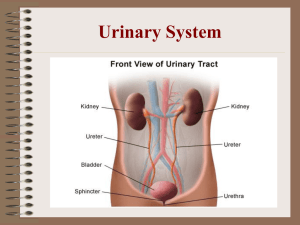
1. Define the essential terms found in the assigned readings. Kidney – bean-shaped organs located retroperitoneally (behind the abdominal contents). They are held in place by connective tissue called renal fascia. The adrenal gland, an endocrine organ, sits on top of each kidney. Papillae – The narrow tips of the renal pyramids. They empty urine into the calyces, cuplike collection structures. Pyramids - The innermost layer of the kidney the pyramids make up the medulla. Each kidney contains 1218 pyramids Aldosterone – A hormone secreted from the adrenal cortex that increases the reabsorption of sodium in the DCT, and where water goes, sodium follows. Afferent arterioles – Formed off cortical radiate arteries. They form a collection of capillaries that direct blood flow to the glomeruli of the nephrons Antidiuretic hormone (ADH) – Also known as vasopressin, is a hormone that controls the permeability of the DCT Anuria – Less than 100 mL of urine output per 24 hours Bladder - a muscular reservoir for urine until it is excreted from the body Composed of 3 layers – the outer lining, the middle smooth muscle, and the inner urothelium which is resistant to bacterial colonization The trigone is the region at the base of the bladder between the ureters and the urethra o This this is the common location of bladder infections Can hold up to 600-1000mls depending on the person. o The urge to urinate usually happens at 200-250mLs of urine Bowman’s capsule – The structure surrounding each glomerulus Creatinine – the end product of protein and muscle breakdown in the body, filtered by the kidneys. o Normal range is 0.5-1.2 mg/dL Distal convoluted tubule (DCT) – Before the collecting tubule, Reabsorbs: H2O, bicarbonate, chloride, and sodium. Excretes: H+, K+, and ammonia Dysuria – Difficulty of pain with urination Efferent arterioles – Capillaries from the glomeruli merge and then form the efferent arterioles that transport blood away from the glomeruli and into the peritubular capillaries. Erythropoietin – A hormone produced by the kidneys in response to decreased renal blood flow and hypoxia. This hormone stimulates the bone marrow to produce RBCs. Glomerular filtrate – Formed when the blood enters the capillaries of the glomerulus by hydrostatic pressure. This pressure forces electrolytes, water, hydrogen, creatinine, and glucose across the glomerular membrane and into the bowman’s capsule. From there, it travels to the PCT and is termed tubular filtrate. Glomerular filtration rate (GFR) – The amount of blood that is filtered by the glomeruli in a set amount of time Normal GFR is approximately 125 mL/min In a healthy adult, 1-3 L of filtrate is excreted as urine per day GFR is dependent on systemic BP, blood flow and volume Kidney maintains rate by increasing or decreasing pressure in the glomerular capillaries: o Constriction on afferent arterioles and dilation of efferent arterioles will decrease pressure and decrease filtration rate o Dilation of afferent arterioles and constriction of efferent arterioles will increase pressure and increase filtration rate o If systolic BP is <70mmHg, kidneys can’t compensate, GFR ↓ Glomerulus – A collection of semipermeable capillaries responsible for filtering blood Loop of Henle – Composed of a descending and ascending tube Descending Reabsorbs: Water o Excretes: Urea Ascending Reabsorbs: Na+, Cl-, K+ Major calyces – Formed by a merging of minor calyces toward the hilum Minor calyx – A small cluster of calyces Nephron – The functional unit of the kidney where the filtering of the blood to produce urine occurs. There are about 80,000 to 1.2 million nephrons within each kidney. 