed: granulation tissue (beefy-red) with blurry edges, no colored exudate or slough Review of immune physiology COMPONENTS OF THE IMMUNE SYSTEM The primary lymphoid organs are the thymus and bone marrow. T cells develop in the thymus, whereas B cells develop in the bone marrow. Mature lymphocytes then migrate to secondary lymphoid structures, including the spleen and lymph nodes. Blood cells are produced in the bone marrow in response to specific hematopoietic growth factors. Granulocytes (neutrophils, basophils, eosinophils) and monocytes (macrophages) are phagocytic cells that provide innate protection. Lymphocytes (B cells, T cells) are specific cells that react only to particular antigens. NK cells are lymphocytes that lack T-cell and B-cell markers and function in innate immune responses. Other blood components produced by bone marrow are erythrocytes and platelets. Neutrophils are the most numerous WBCs in blood. A large storage pool lies in the bone marrow and can be mobilized in response to antigen. Neutrophils are the predominant WBC type in early infection. They migrate to the area by following chemotactic factors and perform phagocytic functions. During acute bacterial infection, larger numbers of immature neutrophils (bands) are released into the blood, which is termed a shift to the left. Chronic infections may produce a shift to the right with more segmented neutrophils than normal. Monocytes located in tissue are called macrophages. Monocytes and macrophages are distributed in strategic locations throughout the body, including the skin, lungs, gastrointestinal tract, liver, spleen, and lymph. Macrophages are powerful phagocytes and are predominant in late inflammation. T lymphocytes, the major effectors of cell-mediated immunity, interact with specific antigens on cell surfaces. They are important in immunity against foreign, infected, or mutant cells. In addition, they secrete cytokines that boost the immune response of B cells and other cell types. T cells are composed of two main subtypes called CD4 (helper) and CD8 (cytotoxic). B lymphocytes are the major effectors of antibody-mediated immunity. The complement system consists of about 20 plasma proteins that interact in a cascade fashion to produce important mediators of inflammation and immunity. The cascade can be activated by microbial antigens (alternative pathway) or by antigen-antibody complexes (classical pathway). Cytokines are peptide factors released by immune cells. They have many functions, including as inflammatory mediators, chemotaxins, intercellular communication signals, growth factors, and growth inhibitors. Macrophages and lymphocytes are important sources of immune cytokines. INNATE DEFENSES AND INFLAMMATION Previous exposure to foreign antigens is not required for the activation of innate immune defenses. Inflammation is an important aspect of innate immunity that involves localization of harmful agents and the bringing of phagocytic cells to the area. Classic manifestations of inflammation are redness, swelling, heat, pain, and loss of function. Inflammatory chemicals such as histamine, prostaglandins, and leukotrienes are released from injured tissues, mast cells, macrophages, and neutrophils. These chemicals increase vascular permeability, vasodilate, and attract immune cells to the area (chemotaxis). Phagocytes migrate to the inflamed area, collect at the side of the vessel, and squeeze through into the tissue. Emigration of neutrophils and macrophages is facilitated by selectins and integrins present on the surface of endothelial cells and leukocytes. Neutrophils arrive in large numbers in acute bacterial infection and begin active phagocytosis. Neutrophils and macrophages produce proteolytic enzymes and oxidizing agents to destroy and digest antigens. With chronic inflammation, macrophages and lymphocytes predominate. Healing is mediated by growth factors released from platelets and immune cells that stimulate fibroblasts to divide and manufacture extracellular matrix proteins. Endothelial cells respond to angiogenic growth factors by forming capillary networks. Inflammatory exudate functions to transport immune cells, antibodies, and nutrients to the tissue and dilute the offending substances. Serous exudate is watery and low in protein; fibrinous exudate is thick, sticky, and high in protein; purulent exudate contains infective organisms, leukocytes, and cellular debris; and hemorrhagic exudate contains red blood cells. Systemic manifestations of inflammation include fever, neutrophilia, lethargy, muscle catabolism, increased acute phase proteins (CRP), and increased ESR. These responses are attributable to the IL-1, IL-6, and TNF-α released from macrophages and inflamed tissues. SPECIFIC ADAPTIVE IMMUNITY Specific immunity refers to functions of B and T lymphocytes. Each lymphocyte recognizes and reacts to only one particular antigen. On initial exposure to an antigen, lymphocytes undergo clonal expansion so that many lymphocytes are distributed