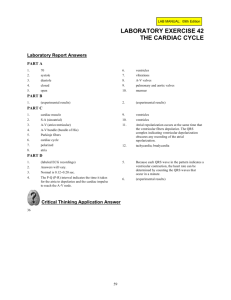
Molloy College The Barbara H. Hagan School of Nursing Nur 2900 Dr. D. Kantor Topic: Management of the Adult with Acute and Chronic Cardiovascular Disorders Classroom Learning Objectives: After completing the required learning activities and participating in classroom activities, the student will: 1. Utilize the nursing process as a framework for the care of patients who have acute and chronic cardiovascular disorders. 2. Describe risk factors associated with the development of acute and chronic cardiovascular disorders. 3. Describe the pathophysiology of acute and chronic cardiovascular disorders.. 4. Discuss clinical manifestations, diagnostic studies and collaborative treatment modalities for patients who have acute and chronic cardiovascular disorders. 5. Discuss the role of the nurse with respect to the treatment of the patient who has acute and chronic cardiovascular disorders. 6. Provide age appropriate, evidenced-based nursing interventions for the patients who have acute and chronic cardiovascular disorders. DK 7/20 Molloy College The Barbara H. Hagan School of Nursing Nur 2900 Dr. D. Kantor Acute and Chronic Cardiovascular Disorders 1. Angina Overview: Chest pain due to myocardial ischemia as a result of insufficient oxygen supply to the heart. Due to atherosclerosis or a blood clot. The decrease in oxygen and blood supply to the heart leads to changes in cellular metabolism which results in angina. On the cellular level, the myocardium becomes hypoxic within the first 10 seconds of coronary occlusion and with total occlusion of coronary arteries, contractility ceases after several minutes leading the deprivation of oxygen and glucose for aerobic metabolism to myocardial cells. Anaerobic metabolism begins and lactic acid accumulates. Lactic acid irritates myocardial nerve fibers and transmits a pain message to the cardiac nerves and upper thoracic posterior nerve roots. This accounts for the referred cardiac pain to the left shoulder and arm. In ischemic conditions, cardiac cells are viable for about 20 minutes. With restoration of blood flow, aerobic metabolism resumes, contractility is restored, and cellular repair begins. Chronic Stable Angina refers to chest pain that occurs intermittently over a long period with the same pattern of onset, duration, and intensity of symptoms. Risk Factors/Etiology 1. Atherosclerosis 2. Coronary Artery Spasm 3. Anemia 4. Exercise/sexual activity 5. Substance abuse (primarily stimulants such as cocaine) 6. Hyperthyroidism 7. CHF 8. Congenital heart defects 9. Pulmonary hypertension 10. Left Ventricular hypertrophy 11. Cardiomyopathy 12. Eating a heavy meal 13. Emotional distress Clinical Manifestations Angina: gradual or sudden onset: pain usually lasts less than 15 minutes and not more than 30 minutesusually about 3 minutes. Location: substernal or anterior chest pain, not sharply localized; radiation to back, neck, arms, jaws, upper abdomen, or fingers. Quality and Intensity: mild-to-moderate pressure, deep sensation, varied patterns of attacks. Patient will c/o tightness, squeezing, crushing or pressure Patient will also c/o 1. Dyspnea 2. diaphoresis and nausea 3. urge to void 4. belching 5. apprehension Diagnostic Studies 1. EKG: will show ST depression, T-wave inversion during acute pain 2. Stress test: will have abnormal EKG and patient will likely c/o chest pain 3. Coronary Arteriography: plaque accumulation 4. Serum Chemistry: elevated cholesterol 5. Cardiac Enzymes: within normal limits if patient did not have an MI 6. Holter monitoring: ST depression, T-wave inversion Treatment Modalities/Collaborative Care 1. Monitor vital signs, EKG, I & O, 2. Semifowler’s, bedrest at first 3. Oxygen via NC 4. Nutrition: Low calorie, low sodium, and low-cholesterol. 