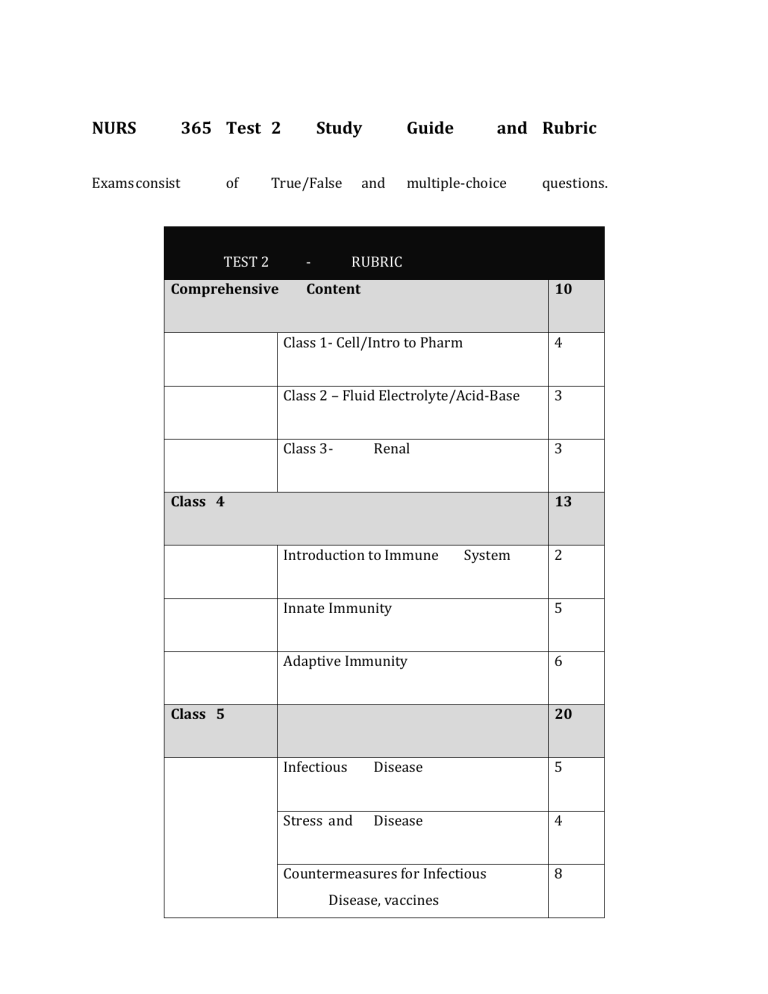
NURS 365 Test 2 Exams consist of Study Guide True/False and - RUBRIC TEST 2 Comprehensive and Rubric multiple-choice Content questions. 10 Class 1- Cell/Intro to Pharm 4 Class 2 – Fluid Electrolyte/Acid-Base 3 Class 3 - 3 Renal Class 4 13 Introduction to Immune System 2 Innate Immunity 5 Adaptive Immunity 6 Class 5 20 Infectious Disease 5 Stress and Disease 4 Countermeasures for Infectious Disease, vaccines 8 Immunodeficiencies Class 6 3 17 Hypersensitivities 4 Wound 2 Healing Autoimmunity, Alloimmunity 4 Anti-virals 2 Drugs: Antihistamines, Glucocorticoids, 5 Anti-inflammatories Total 60 1. CLASS 4 a. Introduction to the Immune System i. The two major lymphoid organs (immature lymphocytes) a Bone Marrow i b Central lymphoid tissue for B lymphocytes Thymus i Central lymphoid tissue for T lymphocytes ii. Secondary Lymphoid organs (mature lymphocytes) a Lymph nodes b Spleen iii. The cell types including cell surface markers, location, and function a Cells of the immune system i Have a very specific developmental pattern ii Have highly specific functions and characteristics iii Can be identified by a specific protein on its cell surface. This is called a Cluster of Differention or CD marker iv B cells 1 Develop in the bone Marrow 2 Have specific antigen receptor called the B cell receptor (BCR) 3 Primary function of the B cell is to make antibody. A fully differentiated B cell is called a Plasma Cell 4 v Identified by the presence of CD19 or CD20 T cells 1 Develop in the Thymus 2 All T cells are CD3+ 3 Have a specific receptor – The cell receptor (TCR) – used to identify antigen 4 Subsets a Cytotoxic T cells (CTL) – Kill tumor cells and virus infected cells. CD8+ b Helper T cells (TH) – help other cells by making important proteins (cytokines). CD4+ i CD4+ cells can be divided into even more groups ii HIV targets CD4 cells, disrupting cell-mediated and antibody immune response vi Natural Killer Cells 1 Specialized cells that kill tumor or virus infected cells 2 Do not have memory, if they see infected cell, they kill it 3 Cell surface receptor: Killer Inhibitory Receptor (KIR) 4 CD56+ vii Dendritic Cells 1 “Professional antigen presenting cells” best at “eating” antigen and presenting it to T cells and/or B cells 2 Found in tissues such as epidermis, mucous membranes CD11c+ viii Granulocytes (major role = phagocytosis) 1 These cells are CD66b+ but can be differentiated from one another by staining 2 Types a Neutrophils (60-70% of granulocytes) i Most abundant cell type in circulation ii Professional phagocyte – important in killing of microorganism iii Part of the Pus at an infected site iv Short lived at infected site v First immune cells to be recruited, which can be through the cytokines produced by macrophages b Eosinophils i Important in parasite clearance but is also associated with allergic disease ii Gets its name because of “eosin” stain iii Kills antibody-coated parasites c Basophils i Found in blood – least abundant cell type ii Get name from “basic” staining iii Promotion of allergic responses and augmentation of antiparasitic immunity ix Monocytes and Macrophages 1 Primary function is phagocytosis 2 Develop in the bone marrow and enter the circulation as monocyte 3 When monocytes are appropriately activated or enter into appropriate tissues they become macrophages 4 x CD14+ Mast Cells 1 Best known role: in allergy, involved in wound healing and defense against pathogens 2 Found in tissue 3 Release preformed granules containing proteases and histamines 4 Histamines help get WBC to the cite of infection iv. The breakdown of a WBC a Men and nonpregnant women: 4500-11,000/mcL3 b Differential: i Neutrophils: 50-62% ii Band neutrophils: 3-6% iii Lymphocytes:25-40% iv Monocytes:3-7% v Eosinophils: 0-3% vi Basophils: 0-1% v. Definitions a Immunity: Ability to resist infection b Antigen: any substance capable of causing an immune response c Tolerance: Immune system normally responds to non-self antigens, but maintains tolerance to self antigens d Breakdown in tolerance: immune responses are not always beneficial and cause tissue damage or death e Lymphatic vessels (lymphatics): carry lymph and work in complement to blood vessels b. Innate and Adaptive Immunity i. Innate (Not antigen-specific, rapid) a Defense mechanisms existing before antigen exposure (rapid onset) i Does not distinguish among antigens (Not antigen specific) ii No enhanced response on second antigen exposure (No memory) iii Promotes initiation of adaptive responses (Antigen presenting cells APCs) iv Although the innate immune system is non-specific, it is selective and can distinguish self from non self b Physical/Mechanical/Chemical Barriers i Physical 1 Oral Mucosa: secretions 2 Gastric Secretions 3 Intact skin ii Mechanical Barriers 1. Cilia in lungs 2. Epithelial cells joined by tight junctions iii BioChemical Barriers 1 ii. Surfactants in lungs Phagocytosis a Steps i Bacterium is phagocytosed by neutrophil ii Phagosome fuses with granules iii pH of phagosome rises, antimicrobial response is activated via lysosomes and bacterium is killed iv pH of phagosome decreases, fusion with lysomes allows acid hydrolases to degrade the bacterium completely v Neutrophil dies by apoptosis and is phagocytosed by macrophage b Outputs of pathogen recognition: These are released once we recognize these pathogens i Cytokines 1 Inflammation 2 Key cytokines a IL-1 (interleukin 1) i Fevers ii Production of IL-6 iii Activates vascular endothelium iv Activates lymphocytes v Local tissue destruction vi Increases access of effector cells b TNF-alpha i Fever ii Mobilization of metabolites iii Shock iv Helps with increasing vascular permeability to allow for increased entry of IgG, complement, and cells to tissues and increased