80% are cortical nephrons o Short and contained within the cortex region 20% are juxtamedullary nephrons o Lie deep within the medulla of the kidney Nocturia – Increased need to urinate at night Oliguria – Decreased urine output, 100-400 mL/24 hours Polyuria – Increased urine output, >2000 mL/24 hours Proximal convoluted tubule (PCT) – Responsible for reabsorbing 65% of the glomerular filtrate. Emerges from bowman’s capsule Reabsorbs: o Glucose, Amino acids, Proteins, Vitamins, Lactate, Urea, Uric acid o Na+, K+, Ca2+, Mg2+, Cl-, HCO3-, H2O Secretes: o Urea, Uric acids, creatinine, H+, NH4+, Some drugs Prostaglandins – Hormones produced by various tissues in the body. Within the kidneys, they trigger vasodilation and increase renal blood flow and lower systemic BP (also increase the excretion of H2O and Na2+ With pts that have renal disease, PG production is decreased which is why we might see the development of hypertension associated with renal failure Renal pelvis – A large collection sac where the major calyces empty Renin – A hormone released by the kidneys that can help to increase systemic BP. Release is stimulated when kidneys detect drop in blood flow or pressure, or a drop in Na is detected. Reacts with angiotensinogen in the liver and makes angiotensin 1 Reacts with ACE secreted by the lungs to form angiotensin 2 Angiotensin 2 constricts the blood vessels to increase BP and stimulates the release of aldosterone which will increase fluid volume by increasing reabsorption of Na+ and subsequently, H2O Vitamin D – Activation of vitamin D begins in the liver and ends in the kidneys. The kidneys turn vitamin D into calcitriol. This activated form of vitamin D is required for the GI tract to absorb Ca2+. Remember! Ca2+ and PO3- have an inverse relationship. When one increases the other decreases o Therefore, since pts with renal disease have ↓calcium, they will have ↑ phosphate levels 2. Describe key anatomical components and functions of the renal system. 1. Main functions of the renal system: o Urine formation and excretion of wastes o Regulation of fluids and electrolytes and acid/base balance To prevent dehydration 99% of glomerular filtrate is reabsorbed Reabsorption & excretion of bicarbonate and hydrogen depends on blood pH When serum osmolality increases because of dehydration, ADH is released and vice versa The rate of reabsorption and secretion of each electrolyte is dependent on the serum concentration of that electrolyte o When higher than normal levels are detected by the kidneys, more of that electrolyte is excreted o Aldosterone secretion stimulates the reabsorption of sodium and secretion of K+ in the DCT o Hormonal Functions 1. Erythropoietin stimulates bne marrow to produce RBCs 2. Vitamin D is not usable until it is converted to its activated form by the kidneys 3. Prostaglandins made by the kidneys trigger vasodilation, increased blood flow to the kidneys, and increases Na+ and water secretion. Lowers systemic BP 4. Bradykinin is released by the kidneys in response to the presence of PGs, ADH and angiotensin 2. It increases the permeability of the capillary membrane to certain solutes and dilates the afferent arteriole to ensure reabsorption of solutes. 3. Describe the procedure for completing a history and physical assessment of the renal and urinary systems. 1. Demographics: o Gender: Women are more prone to UTIs, Men are prone to benign prostatic hypertrophy, nonmalignant enlargement of the prostate gland, and prostate cancer o Age: Older adults are more prone to urinary incontinence, increased urgency, frequency, retention and nocturia. Also, bladder cancer o Race: African American groups have an increased incidence of DM and hypertension. These diseases are both precursors to renal dysfunction o Socioeconomic status: low status has increased development of renal diseases and complications o occupational history, o Diet, o Smoking history 2. Personal and Family History 3. Medication Use 4. Renal and Urinary Assessment 5. Physical: o Inspection, Auscultation, Palpation, and Percussion 4. Explain diagnostic studies relevant to renal system function and the nursing considerations for each study. Laboratory studies: 1. Serum Creatinine – a. Normal range = 0.5-1.2 mg/dL b. Males typically have more creatinine because of larger muscle mass c. With age, muscle mass ↓ therefor creatinine levels decrease i. Creatinine clearance also decreases so normal levels are maintained in healthy, normal adults d. Increases in serum creatinine are not seen until 50% of renal function is lost i. This means that any increase in creatinine warrants immediate investigation and intervention e. Increases may be caused by: i. Acute and/or chronic kidney injury or disease ii. Cancer iii. Diabetic neuropathy iv. Shock v. CHF f. Decreases may be caused by: i. Loss of muscle mass ii. Certain Medications 1. Antibiotics such as: aminoglycosides and cephalosporins 2. Lithium Carbonate 2. Blood Urea Nitrogen – Urea nitrogen is the by-product of protein metabolism that occurs in the liver a. Increased BUN causes: i. Renal dysfunction 1. Elevated Bun is not diagnostic of renal disease but indicates it as a possibility 3. 