Coformer Selection in Pharmaceutical Cocrystal Development
advertisement

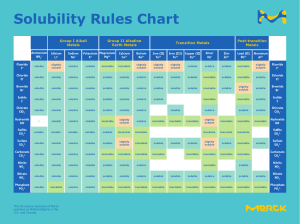
Coformer Selection in Pharmaceutical Cocrystal Development: a Case Study of a Meloxicam Aspirin Cocrystal That Exhibits Enhanced Solubility and Pharmacokinetics MIRANDA L. CHENEY,1,2 DAVID R. WEYNA,1,2 NING SHAN,1 MAZEN HANNA,1 LUKASZ WOJTAS,2 MICHAEL J. ZAWOROTKO2 1 Thar Pharmaceuticals Inc., Tampa, Florida 33612 2 Department of Chemistry, University of South Florida, Tampa, Florida 33620 Received 14 September 2010; revised 3 November 2010; accepted 16 November 2010 Published online 22 December 2010 in Wiley Online Library (wileyonlinelibrary.com). DOI 10.1002/jps.22434 ABSTRACT: Meloxicam is a nonsteroidal anti-inflammatory drug with low aqueous solubility and high permeability. Because of its low solubility under acidic conditions (e.g., pH 1–5), it can take more than 2 h for meloxicam to reach its therapeutic concentration in humans. Although the slow onset of meloxicam does not necessarily impact the current label indications, the slow onset does prevent meloxicam from its potential application for the relief of mild-to-mediumlevel acute pain. Pharmaceutical cocrystallization of meloxicam, which represents a promising approach to generate diverse novel crystal forms, could be used to improve the aqueous solubility and accelerate the onset of action. In this contribution, we describe how a novel method can be used for coformer selection to enable the efficient and effective development of a pharmaceutical cocrystal with desired physicochemical and pharmacokinetic properties. Aspirin was selected as the coformer for meloxicam based upon this alternative route, which combines the supramolecular synthon approach with findings in the previous pharmacological and toxicological studies of meloxicam. The resulting cocrystal of meloxicam and aspirin exhibited superior kinetic solubility and possessed the potential to significantly decrease the time required to reach the human therapeutic concentration compared with the parent drug, meloxicam. © 2010 Wiley-Liss, Inc. and the American Pharmacists Association J Pharm Sci 100:2172–2181, 2011 Keywords: cocrystal; solubility; pharmacokinetics INTRODUCTION Crystalline forms are preferred for oral delivery of active pharmaceutical ingredients (APIs) because crystallization tends to afford highly pure products with superior reproducibility and scalability.1 Typically in drug development, novel API crystal forms, particularly pharmaceutical polymorphs and salts that exhibit diverse physicochemical properties, are identified through screening processes.2,3 More recently, significant efforts have been made in the exploration of pharmaceutical cocrystals as a result of their ability to enhance the physicochemical properties of APIs.4–9 Pharmaceutical cocrystals have been defined as mulCorrespondence to: Ning Shan (Telephone: +1-813-9783980; E-mail: nshan@tharpharma.com), Michael J. Zaworotko (Telephone: +1-813-9743451; E-mail: xtal@usf.edu) Journal of Pharmaceutical Sciences, Vol. 100, 2172–2181 (2011) © 2010 Wiley-Liss, Inc. and the American Pharmacists Association 2172 tiple component crystals in which at least one component is molecular and a solid at room temperature (coformer) and forms a supramolecular synthon with a molecular or ionic API.10 A given API may form cocrystals with a variety of pharmaceutically acceptable and/or approved coformers and such cocrystals can exhibit enhanced solubility,11,12 compressibility,13 stability,14 or bioavailability.15 To date, at least 90 APIs have been targeted for pharmaceutical cocrystallization due, in part, to their undesirable solubility and/or stability and their inherent hydrogen bonding capability.16 For example, lamotrigine, a lowsolubility anticonvulsant drug, was recently targeted for crystal form development in an attempt to enhance the physicochemical and pharmacokinetic (PK) properties.17 In this study, efforts to generate novel materials afforded a variety of crystalline forms including cocrystals, salts, solvates, and hydrates. It was observed that the aqueous solubilities of the JOURNAL OF PHARMACEUTICAL SCIENCES, VOL. 100, NO. 6, MAY 2011 COFORMER SELECTION IN PHARMACEUTICAL COCRYSTAL DEVELOPMENT lamotrigine cocrystals were similar to lamotrigine, whereas the salt of lamotrigine and saccharin showed a substantially higher solubility. In contrast, under acidic conditions designed to mimic the stomach under fasted conditions (pH 1, 37◦ C), the cocrystals exhibited higher solubility compared with the parent lamotrigine, whereas the saccharin salt was the least soluble crystal form. This study exemplifies the ability of different crystal forms to diversify the physicochemical properties of an API. Pharmaceutical cocrystals are also capable of modifying PK properties. As reported in another study, a novel cocrystal of glutaric acid and a sodium channel blocker with