5. IV 6. ABG’s; lytes, cardiac enzymes: CK,LD, Troponin, troponin T and AST 7. Possibly: Percutaneous Coronary Interventions a. Percutaneous Transluminal Coronary Angioplasty: b. Corornary Artery Stent: c. Atherectomy d. Brachytherapy: Complications of Percutaneous Cornary Interventions: dissection, perforation, abrupt closure or vasospasm of the artery, acute MI, acute dsyrhythmias and cardiac arrest. If done as an outpatient, patient generally goes home same day or may stay one night. 8. Medications: a. Nitrates: Short Acting: Nitroglycerin, Long Acting: isorbide dinitrate (Isordil). Nitro also comes as a paste and as a transdermal patch (time release). b. Beta Blockers: (example: metoprolol/Lopressor; Atenolol/Tenormin; carvedilol/ Coreg) The preferred drug for chronic stable angina. c. Calcium Channel Blockers: (example: amlodipine/Norvasc; diltiazem/Cardizem; nifedipine/Procardia). Alert: Increase digoxin levels in first week of therapy therefore digoxin levels must be watched closely. D. ACE inhibitors (angiotensin-converting enzyme inhibitors) (examples: captopril/Capoten; enalapril/Vasotec). Given to patients at high risk of a cardiac event. E. Other: cardiac glycoside Digoxin (Lanoxin), antiarrhythmics 10. Pain medications: morphine or demerol (meperidine) Nursing Management 1. Assess vital signs. 2. Administer oxygen and medications as ordered. 3. Record I & O and check lab studies 4. Assess for chest pain 5. Maintain bedrest 6. Encourage patients to verbalize feelings 7. D/C instructions: NTG tabs good for 6 months, should be kept in bottle, teach difference between MI and cp, avoid activities which may precipitate cp, seek med assistance if pain lasts more than 20 minutes. Patients with other medical-surgical disorders may be hospitalized with a history of angina. Generally these patients are permitted to have Nitroglycerin tablets at the bedside. If you have a patient who has a history of angina, what assessment would you carry out? 2. Stable Myocardial Infarction Overview: An MI is the death of a portion of myocardial tissue due to lack of oxygen from inadequate perfusion. Narrowing eventual obstruction from plaque accumulation. Risk Factors/Etiology 1. Atherosclerosis 2. Inadequate perfusion to meet metabolic demands 3. Embolism or thrombus 4. Coronary artery spasm Stable myocardial infarction refers to patients who had an MI and were treated in telemetry floor or intensive care unit and are then discharged to a medical unit. On telemetry floor or intensive care unit, patient was treated with medications, oxygen therapy and put on bedrest. When patient is transferred to regular medical unit, generally medications are working. Treatment Modalities/Collaborative Care Generally medications given for an MI patient are similar to what is given for hypertension and angina: 1. ACE inhibitors 2. Nitrates 3. Beta blockers but usually not given if patient has congestive heart failure 4. Calcium channel blockers 5. May also have been given thrombolytic therapy anistreplase (Eminase), streptokinase (Streptase) to dissolve clot. Diet restrictions: low cholesterol, low-fat, low sodium diet Nursing Management 1. Assess vital signs 2. Administer oxygen and medications 3. Assess resp and cardiac status 4. Semi-fowler’s 5. D/C teaching: cardiac rehab program, low cholesterol, low-fat, low sodium diet; difference between angina and M. I. pain; rest periods 3. Congestive Heart Failure Overview: Can be due to right sided or left sided heart failure Risk Factors/ Etiology for Left Sided Failure 1. Atherosclerosis 2. Fluid overload 3. MI 4. Valvular Stenosis 5. Valvular Insufficiency 6. Hypertension 7. Cardiac Conduction Deficits 8. Cardiomyopathy 9. Infection 10. Immune and connective disorder 11. Endocrine imbalance Risk Factors/ Etiology for Right Sided Failure 1. Atherosclerosis 2. Left-sided heart failure 3. COPD 4. Valvular Stenosis 5. Valvular Insufficiency 6. Pulmonary Hypertension Pathophysiology for Left Sided: Decreased myocardial contractility or increased myocardial workload, either of which increases left ventricular pressure and left atrial pressure and