4. 5. 6. ii. Liver disease iii. Dehydration – Always consider hydration status iv. Infection v. Consumption of a high protein diet vi. GI bleeding vii. Steroid Use viii. Trauma b. Decreased BUN causes: i. Severe liver damage ii. Malnutrition iii. Low-protein diet iv. Fluid Volume excess BUN/Creatinine Ratio – can be utilized to assess if the cause of elevated BUN is renal or nonrenal a. Normal Ratio Range: 10:1 – 20:1 b. Increased BUN to creatinine ratio: i. Can be caused by hypovolemia or hypotension c. Increased BUN to creatinine ratio: i. Can be caused by fluid volume excess d. Normal ratio, but both levels are increased: i. Renal dysfunction is likely Uric Acid – Formed as a byproduct of purine metabolism. Purines are naturally occurring in body cells and also found in dietary sources such as: organ meats, anchovies, sardines, shellfish, asparagus, beans, mushrooms, and spinach a. Normal Range: 3.5 – 8 mg/dL b. Critical value: >12 mg/dL i. Excess uric acid is termed hyperuricemia ii. Can result in the development of uric acid crystals in the joints aka gout c. Uric acid values are dependent on renal function, rate of purine metabolism, and dietary intake d. Causes of Increased levels: renal failure, multiple myeloma, malnutrition, leukemia, lymphoma, metastatic cancers and alcoholism e. Causes of Decreased levels: Burns, pregnancy, folic acid anemia, Wilson’s disease, and medications such as: allopurinol, rasburicase, azathioprine and warfarin Bicarbonate – Normal range: 22-26 mEq/L a. Decreased levels can be the result of renal failure, DKA, severe diarrhea, burns, and malnutrition. Electrolytes – a. Sodium: i. Late stage renal disease alters Na+ balance because of fluid volume excess due to the kidney’s decreased ability to filter and excrete properly b. Potassium: i. Kidney’s excrete majority of K+ ii. First electrolyte to reflect a change in kidney function iii. K+ levels ↑ as kidney function ↓, hyperkalemia is seen and heart dysrhythmias can occur and require immediate intervention c. Phosphorus: i. Normal range: 2.5 – 4.5 mEq/L ii. Kidney function ↓ causes phosphorus ↑ d. Calcium: i. Normal level: 8.2 – 10.2 ii. Inverse relationship with phosphorus, as kidney function ↓ then Ca2+ ↓ Urine Tests: 1. Bedside Urine dipsticks – Tested at bedside to assess specific gravity, pH, presence of protein, glucose, bilirubin, blood and ketones a. Fresh sample should be used for testing 2. Urinalysis – Overall examination of urine to provide baseline data or to monitor specific characteristics of urine a. Sample should be sent within 1 hour or refrigerated until it can be sent Culture and Sensitivity: Useful to identify the number and types of bacteria present 1. Urine should be collected using clean-catch method and a sterile container Composite Urine Collection: Involves collecting all urine voided for a defined period ranging between 2 and 24 hours. Collected after voiding of first urine of the day (discard this one) 1. Used to measure the quantity of specific components including: o Electrolytes o Minerals o Creatinine o Protein and glucose Creatinine Clearance: 1. 2. 3. 4. Reliable indicator of GFR Used with 24-hour collection but sometimes shorter collection times are ordered Urine and blood sample creatinine levels are compared using special formulas Normal range: 88 – 137 mL/min Urine Cytology: Used to identify any abnormal cells in the urine, which are often present in cases of bladder cancer. Use urine sample other than first void of the day. Send to lab within 1 hour Intravenous Urography: Requires injection of intravenous contrast dye. This dye is circulated through the body where x-rays are taken at specific time intervals. The dye is then filtered by the glomeruli, and then excreted by the kidneys. A final x-ray is taken at this time after the patient urinates to measure any residual urine in the bladder. Indication: o To measure the size and anatomy of the KUB, cysts, tumors, calculi, and any obstructions. Nursing Implications: Preprocedural: 1. 2. 3. 