low solubility was prepared.15 The cocrystal was evaluated with respect to its stability, particle size, intrinsic dissolution rate, and PK properties. The intrinsic dissolution measurements showed that the cocrystal was 18 times more soluble than the API in water at 37◦ C. Additionally, when the cocrystal was administered to dogs in a single oral dose of 50 mg/kg, the area under the curve (AUC) of the resulting PK profile increased approximately three-fold in comparison with the same dose of pure API. A recent review of the scientific and patent literature indicated that there have been at least 10 pharmaceutical cocrystal case studies with PK details reported to date, many of which support that pharmaceutical cocrystals are a viable option to enhance the clinical performance of a poorly soluble API.17,18 Clearly, pharmaceutical cocrystals represent an opportunity to diversify the number of crystal forms of a given API and in turn fine tune or even customize its physicochemical and PK properties without the formation/breakage of covalent bonds. One of the main challenges in pharmaceutical cocrystal development is the selection of coformers that are compatible with a particular API. A general approach to coformer selection is by “tactless” cocrystal screening, whereby a predetermined library of pharmaceutically acceptable/approved compounds is used to attempt cocrystallization. The lead cocrystal candidate with superior physicochemical and pharmacological properties can then be developed into a dosage form. It has been found recently that the exploitation of supramolecular synthons,19 to a certain extent, can facilitate the cocrystal screening process. Specifically, the “supramolecular synthon approach”10,17 uses crystal engineering20 to analyze the supramolecular arrangements that an API might exhibit. The supramolecular synthon approach is a statistical analysis that utilizes the Cambridge Structural Database (CSD)21 to effectively prioritize coformers for crystal form screening if an appropriate supramolecular heterosynthon can be identified. Supramolecular heterosynthons, typically involving hydrogen bonds between different but complementary groups, are exemplified by carboxylic acid/amide and carboxylic acid/aromatic nitrogen supramolecuDOI 10.1002/jps 2173 lar heterosynthons.10 This approach offers little predictability concerning whether there will be property improvement in the resulting cocrystals, thus recent efforts have been directed to correlating the physicochemical properties of coformers to those of the resulting cocrystals.22 However, to the best of our knowledge, very limited progress has been achieved in this context. As part of our continuous exploration of pharmaceutical cocrystals, we herein report an even more refined approach in the identification of a coformer to generate a pharmaceutical cocrystal with superior physicochemical and pharmacological properties. R Meloxicam (Mobic , Boehringer Ingelheim, Ridgefield, CT, USA) is a nonsteroidal anti-inflammatory drug (NSAID) indicated for the relief of the signs and symptoms of osteoarthritis and rheumatoid arthritis.23 The solubility of meloxicam varies depending upon pH and solvent polarity due to interconversion between ionization states.24 Meloxicam was found to be practically insoluble in water25 and is considered a Class II drug (i.e., low solubility and high permeability) by the Biopharmaceutics Classification System.26 Because of its low solubility under acidic conditions, orally delivered meloxicam exhibits a Tmax (time to reach maximum concentration) of 4–6h in humans,23 and requires approximately 2–3h to reach the therapeutic concentration that enables the onset of action.27 Such a slow onset limits meloxicam from its full potential for the application of mildto-medium-level acute pain relief, which by estimation requires the attainment of the therapeutic concentration within approximately 30 min after dosing. It is noted that an accurate prediction for the time required to reach the therapeutic concentration for acute pain relief is difficult for meloxicam. This estimation was determined based on an evaluation of other NSAIDs for the indication of acute pain relief. To decrease the time to reach the therapeutic concentration and accelerate the onset of action, numerous meloxicam-based formulations have been prepared and evaluated with respect to aqueous solubility.28–31 In spite of all the efforts that were taken, a faster onset oral dosage form of meloxicam remains absent to date. Given the fact that pharmaceutical cocrystals can influence the physicochemical properties of APIs including solubility, a study was designed and performed to explore their effect on improving the solubility and subsequently the onset of action of meloxicam. MATERIALS AND METHODS Materials Meloxicam was purchased from Jai Radhe Sales (Ahmedabad, Gujarat, India) with a purity of 99.64% and was used without