reduces cardiac output. Patient also develops impaired oxygenation and respiratory manifestations of fluid overload. Pathophysiology for Right Sided: Increased pressure from left-sided heart failure, increase venous congestion in the systemic circulation with fluid overload, increased resistance in lungs. Clinical Manifestations for Left Sided 1. Dyspnea 2. Paroxysmal nocturnal dyspnea 3 Crackles, wheezes, rhonchi 4. Cough 5. Hemoptysis 6. Gallop rhythm: S3, S4 7. Arrhythmias 8. Fatigue, Anxiety 9. Tachycardia, Tachypnea 10. Diaphoresis Clinical Manifestations for Right Sided 1. Jugular vein distention 2. Anorexia, N/V 3. Abdominal distention, Acites 4. Hepatomegaly 5. Dependent edema, peripheral edema and weight gain 6. s/s of left-sided failure 7. Tachycardia, Gallop rhythm: S3, S4 8. Fatigue, nocturia Treatment Modalities/Collaborative Care As with angina and MI, patients with a history of CHF or patients admitted with CHF may be transferred to regular medical surgical unit from either a telemetry floor or intensive care unit. 1. Oxygen 2. Phosphodiesterase inhibitors (amrinone, milrinone) 3. Inotropic agents (dopamine, dobutamine) 4. ACE inhibitors 5. Diuretics (Lasix) 6. Anticoagulants (Heparin, Coumadin) 7. Vasodilators (hydralazine) 8. Cardiac glycosides (Digoxin) 9. Calcium channel blockers (norvasc, procardia) Nursing Management 1. Assess/Monitor: for pulmonary and systemic fluid overload, vital signs, lung sounds for crackles, wheezes, hemodynamic changes 2. Assess lytes 3. Daily weight 4. Assess for mental changes 5. I and O 6. Hi fowler’s, Oxygen if prescribed, bedrest until stable then OOB as tolerated, assist with ADL’s, fluid and sodium restrictions, emotional support 7. D/C instructions: meds, diet, activity, s/s to report. 4. Basic Dysrhythmias Definition of Dysrhythmias (AKA Arrhythmias): Abnormal electrical conduction or automaticity resulting in changes in heart rate and rhythm. Leads to decrease in cardiac output. Originate in SA (sinoatrial) node, atria or AV (atrioventricular) node or ventricle, name depends on where it originates. Background A cardiac cell is semipermaeable which allows it to maintain a high concentration of potassium and low concentration of sodium inside the cell (refer back to electrolytes if needed). Conversely, a high concentration of sodium and a low concentration of potassium exists outside the cell. At rest, the inside of the cell is polarized, is negative compared to the outside of the cell. When a cell or group of cells are stimulated, each cell membrane changes its permeability and allows sodium to enter the cell rapidly which in turn makes the inside of the cell positive compared to the outside (depolarization). A slower movement of ions across the cell membrane restores the cell to the polarized state called repolarization. EKG 12 leads, measure electrical forces in the frontal plane and horizontal plane. May show changes in electrical conduction suggesting structural changes or damage such as ischemia, infarction, enlarged cardiac chambers, electrolyte imbalances, or drug toxicity. And dysrhythmias. EKG Review P Wave: Represents the time needed for the passage of the electrical impulse to go through the atrium causing atrial depolarization (contraction), should be upright. 0.06-0.12 sec PR Interval: Measured from the beginning of P wave to beginning of QRS complex; it represents time taken for impulse to spread through the atria, AV node, and bundle of His, the bundle branches, and Purkinje fibers, to a point immediately preceding ventricular contraction. 0.12-0.20 sec QRS Interval: Measured from beginning to end of QRS complex; represents the time taken for depolarization (contraction) of both ventricles (systole). < 0.12 sec ST Segment: Measured from the S wave of the QRS complex to the beginning of the T wave; represents the time between ventricular depolarization and repolarization (diastole); should be isoelectric (flat). 