fluid drainage to lymph nodes c IL-6 i Fever ii Induces acute phase protein production ii Chemokines 1 Subset of cytokines that use chemotaxis to attract leukocytes and WBCs to the area for iii Surface co-stimulatory molecules 1 Help with enhancing immune cell attraction, can form immune complexes to increase immune response iii. Inflammation a Characteristics i Pain, redness, swelling, heat and loss of function ii Increased vascular permeability and blood flow (TNF-alpha) iii Exudation of plasma fluid (pus) iv Leukocyte recruitment and extravasation v Inflammation is a protective response intended to isolate infected tissues and prevent the spread of disease vi iv. Initial response to injury or infection Acute Phase Response (helps with innate immunity) a Acute phase proteins are important components of innate immunity: i Promote phagocytosis (CRP, MBL (MBP), collectins) ii Promote blood clots (fibrinogen) in small vessels 1 Block spread of infection iii Complement activators (Complement system) iv TLR signaling induces IL-6, which stimulates Liver to produce Acute-phase proteins 1 Bacteria induce macrophages to produce IL-6, which acts on hepatocytes to induce synthesis of acute-phase proteins v. Fever (pyrexia) a Steps i Tissue becomes infected with bacteria, virus, etc ii White blood cells (leukocytes) respond to infection & release a protein iii Interleukin-1 (IL-1) is produced and stimulates production of Prostaglandins iv Prostaglandins cross blood brain barrier stimulate the hypothalamus which triggers the Preoptic Area v Pre-optic area, in response to the hypothalamus, causes ANS to raise body temperature b Elevated temps impede both viral and bacterial replication vi. NK Cells and Antiviral Immunity a Type 1 Interferons (Interferons-alpha, IFN-beta) b Natural Killer (NK) cells i Directly recognize ligands on virally infected cells 1 Kill virally infected cells 2 Ligands / receptors are poorly characterized 3 ii Involved in anti-tumor immunity Recognize ligands on uninfected cells 1 Uninfected cells are spared 2 Ligands = MHC Class I proteins 3 Receptors a Killer lectin-like receptors (KLR) b Killer cell immunoglobulin-like receptors (KIR) vii. Plasma Protein Systems a Complement System = activation of C3 i Cascade of enzymes ii C3 is activated, leading to activation of other enzymes, resulting in increased protein production 1 Opsonin, a assists with phagocytosis iii Part of the innate immune response iv Functions to destroy invaders and signal other immune cells v Consists of 30 proteins synthesized in the liver vi Always present in high concentrations in the blood and tissue vii b Many complement proteins are inactive Clotting System = trapping infection, while also increasing permeability i ii c Fibrinogen 1 Blood clots 2 Chemotactic factor 3 Increased permeability Kinin- interacts with clotting system Kinin System = increasing permeability, and involved with pain i ii Bradykinin 1 Histamine like effects 2 Stimulates nerve endings Work with Prostaglandins to induce pain viii. Adaptive (Antigen-Specific, slow) a 2 step Process i Clonal Diversity (Production of T and B cells with all possible receptors for antigen) 1 Lymphoid Stem cells from Bone marrow migrate to Thymus (T cells) or Bone Marrow (B cells) to mature into immunocompetent T cells/B cells that then reside in secondary lymphoid organs (Spleen/Lymph Nodes) 2 Lymphoid Stem cells are still naïve at this point as they have not encountered an antigen 3 Generation of Clonal Diversity a All necessary receptor specificities are produced b Takes place in the primary (central) lymphoid organs (thymus, bone marrow) c Results in naïve but immunocompetent T and B cells d 4 Primarily occurs in the fetus T cell Development i The thymus is the central lymphoid organ of T cell development ii Development of antigen-specific T cell receptors (TCRs), surface molecules CD4 and CD8 iii Leave thymus, travel to and reside in secondary lymphoid tissue as mature immunocompetent cells 5 B Cell development i Production, proliferation, differentiation in bone marrow ii Travel to lymphoid tissue and reside there as immunocompetent cells iii Each cell responds to only one specific antigen iv B-cell receptor, CDRs (variable region) v Central tolerance 1 Process in which B cells learn how to distinguish between self and non-self. 2 Any B cells that attack our own tissue are filtered out during the process of central tolerance ii Clonal Selection (Selection, proliferation, and differentiation of individual T and B cells with receptors for a specific antigen) 1 2 Steps: a Antigen processing and presentation i Initiated when T and B cells interact with an antigen ii Must first be processed and then presented by APCs (from innate immunity) iii Results 1 Differentiation of T cells into effector cells, such as T cytotoxic cells 2 Differentiation of B cells into active antibody- producing cells (plasma cells) iv Major Histocompatibility complex 1 Two Classes a Class I i Present endogenous antigens b Class II (usually involved in B cell Clonal Selection) i Present exogenous antigens 2 Present on the surface of all human cells (except RBCs) b Complex cellular interactions i Results in production of effector cells b 1 Plasma Cells 2 Th 3 Tc cells 4 Memory cells Cell-Mediated Immunity i Conversion of Immunocompetent T cells into Effector T cells (i.e. Cytotoxic T Cell) ii TCR is similar to an Fab iii Structure is similar to immunoglobulins 1 Also have variable region (gives ability to interact with multiple antigens) 2 TCR 3 MHC class I (cell mediated) or II (humoral) 4 Co-receptors iv CD3s are present on all T cells v T cells = MHC class I = CD8 vi Antigens must be processed in order for T cells to recognize them vii Sensitization for Killing by NK cells (Antibody Dependent Cellular