4. Pt must complete a bowel prep the night before the procedure Pt must remain NPO 8 hours before the procedure Inform the patient that the procedure lasts only 30-45 min and should not cause pain Inform the patient that they feel a flushing feeling after the dye is injected and a salty taste in their mouth 5. Signed informed consent must be on file 6. Dye is nephrotoxic! Assess baseline creatinine clearance. 7. Question patient regarding any allergies to dye Postprocedural: 1. 2. 3. 4. Pt must increase fluid intake (to flush out dye) Monitor patient I&Os and IV site Be aware of any signs of delayed reaction to contrast: rash, dyspnea, tachycardia Changes is renal labs Renal Ultrasound: Conductive gel is applied to the patient’s skin and an external probe is moved across the abdomen. Ultrasound images are produced back with no harm to the patient Indications: Can be used to determine kidney size. Small kidneys can indicate chronic kidney disease and larger than normal kidneys can indicate polycystic kidney disease or an obstruction. Nursing implications: Patients might be instructed to drink up to 24 oz of fluid 1 hour before the ultrasound and to not void until it is over. No other preparation or monitoring is required. CT Scan: These scans are not commonly used as a first line diagnostic test but may be used to further examine findings from other studies like x-rays or US. Indications: CT scans can detect slight variances in densities, providing more specific results regarding kidney size, tumor or obstruction size, and renal vessels. Nursing Implications: 1. Instruct the patient to remain NPO for several hours prior to the procedure 2. Make sure there is a signed informed consent 3. Educate the patient on the fact that they must remain completely still while the scanner rotates around their body 4. Educate the patient and let them know that the study will last about 10-15 minutes 5. Assess the patient for allergies and baseline renal function. The patient’s renal function will determine whether or not contrast dye is used MRI: MRIs are known for their ability to reveal contrasts between soft tissues in the body Indications: They are useful in examining kidney tissue and assessing for abnormalities Nursing Implications: 1. Educate the patient on: a. The length of time the study takes, up to 90 minutes b. The scan is painless c. Any metal object on the body must be removed d. If the patient has claustrophobia or is unable to lie still, consider sedation, antianxiety medication, or an open MRI system. 2. Make sure a signed informed consent is on file 3. Ask and verify if the patient has a pacemaker or any type of implanted medical device (MRI is contraindicated in this case). 4. Assess for allergies and baseline renal function due to contrast dye that may be used Cystography and Urethrography: For this procedure, contrast dye is injected into the bladder via a catheter or a cystoscope. Then a thin lighted instrument is inserted into the urethra and slowly advanced into the bladder. Indications: Used to assess the bladder for abnormalities, including calculi and masses. It is also used to examine the bladder if trauma is suspected. A urethrography is done to assess for trauma to the urethra A specific type of this test called a voiding cystourethrogram (VCUG) o This type of test is preformed to assess is vesicoureteral reflux is present o The patient is required to void after the bladder is filled with contrast dye while x-rays are taken. o If reflux is present, urine is backflowing from the bladder into the ureters and kidneys, increasing the chance for kidney infection. Nursing Implications: Pre: 1. Educate the patient regarding the risks and indication for the procedure. 2. Make sure informed consent is on file 3. Assess for allergies to contrast, iodine, and shellfish. No contrast enters the bloodstream so there is no risk for nephrotoxicity. Post: 1. Monitor for signs and symptoms of infection. 