CPD
Page 60
Ankylosing spondylitis
multiple choice
questionnaire
CONTINUING
PROFESSIONAL
DEVELOPMENT
Page 61
Read Patience Fordjour’s
practice profile on
respiratory infection
Page 62
Guidelines on
how to write a
practice profile
Ankylosing spondylitis: diagnosis
and management
NS724 Bond D (2013) Ankylosing spondylitis: diagnosis and management.
Nursing Standard. 28, 16-18, 52-59. Date of submission: April 23 2013; date of acceptance: October 18 2013.
Aims and intended learning outcomes
Abstract
This article provides an overview of ankylosing spondylitis, including
signs and symptoms, diagnosis and management. The article focuses
on the difficulties and delays associated with diagnosing this chronic
inflammatory disease and developments in diagnostic criteria. Changes
in the management of patients with the disease are also discussed,
particularly in light of anti-tumour necrosis factor therapy.
Author
Deborah Bond
Lead biologics specialist nurse, Royal National Hospital for Rheumatic
Diseases, Bath.
Correspondence to: Deborah.Bond@rnhrd.nhs.uk
Keywords
Ankylosing spondylitis, anti-TNF therapy, back and joint pain, diagnostic
criteria, inflammatory disease, long-term conditions
Review
All articles are subject to external double-blind peer review and checked
for plagiarism using automated software.
Online
Guidelines on writing for publication are available at
www.nursing-standard.co.uk. For related articles visit the archive and
search using the keywords above.
This article discusses the management of
patients with ankylosing spondylitis in the
context of modern therapy options. After
reading this article and completing the time out
activities you should be able to:
Describe ankylosing spondylitis, including
the signs and symptoms.
Explore the effect of ankylosing spondylitis
on patients’ lives.
Understand the diagnostic criteria
for ankylosing spondylitis and issues
surrounding delay in diagnosis.
Discuss the pharmacological and
non-pharmacological treatment of patients
with this long-term condition.
Introduction
Ankylosing spondylitis is a chronic
inflammatory disease primarily affecting
the spine and sacroiliac joints. It is the most
common of a group of diseases known as
spondyloarthritides, which are rheumatic
diseases with common clinical symptoms. The
disease is estimated to affect up to 1% of the
general population (Baraliakos et al 2011).
However, prevalence varies depending on race,
with 0.04-0.06% of non-Caucasians affected
by the disease compared with 0.1-1.4% of
Caucasians (Boonen and van der Heijde 2004).
Variation in prevalence is thought to occur
because of the presence of the human leucocyte
antigen (HLA)-B27 gene within different
populations. HLA-B27 is a protein on the
surface of white blood cells. The effect of the
gene is unclear (Bowness 2002), but over 90%
of people with ankylosing spondylitis have the
52Downloaded
decemberfrom
18 ::rcnpublishing.com
vol 28 no 16-18by
:: 2013
© NURSING
STANDARD
/ RCN
${individualUser.displayName} on Jun 22, 2014.
For personal
use only. No
other PUBLISHING
uses without permission.
Copyright © 2014 RCN Publishing Ltd. All rights reserved.
and social activities, and increasing the risk of
depression (National Ankylosing Spondylitis
Society (NASS) 2010a). Therefore, early disease
management is essential to prevent damage
and disability. In a survey of people with
ankylosing spondylitis, 72% of respondents
were in employment, however only 38% of
these individuals received advice or help on
coping with symptoms of the condition while at
work (NASS 2010b). Pain, fatigue and physical
limitations were identified as the main factors
affecting a person’s ability to work.
Symptoms
There are a variety of symptoms of ankylosing
spondylitis, and these include:
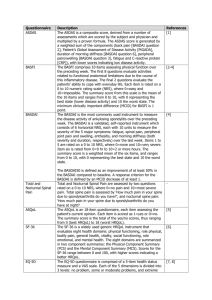
FIGURE 1
Ankylosed vertebrae (bamboo spine)
SCIENCE PHOTO LIBRARY
HLA-B27 gene, although only one in 15 people
who carry it will develop the disease (MiceliRichard and Dougados 2004). This suggests
that environmental factors such as stress might
also influence the development of the disease.
Ankylosing spondylitis is more common in
men than in women, although the reason for
this is unknown. However, estimates vary:
Gladman (2003) reported a 9:1 male to female
ratio of the disease, Rudwaleit et al (2004)
stated that it affects twice as many men as
women, and McKenna (2010) suggested a 5:1
male to female ratio of ankylosing spondylitis.
The onset of ankylosing spondylitis is
typically between 30 and 50 years, although
it can occur earlier (Gossec and Dougados
2004). Like all inflammatory diseases, there
are periods of flare and dormancy that make
it difficult to distinguish inflammatory back
pain from mechanical back pain (Table 1). As a
result, there may be a delay in diagnosis of up to
ten years (Khan 2003).