Cytotoxicity) = anti-cancer antibody treatments 1 Similar to opsonization, falls under adaptive immunity because it involves antibodies 2 Antibody binds antigens on the surface of target cells 3 Fc receptors on NK cells recognize bound antibody 4 Crosslinking of Fc receptors signals the NK cell to kill the target cell 5 c Target cell dies by apoptosis Humoral Immunity i Differentiation of Immunocompetent B cells upon encounter with antigen into Plasma Cells (secrete antibodies) ii B Cell Clonal Selection 1 Antigen binds to B cell Receptor 2 Processed inside Cell 3 Presented on the surface by MHC Class II (always interacts with CD4) 4 Antigen interacts with CD4 on T helper cell 5 T helper cells a Have TCR b CD4 on cell surface interacts with antigen presented by MHC Class II c 6 Release cytokine signal (IL-4) B cell then differentiates into plasma cell that then secretes antibodies ix. Innate/Adaptive connection a Antigen-presenting cells i Dendritic Cells ii Macrophages x. Definition of an antigen xi. How do we recognize self/non-self xii. Seven aspects of innate immunity xiii. Types of adaptive immunity: humoral, cellular xiv. Components of an antibody xv. Types of antibodies/immunoglobulins, where they are primarily found and their function a Immunoglobulin (Ig) (more generic antibody) i Defined as the antigen binding molecules on B cells ii Antibodies = more specific antigen iii Produced by B cells iv Fab region = interacts with antigen v Fc region = constant region = where function comes from = attaches to B cell vi Light Chains and Heavy Chains vii CDRs = variable region = gives antibodies ability to interact with different antigens b Types of Ig i IgM = big = pentamer joined by J chain = 5 1 Stable in pentamer form 2 J chain joins 5 monomeric IgM together to form pentameric IgM ii IgA = largely in secretions and in gut = 2 1 Dimeric (secretory) especially IgA protects mucosal surfaces 2 Must be transported across epithelia (membrane) into mucosal lumen iii 3 Joined by J chain to form dimeric IgA 4 Secretory in nature a In breast milk b In GI tract IgG = most abundant = Passed down from Mom during pregnancy 1 IgG transferred from Mom to baby, acts as babies immune system a Baby will begin to create their new IgG once they grow older b 2 Will start making IgA around 1 year Fights most of our infections xvi. Role of major histocompatibility complex (MHC), what cell types a Involved in Antigen Processing and Presentation b Glycoproteins on the surface of all human cells (except RBCs) c Also called Human Leukocyte Antigens (HLAs) d Class I (always interacts with CD8) i e Present endogenous antigens Class 2 (always interacts with CD4) i Present exogenous antigens xvii. Types of T cells and their functions xviii. Opsonization a Overlap between Innate and Adaptive immunity b Antibodies form a layer around bacterium to help with engulfment process by macrophage 2. CLASS 5 a. Infection/Inflammation - some overlap with Class 4 i. First line of defense against infection 1. Physical Barriers i Skin ii Mucosa iii ii. How inflammation aids in protecting against infection iii. Shapes of bacteria 1. 2. 3. Spheres | Cocci i Diplococci ii Streptocci iii Tetrad iv Staphylococci v Sarcina Rods (Bacilli) i Chain of Bacilli ii Flagellate rods iii Spore-Former Spirals i Vibrios ii Spirilla iii Spirochaetes iv. Factors for Infection 1. Communicability: ability to spread from one individual to others and cause disease 2. Infectivity: ability of pathogen to invade and multiply in the host 3. Virulence: capacity of a pathogen to cause severe disease i Measles: Low ii Rabies: High 4. Pathogenicity: Ability of an agent to produce disease (what kind of damage it can do) i True pathogens have devised means to circumvent normal immune responses 5. Port of entry: route by which a pathogenic microorganism infects the host 6. Toxigenicity: ability to produce soluble toxins or endotoxins i v. Goes hand in hand with virulence Causes of infection – know each type 1. Viruses i Most common affliction of humans ii Need permissive host cell iii Steps in Viral Reproduction 1 Attachment 2 Penetration 3 Uncoating 4 Replication 5 Assembly 6 Release 2. Bacteria i Prokaryotes: lack discrete nucleus ii Classified by 1 O2 metabolism a Aerobic b Anaerobic 2 Motility 3 Shape 4 Staining a Gram Positive i Very thick Peptidoglycan outer layer ii Absence of outer membrane layer iii E. Coli b Gram Negative i Thinner peptidoglycan layer ii Have outer membrane layer iii Diagnosed by culture & Sensitivity 1 Antibiotic susceptibility: figure out what kind of medication iv Bacteremia (presence) or septicemia (growth) 1 A result of a failure of the body’s defense mechanisms 2 Septicemia – Usually caused by gram-negative bacteria, release endotoxins in the blood 3 Toxins released in the blood a Release of vasoactive peptides and proinflammatory cytokines b Produce widespread vasodilation, increased capillary permeability i Can lead to hypertension, and further -> shock c Activate clotting cascades i Can lead to Disseminated Intravascular Coagulation (DIC) 1 Leads to sepsis d Leading to septic (endotoxic) shock 3. Fungi i Characteristics 1 Large eukaryotic microorganisms 2 thick, rigid cell walls without peptidoglycan a Walls made up of polysaccharides b Need different medications than bacteria 3 Single celled = yeasts 4 Multi-celled = mold (filaments or hyphae) 5 Both = dimorphic 6 Reproduce by simple division or budding ii Fungal Infection 1 Mycoses: diseases caused by fungi a Superficial, deep, or opportunistic 2 Dermatophytes: fungi that invade the skin, hair or nails a Diseases they produce are called tineas (ringworm) i Tinea capitis, tinea pedis, and tinea cruris 3 Pathogenicity a Adapt to host environment b Suppress the immune defenses c Usually controlled by phagocytes, T