2. Educate the patient on the signs and symptoms of infection and adequacy of urine output once discharged Renography (Kidney Scan): A radionuclide is injected IV and is absorbed by the kidney tissue. An external probe is placed over the kidney to detect radiation emissions and images are produced. Indication: Useful in determining kidney size, renal blood flow, glomerular and tubular filtration, and urinary excretion. Nursing Implications: Make sure signed informed consent is on file. There is no specific patient preparation or monitoring required for this procedure. Renal Biopsy: This test involves removing a tissue sample via a small percutaneous (through the skin and tissue) site using US or CT guidance while the patient is sedated and lying in the prone position. Indication: This study is useful in ruling out malignant processes and diagnosing renal abnormalities that have not been successfully diagnosed with other tests. Nursing Implications: Pre-: 1. Educate the patient regarding the risks and the procedure itself. 2. Make sure signed informed consent is on file. 3. Patient must be NPO for 4-6 hours prior to the procedure 4. The patient must also stop taking aspirin, warfarin, and other agents that may affect the ability of blood-clotting 5. Send a type and screen and coagulation values to the lab before the study 6. Obtain baseline vital signs and monitor vital signs frequently during the biopsy Post-: 1. Apply manual pressure to the site until bleeding has stopped. 2. Assess H&H levels 3. Assess for signs of internal bleeding such as, flank pain, decreased urine output, decreased BP, hypovolemia, and shock. 4. Patient must remain on bedrest for up to 24-hours 5. Educate the patient that some local discomfort may occur, but pain that radiates to the abdomen and flank should be reported. 6. Patient should increase his fluid intake. 7. Hematuria is a common complication, but it usually resoles after 48-72 hours. The HCP should be notified if it lasts more than 72 hours or if there are blood clots in the urine. 8. Avoid heavy lifting for 1 week 9. Do not resume taking anticoagulants until instructed by the HCP Cystoscopy: A cystoscope is a tubular lighted device that is inserted through the urethra while the patient is sedated and in the lithotomy position. Indications: This is a surgical procedure utilized to treat and or diagnose bladder problems. It can be preformed using local or general anesthesia. - As a diagnostic tool, this procedure can be used to assess for bladder trauma, urethral trauma, or urinary tract obstructions. Can also be used to remove an enlarged prostate gland, bladder tumors, or renal calculi. Nursing Implications: Pre-: 1. Educate the patient regarding: a. Indication and risk for the study b. NPO after midnight c. Bowel prep required before the procedure 2. Make sure signed informed consent is on file 3. Assess baseline vital signs before the procedure, frequently during the procedure, and immediately after the procedure. Post-: 1. Assess urine volume to ensure adequate output 2. Educate the patient regarding: a. Expected finding following the procedure such as: urinary frequency and pink tinged urine. b. Gross bleeding and/or clots should be reported to the healthcare provider c. Mild analgesics and topical treatments like warm moist heat and sitz baths may be used to manage discomfort d. Monitor for signs and symptoms of infection such as fever, chills, and dysuria. Chapter 62 5. Describe the epidemiology of renal disorders. 1. Polycystic kidney disease o PKD is one of the most common genetic disorders in the world. It affects 1 in 600,000 people in the U.S. and 12.5 million people worldwide o PKD represents 10% to 15% of chronic renal disorders o Two forms of PKD: 1. Childhood: - Autosomal recessive - Less common, rapid and progressive, leads to lung and liver dysfunction and ESRD - Causes death during infancy or childhood 2. Adult: - Autosomal dominant - Affects 1 in 540,000 - 50% chance of genetic inheritance - Cysts are not limited to kidneys, may affect liver, spleen and pancreas - Lies dormant for many years before emerging in 30s and 40s - Prevalence is equal for men and women 2. Pyelonephritis o One of the most common renal diseases o More prevalent in women, especially young women o Older adults and infants are also at increased risk because anatomical variations and hormonal differences o Major risk factor is multiple preexisting UTIs, treated or untreated. 