further purification. All other JOURNAL OF PHARMACEUTICAL SCIENCES, VOL. 100, NO. 6, MAY 2011 2174 CHENEY ET AL. chemicals were supplied by Sigma–Aldrich (St Louis, MO, USA) and used without further purification. Synthesis of Meloxicam Aspirin Cocrystal Cocrystals of meloxicam and aspirin (1) were successfully prepared by solution,32 slurry,17 and solventdrop grinding33 methods. Solution—23.2 mg (0.0660 mmol) of meloxicam and 11.0 mg (0.611 mmol) of aspirin were dissolved in 8 mL of ethyl acetate at room temperature and left to slowly evaporate. Cocrystals of 1 were obtained (ca. 35% yield) concomitantly with crystals of meloxicam form I and aspirin. Slurry—0.905 g (2.56 mmol) of meloxicam and 0.452 g (2.51 mmol) of aspirin were slurried in 3 mL of tetrahydrofuran (THF) overnight sealed under ambient conditions at approximately 250 rpm. The resulting solid was filtered and washed with THF. 1 was isolated in 96% yield. Solvent-drop grinding—0.182 g (0.517 mmol) of meloxicam was ball-milled (SPEX Mixer/Mill 8000M, Spex Sample Prep, Metuchen, NJ, USA) with 0.0966 g (0.536 mmol) of aspirin and 40 :L of chloroform for 30 min to obtain 1 in approximately 100% conversion, as evidenced by the powder X-ray diffraction (PXRD) and differential scanning calorimetry (DSC) analyses. Crystal Form Characterization Single-Crystal X-Ray Diffraction Single-crystal analysis for 1 was performed on a Bruker-AXS SMART APEX CCD diffractometer (Bruker, Madison, WI, USA) using Cu K" radiation (λ = 1.54178 Å). Data for 1 were collected at 293 K. Lattice parameters were determined from least-squares analysis, and reflection data were integrated using SAINT (Bruker, Madison, WI, USA).34 Structures were solved by direct methods and refined by full matrix least squares based on F2 using the SHELXTL package (Gottingen, Germany).35 All nonhydrogen atoms were refined with anisotropic displacement parameters. All hydrogen atoms bonded to carbon, nitrogen, and oxygen atoms were placed geometrically and refined with an isotropic displacement parameter fixed at 1.2 times Uq of the atoms to which they were attached. Hydrogen atoms bonded to methyl groups were placed geometrically and refined with an isotropic displacement parameter fixed at 1.5 times Uq of the carbon atoms. Powder X-ray Diffraction 1 was characterized using a D-8 Bruker X-ray Powder Diffractometer (Bruker, Madison, WI, USA) using Cu K" radiation (λ = 1.54178 Å), 40 kV, 40 mA. Data were collected at room temperature over an angular range of 3◦ to 40◦ 2θ value in continuous scan mode using a step size of 0.05◦ 2θ value and a scan rate of 5◦ /min. JOURNAL OF PHARMACEUTICAL SCIENCES, VOL. 100, NO. 6, MAY 2011 Calculated PXRD A calculated PXRD diffractogram was generated from the single-crystal structure of 1 using Mercury 2.2 (Cambridge Crystallographic Data Centre, Cambridge, UK) and compared with the pattern obtained for the bulk sample. Differential Scanning Calorimetry Differential Scanning Calorimetry was performed on a PerkinElmer Diamond differential scanning calorimeter (PerkinElmer, Waltham, MA, USA) with a scan range of 25◦ C–280◦ C, scan rate of 10◦ C/min, and nitrogen purge of approximately 30 psi. Fourier-Transform Infrared Spectroscopy Fourier-transform infrared spectroscopy (FTIR) analysis was performed at room temperature on a PerkinElmer Spectrum 100 FTIR spectrometer (PerkinElmer, Waltham, MA, USA) equipped with a solid-state attenuated total reflectance (ATR) accessory. Solubility Study Kinetic solubility was measured for meloxicam and 1 in deionized water at 25◦ C to enable an initial solubility comparison between the API and cocrystal. Subsequently, an additional solubility evaluation of meloxicam and 1 was performed in the pH 7.4 phosphate buffer at 37◦ C to facilitate a fair comparison between the resulting solubility data and the following animal PK study. Before the solubility study, meloxicam and 1 were sieved to achieve a particle size between 53 and 75 :m. The solubility study was conducted by adding increments of a specified amount of solvent to a preweighed amount of meloxicam and 1. Solubility was determined by adding water or pH 7.4 phosphate buffer in 10 mL increments approximately every 10 min with constant agitation until complete dissolution was observed. The experiment was repeated twice to allow for statistical analysis. Animal PK Study Pharmacokinetic studies were conducted using a single-dose oral administration of meloxicam and 1. An intravenous (IV) dose of pure meloxicam (1 mg/kg) was also administered to enable calculation of bioavailability. Five male Sprague–Dawley rats (250–300 g) with preimplanted indwelling jugular vein catheters were used for each crystal form. Meloxicam and 1 were administered at a dosage of 1 mg/kg meloxicam or its equivalent. For oral administrations, a mixture of 5% polyethylene glycol 400 (PEG 400) and 95% methyl cellulose aqueous solutions were used as the vehicle to