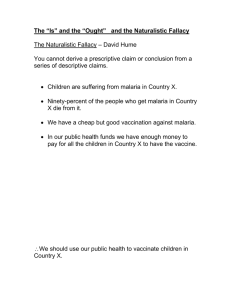
Malaria: Life Cycle, Pathophysiology, Diagnosis & Treatment
advertisement

Malaria: It is the commonest parasitic infection Live cycle:sporozites occur in the salivary glands of mosquitoafter a mosquito takes a blood meal these sporozites injected in the blood and go to the liver then emerge in the bloodstream as merozoites these merozoites enter RBCsthen RBCs ruptured and give gametocytesthese gametocytes are taken by mosquito in a blood meal then go to the salivary glands of mosquito and change into sporozites. The whole pathology occurs within the RBCs. Pathophysiology:-the whole pathophysiology takes place within the RBCs. -When the malaria parasite enter the RBCs:1. It reacts with HB & the component of RBCs & releases cytokines which produces TNF which is responsible of fever… (Cytokines also increases the capillary permeability). 2. It lead to release of cytoadherent which change the RBCs into knobs. ))تبقى زي الصمغ وتلصق مع بعض Cytoadherent attack the normal and abnormal RBCsclump together. 3. Rouset formation: It's due to clumping of infected RBCs (RBCs gather and make lines) these RBCs can obstruct blood vessels. This rouset formation is responsible for cerebral malaria & pulmonary edema (also may be due to increased capillary permeability caused by cytokines). Presentation:A. Muscles:Myalgia (muscle pain) malaria parasite causes damage of the muscles lead to release of CDK (creatinine phosphokinase) lead to myalgia. B. Lungs:Pulmonary edema edema due to increased capillary permeability. C. Kidney:Renal failure malaria lead to tubular necrosis & damage the glomeruli (so malaria doesn’t cause HTN) D. GIT:(Can cause everything in GIT) 1. Abdominal pain. 2. Vomiting & diarrhea. 3. Malabsorption. 4. Hypoglycemia Prevent sugar absorption Stimulate pancreas to release insulin E. Brain: Brain edema Cerebral malaria "unknown mechanism" F. Orthostatic hypertension:Pt can't maintain his normal bp when standing up which lead to dizziness & syncope. G. Severe metabolic acidosis:lactic acidosis. 1. 2. 3. 4. *Laboratory indicators of severity of malaria (indicate poor\bad prognosis): Low blood sugar Increased cpk Lactic acidosis Low HB Diagnosis:1. Blood film:-by seeing Trophozoites inside the RBCs (ring stage)blue Chromatinpink -it’s the definitive diagnostic tools -Advantages of BF: Cheap. Tell you about response to treatment. Tell about the degree of parasitaemia. -Disadvantages of BF: The minimal number of …. That should be seen to diagnose malaria is 200 ……. need honest technician . 1 cross (+) in BF = in every 100 film10 parasites 2 crosses (++) you see from 10-100 parasites BF also show you the type parasite:-P.falciparum 90% of cases -P.vivax10-12% of cases -P.malariaenone in Sudan -P.ovale none 2. ICT Rapid test . Tell you if there is malaria or not but doesn’t tell the degree of parasitemia. Contain antibodies for Vivax & Falciparum tells you which one is positive but doesn’t tell the degree of parasitemia. Malaria is divided clinically into:1. Simple malaria 2. Complicated malaria Simple malaria:Its characterized by:1. Fever : the most important feature & sometimes simple malaria is called malaria fever. 2. Headache. 3. Convulsion (febrile convulsion). 4. Malaise. 5. Aches & pain. 6. Diarrhea & vomiting. 7. Coughs. Complicated malaria: Severe complicated malaria is a medical emergency, and if the patient not treated properly ,the patient will die in few hours. Criteria of complicated malaria :1. Cerebral malaria Repeated convulsion & coma. 2. Hyperpyrexia :temp>41 3. Hypoglycemia It’s a serious complication It's more common in children & pregnant women 4. Pulmonary edema . 5. Renal failure. 6. Hypotension. Can't be treated unless you treat malaria doesn’t respond to fluids & if you give the patient large amount if fluidsincreased risk of fluid overload P.edema. 7. Acidosis. 8. Severe anemia Sudden & very low HB. 9. DIC 10. Jaundice (more in adult). 11. Hyperparasitemia …………………………………………………. If you find one or more this is complicated malaria. The commonest presentation of complicated malaria 1. Cerebral malaria (coma). 