1. These infections can be caused by pregnancy, sexual activity, BPH, urinary stones, vesicoureteral reflux 3. Glomerulonephritis o This is an inflammation of the glomeruli of the kidney o 3rd leading cause of CKD in the US o Caused by autoimmune diseases such as lupus, vasculitis, or an infection from streptococcus o Classified as acute or chronic: 1. Acute: develops as a result of a complication from an infection, and can be found in patients of all ages but mostly children and young adults 2. Chronic: Results from some of the same causes as acute and can also be genetic - Develops slower with fewer symptoms - Can cause irreversible damage o Risk factors: 1. Recent strep infections 2. Autoimmune diseases such as lupus, vasculitis, HTN, and diabetes 4. Chronic kidney disease o CKD is a worldwide health problem that is steadily increasing in incidence and prevalence o Prevalence is higher for individuals 60 or older o Rates are higher in African Americans and Native Americans o Higher rates in men o Most common causes are HTN and DM o Other risk factors include hyperlipidemia, smoking, use of recreational drugs, NSAIDs, obesity, glomerulonephritis, PKD, lupus, atherosclerosis 6. Correlating clinical manifestations to pathophysiological process of: 1. Polycystic kidney disease o Large fluid filled cysts are formed in the cortex and medulla of kidneys through repeated cell division within the renal tubules. o The progressive expansion of these cysts causes them to separate and become isolated sacs. o These cysts become large and compress the surrounding tissue causing: 1. Hypertension because of damage to surrounding renal tissue 2. Hematuria after rupture of large cysts 3. Pain in lower back, abdominal, and flank area and headaches. 4. Symptoms of UTI because of obstruction to urinary flow 5. Enlarged kidneys, increased abdominal girth, and costovertebral tenderness that can be felt on palpation o PKD progresses to ESRD in 50% of patients by age 60 o Remaining 50% of patients have mild to moderate symptoms and generally dies from complications such as infection or impaired renal function 2. Pyelonephritis o This disease is an inflammation of the functional renal tissue and urinary collecting system. The most common cause is a bacterial infection (E. coli) because of contamination of the urinary meatus with bacteria found in the GI tract that ascend via the ureters to the renal tissue o Manifestation include S/S of infection 1. Fever 2. Chills 3. N&V 4. Back or flank pain o Costovertebral tenderness and kidney enlargement can be noted on palpation o Symptoms of UTI: 1. Dysuria, polyuria, and hematuria 3. Glomerulonephritis o This disease is an inflammation of the glomeruli triggered by an immunological mechanism. There are two types if immunological conditions affecting the glomerulus in glomerulonephritis o Type 1: Antibodies produced are specific to antigens within the glomeruli and glomerular basement membrane. Immunoglobulin and complement are deposited along the basement membrane. o Type 2: Antibodies react to antigens not specific to the glomerulus but still deposit immune complexes along the GBM. o Both types result in an accumulation in the glomeruli and GBM that result in injury to the GBM and a decrease in effective filtration 1. Patients are edematous with ↓urine output and hypertension - Acistes, peripheral edema, generalized body edema, and periorbital edema - Abdominal and flank pain may be present 2. BUN and creatinine levels ↑ o ↓ GFR and ↑ permeability to larger size proteins 1. Protein, blood, WBCs, and casts are seen in the urine (hematuria) 4. Chronic kidney disease o CKD is the progressive irreversible loss of kidney function o It is characterized by slow increases in BUN and creatinine o Longer and more insidious onset than AKI o May be the result of poorly managed AKI o May be asymptomatic until very little renal function remains o Typical S/S of renal failure 7. Discuss the medical management of: 1. Polycystic kidney disease o Diagnosis: Diagnosis is based on clinical manifestations and patient and family history. 