lymphocytes 4 Candida albicans a Most common cause of fungal infections b Opportunistic c Found in normal microbiome of skin, GI tract, vagina of many individuals d Localized infection if overgrowth occurs e Disseminated infection if immunocompromised i Common in cancer patients 4. Parasitic Infection i Characteristics 1 Symbiotic (parasitic) 2 Unicellular protozoa to large worms (helminths) 3 Protozoa include malaria, amoebae, flagellates 4 More common in developing countries 5 Spread human to human via vectors 6 Usually ingested 7 Tissue damage vi. Steps in Phagocytosis vii. How bacteria evade our immune system/develop antibiotic resistance 1. Evasion techniques i Coating to evade phagocytes ii Degrade complement and IgA 1 These are important for our immunity 2 Some proteases (enzymes that break down proteins) degrade these immunoglobulins iii Toxins 1 Ability to nullify effects of chemotaxis from chemokines iv Molecular mimicry 1 Proteases from pathogens can mimic immunoglobulin parts 2 v Can lead to hypersensitivity reactions Antibiotic resistance 1 Multi-drug Resistant Staph Aureus (MRSA) example of antibiotic resistance 2 vi Gotta stay one step ahead of the pathogens Biofilm 1 Microorganisms exist as a complex of biofilms, gives survival advantage to bacteria vii Change antigens 1 Antigenic Drift a More gradual mutations of surface antigens 2 Antigenic Shift a Major shifts in genetic recombination, usually in species jumping viii. Antimicrobial/Antibacterial Drugs 1. Principles of antibiotic use i Narrow-spectrum 1 More specific to category of bacteria (i.e. gramnegative cocci, bacillus) 2 Active against very few species of organisms 3 Typically want to use narrow-spectrum ii Broad-spectrum 1 May start at offset with broad spectrum, then with more cultures/labs can fine-tune antimicrobial therapy, move to narrow specturm iii Bactericidial = kill iv Bacteriostatic = suppress v Host defenses are essential to the success of antibiotic therapy vi Patient Education: 1 Patients should complete entire course to get rid of the infection 2 Failure – promotes resistance 3 Drug reactions/allergies vii Combinations of Antibiotics are appropriate 1 Treatment of severe infections 2 Infection > 1 organism 3 Tuberculosis treatment 4 Combination of bactericidal effects viii Indications for Antibiotics prophylaxis 1 Certain surgeries (dental) 2 Neutropenia (immunosuppressed) 3 Recurrent UTI 4 Risk of bacterial endocarditis ix Antibiotics misuses 1 Treatment of viral infections 2 Treatment of Fever of Unknown Origin (FUO) if not immunocompromised 3 Treatment w/o information on bacteria 4 Treatment in the absence of drains/removal of debris 2. Desirable traits of an antibiotic i Selective Toxicity 1 Ability to injure the pathogen without harming healthy cells 2 Our cells are different than the pathogens so drugs are tailored to take advantage of these differences: a Bacterial cell wall (structure/protoplasm) inhibition i Penicillin’s, cephalosporins, bacitracin, vancomycin b Bacterial protein synthesis (ribosomes) inhibition i Chloramphenicol, erythromycin, tetracyclines, streptomycin c Bacterial DNA/RNA (nucleic acid/enzymes) inhibition i Quinolones, rifampin d Bacterial enzymes (folic acid synthesis) inhibition i Sulfanilamide, trimethoprim 3. Know how antibiotics work 4. Bactericidal versus bacteriostatic 5. Major adverse side effects of all antibiotics (penicillin, fluoroquinolones, macrolides) i Pencillin 1 Allergic reactions 2 Hyperkalemia ii Fluoroquinolones 1 Tendon Rupture 2 Phototoxicity iii Macrolides 1 GI effects 2 Prolonged QT duration – sudden cardiac death 6. Classes of antibiotics i Bacterial Cell Wall Inhibition 1 Penicillins (PCNs) a Therapeutic Uses i Primarily Gram (+); broad and narrow spectrum b Contraindications i Caution with Renal dysfunction 1 Increased PCN blood levels ii Severe PCN allergy 1 Wear Medic Alert c Adverse effects i Allergy ii Electrolyte imbalances (IV) 1 Hyperkalemia – cardiac 2 Due to mixture of potassium penicillin, potassium comes with it 2 Cephalosporins (Ceph) a Therapeutic Uses i Primarily Gram (+), multiple generations b Contraindications c i Severe PCN allergy ii Do not drink alcohol with Adverse effects i Bleeding 1 Monitor; use caution with pts on anticoagulants 2 Interferes with prothrombin levels by interfering with Vit K ii ii Thrombophlebitis Bacterial Protein Synthesis: Bacteriostatic 1 Tetracyclines a Therapeutic Uses: i Acne ii Gum disease (periodontal disease) b Contraindications c i Pregnant women ii Children under 8 Adverse effects i Hepatotoxicity ii Nephrotoxicity iii Photosensitivity iv Discolor teeth v GI irritation vi Suprainfection 1 C. diff diarrhea 2 Macrolides a Therapeutic Uses i Substitute in PCN allergy b Contraindications i Avoid admin with CYP3A4 inhibitors (increase risk of QT) 1 CYP3A4 are important in med clearance c Adverse effects i GI effects ii QT prolongation – sudden cardiac death iii Bacterial Protein Synthesis: Bactericidal 1 Aminoglycosides a Therapeutic uses i Narrow spectrum; serious infections; aerobic gram (-) bacilli b Contraindications i Pencillin (inactivates), do not administer together c Adverse effects i Nephrotoxicity ii Ototoxicity (transient hearing loss) iii Neuromuscular blockade = respiratory depression iv Bacterial Metabolites Inhibition (folic acid) 1 Sulfanomides & Trimethoprim – Bacterostatic a Therapeutic Uses i UTIs ii Combination TMP/SMZ more powerful b Contraindicaitons i Pregnant women, nursing mothers, infants under 2 months 1 Bilirubin build up in brain c Adverse effects i Hypersensitivity (StevensJohnson syndrome) ii Photosensitivity iii Hematologic-hemolytic anemias iv Renal (crystalluria) 1 Drink plenty of water v Bacterial DNA/RNA inhibition 1 Fluroquinolones (Cipro) a Therapeutic uses i Broad-spectrum’ wide