facilitate oral gavage. Meloxicam and 1 were observed as insoluble in the vehicle. For the IV administration, meloxicam was DOI 10.1002/jps COFORMER SELECTION IN PHARMACEUTICAL COCRYSTAL DEVELOPMENT dosed as a PEG 400/dimethyl sulfoxide solution. After dosing, 0.2 mL of blood was withdrawn at 5, 15, 30, 45, 60, 120, 240, 480, 720, and 1440 min. The blood samples were immediately clotted and centrifuged at room temperature to obtain the rat serum samples, which were subsequently processed and analyzed by liquid chromatography/mass spectrometry according to the literature.36 The PK data were processed by the WinNonlin Professional version 4.0.1 (Pharsight Corporation, West Chester, PA, USA). RESULTS AND DISCUSSION Coformer Selection for Meloxicam The selection of appropriate coformers for pharmaceutical cocrystallization of meloxicam was initialized via the supramolecular synthon approach. Analysis of form I37 of meloxicam (Refcode: SEDZOQ) from a supramolecular synthon approach indicates that meloxicam molecules form supramolecular chains that are sustained by sulfonyl-amide and sulfathiazole–alcohol supramolecular heterosynthons (Fig. 1). The chains are held together by various weak interactions, stacking along the a-axis in a slipped fashion. Thus, for meloxicam cocrystallization, one or all of these supramolecular synthon motifs must be interrupted.38 The CSD analysis examined the reliability of supramolecular heterosynthon versus homosynthon formation between a simple azole (fivemembered ring containing one nitrogen atom and at least one additional heteroatom) and a carboxylic acid, a primary amide, or an alcohol. Only hydrogen bonding interactions were considered for heterosynthon and homosynthon formation.39 A search of the CSD40 for entries that contain both an azole and a carboxylic acid moiety resulted in 450 hits. A closer look at the 450 entries revealed that the carboxylic acid dimer or catemer occurred in 39 entries, or 9% of the time. However, when the 450 entries 2175 were investigated for the presence of the azole–carboxylic acid supramolecular heterosynthon, 102 entries (23%) were identified. Thus, when an azole and carboxylic acid are present in the same crystal structure, the supramolecular heterosynthon is more likely to occur. Because of the potential for meloxicam to generate salts or neutral complexes depending upon the acidity of the complexing moiety, carboxylate–azole interactions were also searched in the CSD. The search result suggested that the carboxylate–azole supramolecular heterosynthon could also be a potential target supramolecular heterosynthon. Interestingly, a search of the CSD indicated that a cocrystal of meloxicam with a coformer containing a primary amide moiety is less likely to occur due to the greater percentage of occurrence of the amide supramolecular homosynthon versus the heterosynthon. In addition, complexation of alcohols with azoles was also studied in the CSD. Collectively comparing the occurrence of the supramolecular homosynthon with the heterosynthon, heterosynthon formation dominates in all cases except for primary amides. The analysis revealed that the azole–carboxylic acid and azole–alcohol supramolecular heterosynthons are persistent. The results of these searches are listed in Table 1. Simultaneously, special attention was drawn to the US Food and Drug Administration Summary Basis of R Approval (SBA) document for Mobic . It was observed that the oral coadministration of meloxicam and aspirin (1000 mg three times a day) to healthy humans would lead to an unexplained increase of AUC and Cmax (maximum plasma concentration) of meloxicam. Therefore, the concomitant administration of meloxicam and aspirin was “not generally recommended,” although no significant adverse effect was reported as a consequence of this coadministration. Realizing that aspirin is an aromatic carboxylic acid, coupled with the CSD analytical results, we speculated that meloxicam and aspirin would form a cocrystal Figure 1. Meloxicam molecules oriented in a chain motif (CSD Ref. code: SEDZOQ). DOI 10.1002/jps JOURNAL OF PHARMACEUTICAL SCIENCES, VOL. 100, NO. 6, MAY 2011 2176 CHENEY ET AL. Table 1. Summary of the CSD Analysis of the Azole Moiety and its Interaction with an Additional Complementary Functional Group Complementary No. of Entries Containing Functional Group Both Moieties Carboxylic acid Carboxylate Alcohol Primary amide a b 450 1708 722 115 Entries that Contain the Supramolecular Heterosynthona Entries that Contain the Supramolecular Homosynthonb Distance Range (Å) 102 (23%) 123 (7%) 296 (41%) 24 (21%) 39 (9%) NA 184 (25%) 64 (56%) 2.50–2.80 2.59–2.90 2.60–3.10 2.80–3.20 The supramolecular heterosynthon is typically an azole hydrogen bonded to a complementary functional group. The supramolecular homosynthon represents the complementary functional group only (i.e., carboxylic acid dimer). using the conventional cocrystallization