Ankylosing spondylitis causes pain and
stiffness in the back, eventually resulting in
joint damage and fusion predominantly of the
sacroiliac joints, and ankylosing of the vertebrae
leading to a classic bamboo spine (Figure 1),
although this does not always occur. It can affect
the rest of the axial skeleton (shoulders and
hips), leading to reduced range of motion and
pain. Some individuals develop joint destruction
and may require total joint replacement. This
can occur at a much earlier age than usual in
individuals with ankylosing spondylitis. The
disease can also cause peripheral symptoms
affecting the knees, hands and feet, which can
appear similar to rheumatoid arthritis, with
patients experiencing pain and swelling. This
can lead to misdiagnoses, thereby delaying
appropriate treatment (Khan 2003).
There are several extra-articular
(non-skeletal) features that may be associated
with ankylosing spondylitis, for example acute
anterior uveitis affects between 25% and 40% of
people with ankylosing spondylitis (Gossec and
Dougados 2004). Acute anterior uveitis or iritis,
characterised by inflammation of the iris, may be
the first indication that a person has ankylosing
spondylitis. This condition needs to be treated
as an emergency to prevent long-term problems
such as glaucoma or reduced vision (Khan 2003).
Cardiovascular manifestations such as valve
disorders and aortic incompetence may be more
common in those who are HLA-B27 positive and
can worsen with age (Bakland et al 2011).
Ankylosing spondylitis can have a significant
effect on patients’ lives, affecting work, family
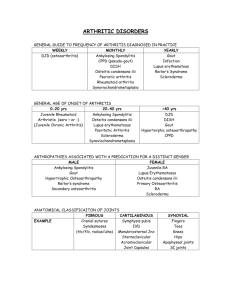
TABLE 1
Comparison of inflammatory and mechanical back pain
Inflammatory back pain
Mechanical back pain
Onset in those under 40 years.
Onset at any age.
Insidious onset.
More likely to be sudden onset.
Symptoms improve with exercise.
Symptoms often become worse with
exercise.
No improvement in symptoms
with rest.
Symptoms often improve with rest.
Pain at night, with improvement
on getting up.
Pain at night is less likely.
(Adapted from Sieper et al 2009a, Harris et al 2012)
© NURSING
/ RCNbyPUBLISHING
:: vol
nouses
16-18
:: 2013
53
Downloaded
fromSTANDARD
rcnpublishing.com
${individualUser.displayName} on Jun 22, 2014. For december
personal use18
only.
No28
other
without
permission.
Copyright © 2014 RCN Publishing Ltd. All rights reserved.
CPD inflammatory conditions
Early morning stiffness – can take from a few
minutes to many hours to ease, and it can
take up to two or more hours for a person
to get going in the morning. Sitting down
for any length of time can cause the spine to
stiffen up again (Khan 2003).
Pain – tends to develop gradually over weeks
or months rather than days, and occurs
mainly in the spine. Pain is worse at rest and
is eased by exercise (Sieper et al 2009a).
Enthesitis – is pain and swelling where
ligaments and tendons attach to bone.
A common site is the heel and pain on
walking can be significant, particularly in
the morning when the heel has been rested
overnight (Gossec and Dougados 2004).
Fatigue – constant exhaustion not relieved
by sleep (Mengshoel 2010).
Feverishness or night sweats – are commonly
reported symptoms in people with
ankylosing spondylitis. However, these
symptoms are also associated with other
inflammatory and autoimmune disorders
and there is a lack of evidence about the
cause of feverishness or night sweats (Mold
et al 2012).
Shortness of breath – as the disease
progresses it can cause fusion of the
thoracic vertebrae and also the attached
ribs, limiting expansion of the chest. If
the spine becomes fully ankylosed it can
lead to a stoop, which will also limit chest
expansion (Khan 2003).
Flares – individuals can go through periods
where ankylosing spondylitis is dormant
and then flares up. Cooksey et al (2009)
suggested that 70% of people with the
disease experience flares in any one week.
Complete time out activity 1
BOX 1
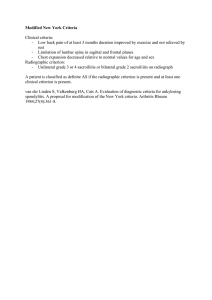
Modified New York criteria for diagnosis of ankylosing spondylitis
Clinical criteria:
Low back pain for more than three months, which is improved by exercise
and not relieved by rest.
Limitation of lumbar spine motion in both the sagittal and frontal planes.
Limitation of chest expansion relative to normal values for age and sex.
Radiological criterion:
Sacroiliitis grade 2 or above. Grade 2 is bilateral sacroiliitis, grade 3-4 can
be unilateral or bilateral depending on the degree of fusion.
Diagnosis:
Definite ankylosing spondylitis if radiological criterion is present, including
at least one clinical criterion.
Probable ankylosing spondylitis if three clinical criteria are present, or if the
radiological criterion is present, but there are no clinical signs of disease.