variety b Contraindications i IV avoided in children due to risk of tendon rupture c Adverse effects i Risk for tendon rupture ii Phototoxicity iii Absorption can be reduced by cationic solutions 1 Milk, antacids, etc 7. Classes of anti-fungals i Polyene antibiotics 1 Amphotericin B a Broad Spectrum antifungal agent b Highly toxic i Infusion reaction and renal damage occur in many patients ii c Given IV, no oral administration Uses: i Drug of choice for most systemic mycoses ii Before amphotericin B, systemic fungal infections were usually fatal d Adverse effects i Infusion reaction 1 Fever, chills, rigors, nausea, and headache 2 Pro-inflammatory cytokines 3 Symptoms begin 1-3 hrs after start of infusion ii Nephrotoxicity iii Hypokalemia 1 Affects pores of renal tubule collecting duct leading to leakage of potassium and loss iv Bone marrow suppression ii Azoles 1 Example: Fluconazole [Diflucan] 2 Characteristics a Broad Spectrum antifungal drugs b Alternative to amphotericin B for most systemic mycoses c Lower toxicity d Can be given orally e Disadvantage i Inhibit P450 drug-metabolizing enzymes and can increase levels of many other drugs iii Echinocandins iv Pyrimidine analogs 8. Vaccines i Preparation Types 1 Attenuated 2 Killed a Typhoid b Uses killed bacteria for delivery 3 Toxoid a Diphteria, tetanus b Antigenicity is preserved, but no longer toxic 4 Subunits a Pertussis, HepB, Pneumococcoal b Attach to carrier proteins 5 Nucleic Acid ii Features of effective vaccines 1 Safe 2 Protective 3 Gives sustained protection 4 Induces neutralizing antibody 5 Induces protective T cells 6 Practical Considerations b. Stress and disease i. What triggers a stress response and signs and symptoms 1. Stress is triggered by a perceived or anticipated threat that disrupts a person’s homeostasis i May stem from 1 Psychological/emotional (fear, social rejection) 2 Physical (dramatic temp changes, abuse) 3 Physiologic (infection, inflammation) stimuli 2. Stress affects the immune system i Stress directly related to proinflammatory cytokines ii Link between stress, immune function, and disease/cancer iii Immune system affected by neuroendocrine factors iv Stress response decreases T-cell cytotoxicity and Bcell function v 3. Signs and Symptoms of Stress, precipitating factor for some diseases and may worsen conditions ii. i Ulcers ii Asthma iii Anxiety iv Depression v Diabetes How the Sympathetic Nervous System (SNS) responds to stress 1. General Adaptation Syndrome i Alarm Stage 1 Stressor triggers the hypothalamic-pituitaryadrenal (HPA) axis a Activates sympathetic nervous system 2 Arousal of Body defenses 3 Steps 4 a b Brain i ACTH ii Nerve Signal Adrenal Gland Releases i Cortex 1 Glucocorticoids (cortisol) a Liver releases glucose ii Medulla 1 Adrenaline (epinephrine) a Increased heart rate, breathing rate, blood sugar 2. Resistance/adaptation stage i Begins with the actions of adrenal hormones ii Mobilization contributes to fight or flight 3. Exhaustion stage (allostatic overload) i Occurs only if stress continues and adaptation is not successful ii Leads to stress-related disorders iii Allostasis 1 “Stability through change” 2 Brain continuously monitors for future events and anticipates what is required from neuroendocrine and autonomic systems 3 Allostatic Overload a Overactivation of adaptive systems b Highly individualized iii. Catecholamines (Neuroendocrine regulation) 1. Released from chromaffin cells of the adrenal medulla i Epinephrine released binds to adrenergic receptors 2. α-adrenergic receptors i α1 and α2 3. β-adrenergic receptors i β1 and β2 4. Mimic direct sympathetic stimulation iv. What are the effects of epinephrine 1. Increased heart rate, breathing rate, blood sugar 2. Stimulates both alpha and beta adrenergic receptors 3. Greatest influence on cardiac action i Increased heart rate – B1 ii Increased force cardiac contraction: B1 4. Epinephrine also has metabolic effects i Increased hepatic gluconeogenesis: B2 ii Increased hepatic and muscle glycogenolysis: B2 iii Increased Glucagon and renin: B1 5. Pulmonary effects of epinephrine i Smooth muscle relaxation of bronchial smooth muscles – cause bronchodilation: B2 v. Adrenergic receptors 1. What they are (alpha 1 and 2, beta 1 and 2) 2. What are the primary responses of each 3. How that relates to the stress response and clinical manifestations (ex. If beta 1 is stimulated/blocked…you will see x clinical response) 4. Alpha-adrenergic receptors i Alpha 1 1 Blood Vessels: Increased Vasoconstriction 2 Heart: Increased Contractility ii Alpha 2 1 Neurons: Inhibition 5. Beta-adrenergic receptors i Beta 1 1 Heart: Increased HR, conduction, contractility ii Beta 2 1 Lung: Bronchodilation 2 GI: decreased motility vi. Hypothalamic-Pituitary-Adrenal (HPA) axis 1. Hypothalamus secretes corticotropin-releasing hormone (CRH) 2. Pituitary releases adrenocorticotropic hormone (ACTH) 3. Adrenals secrete cortisol and catecholamines i Cortisol 1 Secreted during stress 2 Reaches all tissues 3 Stimulates gluconeogenesis 4 Elevates the blood glucose level 5 Affects protein metabolism 6 Powerful anti-inflammatory and immunosuppressive agent 7 Effects: a Used therapeutically as power antiinflammatory/immunosuppressive agents b Influence virtually all immune cells c Elevated Levels may decrease innate immunity and increase autoimmune responses 4. Stress triggers the HPA axis c. Immunodeficiencies i. Know the dangers for patients with immune deficiencies 1. Major Concepts a. Main symptoms is recurring infections b. Types of infections indicate immune defect c. Family history is important for diagnosis d. Failure to thrive 1 Lack of adequate nutrition e. The type of infection that the patient has is often the first clue that something is wrong with the immune system ii. Types of Immune