techniques and that it could increase the in vivo absorption of meloxicam.41 Such an AUC improvement could potentially reduce the time to reach the therapeutic concentration and result in a faster onset. With this in mind, aspirin was selected as the coformer in the study of meloxicam cocrystallization. the C C aromatic region. After cocrystallization, the carbonyl peak of aspirin shifted from its original position of 1751 to 1756 cm−1 . The FTIR peaks associated with the C C stretch on the aromatic ring systems shifted from 1455 cm−1 for aspirin and 1457 cm−1 for meloxicam to 1447 cm−1 in 1. Solid-State Characterization To confirm that 1 is a cocrystal and identify the proton location, three factors were taken into consideration: pKa value [i.e., pKa(base) − pKa(acid) ], C O bond lengths of aspirin, and the C N C angle of the meloxicam sulfathioazole ring. The difference in pKa values between the base and the acid is widely used as a guide for determining whether an experiment will result in the formation of a salt or cocrystal.42–45 It is generally accepted that if pKa < 0, a cocrystal will almost always result, and if the pKa > 3, the result will most likely be a salt. When the pKa falls in between (i.e., 0 < pKa < 3), the product can Cocrystals of meloxicam and aspirin (1) were obtained from grinding, solution, and slurry. Solid-state physical characterizations including X-ray diffraction, DSC, and FTIR were performed on 1. Singlecrystal X-ray diffraction showed that 1 crystallizes in the space group P21 /c. The asymmetric unit of 1 contains one meloxicam molecule and one aspirin molecule. The meloxicam dimer is observed in 1 with the planar meloxicam molecules held into the dimer conformation by OH···S interactions. The supramolecular heterosynthon that sustains the 1:1 complex of meloxicam and aspirin is a two-point recognition OH···N (O···N 2.665(3) Å) and NH···O (N···O 2.856(3) Å) hydrogen-bonded dimer (Scheme 1). As the meloxicam aspirin units extend along the a-axis, corrugated sheets are formed and propagated with a dihedral angle of 73.69◦ (Fig. 2). The corrugated sheets stack with a separation distance of approximately 3.87 Å, producing a herringbone motif. The crystallographic details of 1 are listed in Table 2. To confirm the homogeneity of the powder obtained from grinding, the experimental PXRD profile has been compared with the profile calculated from the single-crystal X-ray diffraction data. As shown in Figure 3, the single-crystal structure represents the solid-state form of the powder from grinding. Additional characterization results of 1 including DSC and FTIR are shown in Figures 4 and 5, respectively. As shown in the DSC curve, 1 exhibited a melting point of 166◦ C, which is between the melting points of aspirin (140◦ C) and meloxicam (254◦ C). No thermal event of dehydration or desolvation was observed throughout the characterization. It was observed that the cocrystal decomposed after heating to a temperature higher than the melting point of 1. A comparison of the FTIR spectra of 1 to meloxicam and aspirin showed distinct shifts in both the carbonyl and JOURNAL OF PHARMACEUTICAL SCIENCES, VOL. 100, NO. 6, MAY 2011 Salt or Cocrystal? Table 2. Crystallographic Data of 1 Empirical formula Formula weight C23 H21 N3 O8 S2 531.55 Temperature Wavelength Crystal system, space group Unit cell dimensions 293(2) K 1.54178 Å Monoclinic, P21 /c a = 6.8026(4) Å; α = 90◦ b = 19.158(1) Å; β = 94.914(4)◦ c = 18.758(1) Å; γ = 90◦ 2435.6(2) A3 4, 1.450 Mg/m3 2.459 mm−1 1104 0.40 × 0.30 × 0.18 mm3 3.30–67.21◦ −8 ≤ h ≤ 8, −22 ≤ k ≤ 22, −22 ≤ l ≤ 21 15496/4238 [R(int) = 0.0502] 67.24◦ ; 97.3% Semiempirical from equivalents 0.6655 and 0.4392 Volume Z, Calculated density Absorption coefficient F(000) Crystal size Theta range for data collection Limiting indices Reflections collected/unique Completeness to theta Absorption correction Maximum and minimum transmission Refinement method Data/restraints/parameters Goodness-of-fit on F2 Final R indices [I > 2sigma(I)] R indices (all data) Largest diff. peak and hole Full-matrix least-squares on F2 4238/0/330 1.020 R1 = 0.0419, wR2 = 0.1043 R1 = 0.0593, wR2 = 0.1143 0.200 and −0.280 eÅ−3 DOI 10.1002/jps COFORMER SELECTION IN PHARMACEUTICAL COCRYSTAL DEVELOPMENT 2177 Figure 2. Primary supramolecular units of meloxicam and aspirin translating along the 21 screw axis. be either species or present partial proton transfer.46 The pKa value of 0.68 for 1 implies cocrystal formation but is not definitive. In addition, the C O bond lengths were measured and found to be 1.311 and 1.212 Å, indicating aspirin is present as the neutral species. The C N C angle of the sulfathiazole ring is also a valuable indicator of protonation where a protonated species will maintain a larger angle (ca. 113◦ )24 in comparison with the neutral species (ca. 109◦ ).37,47 The C N C angle in 1 was 110.20◦ , suggesting that meloxicam is also present