(van der Linden et al 1984)
In individuals where ankylosing spondylitis
starts at a young age, there may be increased
comorbidities such as cardiovascular disease,
amyloidosis and infection, and complications
of a fused spine such as spinal fractures,
resulting in increased mortality (Bakland
et al 2011). According to Peters et al (2010),
the risk of myocardial infarction is almost
four times higher in people with the disease
compared with the general population – this
is similar to other inflammatory disorders.
It is, therefore, important that people
with the disease are monitored carefully
and that developing comorbidities such as
hypertension or hypercholesterolaemia are
managed appropriately.
Diagnosis
A better understanding of ankylosing
spondylitis and developments in diagnostic
techniques have led to changes in the diagnostic
criteria for the disease. Initially, ankylosing
spondylitis was thought to be a variation of
rheumatoid arthritis, however it was not until
the advent of diagnostic tests such as that for
the HLA-B27 gene that ankylosing spondylitis
was recognised as being different from
rheumatoid arthritis. The modified New York
criteria can be used to diagnose ankylosing
spondylitis (van der Linden et al 1984) (Box 1).
One of the difficulties associated with using
the modified New York criteria is that it can
take up to five years before there is radiological
evidence of sacroiliitis, by which time there
might be significant joint destruction. Use
of more advanced imaging technology such
as magnetic resonance imaging reduces the
time to diagnosis, with images showing
inflammatory changes years before bony
damage occurs. In 2009, the Assessment
of SpondyloArthritis International Society
(ASAS) published a consensus statement on
the classification of axial spondyloarthritis
(Rudwaleit et al 2009) (Figure 2).
Assessment
There is an internationally recognised set of
outcome measures for use with patients who
have ankylosing spondylitis known as the
Bath indices. These were designed to provide
comprehensive information relating to an
individual’s disease and the effect on his or her
life and health (Irons and Jeffries 2004). The
indices were devised in the 1990s and include
(Irons and Jeffries 2004):
54
decemberfrom
18 ::rcnpublishing.com
vol 28 no 16-18by:: ${individualUser.displayName}
2013
© NURSING
STANDARD
/ RCN
Downloaded
on Jun 22, 2014.
For personal
use only. No
other PUBLISHING
uses without permission.
Copyright © 2014 RCN Publishing Ltd. All rights reserved.
Bath ankylosing spondylitis disease activity
index (BASDAI).
Bath ankylosing spondylitis functional index
(BASFI).
Bath ankylosing spondylitis global score
(BAS-G).
Bath ankylosing spondylitis metrology index
(BASMI).
The Bath indices are patient-reported outcome
measures and use visual analogue scales
(VASs). These scales are designed to gauge
an individual’s level of agreement with a
statement. Scores range from 0-10, with 0
being good and 10 being bad. The use of VASs
has limitations in that patients’ experiences,
perceptions and life issues can affect how
they perceive their disease and scores can be
influenced by other events that may act as
additional stressors. It is, therefore, possible
that the patient’s physical, objective score,
such as inflammatory markers and metrology,
indicate improvement, while subjective
measures, such as pain, may worsen (Kievit
et al 2010). The Bath indices, in particular
the BASDAI, are used as part of the screening
process to assess the patient’s suitability for
anti-tumour necrosis factor (TNF) therapy
(Irons and Jeffries 2004).
Complete time out activity 2
Alternatives to the Bath indices have been
suggested, such as the ankylosing spondylitis
disease activity score (ASDAS) (Gossec and
Dougados 2004). This scoring system attempts
to make assessment a more objective process,
with the use of inflammatory markers such as
C-reactive protein or erythrocyte sedimentation
rate. However, it is important to note that as
many as 50% of individuals with ankylosing
spondylitis will not have raised inflammatory
markers, thereby reducing the reliability of the
ASDAS (Gossec and Dougados 2004).
Treatment
For many patients, ankylosing spondylitis
remains a mild disease that has minimal effects
on their activities of daily living and can be
self-managed.
Non-pharmacological interventions
Exercise Daily exercise might be helpful in the
treatment of ankylosing spondylitis, and should
include stretching and strengthening activities.
Dagfinrud et al (2008) found sufficient
evidence to support the conclusion that any
form of exercise is better than no exercise in
the management of ankylosing spondylitis, and
that supervised group therapy is preferable to
group physiotherapy alone.
Patients can access NHS run courses that
include education on various topics, including
exercise, treatments and self-management
of ankylosing spondylitis. These courses are
available on an inpatient or outpatient basis
and some run on a one-day-a-week basis, while
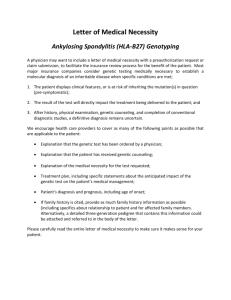
FIGURE 2
Assessment in SpondyloArthritis International Society classification criteria for axial
spondyloarthritis (in patients with chronic back pain and age at onset under 45 years)
Sacroiliitis on imaging plus one or
more axial spondyloarthritis feature
or
Sacroiliitis on imaging:
Active (acute) inflammation on magnetic
resonance imaging highly suggestive
of sacroiliitis associated with axial
spondyloarthritis.