throughout the body that can recognize and react to that particular antigen. These cells are called memory cells. Subsequent exposure results in a much faster and larger lymphocyte response. T lymphocytes are able to bind antigens only when they are displayed on the surface of cells. Cytotoxic T cells (CD8+) react to cells that have foreign MHC class I proteins on their surface. T helper cells (CD4+) bind to cells that have MHC class II proteins on their surface. MHC class II proteins are found on antigen-presenting cells (B cells, dendritic cells, and macrophages). These cells engulf foreign antigens and combine the antigens with MHC class II proteins on their cell surface. T cells, which mature in the thymus, have two major subgroups: T helper cells and cytotoxic T cells. T helper cells perform a central role in specific immunity. Activation of T helper cells results in secretion of the cytokines necessary for clonal expansion of T and B lymphocytes. Cytotoxic T cells locate and lyse abnormal cells through the actions of perforins. B- and T-cell functions are interdependent. T cells cannot respond to soluble antigens. B cells can process free antigen and present it to T cells. On first exposure, B cells are minimally activated by antigen unless they are stimulated by cytokines and coreceptors from T cells. B lymphocytes mature in bone marrow and lymph tissue. B cells have receptors on their surfaces that can bind antigens. Each B cell binds only one particular antigen. With appropriate T helper cell help, antigen binding causes the B cell to divide (clonal expansion). Some of the daughter cells become plasma cells, which actively produce and secrete antibodies. Other daughter cells (memory cells) resemble the original cell and are distributed in lymph throughout the body. On subsequent exposure to the antigen, antibody production is rapid. Antibodies are proteins that specifically bind a particular antigen. Antibodies have several functions, including precipitation, agglutination, neutralization, opsonization, and complement activation. The five major antibody classes are IgG, IgM, IgA, IgD, and IgE. Antibody class is determined by the structure of the Fc portion. IgG is the most prevalent antibody class (75%). IgM is the first kind to be produced on antigen exposure. IgA is found primarily in body secretions. IgD is present on the B-cell membrane and functions in signal transduction. IgE binds to basophil and mast cell membranes and mediates inflammation and allergy. Administration of preformed antibodies confers passive immunity. Passive immunity provides immediate but temporary protection. Active immunity occurs when individuals are exposed to antigen that stimulates their own lymphocytes to produce memory cells. Active immunity confers long-term protection but may take several weeks to develop. INTEGRATED FUNCTION AND REGULATION OF THE IMMUNE SYSTEM Specific and innate immune cells work together to protect the body from foreign antigens. Macrophages and dendritic cells play a central role because they are commonly the first immune cells to encounter the antigen. Macrophages secrete cytokines that stimulate WBC production and help WBCs locate the area. Tissue reactions activate the clotting cascade and kinin system, which help to localize the antigen and promote movement of fluid and immune cells into the tissue. Macrophages and dendritic cells are antigen-presenting cells that engulf and display antigen on their cell surface in association with MHC class II proteins. T helper cells are specifically activated by these antigen-presenting cells. T helper cells secrete cytokines that stimulate the production of WBCs in the marrow, initiate proliferation of mature B and T cells, and stimulate the phagocytic potential of macrophages and neutrophils. B-cell proliferation and antibody secretion usually require T-cell help. B cells internalize and present antigen to T cells, which then stimulate B-cell proliferation. B cells secrete antibodies that help phagocytic cells localize and destroy antigens. The immune response to primary exposure is slow and often insufficient to prevent illness. Memory cells that develop during primary exposure can mount a more effective response on subsequent exposure and usually prevent manifestations of illness. T and B lymphocytes must be tolerant to self. T lymphocytes capable of reacting with self tissue are thought to be destroyed or permanently inactivated during development in the thymus. One theory suggests that lymphocytes must come in contact with all self antigens during development, and those that do not specifically bind self antigens are allowed to survive. B cells are subject to careful regulation by T helper cells and by negative feedback from high concentrations of circulating antigen-antibody complexes. Mechanisms to inhibit and control the immune response include regulatory T-cell cytokines, complement inhibitors, degradation of inflammatory mediators, circulating antiproteases, and antioxidants.