0.12 sec T Wave: Represents time for ventricular repolarization; should be upright. 0.16 sec QT Interval: Measured from the beginning of QRS complex to end of T wave; presents time taken for entire electrical depolarization and repolarization of the ventricles. 0.34-0.43 sec Definition of Dysrhythmias (AKA Arrhythmias): Abnormal electrical conduction or automaticity resulting in changes in heart rate and rhythm. Leads to decrease in cardiac output., which is the issue. Originate in SA (sinoatrial) node, atria or AV (atrioventricular) node or ventricle, name depends on where it originates. Risk Factors/Etiology 1. Congenital 2. Myocardial ischemia 3. Organic heart disease 4. Drugs: Side effects and toxicity 5. Conductive tissue degeneration 6. Electrolyte imbalance 7. Acid-base imbalances 8. Cellular hypoxia Clinical Manifestations 1. Asymptomatic 2. Palpitations, chest pain 3. Dizziness, weakness, fatigue 4. Feelings of impending doom 5. Irregular heart rhythm, bradycardia, or tachycardia 6. Hypotension 7. Syncope 8. Altered level of consciousness 9. Diaphoresis; cold, clammy skin 10 N/V If patient has a life-threatening dysrhythmias- assessment will reveal pulselessness, absence of respirations, and no palpable blood pressure. Diagnostic Studies 1.EKG will show change in rate and rhythm 2. Lytes Regular Sinus Rhythm: Rate is between 60 and 100 beats/minute; One P wave before each QRS complex; P waves are uniform. PRI is consistent and measures between 0.12 sec to 0.20 secs. Basic Dysrhythmias 1. Atria a. Premature atrial contraction (PAC): Occurs when atrial tissue becomes irritable. This ectopic focus fires an impulse before the next impulse is due. P waves are premature and differ in configuration from normal P waves. May be due to digoxin toxicity, aminophyline, adrenergics, or caffeine or anxiety. Usually not treated but underlying cause may be. b. Atrial Flutter: Atrial rhythm rate will be 250-400 beats/minute. Ventricular rate depends on the degree of the AV block but will usually be 60-100 beats/minute. Saw tooth P wave. Due to heart failure, tricuspid or mitral valve disease, pulmonary embolism, cor pulmonale, inferior wall MI and digoxin toxicity. Treated with: Cardioversion if patient is unstable and ventricular rate is greater than 150 beats/min; medications (calcium channel blockers, beta blockers, antiarrhythmics, diltiazem; also heparin or coumadin c. Atrial Fibrillation: Atrial rhythm very irregular with more than 400 beats/minute and ventricular rate will be very irregular. QRS complexes of uniform configuration and duration; PR interval not discernible; No P waves or P waves are erratic, irregular, baseline fibrillatory waves. Due to heart failure, COPD and other etiologies. Treated with: Cardioversion if patient is unstable and ventricular rate is greater than 150 beats/min; medications (calcium channel blockers, beta blockers, antiarrhythmics); also heparin or coumadin. Also radiofrequency catheter ablation to the His bundle to interrupt all conduction between atria and ventricles. Also Maze procedure: sutures placed in stragetic sites in atria to prevent the atrial fibrillation. d. Sinus Tachycardia: Atrial and ventricular rhythms are regular but rate is more than 100 beats/minute but rarely more than 160. Normal P waves precedes each QRS complex. Due to: normal physiologic response to fever, exercise, anxiety, pain, dehydration and many other causes. Treated with: Correction of underlying cause; if patient is symptomatic: calcium channel blockers, beta blockers e. Sinus Bradycardia: Atrial and ventricular rhythms are regular but rate is less than 60 beats/minute. Normal P waves precedes each QRS complex. Due to increased intracranial pressure, increased vagal tone due to val salva maneuver, intubation, mechanical ventilation, hypothyroidism and others. Can also occur in normal conditioned heart as with athletes. Treated with: Correction of underlying cause; if low cardiac output atropine; temporary or