Or:
Definite radiographic sacroiliitis according
to the modified New York criteria.
(Adapted from Rudwaleit et al 2009, Sieper et al 2009b)
Positive test for HLA-B27 gene plus two or
more other axial spondyloarthritis features
Axial spondyloarthritis features:
Inflammatory back pain.
Arthritis.
Enthesitis (heel).
Uveitis.
Dactylitis.
Psoriasis.
Crohn’s disease or diagnosis of colitis.
Good response to non-steroidal
anti-inflammatory drugs.
Family history of axial spondyloarthritis.
Positive test for HLA-B27 gene.
Elevated C-reactive protein levels.
1 What effect might
the symptoms of
ankylosing spondylitis
have on a 21-year-old
man? How might these
symptoms affect this
person’s self-esteem
and confidence, and
what could you do to
help improve his quality
of life?
2 Read the personal
accounts of living with
ankylosing spondylitis
using the following NASS
web address: tinyurl.
com/mch48cp. Reflect
on what a diagnosis of
ankylosing spondylitis
might mean for patients
and their families. What
support might family
members require and
what resources could
you direct them to?
© NURSING
/ RCNbyPUBLISHING
:: vol
nouses
16-18
:: 2013
55
Downloaded
fromSTANDARD
rcnpublishing.com
${individualUser.displayName} on Jun 22, 2014. For december
personal use18
only.
No28
other
without
permission.
Copyright © 2014 RCN Publishing Ltd. All rights reserved.
CPD inflammatory conditions
others are an intensive two-week programme.
Education An understanding of ankylosing
spondylitis and the various aspects of
management is one of the most important
aspects of treatment. Patients who are engaged
with and participate in the management of
their disease are more likely to have better
outcomes than those who do not actively
participate in disease management (NASS
2012). Individuals’ understanding of the
disease and learning will vary, therefore
education should be tailored to the individual.
However, there is some basic information
that all patients will need to be given about
the disease, including signs and symptoms,
short and long-term effects, treatment options,
and general health issues such as smoking
reduction and cessation, weight management
and limiting alcohol intake. Individuals should
also be provided with information that they
can give to employers, schools and family
members (NASS 2010a).
Symptom control
If possible, management of ankylosing
spondylitis should involve the multidisciplinary
team. For many patients, pain, physical
limitations and fatigue are the main symptoms
that need to be addressed (Heiberg et al 2011).
Pain and physical limitations are managed
most effectively through a combination of
medication and exercise (NASS 2010a).
Physical limitations might also be addressed
with physiotherapy, occupational therapy
and medication.
Fatigue, although significant, is frequently
ignored by healthcare professionals (Davies
et al 2013, Hammoudeh et al 2013). Physical,
mental and activity-related fatigue, and loss
of motivation may be common in people with
ankylosing spondylitis (Missaoui and Revel
2006). Fatigue can also be associated with the
disease, drug treatment or other conditions
such as depression. It is not unique to
ankylosing spondylitis and is common in other
inflammatory disorders such as rheumatoid
arthritis (Husted et al 2009, National
Rheumatoid Arthritis Society 2010).
There appears to be a link between fatigue
and factors such as pain, sleep and activity.
If sleep patterns can be improved, pain and
fatigue will also be improved (Mengshoel
2010). Mengshoel (2010) distinguished
between tiredness associated with daily life
such as work and sport, and fatigue associated
with illness. She described fatigue as an
unnatural whole body tiredness that leads to
feelings of exhaustion, helplessness and pain.
Pain at night is significant because it leads to
disturbed sleep. Lack of sleep affects function
and the individual’s ability to cope with fatigue
(Farren et al 2013). Hammoudeh et al (2013)
stated that pain at night occurs in 62-63%
of people with ankylosing spondylitis and
Mengshoel (2010) suggested that fatigue levels
increase about 24 hours after pain peaks. Advice
for patients should be centred on managing
factors that worsen fatigue as shown in Box 2.
There is some debate as to whether
medications lessen fatigue, particularly
in relation to the use of non-steroidal
anti-inflammatory drugs (NSAIDs)
(Dernis-Labous et al 2003). There is no
definitive answer to this and pharmacological
management of patients’ fatigue appears to
depend on individual response. There have
been more encouraging reports of fatigue
reduction with anti-TNF therapies, with
BOX 2
Advice for patients on managing factors that
worsen fatigue
Good sleep hygiene:
Avoid stimulants before bed.
Ensure hot baths are taken at least one hour
or more before bed to allow body temperature
to drop.
Ensure the bedroom is not too hot and
bedclothes are not too heavy. A good supportive
mattress may also be helpful to ensure comfort.
Diet and fluids:
Consume a healthy and balanced diet and remain
hydrated with non-alcoholic fluids.
Exercise:
Ensure exercise is regular, varied and manageable,
including exercises designed to improve muscle
strength, spinal flexibility and stability.
Pacing:
Understand and apply pacing to break activities
into small more manageable parts.
Plan ahead. If an individual knows he or she has
a busy day, the advice would be to take it easy
before and afterwards.