Deficiencies (examples of disease diagnoses and clinical Manifestations) iii. Primary vs Secondary 1. Primary (congenital) a. Genetic anomaly b. Disease in which ther is a failure of immunological functions as a result of defects in genes for components of the immune system c. Inherited – not acquired d. Primary Immune defects are can involve one defective gene 1 XLA a 2 SCID a 3 Aire gene IPEX a 5 Rag, y common chain gene APECED a 4 BTK gene FoxP3 gene Bare Lymphocyte Syndrome a MHC gene 2. Secondary (acquired) a. Caused by another illness b. More common c. Unlike primary, these are not diseases that we are born with and cannot be genetically passed on to our offspring iv. HIV causes AID 1. Pathophysiology a. The cells involved and their roles 1 Affects CD4+ cells a HIV’s Gp120 binds to CD4 cells b. Pathogenesis 1 Retrovirus a Genetic info is in the form of RNA b Contains reverse transcriptase to convert RNA into double stranded DNA c HIV Integrase i Inserts new DNA into the affected cell d Protease i Necessary for processing and assembling virions c. The HIV enzymes required for viral replication and how they work d. “Acute phase” and what it means in HIV, symptoms e. “Clinical latency” and what it means in HIV, symptoms 2. Clinical Manifestations a. Serologically negative, serologically positive but asymptomatic, early stages of HIV, or AIDS b. Window Period c. Th cells <200 cells/mm3 diagnostic for AIDS d. Diagnosis of AIDS is made in association with various clinical conditions 1 Atypical or opportunistic infections and cancer 2 Presence of antibodies against HIV 3 Western Blot analysis 3. The clinical presentation of HIV – differentiate the 3 phases a. Viral loads and CD4 counts in each phase in general (not specific numbers) 4. What CD4 count is indicative of HIV progression to AIDS (the number in cells/ml) <200 cells/mm3 5. Pharmacological HIV Treatment a. Define/describe mechanism of action of antiretroviral therapy (ART; HAART) 1 Antiretroviral Therapy (ART) combination of the following a Reverse transcriptase inhibitors b Protease inhibitors c Integrase Inhibitors d Fusion inhibitors e CCR5 antagonist 2 HAART – Combination therapy a Most patients take around 30-45 pills a day b Cost is astronomical b. Antibiotics/antifungals given prophylactically c. Define protease enzyme 1 6. Laboratory Monitoring for HIV Infection and Efficacy of Drug Therapy 7. Whats the overall treatment goal, CD4 T-cell counts 3. CLASS 6 a. Wound Healing i. Types of healing (first intention, second intention, etc.) a Primary Intention i Wounds that heal under conditions of minimal tissue loss b Secondary intention i Wounds that require a great deal more tissue replacement 1 Examples a open wound b Myocardial infarction replaced with fibrous tissue c Regeneration = replacement of damaged tissue with healthy tissue i Resolution = ii Return to original structure and function d Repair i Replacement of destroyed tissue with scar tissue 1 Composed primarily of collagen to restore the strength of the tissue but not its function e Healing Processes i Filing in the wound ii Sealing the wound (epithelialization) iii Shrinking the wound (contraction) ii. Phases of Wound Healing (overlapping) a Phase I: Inflammation i ii iii Coagulation 1 Immediate 2 Short and quick Infiltration of wound-healing cells 1 Platelets 2 Neutrophils 3 macrophages Angiogenesis 1 Forming of capillaries to provide area with needed blood flow b Phase 2: Proliferative and new tissue formation i Granulation 1 Healthy tissue that surrounds and grows into the wound ii Epithelization (Keratinocyte Migration) 1 iii Occurs under the scab Requires fibroblast proliferation, collagen formation, wound contraction (myofibroblasts: important for closing up the wound) 1 Connective protein proliferations c Phase 3: Remodeling and maturation phase i Continuation of cellular differentiation 1 End of angiogenesis ii Scar Tissue formation iii Scar remodeling iii. Dysfunctional Wound healing a May occur during any phase of wound healing i Ischemia ii Excessive bleeding iii Excessive fibrin deposition iv Predisposing disorders 1 Diabetes 2 Obesity a Elevated levels of proinflammatory cytokines affecting leukocytes 3 Wound infection 4 Inadequate nutrients 5 Numerous drugs a 6 b NSAIDs Tobacco Smoke Dysfunction during reconstructive phase i Dysfunctional collagen synthesis, resulting in 1 Keloid scar a Raised, but extend beyond boundary of affected tissue b 2 Do not regress Hypertrophic scar a Contained within the site of injury and may regress over time ii Wound disruption 1 Dehiscence (increases risk of infection) a Wound pulls apart at a suture line b Obesity major risk factor c Calls for immediate attention due to high risk for infection iii Contracture 1 Usually at joint sites 2 Term for meaning a decrease in passive range of motion at a joint iv. Terms: Dehiscence, keloid, etc. ] b. Hypersensitivities i. Types of hypersensitivity reactions (I-IV) 1. Definition and generally how hypersensitivity reactions work i Diseases caused by an exaggerated immune response ii Could be response against a pathogen, nonpathogen or self iii 4 Types of Hypersensitivity Reactions 1 Type 1 (IgE) = seasonal allergies = mast cell activation a IgE-mediated allergic reactions i Systemic anaphylaxis ii Acute urticaria iii Seasonal rhinoconjunctivitis iv Asthma v Food Allergy b Effector mechanism = Mast-Cell activation c Ige attaches to Mast cells i Mast cell is now sensitized ii Once enough IgE attaches to mast cell, degranulation occurs 1 Release of histamines (allergic reactions) 2 Type 2 (IgG) = some drug allergies (penicillin) a Cell- or matrix- associated antigen with cell-surface receptor b Effector mechanism = complement, FcR+ cells (phagocytes, NK cells) i c Antibody alters signaling Mediated by IgG d Specific