Head Injury Case Study: Post-Craniotomy Care
advertisement

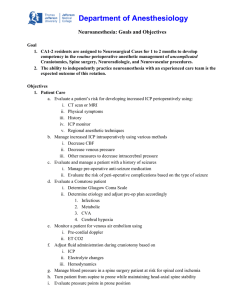
Case Study #3: Patient with Head Injury (56a) How did this case enhance your mastery of the content? It’s broken down into better memorable chunks, which is beneficial for my brain when learning convoluted content regarding the brain. For example, the list below is post-craniotomy. This list makes sense after both listening to the audio, reading the PPs, and then doing the case study. It’s starting to gel much better. The Glasgow Coma Scale “reinactment” helped me to better discern what each level or downgrade meant regarding patient status. ICP monitor Ventricular catheter Arterial catheter Cardiac monitoring ET tube with mechanical ventilation Head dressing D&I NS at 75 mL/hr NG tube to suction Measure ICP hourly HOB elevate 30-45 degrees (Elsevier, 2020). Using this case and all your prior knowledge, develop one nursing intervention applicable for this case study. Measure ICP hourly post craniotomy to ensure procedure is affective but also to ensure the ICP isn’t becoming worse from a post-op surgical bleed. -Describe two clinical outcomes anticipated for this case study scenario. **S.M.A.R.T. form** 1- Will keep HOB at 30* to avoid increased ICP this shift. 2- Will provide patient with stool softener for BMs, in order to avoid straining/Valsalva Maneuver and possibly increasing ICP this shift.