Identify activity patterns through the use of
diaries and activity records. This can help to
pace and plan activity.
Pain management:
Use non-pharmacological interventions, such
as exercise.
Use pharmacological interventions, such as
non-steroidal anti-inflammatory drugs and
anti-tumour necrosis factor therapy.
(National Rheumatoid Arthritis Society 2010)
56
decemberfrom
18 ::rcnpublishing.com
vol 28 no 16-18by:: 2013
© NURSING
STANDARD
/ RCN
Downloaded
${individualUser.displayName} on Jun 22, 2014.
For personal
use only. No
other PUBLISHING
uses without permission.
Copyright © 2014 RCN Publishing Ltd. All rights reserved.
positive responses to etanercept (Hammoudeh
et al 2013), golimumab (Deodhar et al 2010)
and adalimumab (Revicki et al 2008).
Complete time out activity 3
Pharmacological interventions
For the majority of patients, symptoms of
ankylosing spondylitis will be managed using
a variety of treatment options. At all times, the
prescriber needs to be aware of the risk and
benefit of particular drugs, as well as any other
comorbidities the individual may have. This
is especially important in people who have
long-term health conditions that may require
lifelong use of medications. This article focuses
on the use of pharmacological treatments
aimed at controlling disease activity; however,
many patients will require other treatments
such as analgesics, antidepressants, hypnotics
and antispasmodics.
Non-steroidal anti-inflammatory drugs
NSAIDs can be effective in reducing the pain
and inflammation associated with ankylosing
spondylitis and rheumatoid arthritis (Escalas
et al 2010). Poddubnyy et al (2012) and Kroon
et al (2012) published evidence suggesting
that NSAIDs have a disease-modifying action
in ankylosing spondylitis and may limit the
development of ankylosis. NSAIDs should
be taken on a regular basis if the individual
is experiencing prolonged, active and
symptomatic disease (Braun et al 2011).
For most patients, the use of NSAIDs such as
naproxen or ibuprofen is preferable because they
are associated with a low risk of cardiovascular
problems (National Institute for Health and
Care Excellence (NICE) 2009). It is important
to be aware that there are safety risks associated
with NSAIDs and they should only be prescribed
when the patient’s full medical history is known.
These drugs should be avoided where there
is a history of cardiovascular, renal or gastric
problems. It is recommended that an appropriate
proton pump inhibitor is prescribed at the same
time as the NSAID especially when, as with
ankylosing spondylitis, patients may be receiving
treatment for many years (NICE 2009).
With regular use of NSAIDs, effectiveness can
diminish and many patients will have tried three
or more NSAIDs over the years to maintain a
reduction in pain and stiffness (Dougados et al
2002). NSAIDs in combination with analgesics
tend to be more effective than either treatment
alone (NICE 2009, Ong et al 2010).
Disease-modifying anti-rheumatic drugs
Disease-modifying anti-rheumatic drugs are
used regularly in rheumatology to treat a
number of inflammatory conditions, however
they seem to have little or no effect on patients
with axial ankylosing spondylitis (Zochling
et al 2006). Methotrexate or sulfasalazine
may be used in the treatment of patients with
peripheral problems such as pain and swelling
of the joints of the hands and feet (Zochling
et al 2006).
Biologic disease-modifying anti-rheumatic
drugs The development of biologic therapies
such as anti-TNF drugs have resulted in
advances in the treatment of ankylosing
spondylitis and the limitation of disease
progression potentially leading to reduced
disease activity. Evidence suggests that
anti-TNFs are the most effective of the
biologics in treating ankylosing spondylitis
(Zochling et al 2006).
Before an individual can be considered
for anti-TNF therapy, active disease as
defined by NICE (2008) must be established.
This includes a diagnosis of ankylosing
spondylitis using the modified New York
criteria, previous NSAID use, and appropriate
BASDAI and pain scores of 4 or above on the
VAS. The BASDAI and pain scores have to
be repeated three months apart in line with
NICE requirements.
The patient should undergo a thorough
assessment to identify actual and potential risk
factors before treatment. The Royal College
of Nursing (RCN) (2009) provides useful
information on assessing, managing and
monitoring biologic therapies for inflammatory
arthritis. Relevant investigations such as chest
X-ray also need to be completed.
Complete time out activity 4
Several biologic therapies are used in
rheumatology, including anti-TNF agents,
B cell depletors, interleukin-6 inhibitors
and T cell modulators. However, only
anti-TNF therapy appears to have an effect
in the management of ankylosing spondylitis
(Singh et al 2011). The main anti-TNF
therapies are adalimumab, etanercept,
golimumab and infliximab. Certolizumab
pegol is also awaiting licensing for this
indication. These therapies are grouped
according to their mode of action, which is
to block the action of a protein or eliminate
a cell. In this case, the purpose of these
therapies is to block the action of TNF
proteins. Soluble receptors (cepts) compete
with TNF-receptors to reduce the amount
of TNF attaching to cell receptors
(Abbas and Lichtman 2006).