as the neutral species. Therefore, it is confirmed from all three considerations that 1 is indeed a cocrystal. Solubility Study A kinetic solubility study of meloxicam and 1 was performed as a preliminary solubility comparison DOI 10.1002/jps between the original API and the resulting cocrystal. It showed that the aqueous solubility of meloxicam at room temperature was approximately 0.001 mg/mL, whereas that of 1 was comparable at ca. 0.0013 mg/mL.48 However, a much more significant solubility difference was observed in conditions designed to mimic a part of the mammalian gastrointestinal tract. In a pH 7.4 phosphate buffer solution at 37◦ C, the solubility of meloxicam was found to be approximately 0.005 mg/mL, whereas that of 1 was found to be approximately 0.22 mg/ mL. It is noted that this solubility study did not use the standard United States Pharmacopeia (USP) apparatus due to the limitations of our inhouse facility. Nevertheless, it is believed that our solubility study produced reasonably comparable results. JOURNAL OF PHARMACEUTICAL SCIENCES, VOL. 100, NO. 6, MAY 2011 2178 CHENEY ET AL. Figure 3. Profiles of (a) experimental PXRD of 1 and (b) calculated PXRD of 1 based on the single-crystal X-ray diffraction data. PK Study Inspired by these promising solubility study results, an animal PK study was conducted. Meloxicam and 1 were each administered as a single-dose suspension in PEG 400 to male Sprague–Dawley rats (n = 5) via oral gavage at an equivalent dose of 1 mg/kg. The PK profiles of meloxicam and 1 are presented in Figure 6. Significant improvement of meloxicam absorption was observed after oral administration of 1, which exhibited an oral bioavailability of 69% compared with 16% for meloxicam. In addition, the plasma concentration correlating to the time to reach the human therapeutic concentration of meloxicam (i.e., 2 h) was found to be 0.51 :g/mL. It was noted that the Cmax of 1 is over four times greater than that of meloxicam, although the Tmax of both 1 and meloxicam is Figure 4. DSC profile of 1. The cocrystal melts at approximately 166◦ C and decomposes at higher temperatures. Thermal events of cocrystal decomposition were omitted for clarity. 4 h. As a result, the concentration of 0.51 :g/mL was achieved only approximately 10 min after oral administration of an equivalent dose of 1. Given that the efficacy of meloxicam is directly associated with its plasma concentration, the onset of action should be much faster for 1 compared with that of meloxicam with the same dose. The PK study result illustrated that 1 is a promising candidate for the development of a meloxicam oral dosage form indicated for rapid mild-to-medium acute pain relief. A summary of the PK parameters are included in Table 3. In light of the precaution outlined in the SBA associated with concomitant administration of meloxicam and aspirin, there is a potential for adverse effects after oral administration of 1. However, no significant adverse effects were observed during our rat PK study. Furthermore, only 7.7 mg of aspirin (i.e., 2% of the regular human adult dose)49 is present in 1 when the largest approved human dose of meloxicam (i.e., 15 mg) is used. 1 was also well tolerated when a single dose with a 10-fold dosage increase (i.e., 10 mg/ kg meloxicam equivalent, equivalent to a 333 mg Table 3. Pharmacokinetic Parameters for 1 and Meloxicam from a Single-Dose Oral Gavage Administration of 1 mg/kg Meloxicam or its Equivalent of 1 Scheme 1. Molecular structure of meloxicam and aspirin. JOURNAL OF PHARMACEUTICAL SCIENCES, VOL. 100, NO. 6, MAY 2011 Cmax (:g/mL) Time to reach therapeutic concentration (min) Tmax (h) Mean residence time (h) AUC0–24h (:g·h/mL) Mean absorption time (h) Bioavailability 1 Meloxicam 2.70 10.6 0.59 120 4.00 24.56 44.14 9.86 69(7)% 4.00 21.80 10.0 7.10 16(4)% DOI 10.1002/jps COFORMER SELECTION IN PHARMACEUTICAL COCRYSTAL DEVELOPMENT 2179 Figure 5. FTIR spectrum of (a) 1, (b) aspirin, and (c) meloxicam. The carbonyl shift is highlighted by a dashed blue line and the C C aromatic shift is highlighted by a dashed orange line. Figure 6. Plasma PK profiles over 24 h for 1 and meloxicam from a 1 mg/kg dose of meloxicam or its equivalent of 1. human dose50 ) was administered in an additional rat PK study, as no significant adverse effect was found in the clinical observations. CONCLUSIONS In summary, we have targeted and prepared a cocrystal of meloxicam and aspirin, 1, which enabled an approximately 12-fold decrease in the time required to reach a concentration of 0.51 :g/mL in rats compared with pure meloxicam at an equivalent dose. Such an improvement could also translate to a faster onset of pain relief in humans.51 For the first time, the selection of a coformer was guided by the combination of the supramolecular synthon approach and findings in the pharmacological and toxicological studies of the parent API, while the intensive cocrystal form DOI 