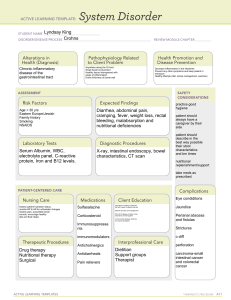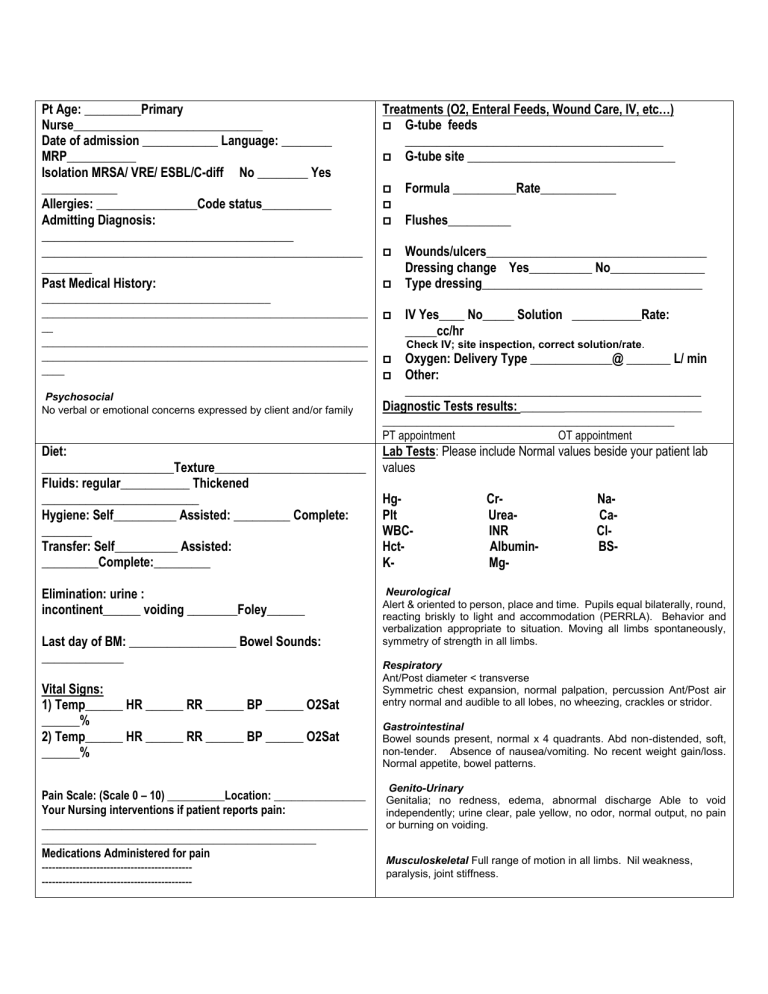
Pt Age: _________Primary Nurse______________________________ Date of admission ____________ Language: ________ MRP___________ Isolation MRSA/ VRE/ ESBL/C-diff No ________ Yes ____________ Allergies: ________________Code status___________ Admitting Diagnosis: ________________________________________ ___________________________________________________ ________ Past Medical History: ________________________________________ _________________________________________________________ __ _________________________________________________________ _________________________________________________________ ____ Psychosocial No verbal or emotional concerns expressed by client and/or family Treatments (O2, Enteral Feeds, Wound Care, IV, etc…) G-tube feeds _________________________________________ G-tube site _________________________________ Formula __________Rate____________ Flushes__________ Wounds/ulcers___________________________________ Dressing change Yes__________ No_______________ Type dressing___________________________________ IV Yes____ No_____ Solution ___________Rate: _____cc/hr Check IV; site inspection, correct solution/rate. Oxygen: Delivery Type _____________@ _______ L/ min Other: _______________________________________________ Diagnostic Tests results: _______________________________ ___________________________________________________ PT appointment OT appointment Diet: _____________________Texture________________________ Fluids: regular___________ Thickened _________________________ Hygiene: Self__________ Assisted: _________ Complete: ________ Transfer: Self__________ Assisted: _________Complete:_________ Lab Tests: Please include Normal values beside your patient lab values Elimination: urine : incontinent______ voiding ________Foley______ Neurological Alert & oriented to person, place and time. Pupils equal bilaterally, round, reacting briskly to light and accommodation (PERRLA). Behavior and verbalization appropriate to situation. Moving all limbs spontaneously, symmetry of strength in all limbs. Last day of BM: _________________ Bowel Sounds: _____________ Vital Signs: 1) Temp______ HR ______ RR ______ BP ______ O2Sat ______% 2) Temp______ HR ______ RR ______ BP ______ O2Sat ______% Pain Scale: (Scale 0 – 10) __________Location: ________________ Your Nursing interventions if patient reports pain: _________________________________________________________ ________________________________________________ Medications Administered for pain --------------------------------------------------------------------------------------- HgPlt WBCHctK- CrUreaINR AlbuminMg- NaCaClBS- Respiratory Ant/Post diameter < transverse Symmetric chest expansion, normal palpation, percussion Ant/Post air entry normal and audible to all lobes, no wheezing, crackles or stridor. Gastrointestinal Bowel sounds present, normal x 4 quadrants. Abd non-distended, soft, non-tender. Absence of nausea/vomiting. No recent weight gain/loss. Normal appetite, bowel patterns. Genito-Urinary Genitalia; no redness, edema, abnormal discharge Able to void independently; urine clear, pale yellow, no odor, normal output, no pain or burning on voiding. Musculoskeletal Full range of motion in all limbs. Nil weakness, paralysis, joint stiffness. Medication name, dose, route, time of administration Time Drug Name/Action Plan of Care for Patient/Nursing Interventions Side Effects Patient Education PRN Medications: Other