Complete time out activity 5
3 Reflect on a
time when you were
extremely tired, perhaps
after a long shift. How
did it make you feel and
how did you cope with
it? How do you think you
would cope if you had
to deal with extreme
fatigue on a daily basis?
4 Read the RCN (2009)
document on assessing,
managing and monitoring
biologic therapies for
inflammatory arthritis.
Look, in particular, at
the section on screening.
Why is screening so
important? You may wish
to discuss your thoughts
with a colleague.
5 Access the most
recent copy of the British
National Formulary and
list some of the side
effects associated with
anti-TNF therapies.
© NURSING
/ RCNbyPUBLISHING
:: vol
nouses
16-18
:: 2013
57
Downloaded
fromSTANDARD
rcnpublishing.com
${individualUser.displayName} on Jun 22, 2014. For december
personal use18
only.
No28
other
without
permission.
Copyright © 2014 RCN Publishing Ltd. All rights reserved.
CPD inflammatory conditions
Monitoring
6 Consider the
implications for
individuals undergoing
long-term treatment
with immunosuppressant
therapies. How would
you help to prevent the
risk of infection. Provide
the rationale for your
suggestions.
7 Now that you have
completed the article,
you might like to write
a practice profile.
Guidelines to help you
are on page 62.
Once on a treatment regimen, patients
need to be monitored to ensure the safety
and effectiveness of any drugs. They should
be advised to have regular blood tests to
identify any adverse events that may occur
as a result of immunosuppression, such
as increased infections (Ding et al 2010).
There also needs to be evidence that the
treatment has reduced disease activity
as identified by NICE (2008). This means
that the BASDAI and pain scores have to
drop by 2cm or 50% from the original
VAS scores before treatment, and this has
to be reassessed every three months. If there
is any indication of initial non-response
or later failure, the scores should be
repeated six weeks later, and if there has
been no improvement the treatment should
be stopped.
Although NICE (2008) does not
recommend switching to an alternate
anti-TNF drug, there is some evidence to
show that individuals might respond to an
alternative anti-TNF because the drugs are
slightly structurally different from each other
(Lie et al 2011, Glintborg et al 2013).
Complete time out activity 6
Conclusion
Ankylosing spondylitis can cause severe pain,
fatigue and disability, thereby affecting all
aspects of an individual’s life. Identifying
the disease early is crucial to limit the physical
and psychological effects on patients.
Involvement of the multidisciplinary team and
local support groups can help the individual to
maintain a normal life with minimal disruption.
It has been shown that regular exercise can
reduce pain and maintain mobility. This,
combined with appropriate pain management,
can reduce the effect of fatigue and the incidence
of depression. NSAIDs and analgesics are
the mainstay of treatment for many people and
may limit disease progression. However, for
those with more advanced or debilitating disease,
newer biologics have been developed and are
associated with reduced pain and disability NS
Complete time out activity 7
References
Abbas AK, Lichtman AH (2006)
Basic Immunology Functions
and Disorders of the Immune
System. Second edition. Saunders
Philadelphia PA.
Bakland G, Gran JT, Nossent JC
(2011) Increased mortality in
ankylosing spondylitis is related
to disease activity. Annals of
the Rheumatic Diseases. 70, 11,
1921-1925.
Baraliakos X, Listing J, Fritz C et al
(2011) Persistent clinical efficacy
and safety of infliximab
in ankylosing spondylitis after
8 years-early clinical response
predicts long-term outcome.
Rheumatology. 50, 9, 1690-1699.
Boonen A, van der Heijde D (2004)
Epidemiology and socioeconomic
impact. In Dougados M,
van der Heijde D (Eds) Ankylosing
Spondylitis. Health Press, Oxford,
24-31.
Bowness P (2002) HLA B27 in
health and disease: a double-edged
sword? Rheumatology. 41, 8,
857-868.
Braun J, van den Berg R, Baraliakos X
et al (2011) 2010 update of the
ASAS/EULAR recommendations for
the management of ankylosing
spondylitis. Annals of the Rheumatic
Diseases. 70, 6, 896-904.
Cooksey R, Brophy S, Gravenor MB,
Brooks CJ, Burrows CL, Siebert S
(2009) Frequency and
characteristics of disease flares in
ankylosing spondylitis.
Rheumatology. 49, 5, 929-932.
Dagfinrud H, Kvien TK, Hagen KB
(2008) Physiotherapy interventions
for ankylosing spondylitis. Cochrane
Database of Systematic Reviews.
Issue 1, CD002822.
Davies H, Brophy S, Dennis M,
Cooksey R, Irvine E, Siebert S
(2013) Patient perspectives of
managing fatigue in ankylosing
spondylitis, and views on potential
interventions: a qualitative study.
BMC Musculoskeletal Disorders.
14, 163.
Deodhar A, Braun J, Inman RD
et al (2010) Golimumab reduces
sleep disturbance in patients with
active ankylosing spondylitis:
results from a randomized,
placebo-controlled trial. Arthritis
Care and Research. 62, 9, 1266-1271.