10.1002/jps screening was avoided. Considering that pharmaceutical cocrystallization is frequently used to improve the properties of existing APIs, the selection of coformers could be facilitated by the available pharmacological and toxicological information of the parent APIs. In many cases, drug interactions as well as drug–excipient interactions have been well studied and reported for the parent APIs. Such information could be incorporated in pharmaceutical cocrystal design targeting a specific physicochemical and/or pharmacological property. As demonstrated herein, pharmaceutical cocrystal development becomes more efficient and effective with the strategy of combining the supramolecular synthon approach and the available preclinical/clinical information. Further pharmaceutical cocrystal development is underway with this approach. Crystallographic data of 1 have been deposited with the Cambridge Crystallographic Data Centre (CCDC) as a supplementary publication number CCDC 801314. Copies of the data can be obtained free of charge on application to CCDC via www.ccdc.cam.ac.uk/data request/cif. ACKNOWLEDGMENTS We thank Mr. Raymond Houck for stimulating discussions and valuable input to the project and Dr. William Weiss for his assistances in the PK testing. REFERENCES 1. Allen LV, Popovich NG, Ansel HC. 2005. Ansel’s pharmaceutical dosage forms and drug delivery systems. Baltimore, Maryland: Lippincott Williams and Wilkins. JOURNAL OF PHARMACEUTICAL SCIENCES, VOL. 100, NO. 6, MAY 2011 2180 CHENEY ET AL. 2. Haleblian J, McCrone W. 1969. Pharmaceutical applications of polymorphism. J Pharm Sci 58:911–929. 3. Berge SM, Bighley LD, Monkhous DC. 1977. Pharmaceutical salts. J Pharm Sci 66:1–19. 4. Vishweshwar P, McMahon JA, Bis JA, Zaworotko MJ. 2006. Pharmaceutical co-crystals. J Pharm Sci 95:499–516. 5. Schultheiss N, Newman A. 2009. Pharmaceutical cocrystals and their physicochemical properties. Cryst Growth Des 9:2950–2967. 6. Shan N, Zaworotko MJ. 2008. The role of cocrystals in pharmaceutical science. Drug Discovery Today 13:440–446. 7. Aakeröy CB, Forbes S, Desper J. 2009. Using cocrystals to systematically modulate aqueous solubility and melting behavior of an anticancer drug. J Am Chem Soc 131:17048–17049. 8. Childs SL, Chyall LJ, Dunlap JT, Smolenskaya VN, Stahly BC, Stahly GP. 2004. Crystal engineering approach to forming cocrystals of amine hydrochlorides with organic acids. Molecular complexes of fluoxetine hydrochloride with benzoic, succinic, and fumaric acids. J Am Chem Soc 126:13335–13342. 9. Remenar JF, Morissette SL, Peterson ML, Moulton B, MacPhee JM, Guzman HR, Almarsson Ö. 2003. Crystal engineering of novel cocrystals of a triazole drug with 1,4dicarboxylic acids. J Am Chem Soc 125:8456–8457. 10. Almarsson Ö, Zaworotko MJ. 2004. Crystal engineering of the composition of pharmaceutical phases. Do pharmaceutical cocrystals represent a new path to improve medicines? Chem Commun 1889–1896. 11. Remenar JF, Peterson ML, Stephens PW, Zhang Z, Zimenkov Y, Hickey MB. 2007. Celecoxib:Nicotinamide dissociation: using excipients to capture the cocrystal’s potential. Mol Pharm 4:386–400. 12. Good DJ, Rodriguez-Hornedo N. 2009. Solubility advantage of pharmaceutical cocrystals. Cryst Growth Des 9:2252– 2264. 13. Karki S, Friščić T, Fabian L, Laity PR, Day GM, Jones W. 2009. Improving mechanical properties of crystalline solids by cocrystal formation: new compressible forms of paracetamol. Adv Mater 21:3905-3909. 14. Trask AV, Motherwell WDS, Jones W. 2005. Pharmaceutical cocrystallization: engineering a remedy for caffeine hydration. Cryst Growth Des 5:1013–1021. 15. McNamara DP, Childs SL, Giordano J, Iarriccio A, Cassidy J, Shet MS, Mannion R, O’Donnell E, Park A. 2006. Use of a glutaric acid cocrystal to improve oral bioavailability of a low solubility API. Pharm Res 23:1888–1897. 16. Lipinski CA. 2000. Drug-like properties and the causes of poor solubility and poor permeability. J Pharmacol Toxicol Methods 44:235–249. 17. Cheney ML, Shan N, Healey ER, Hanna M, Wojtas L, Zaworotko MJ, Sava V, Song S, Sanchez-Ramos JR. 2010. Effects of crystal form on solubility and pharmacokinetics: a crystal engineering case study of lamotrigine. Cryst Growth Des 10:394–405. 18. Shan N, Zaworotko M. 2010. Polymorphic crystal forms and cocrystals in drug delivery (crystal engineering). In Burger’s Medicinal Chemistry and Drug Discovery, p 187–218. 19. Desiraju GR. 1995. Supramolecular synthons in crystal engineering - a new organic-synthesis. Angewandte Chemie 34:2311–2327. 20. Desiraju GR. 1989. Crystal Eng. 21. Allen FH. 2002. The Cambridge Structural Database: a quarter of a million crystal structures and rising. Acta Crystallogr Sect B-Struct Sci 58:380–388. 22. Stanton MK, Bak A. 2008. Physicochemical properties of pharmaceutical co-crystals: a case study of ten AMG 517 cocrystals. Cryst Growth Des 8:3856–3862. R 23. Mobic FDA Summary Basis of Approval (NDA # 020938). JOURNAL OF PHARMACEUTICAL SCIENCES, VOL. 100, NO. 6, MAY 2011 24. Luger P, Daneck K, Engel W, Trummlitz G, Wagner K. 1996. Structure and physicochemical properties of meloxicam, a new NSAID. Eur J Pharm Sci 4:175–187. 