cell or tissue (tissue-specific antigens) is the target of an immune response e Occur when antibodies react to altered components of self f NOT a soluble antigen g Five mechanisms: i Cell is destroyed by antibodies and complement ii Cell destruction through phagocytosis iii Soluble antigen may enter the circulation and deposit on tissues; tissues destroyed by complement and neutrophil granules iv Antibody-depended cell-mediated cytotoxicity (ADCC) v Target cell malfunction (e.g., Graves – targets thyroid) 3 Type 3 (IgG) a Immune complex mediated b Antigen-antibody complexes are formed in the circulation first and are later deposited in vessel walls or extravascular tissues i Large release of lysosomal enzymes c Not organ specific d Serum sickness i Raynaud phenomena e Arthus reaction 4 Type 4 (does not involve any antibodies, cellmediated, cytotoxic T cells) a Cell mediated hypersensitivity reactions b Does not involve antibody c Cytotoxic T lymphocytes or lymphokineproducing Th1 and Th17 cells i Direct killing by Tc or recruitment of phagocytic cells by Th1 and Th17 cells d Examples: i Graft rejection ii Tuberculosis skin test iii Allergic reactions from poison ivy or metals iv Celiac 2. Apply these principles to organ rejection, GVHD, hemolytic anemias ii. Know Allergy/Anaphylactic Reactions, principle cells, Ab, clinical signs/symptoms and processes involved in allergic reactions c. Autoimmunity i. Know examples discussed in class of autoimmune disorders a b Organ Specific i Goodpasture’s syndrome ii Type 1 diabetes mellitus iii Multiple sclerosis iv Graves’ disease v Vitiligo vi Bullous pemphigoid Systemic: (throughout the body) i Polymyositis: “Many muscle inflammation” 1 Inflammation of a group of muscles, or muscles in general ii. Understand the pathophysiology of autoimmune disorders a Causes i Environment 1 Pathogens, drugs, toxins, and hormones are just a few ways that the environment can trigger autoimmunity ii Genes and Autoimmunity 1 The concept that a single gene mutation leads to a single autoimmune disease is the EXCEPTION not the rule 2 Because of this, autoimmune diseases are generally classified as COMPLEX diseases as there is not a single “pinpoint-able” gene b Immune Regulation i A defect in any arm of the immune system can trigger autoimmunity a Innate immunity (Neutrophils Complement) 2 Acquired Immunity a Cell-Mediated Immunity (T Cells) i Multiple Sclerosis (Brain and Spinal Cord demyelination) 1 T cells (predominantly) attack the myelin sheath surrounding the axons of our nerve cells 2 MS patients can have autoantibodies and/or selfreactive T cells which are responsible for the demyelination b Humoral Immunity (B Cells) i Myasthenia Gravis 1 Disease marked by progressive weakness and loss muscle control 2 Classified as “B Cell” disease 3 Autoantibodies against nicotinic acetylcholine receptors c Symptoms i Initial diagnosis may be missed in patients as diseases present with general symptoms 1 Fever, muscle ache, fatigue, joint pain, changes in weight ii However, disease specific symptoms are often the first sign of autoimmune illness d 1 Dry mouth, dry eyes – Sjogren’s 2 Changes in metabolism – Grave’s Diagnosis i General tests 1 Low RBC count (anemia) 2 C reactive protein 3 Autoantibody titers (anti DNA, anti phospholipids, etc) very telling if autoimmune 4 ii e Presence of Rheumatoid factor Disease specific tests 1 Neurologic exam – MS 2 Fasting glucose – Diabetes 3 TSH levels – Graves Treatment i The key to treating autoimmunity is immunomodulation iii. Alloimmunity (immune response to nonself antigens from a member of the same species) a Transfusion reactions i ABO Blood group 1 A and B carbohydrate antigens 2 Can be simultaneously expressed a Blood types passed on which erythrocytes expressed b i A ii B iii O (neither expressed) iv AB (both expressed) Example i Person with blood type A receives type AB or B blood, transfused erythrocytes destroyed 1 Type A people will have A antigens on their erythrocytes and Anti-B antibodies in their serum 2 Type O – universal donor (no antigens on their erythrocytes) ii Type AB – universal recipient (no antibodies in their serum) ii Rh blood group (antigen D) 1 Antigens expressed only on RBCs 2 Rh-positive a If baby is rh-positive (d positive), 3 Rh-negative 4 Hemolytic disease of newborn iv. Know blood types, universal donor/recipient v. Be able to apply this knowledge to what occurs in blood transfusions d. Drugs i. Antiviral Therapy/Drugs – for HIV and other diseases a Characteristics i Our ability to treat viral infections remains limited ii Viruses use biochemical machinery of host cells to reproduce iii Difficult to suppress viral replication without doing significant harm to the host iv Antivirals suppress biochemical processes unique to viral reproduction b Herpes i Acyclovir (Zovirax) 1 Active only against members of the herpesvirus family 2 Agent of first choice for herpes simplex virus (hsv) or varicella-zoster virus infection 3 ii Herpesvirus develops resistance to acyclovir Cytomegalovirus Infection 1 CMV: member of the herpesvirus group 2 Transmitted by direct contact with body fluids 3 50% to 80^ of Americans age 40 years or older harbor the virus 4 Can remain dormant for life 5 Immunosuppressed patients at high risk for reactivation of dormant virus iii Ganciclovir [Cytovene, Vitrasert, Zirgan] 1 Synthetic antiviral agent 2 Uses a Herpes simplex virus, including CMV b Prevnetion and treatment of CMV infection in immunocompromised patients, including transplant patients, those with HIV infection, and those receiving immunosuppressive drugs 3 c Serious side effects a Granulocytopenia b Thrombocytopenia Hepatitis i Viral hepatitis is the most common liver disorder ii Millions of Americans are infected iii Six different viruses can