Dernis-Labous E, Messow M,
Dougados M (2003) Assessment
of fatigue in the management of
patients with ankylosing spondylitis.
Rheumatology. 42, 12, 1523-1528.
Ding T, Ledingham J, Luqmani R
et al (2010) BSR and BHPR
rheumatoid arthritis guidelines on
safety of anti-TNF therapies.
Rheumatology. 49, 11, 2217-2219.
Dougados M, Dijkmans B, Khan M,
Maksymowych W, van der Linden SJ,
Brandt J (2002) Conventional
treatments for ankylosing
spondylitis. Annals of the Rheumatic
Diseases. 61, Suppl 3, iii40-iii50.
Escalas C, Trijau S, Dougados M
(2010) Evaluation of the treatment
effect of NSAIDs/TNF blockers
according to different domains in
ankylosing spondylitis: results of a
meta-analysis. Rheumatology. 49, 7,
1317-1325.
58
decemberfrom
18 ::rcnpublishing.com
vol 28 no 16-18by:: ${individualUser.displayName}
2013
© NURSING
STANDARD
/ RCN
Downloaded
on Jun 22, 2014.
For personal
use only. No
other PUBLISHING
uses without permission.
Copyright © 2014 RCN Publishing Ltd. All rights reserved.
Farren W, Goodacre L, Stigant M
(2013) Fatigue in ankylosing
spondylitis: causes, consequences
and self-management.
Musculoskeletal Care. 11, 1, 39-50.
Gladman D (2003) Established
criteria for disease controlling drugs
in ankylosing spondylitis. Annals
of the Rheumatic Diseases. 62, 9,
793-794.
Glintborg B, Østergaard M,
Krogh NS et al (2013) Clinical
response, drug survival and
predictors thereof in 432 ankylosing
spondylitis patients after switching
tumour necrosis factor D inhibitor
therapy: results from the Danish
nationwide DANBIO registry. Annals
of the Rheumatic Diseases. 72, 7,
1149-1155.
Gossec L, Dougados M (2004)
Clinical features. In Dougados M,
van der Heijde D (Eds) Ankylosing
Spondylitis. Health Press, Oxford,
32-45.
Hammoudeh M, Zack DJ, Wenzhi L,
Stewart VM, Koenig AS (2013)
Associations between
inflammation, nocturnal back
pain and fatigue in ankylosing
spondylitis and improvements
with etanercept therapy. Journal
of International Medical Research.
41, 5, 1150-1159.
Harris C, Gurden S, Martindale J,
Jeffries C (2012) Differentiating
Inflammatory and Mechanical
Back Pain: Challenge Your Decision
Making. www.astretch.co.uk/
M208%20IBP%20Module%20
Booklet.pdf (Last accessed:
December 5 2013.)
Heiberg T, Lie E, van der Heijde D,
Kvien TK (2011) Sleep problems
are of higher priority for
improvement for patients with
ankylosing spondylitis than for
patients with other inflammatory
arthropathies. Annals of the
Rheumatic Diseases. 70, 5, 872-873.
Husted JA, Tom BD, Schentag CT,
Farewell VT, Gladman DD (2009)
Clinical and epidemiological
research extended report:
occurrence and correlates of fatigue
in psoriatic arthritis. Annals of
the Rheumatic Diseases. 68, 10,
1553-1558.
Irons K, Jeffries C (2004) The
Bath Indices. Outcome Measures
for Use with Ankylosing Spondylitis
Patients. NASS, Surrey.
Khan MA (2003) Clinical features
of ankylosing spondylitis. In
Hochberg MC, Silman AJ, Smolen S,
Weinblatt ME, Weisman MH (Eds)
Rheumatology. Third edition.
Ankylosing Spondylitis Excerpta
Medica Publications, London,
1161-1181.
Kievit W, Hendrikx J,
Stalmeier PF, van de Laar MA,
Van Riel PL, Adang EM (2010)
The relationship between change
in subjective outcome and change
in disease: a potential paradox.
Quality of Life Research. 19, 7,
985-994.
Kroon F, Landewé R, Dougados M,
van der Heijde D (2012) Continuous
NSAID use reverts the effects of
inflammation on radiographic
progression in patients with
ankylosing spondylitis. Annals of
the Rheumatic Diseases. 71, 10,
1623-1629.
Lie E, van der Heijde D, Uhlig T
et al (2011) Effectiveness of
switching between TNF inhibitors
in ankylosing spondylitis: data
from the NOR-DMARD register.
Annals of the Rheumatic Diseases.
70, 1, 157-163.
McKenna F (2010)
Spondyloarthritis. Arthritis
Research UK, Chesterfield.
Mengshoel AM (2010) Life
strain-related tiredness and
illness-related fatigue in
individuals with ankylosing
spondylitis. Arthritis Care and
Research. 62, 9, 1272-1277.
Miceli-Richard C, Dougados M
(2004) Genetic aspects. In
Dougados M, van der Heijde D (Eds)
Ankylosing Spondylitis. Health
Press, Oxford, 17-23.