25. Ghorab MM, Abdel-Salam HM, El-Sayad MA, Mekhel MM. 2004. Tablet formulation containing meloxicam and betacyclodextrin: mechanical characterization and bioavailability evaluation. AAPS PharmSciTech 5 :59. 26. Takagi T, Ramachandran C, Bermejo M, Yamashita S, Yu LX, Amidon GL. 2006. A provisional biopharmaceutical classification of the top 200 oral drug products in the United States, Great Britain, Spain, and Japan. Mol Pharm 3:631–643. 27. Auvinet B, Ziller R, Appelboom T, Velicitat P. 1995. Comparison of the onset and intensity of action of intramuscular meloxicam and oral meloxicam in patients with acute sciatica. Clin Ther 17:1078–1090. 28. Han HK, Choi HK. 2007. Improving absorption of meloxicam via salt formation with ethanolamines. Eur J Pharm Biopharm 65:99–103. 29. Ki HM, Choi HK. 2007. The effect of meloxicam/ethanolamine salt formation on percutaneous absorption of meloxicam. Arch Pharm Res 30:215–221. 30. Mezei T, Mesterhazy N, Bako T, Porcs-Makkay M, Gyula S, Balazs V. 2009. Manufacture of high-purity meloxicam via its novel potassium salt monohydrate. Organic Process Res Dev 13:567–572. 31. Rao KP, Saran TSV, Shivappa NN, Shulamite A, Sachin K, Hiremath VA. 2009. Studies on meloxicam microcrystals for improving drug therapy. Indian J Pharm Sci 71:167–168. 32. Childs SL, Rodriguez-Hornedo N, Reddy LS, Jayasankar A, Maheshwari C, McCausland L, Shipplett R, Stahly BC. 2008. Screening strategies based on solubility and solution composition generate pharmaceutically acceptable cocrystals of carbamazepine. Cryst Eng Comm 10:856–864. 33. Friščić T, Jones W. 2009. Recent advances in understanding the mechanism of cocrystal formation via grinding Cryst Growth Des 9:1621–1637. 34. BrukerSMART, SAINT-Plus, SADABS, XP and SHELXTL. 1997. Madison, Wisconsin. 35. Sheldrick GM. 1997. SHELXTL. Gottingen, Germany: University of Gottingen. 36. Castel-Branco MM, Almeida AM, Falcao AC, Macedo TA, Caramona MM, Lopez FG. 2001. Lamotrigine analysis in blood and brain by high-performance liquid chromatography. J Chromatogr B 755:119–127. 37. Fabiola GF, Pattabhi V, Manjunatha SG, Rao GV, Nagarajan K. 1998. 4-Hydroxy-2-methyl-N-(5-methyl-1,3-thiazol-2-yl)2H-1,2-benzothiazine-3-carboxamide 1,1-dioxide. Acta Crystallogr Sect C 54:2001–2003. 38. Childs SL, Hardcastle KI. 2007. Cocrystals of piroxicam with carboxylic acids. Cryst Growth Des 7:1291–1304. 39. The range for the hydrogen bond was determined for each search by manual examination of the entries at or near the bottom of the bell curve of the histogram. All entries outside of the defined distance range were excluded. 40. CSD version 5.31, November 2009 release including May 2010 update. Search parameters: Organics only, 3D coordinates determined, R < 7.5%. 41. The AUC increase of meloxicam by its coadministration with aspirin could also be the result of GI physiological effects. Further investigation is required to validate this hypothesis. 42. Bhogala BR, Basavoju S, Nangia A. 2005. Tape and layer structures in cocrystals of some di- and tricarboxylic acids with 4,4’bipyridines and isonicotinamide. Cryst Eng Comm 7:551–562. 43. Delori A, Suresh E, Pedireddi VR. 2008. pKa-directed hostguest assemblies: rational analysis of molecular adducts of 2,4-diamino-6-methyl-1,3,5-triazine with various aliphatic dicarboxylic acids. Chem-Eur J 14:6967–6977. DOI 10.1002/jps COFORMER SELECTION IN PHARMACEUTICAL COCRYSTAL DEVELOPMENT 44. Mohamed S, Tocher DA, Vickers M, Karamertzanis PG, Price SL. 2009. Salts or cocrystals? A new series of crystal structures formed from simple pyridines and carboxylic acids. Cryst Growth Des 9:2881–2889. 45. Stahl PH, Wermuth CG. 2002. Handbook of pharmaceutical salts: Properties, selection, and use. Zurich, Switzerland: WILEY-VCH. 46. Childs SL, Stahly GP, Park A. 2007. The salt-cocrystal continuum: the influence of crystal structure on ionization state. Mol Pharm 4:323–338. 47. Cheney ML, Weyna DR, Shan N, Hanna M, Wojtas L, Zaworotko MJ. 2010. Supramolecular architectures of meloxi- DOI 10.1002/jps 48. 49. 50. 51. 2181 cam carboxylic acid cocrystals, a crystal engineering case study. Cryst Growth Des 10:4401–4413. All concentration values in this manuscript refer to meloxicam equivalent concentrations. The regular human dose of 325 mg was used for calculation. For further information, see FDA Orange Book. US FDA CDER. 2005. Guidance for Industry: Estimating the maximum safe starting dose in initial clinical trials for therapeutics in adult healthy volunteers. Busch U, Schmid J, Heinzel G, Schmaus H, Baierl J, Huber C, Roth W. 1998. Pharmacokinetics of meloxicam in animals and the relevance to humans. Drug Metab Dispos 26:576–584. JOURNAL OF PHARMACEUTICAL SCIENCES, VOL. 100, NO. 6, MAY 2011