2. Anemia HF. 3. Hypoglycemia 4. Hyperpyrexia associated with hyperparasitemia. Investigation for complicated malaria: 1. CBC for anemia 2. Urea & electrolytes for RF 3. Chest X-ray for pulmonary edema to exclude severe pneumonia :because its DD for malaria 4. RBG for hypoglycemia 5. ABG for acidosis 6. Urine general 7. Lumbar puncture if you suspect meningitis as DD for convulsion and fever. Treatment of malaria:1. First you have to diagnose malaria 2. Classify it simple or complicated(both are dangerous because simple malaria can change to complicated within few hours) 3. Give medication according to the national protocol: first line: coartem second line: DHAP third line: quinine\artesunate (iv\im) *Coartem= artemether + lumefantrine *DHAP= dihydroartemesinin+piperaquine For simple malaria start with the first linecoartem If no response give DHAP Also yet no response give quinine or artesunate For complicated start with the third line: either quinine or artesunate iv\im Coartem 6doses Given at……….,then after 8 hours then after 12 hours Artesunate : فتايل3 يجي في شكل Powder, NaHCO3, NS powder has 3 concentrations: 30, 60,120mg )ازرق,اصفر,)اخضر Dose Weight ≤20kg3mg\kg Weight>20kg2.4mg\kg How do you give it? 1. You dissolve the powder in NaHCO3 (pour NaHCO3 in the powder till it become crystal clear & don’t start with NS because powder doesn’t dissolve in it) 2. Then add NS this dose should be given within 30 minutes ,because after 30 minute it becomes unstable. give it IV (preferred) but you can give it IM (we don’t prefer im ) SE: no SE unless you give a large dose (eg.80\kg)this causes severe hemolysis. how many doses? 3doses When do you give it? At….time then after 12 hours & then after 24 hours if you come after 24 hours & you find the pt has improved clinically (no symptoms) &laboratory (-ve BF) you have to give him coartem before discharge (take the pills home) if you come after 24 hours & you find that the pt is febrile & not improved , what shall you do? Give him another dose of artesunate , yet not improved give another dose till you reach 7 doses & don’t give more than 7 doses. (Dx may be wrong ). (max is 7 doses). Quinine:You can give quinine but recommended is artesunate iv dose : 10mg\kg\dose Dissolve it in D5% 1mg in 1ml of d5% to avoid hypoglycemia (e.g.mg200in200ml) Give it slowly within 3hours 3doses\day: every 8hours. you can give quinine im (deep im 60 mg in 1ml NS or d5%) Duration of Rx: 3doses \day usually for 48 hours (pt usually improve after 48 hours ,no symptoms) & then the pt can tolerate quinine tablets so give him the same dose 8 hourly tabs for another 7 daystotal duration quinine is 9days at least . SE: 1. HYPOGLYCEMIA 2. Arrhythmia 3. Hypotension تسبب الموت لوالدرب مشى سرعة123 4. Tinnitus\deafness 5. Blindness Malaria vivax: الحمى الحبشية account for 12% OF malaria parasite cases. cause malaria parasite resistant . also can cause : 1. 2. 3. 4. Hyperparasitemia + fever Thrombocytopenia Coma Relapsing fever characteristic for vivax because merozoites of vivax can stay in the liver for 70 years. So once you treated vivax you have to eradicate merozoites from the liver by giving primaquine daily at least for 2-3 weeks otherwise you get relapsing fever p.malariae can cause nephrotic syndrome. ))غرب أفريقيا if the pt is splectomized give fansider +artesunate as prophylaxis in simple malaria ,quinine is contraindicated, you have to follow the protocol. if you give the pt quinine & after 3 days three days there is no improving it is most likely other diagnosis or quinine resistant ما عندنا في السودان Other DD for malaria 1. Typhoid fever 2. Severe pneumonia 3. Brucellosis 4. meningitis 5. Hepatitis 6. Kalazar 7. Leukemia Congenital malaria: 1. 2. 3. 4. 5. Neonates presented with criteria:Fever Jaundice Anemia Splenomegaly +ve BFFM Treatment : Quinine im 10mg \kg for 5-6days PD. Give sugar through NG tube because these are very sensitive to low blood sugar. prognosis :is very good Malaria with –ve BFFM:-don’t allow pt in Sudan die with fever unless you give antimalarial drugs because it's an endemic area في غانا في ناس ماتوا وبعد الوفاة لقوا ادمغتهم مالنه طفيليات بالرغم من ان التحاليل كانت سلبية Prognosis of cerebral malaria is good & we rarely lose pt due to cerebral malaria. Quinine IM Deep IM Instead of 1mg in 1ml of d5% when you give quinine IVhere 60 mg in 1ml of NS or d5% due to absorption is less.