1. Lab tests such as UA may reveal hematuria or bacteriuria 2. Definitive diagnosis is made using abdominal US, MRI, and CT scan o Treatment: 1. Severe PKD: Treatment is consistent with ESRD where hemodialysis or peritoneal dialysis is used 2. Treatment goals for PKD: - Managing UTIs, pain, and hypertension. - Regular check-ups and immediate treatment for clinical manifestations of infection - Antibiotics to control spread of infection to the kidneys - Pain can be controlled with acetaminophen or morphine - Severe pain may require nephrectomy - Hypertension can be managed with ACE inhibitors and angiotensin receptor blockers - Lifestyle changes for proper diet, exercise, and smoking cessation - Renal transplant may be the only curative measure o Complications: 1. Severe hypertension 2. Renal calculi 3. Recurrent UTIs 4. Hematuria 5. Heart valve abnormalities 6. PKD patients are also at increased risk of developing aneurysms in the aorta or cerebral circulations 7. Cysts in the liver that may impair normal function in degrading digestive waste products 8. Cysts in the intestines that can cause diverticulosis 9. Renal Failure 2. Pyelonephritis o Diagnosis: H&P combined with lab results 1. Lab Tests: - UA, Urine culture, blood cultures and CBC 2. Imaging Studies: May be completed for cases that present mor subtly - CT scan and US: May reveal renal structures that are reduced in size or hydronephrosis (edema or retained fluid in the kidneys) o Treatment: Hospitalization to allow treatment with IV antibiotics 1. Medications: - Broad spectrum antibiotics with an aminoglycoside - Bactrim is usually used but contraindicated for patients with sulfa allergies - Fluoroquinolones + Bactrim are also used but contraindicated for children and child-bearing women 2. Other: Increase fluid intake, NSAIDs and narcotic pain meds, Pyridium as a urinary analgesic, and drinking cranberry juice o Complications: 1. Recurrent infections can lead to scarring, CKD, or permanent damage 2. May progress to urosepsis – changes in mental status, tachycardia, tachypnea, hypotension, oliguria, and fever are early signs of urosepsis 3. Glomerulonephritis o Diagnosis: Bases on complete medical history, labs, and physical examination 1. UA may reveal presence of WBCs, RBCs, proteins and casts 2. CBC and differential may reveal ↑WBCs 3. ↑BUN and Creatinine 4. ↓Albumin and complement levels o Treatment: Based on the cause of the disease and symptom management 1. Medications: - Penicillin of infection is actively present - Diuretics & other antihypertensives - Corticosteroids to modulate the inflammatory response - Plasmapheresis may be considered to reduce the inflammatory response 2. Fluid and sodium restriction, protein restriction o Complications: 95% recover if treated early. If untreated or pt is unresponsive to treatment, CKD may develop. Can rapidly progress to renal failure 4. Chronic kidney disease o Diagnosis: 1. Based on consistently elevated creatinine levels and decreased creatinine clearance both of which are impacted by the GFR 2. Persistent presence of protein/albumin in the urine 3. RBCs, WBCs, protein, casts, and glucose in UA 4. Imaging studies and US, CT scan, and renal biopsy can provide further information on kidney status and function o Treatment: Renal replacement therapies o Complications: 8. Discuss the nursing management of: 1. Polycystic kidney disease o Assessments: 1. Vital signs: ↑ temp may indicate infection, ↑ BP from hypertension, ↑ HR from infection or pain 2. Oxygenation: Anemia may impair cellular oxygen exchange which can lower oxygen saturation 3. Daily Weight: ↑ sodium = ↑ water retention 4. Lab Values - H&H: renal disease interferes w/erythropoietin production - Creatinine/BUN: Renal impairment decreases clearance of wastes - Na+ levels: PKD pts may retain Na+, causes ↑BP & fluid overload - K+ levels: PKD pts have ↓ renal clearance of K+ - Ca2+ level: Impaired conversion of Vit D for calcium absorption - PO43- level: inverse Ca2+ and PO43- relationship - UA/Urine cultures: high risk for UTIs, avoid ascension of infection to kidneys o Actions: 1. Diet modification: ↓Na+, ↓ Protein, ↓K+, ↓PO432. Fluid Restriction: Excess fluid not excreted, overload and HF may occur 3. Administer anti-hypertensives: Uncontrolled HTN is a serious complication of PKD 4. Administer antibiotics: To control spread of UTI 5. Administer Pain medications: To manage pain associated with PKD 2. Pyelonephritis o Assessments: 1. Vital Signs: ↑ Temp from infection, ↓BP & ↑HR can result from poorly treated infection 2. Pain: back and flank pain can indicate pyelonephritis 3. Labs: - UA and urine culture: diagnostic tool and to help identify the pathogen - WBC count: reveals leukocytosis and immature cells = infection - Blood cultures: positive = septicemia o Actions: 1. Administer antibiotics as ordered 2. Administer pain meds as ordered 3. Provide adequate hydration PO or Iv as ordered o Teaching: 1. Explain the importance of taking prescribed antibiotics 2. Explain the importance of rest 3. Instruct pt on how to avoid UTIs 4. Explain disease and condition to pt 3. Glomerulonephritis o Assessments: 1. Vital signs: ↑ BP 2. Daily weights: fluid retention 3. I&Os: Fluid retention and sodium retention 4. Measure abdominal girth or extremity size to assess fluid retention 5. Skin condition: edema can cause skin breakdown 6. Dietary intake: Risk for malnourishment because of excessive protein loss in the urine. Protein intake can be limited if BUN is ↑ and there are no signs of malnourishment o Actions: 1. Administer antihypertensives (diuretic or ACE inhibitors) and corticosteroids 2. Maintain low-moderate protein intake 3. Dietary and sodium restriction 4. Chronic kidney disease o Assessments: o Actions: o Teaching: 9. Design a plan of care that includes pharmacological, dietary and lifestyle conservations for patients with renal failure. 10. Describe the indications, management, and complications associated with renal replacement therapies. 11. Describe the indications, management and complications associated with renal transplantation. 12. Describe gerontologic considerations related to upper urinary tract function. 13. Be able to state the purpose, action, adverse, side effects, and usual dosages of the following medications: Miscellaneous Agents • Calcium acetate - • Sevelamer - • - Purpose: For anemia associated with chronic kidney disease Action: Stimulates erythropoiesis, aka the production of RBCs Adverse side effects: Hypertension, HF, MI, thromboembolic events, SJS, transient rashes Usual dosage: SC, 50-100 units/kg 3 times weekly initially, do not exceed hgb 11g/dL for patients on dialysis and 10 g/dL for patients not on dialysis Nephrocaps - • Purpose: To reduce serum phosphate levels in patients with hyperphosphatemia related to ESRD Action: It is a polymer that binds to phosphate in the GI tract, preventing its absorption Adverse side effects: diarrhea, dyspepsia, vomiting, Bleeding GI ulcer, bowel obstruction, esophageal obstruction, colitis, constipation, flatulence, nausea, ulceration Usual dosage: 800-1600 mg 3 times daily with meals Erythropoietin - • Purpose: To control hyperphosphatemia in ESRD Action: Binds to dietary phosphate to form an insoluble calcium phosphate complex, which is excreted in the feces, resulting in decreased serum phosphate levels Adverse side effects: Arrhythmias, bradycardia, hypercalcemia, constipation, nausea, vomiting, headache, tingling Usual dosage: 2001-2668mg with each meal Purpose: In the wasting syndrome in chronic renal failure; uremia; impaired metabolic functions of the kidney and to maintain levels when dietary intake of vitamins is inadequate, or excretion or loss is excessive. Also, highly effective as a stress vitamin. Action: Multivitamin Calcium carbonate - Purpose: For the treatment of hyperphosphatemia in ESRD Action: Replacement of calcium deficiency, control of hyperphosphatemia in ESRD Adverse side effects: Arrhythmias, constipation, nausea, vomiting, headache, tingling, bradycardia, calculi, hypercalciuria • Folic acid - • Purpose: For the prevention and treatment of anemia Action: Required for protein synthesis and RBC function. Stimulates the production of RBCs, WBCs, and platelets. Adverse side effects: rash, irritability, difficulty sleeping, malaise, confusion, fever Usual dosage: 1mg/day initially then 0.5mg maintenance dose Sodium polystyrene sulfonate - • Usual dosage: 1g with each meal, increase to 4-7g as needed Purpose: For mild to moderate hyperkalemia Action: Exchanges sodium ions for potassium ions in the intestine to reduce serum potassium levels Adverse side effects: constipation, fecal impaction, hypocalcemia, hypokalemia, hypomagnesemia, sodium retention, intestinal necrosis, anorexia, ischemic colitis, nausea, vomiting, gastric irritation Usual dosage: 15g 1-4 times daily with water (up to 40g 4 times daily) Benadryl - Purpose: It is estimated that at least 40% of patients with end-stage renal disease suffer from pruritus. Currently, the only approved treatment is an antihistamine, such as Benadryl