Missaoui B, Revel M (2006)
Fatigue in ankylosing spondylitis.
Annales de Readaptation
et de medicine Physique. 49, 6,
389-391.
Mold JW, Holtzclaw BJ,
McCarthy L (2012) Night sweats:
a systematic review of the
literature. Journal of the
American Board of Family
Medicine. 25, 6, 878-893.
National Ankylosing Spondylitis
Society (2010a) Looking Ahead.
Best Practice for the Care of People
with Ankylosing Spondylitis (AS).
NASS, Surrey.
National Ankylosing Spondylitis
Society (2010b) Working with
Ankylosing Spondylitis. NASS,
Surrey.
National Ankylosing Spondylitis
Society (2012) Ankylosing
Spondylitis (AS), Guidebook,
Answers and Practical Advice.
NASS, Surrey.
National Institute for Health
and Care Excellence (2008)
Adalimumab, Etanercept and
Infliximab for Ankylosing
Spondylitis. Technical appraisal
No. 143. NICE, London.
National Institute for Health
and Care Excellence (2009)
Rheumatoid Arthritis. Clinical
guideline No. 79. NICE, London.
National Rheumatoid Arthritis
Society (2010) Fatigue –
Beyond Tiredness. www.nras.
org.uk/includes/documents/
cm_docs/2010/f/fatigue_beyond_
tiredness_aug_10.pdf (Last
accessed: December 5 2013.)
Ong CK, Seymour RA, Lirk P,
Merry AF (2010) Combining
paracetamol (acetaminophen)
with nonsteroidal antiinflammatory
drugs: a qualitative systematic
review of analgesic efficacy
for acute postoperative pain.
Anesthesia and Analgesia. 110, 4,
1170-1179.
Peters MJ, Visman I, Nielen MM
et al (2010) Ankylosing spondylitis:
a risk factor for myocardial
infarction? Annals of the
Rheumatic Diseases. 69, 3,
579-581.
Poddubnyy D, Rudwaleit M,
Haibel H et al (2012) Effect of
non-steroidal anti-inflammatory
drugs on radiographic spinal
progression in patients with axial
spondyloarthritis: results from
the German Spondyloarthritis
Inception Cohort. Annals of the
Rheumatic Diseases. 71, 10,
1616-1622.
Revicki DA, Luo MP,
Wordsworth P et al (2008)
Adalimumab reduces pain,
fatigue, and stiffness in patients
with ankylosing spondylitis:
results from the adalimumab
trial evaluating long-term
safety and efficacy for
ankylosing spondylitis (ATLAS).
Journal of Rheumaology. 35, 7,
1346-1353.
Royal College of Nursing (2009)
Assessing, Managing and
Monitoring Biologic Therapies for
Inflammatory Arthritis: Guidance
for Rheumatology Practitioners.
RCN, London.
Rudwaleit M, Listing J, Brandt J,
Braun J, Sieper J (2004) Prediction
of a major clinical response
(BASDAI 50) to tumour necrosis
factor D blockers in ankylosing
spondylitis. Annals of the
Rheumatic Diseases. 63, 6,
665-670.
Rudwaleit M, van der Heijde D,
Landewé R et al (2009) The
development of Assessment
of SpondyloAarthritis
International Society
classification criteria for axial
spondyloarthritis (part II):
validation and final selection.
Annals of the Rheumatic Diseases.
68, 6, 777-783.
Sieper J, van der Heijde D,
Landewé R et al (2009a) New
criteria for inflammatory back
pain in patients with chronic back
pain: a real patient exercise by
experts from the Assessment of
SpondyloArthritis International
Society (ASAS). Annals of the
Rheumatic Diseases. 68, 6,
784-788.
Sieper J, Rudwaleit M,
Baraliakos X et al 2009b)
The assessment of
SpondyloArthritis International
Society (ASAS) Handbook: a guide
to assess spondyloarthritis. Annals
of the Rheumatic Diseases. 68,
Suppl 2, ii1-44.
Singh JA, Wells GA,
Christensen R et al (2011)
Adverse effects of biologics: a
network meta-analysis and
Cochrane overview. Cochrane
Database of Systematic Reviews.
Issue 2, CD008794.
van der Linden S, Valkenburg HA,
Cats A (1984) Evaluation of
diagnostic criteria for ankylosing
spondylitis. A proposal for
modification of the New York
criteria. Arthritis and Rheumatism.
27, 4, 361-368.
Zochling J, van der Heijde D,
Burgos-Vargas R et al (2006)
ASAS/EULAR recommendations
for the management of ankylosing
spondylitis. Annals of the
Rheumatic Diseases. 65, 4,
442-452.
© NURSING
/ RCNbyPUBLISHING
:: vol
nouses
16-18
:: 2013
59
Downloaded
fromSTANDARD
rcnpublishing.com
${individualUser.displayName} on Jun 22, 2014. For december
personal use18
only.
No28
other
without
permission.
Copyright © 2014 RCN Publishing Ltd. All rights reserved.