cause acute hepatitis (A,B,C,D,E, and G) iv Only B, C, and D can cause chronic hepatitis (B, C account for 90%) v Hep C Virus (HCV) 1 Differences in HCV: 6 genotypes 2 Transmission: primarily through exchange of blood; sexual transmission (rare) 3 Even with no symptoms, can be transmitted 4 Slow progression can lead to liver failure, cancer, and death 5 Leading reason for liver transplantation 6 Drugs a Pegylated interferon alfa combined with ribavirin b vi Pegylated helps maintain drug in body Interferon Alfa (drug use to treat) 1 Interferon family a Alpha, beta, gamma b Alpha used to treat hepatitis c None can be administered orally 2 Conventional versus long-acting interferons 3 Adverse effects a Flu-like symptoms b Neuropsychiatric effects, especially depression c Fatigue, thyroid dysfunction, heart damage, and bone marrow suppression, manifesting as neutropenia and thrombocytopenia vii Hep B 1 1.4 million people have chronic hep B 2 11,000 require hospitalization for deep fatigue, muscle pain, and jaundice 3 Chronic infection develops in 3%-5% of infected adults 4 Chronic infection can lead to cirrhosis, hepatic failure, hepatocellular carcinoma, and death 5 Transmission via blood and semen 6 HBV vaccine and drugs: a d Interferon alpha 2beta, Lamivudine Influenza i Characteristics 1 Serious respiratory tract infection 2 Major cause of morbidity and mortality worldwide 3 Caused by influenza viruses, which are highly variable and undergo constant evolution ii a Type A (more infectious) b Type B Management 1 Influenza managed by vaccination (primary strategy) and drugs 2 Drugs a Adamantanes and neuraminidase inhibitors 3 Vaccines a Influenza vaccines change yearly based on identification of strains by CDC, FDA, WHO iii Drugs for Influenza 1 Neuraminidase inhibitors a Oseltamivir (Tamiflu) b Zanamivir [Relenza] c Block the function of the viral neuraminidase protein e HIV i Characteristics 1 HIV is a retrovirus (HIV1 and 2) 2 HIV has RNA as genetic material 3 Uses reverse transcriptase to convert RNA into DNA and integrase to insert its DNA into ours 4 Target cells: CD4 T cells (helper lymphocytes) 5 Transmission via blood and body fluids (virus is present in all body fluids) ii Classification of Antiretroviral Drugs 1 5 Types of antiretroviral drugs a Inhibit enzymes required for HIV i Reverse transcriptase inhibitors 1 Blocks reverse transcriptase 2 Nucleoside Reverse Transcriptase Inhibitors (NRTIs) a Zidovudine [Retrovir] i Inhibits HIV replication by suppressing synthesis of viral DNA b Adverse effects i Hematologic toxicity ii Lactic acidosis with hepatomegal y iii Myopathy iv Gastrointesti nal effects v Central nervous system (CNS) reactions vi Others c Drug Interactions d Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs) i Efavirenz [Sustiva] ii Preferred agent for treating HIV iii Only NNRTI recommende d for first-line therapy of HIV infection iv Drug interactions v Adverse effects vi Transient adverse CNS effects in 50% of patients vii Rash viii Teratogenicit y ii Integrase strand transfer inhibitors 1 Blocks integration into DNA iii Protease inhibitors (similar to neuraminidase inhibitors) 1 Proteases are important for release of virus to other cells b Block viral entry into cells i Fusion inhibitors ii CCR5 antagonists 1 Blocks attachment point for virus iii ii. Antihistamine Drugs iii. Treatment of anaphylactic reactions iv. Know which drugs are used based upon severity of reaction v. Know the clinical presentation of overdose of antihistamines, anticholinergic syndrome vi. Glucocorticoid therapy 1. Mechanism of action and considerations for safe use vii. Anti-inflammatory, 1. Know mechanisms of action of NSAIDs and ASA viii. NSAIDs, ASA 1. Clinical effects of COX-1 and COX-2 inhibition 2. Clinical indications/uses and precautions related to NSAIDs 3. Adverse side effects 4. Effects on platelet aggregation 5. Drug-Food interactions COMPREHENSIVE CONTENT CLASS 1: CELL, GENETICS, & INTRO TO PHARMACOLOGY 1. Altered cell biology a. Types of cell & tissue alterations and injuries (hyperplasia, metaplasia, dysplasia, hypertrophy, atrophy, etc.) 2. Genetics i. Heterozygous vs. homozygous 3. Intro. to Pharmacology a. Basic definitions/principles of absorption, metabolism, distribution and excretion and how aging affects these i. How drug route affects these concepts ii. Principles associated with: 1. lipid solubility, water solubility, polar, b. Routes of administration – enteral versus parenteral and first pass effect c. Principles of safe medication administration and education about medication - nursing responsibilities CLASS 2: FLUID & ELECTROLYTES – ACID-BASE IMBALANCES • Fluid and Electrolytes o Hyper/Hypotonic fluid imbalances, causes, and associated ICF/ECF fluid shifts o Edema – what leads to edema Oncotic/osmotic/capillary hydrostatic pressures o Types of electrolyte imbalances (Sodium, Potassium, Chloride) • Causes Acid-base o Know pH range (know actual values) o Metabolic Acidosis and Alkalosis and Respiratory Acidosis and Alkalosis Causes Associated ABC changes - Know trends (ex. If PCO2 is increased and HCO3 is decreased this means…) o Interpretation of Blood Gas results Know normal values (pH, HCO3, PaCO2, PaO2) CLASS 3: RENAL 1. Renal Alterations a. Definitions related to urine and urine output (anuria, oliguria, dysuria, polyuria, hematuria, pyuria, bacteruria, etc.) b. Nephrotic vs. Nephritic syndrome c. Common causes and symptoms of: i. Cystitis, Acute Pyelonephritis ii. Renal calculi (most common type) d. Acute Kidney injury (AKI) i. Mechanisms/causes of (Prerenal, Intrarenal, Postrenal) e. Definitions and Clinical Manifestations of: i. Nephrolithiasis 2. Diuretics a. Indications for use i. General mechanism/site of action for each class of diuretics: loop, thiazide, K+ sparing, osmotics