permanent pacemaker, dopamine or epinephrine infusion. F. Premature Ventricular Contraction: Atrial rhythm is regular but ventricular rate is irregular. QRS complex is premature, usually followed by a complete compensatory pause. QRS complex is wide and distorted usually greater than 0.14 sec. The QRS complex occurs as singly, in pairs, or in threes. Treated with amiodarone, procainamide, or lidocaine. Also with potassium if hypokalemic and/or magnesium sulfate if hypomagnesemia is underlying cause. G. Ventricular Tachycardia: Ventricular rate is 140 to 220 beats/minute, rhythm can be regular or irregular. QRS complex is wide, bizarre, and independent of P waves. P waves are not discernible. may require CPR if meds unsuccessful H. Ventricular Fibrillation: Ventricular rhythm chaotic, rate is rapid. QRS complex is wide and irregular (basically not present), no visible P waves. Requires CPR Overall Treatment Modalities/Collaborative Care Treatment is dependent on the dysrhythmia. 1. Monitoring 2. Oxygen 3. Medications 4. Pacemaker insertion: permanent or temporary. Batteries last 4-12 years. Done with overnight staypatient on bedrest until pacemaker is checked as working properly. 5. Defibrillation: unsynchronized shock used for ventricular fibrillation or Pulselessness ventricular tachycardia 6. Cardioversion: Synchronized shock used for atrial dysrhythmias or ventricular tachycardia Nursing Management 1. Assess vital signs 2. Administer medications as ordered 3. Administer oxygen as ordered 4. Telemetry monitoring 5. D/C teaching. Nursing Care of the Patient Who Has Acute and Chronic Cardiovascular Disorders Critical Thinking Questions: 1. What would you anticipate the overall goals of nursing care for patients with Acute and Chronic Cardiovascular Disorders to be? 2. What is the overriding issue for patients with acute and/or chronic cardiovascular disorders? What is the role of the nurse in assisting patients with these disorders? 3. You have a patient with a history of angina. Describe what care you would provide this patient with and why. 4. How would you complete the following nursing diagnosis statements and how do they pertain to patients who have Common Cardiovascular Disorders? Do you agree or disagree with the priority numbers that are indicated (Be sure to be able to provide rationales for your answer)? 1. Decreased Cardiac Output 2. Acute Pain 3. Activity Intolerance 4. Fluid Volume Excess 5. Risk for Skin Impairment 6. Altered Tissue Perfusion 7. Self Care Deficit 8. Powerlessness DK 8/09; rev 1/14; 7/20 Molloy College The Barbara H. Hagan School of Nursing Nur 2900 Dr. D. Kantor Critical Thinking Exercises for the Patient with Acute and Common Cardiovascular Disorders Exercise #1 What nursing care should be anticipated for a patient with angina? The health care practitioner has given the patient a prescription for NTG, what discharge instructions should be given? 2. What are the top three priority nursing interventions for a patient who has been diagnosed with a stable MI? What are your rationales? 3. A patient has been diagnosed with Congestive Heart Failure. What are the differences in clinical manifestations between left and right-sided heart failure? What is the supportive pathophysiology to support the differences? What nursing interventions do you anticipate for this patient? What are your rationales? 4. Be able to explain the different types of dysrhythmias discussed in class. Which ones are lifethreatening? Why? What is the overall nursing care for a patient with a dysrhythmia? 5. Think about the various clinical manifestations that may arise in patients with cardiac disorders. Based on what we discussed in class, think about what clinical manifestations should be addressed immediately, which are a concern but are not life threatening, and which are expected. What are the physiological risks for the patient with the diseases discussed in class, how will nursing address these? dk 1/14