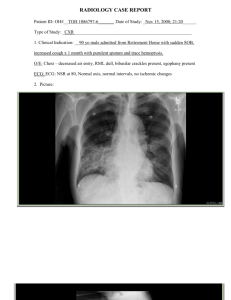
OVERVIEW Pathophysiology Oxygenation Hypoxemia ( O2 in blood) Hypoxia ( O2 in cells) Anoxia (Total absence of O2 in cells) By: Sir Ronie TERMS • • • • Cells- basic unit of life Tissues-made up of combined cells Organs-made up of combined tissues Organic Hypoxia- S/sx will occur once there is an organ damage Functions Respiratory System ▪ O2 (in) → ABN: O2 input → Hypoxemia → Hypoxia→ Anoxia→ Cellular Death ▪ Co2 (out) Cellular death Factors that affect the inhalation: Systems Involved ✓ Respiratory ✓ Cardiovascular ✓ Hematology Vital Organs Involved ✓ ✓ ✓ ✓ Heart Lungs Kidneys Brain 1. OBSTRUCTIVE DISORDER -there is an airway obstruction due to: Mucus Bronchoconstriction Foreign objects ❖ ✓ ✓ ✓ Management: Mucus- DOC: mucolytics Bronchoconstriction- DOC: bronchodilators Foreign objects- Heimlich maneuver ✓ LAST RESORT: INTUBATION - is the act of inserting a tube into a bodily orifice to remove or add fluids or air. artificial airways Uses: *These organs reacts/gives signal once hypoxia occurs • Endotracheal Tube (ET tube) - *Therefore s/sx of hypoxia are organic or in cellular origin • Tracheostomy tube - • is a flexible plastic tube that is placed through the nose or mouth into the trachea, or windpipe, to help a patient breathe. is a curved tube that is inserted into a tracheostomy stoma. Ventilation support VENTILATION (inhalation and exhalation) The exchange of air between the lungs and the atmosphere so that oxygen can be exchanged for carbon dioxide in the alveoli (the tiny air sacs in the lungs). help keeps oxygen flowing throughout the body by pushing air into the lungs. 2 TYPES: 1. 2. “First Tx of choice is to GET RID OF THE C/A” 2. INFECTIOUS DISORDER -there is an airway infection due to: C/A: Bacteria, Virus, Fungi ❖ Management: Once c/a enters The body it causes “Viruses are self-limiting (does not replicate) therefore it can be managed by rest and increase fluid intake” Manual- Bag Valve Mask (BVM/Ambu Bag) Machine- Mechanical ventilator Bacteria – antibiotics (anti-infectives) Virus – antivirals (severe); key for viruses is the viral load Fungi – rare (indicates pt. is immunocompromised); antifungal *Get rid of the C/A or COI (chain of infection) leads to Inflammation ❖ Management: (anti-inflammatory) NSAIDs-mild to moderate inflammation Corticosteroids-moderate to severe Obstruction ❖ Management: ❖ Mucus- DOC: mucolytics ❖ Bronchoconstriction- DOC: bronchodilators OVERVIEW 3. TRAUMA • • Pain bleeding A. Penetration (e.g., chest injury) B. Rib fracture C. Blunt Trauma (Internal bleeding) ❖ Management Pain- (Subjective) analgesics - Mild-moderate (NSAIDs) - Moderate-Severe (Opioids) Lung collapse Atelectasis PAIN SCALE 1-3: Mild -distractions (guided imagery), acupressure, deep breathing 4-6: Moderate 7-10: Severe Bleeding – Thoracostomy + 3-way Bottle System - Thoracostomy (opening of the thorax at the mid-axillary 4th-5th intercostal area) BOTTLES & FUNCTIONS Bottle A: Drainage Bottle B: Maintain negative pressure Bottle C: Suction Tx of Atelectasis “Dili niya ipagawas tanang hangin inig exhale naa syay ✓ perform intubation ipabilin para kadtong nabilin nga hangin mao toy matulod ✓ connect pt. to mechanical ventilator pag inhale ug balik sa mechanical ventilator” ✓ PEEP (Positive End Expiratory Pressure) -setting of mechanical ventilators done by respiratory therapist in collab with the doctor). -Function: to reverse atelectasis COPD (Chronic Obstructive Pulmonary Disorder) Nature of the D/O: • chronic • progressive • irreversible - Commonly in geriatric patients- Types of COPD Obstructive Disorders 1. Chronic Bronchitis 2. Chronic emphysema Others: (eliminated in the COPD category) • • • • • Bronchiectasis ➔ Eliminated due to early death/mortality caused by: malnutrition, tuberculosis, and poor hospitalization ➔ Lifespan: 37 y.o. (Brunner & Suddarth); 30-40 y.o. (Philippines) Asthma ➔ reversible Cystic Fibrosis ➔ Eliminated because it is a multisystem d/o Acute bronchitis ➔ Reversible and sudden/explosive Acute emphysema ➔ Reversible and sudden/explosive Infectious Disorders Causative agents 1. Bacteria ➔ Upper respi ➔ Lower respi Junction: trachea/windpipe Leading cause of UPPER RESPI INFECTION: ▪ GABHS (Group A Beta Hemolytic Streptococcus) ➢ Can lead to heart disease ➢ Common in pedia ➢ Recurrent sore throat in pedia can lead to heart disease “Antibiotics➢ Can become systemic usually taken for ➢ Causes inflammation of endocardium (where heart valves located) 7 days” ➢ Results to heart valve damage RANITIDINE (Zantac) ➢ Pinnacle of Heart damage is Heart Failure (HF) H2 Receptor Blocker → decreases production of ❖ Tx: Penicillin/Pen G (4-6 weeks) hydrochloric acid Leading cause of LOWER RESPI INFECTION: ▪ PNEUMONIA ➢ Given with antibiotics to prevent gastric upset. Bacteria: PTB, Hemophilus, Staphylococcus, Acinetobacter ❖ Tx: → PTB – RIPES (RIPE -oral; taken 6 AM before meals for easy absorption;) (S-IM); 6 mos → Hemophilus: Betalactams (Cefuroxime), Azithromycin – taken for 3days → Staphylococcus: Methicillin, Vancomycin → Acinetobacter: if (+) in gram staining Abbreviations: __ pc → post cebum “after meals” __ ac → ante cebum “before meals” -multidrug resistant bacteria; mechanical ventilation assistive pneumonia -Meropenem, ipanemem 2. Virus ▪ ▪ Adenovirus: common colds Coronavirus: C/A: SARS COV 2 ❖ Tx: →acyclovir →ganciclovir →atazanavir →tocilizumab (1 shot is worth 6k to 10k, 3x a day) →remdesivir (1 dose is worth 50k to 70k, good for 1 week) 3. Fungi (Fungal Pneumonia) ❖ Tx: →Amphotericin B Traumatic Disorders PENETRATIONS: Pneumothorax - air in thoracic cavity; Example: Stabbed wound Hemothorax – blood in thoracic cavity; Example: Rib Fracture (flail chest) Hydrothorax – water in thoracic cavity; Example: Penetrated under water There will be a sucking motion because of the negative pressure. COMPLICATIONS: • Pleural Effusion increase water in pleural - Not a primary disease - A secondary condition to trauma, lung cancer and TB ❖ Mgt: →Thoracentesis - done at the back depending on the location as seen on X-ray. - at lower costal margin Given to COVID pts. Management of COPD: 1. Bronchodilators ➔ Sympathetic drugs (SNS) → Receptors: Beta 1 (heart) and 2(lungs) o Function of B2: dilation of smooth muscle o Effect of bronchodilator to B1: HR CAUTION!!! Do not give propranolol together with bronchodilator or to patients with COPD because it reverses the effect of the bronchodilators causing Bronchoconstriction to B2 (lungs). Be careful in giving to patient with ▪ ▪ HR: FACTORS THAT COULD HR Hx of ANXIETY (mild, moderate, severe, panic) -because it can cause palpitation CYSTIC FIBROSIS - Altered anion (chloride) transport -Genetic: Autosomal recessive -Defect in chromosome #7 (“syetec fibrosis”) -Sticky semen: Exocrine glands 1.LUNGS mucus plugging → prepare suction promote breast feeding: r/f infection → PNEUMONIA 2. SKIN (sweat glands) Two types: eccrine (panit), apocrine (oily) sticky sweat and odorous 12 yo greatest fear in acne and body odor (hygienic prob) Babies are obligatory nose breather -SIDS (sudden infant death syndrome) -Sternocleidomastoid & trapezius muscle for neck movement -11th cranial nerve (spinal or accessory) -head sag phenomena (first month) Altered anion -Found at the right side of the periodic table -Negatively charge Major extracellular anion CHLORIDE → Normal: 95-105 meq/L Major intracellular anion SODIUM → Normal: 135-145 meq/L 3.PANCREAS (endo-exocrine gland) secretes (Amylase-Lipase-Trypsin enzymes) Once fat is not absorbed: • failure to thrive • STEATORRHEA (FAT IN STOOLS) • Vitamin deficiency (water-soluble taken OD) K+: 3.5-5.5 meq/L (major intracellular cation Na+: 135-145 meq/L (major intracellular anion) Extracellular (2 compartments) -blood -3rd space Fat soluble: • • • • A-ABN: xeropthalmia (nigh blindness) D-for Ca+ absorption. ABN: bone deformities (rickets) EK-blood coagulation 4.LIVER +GALLBLADDER 5.MALE REPRODUCTIVE GLANDS- impotence, infertility 1tsp (5 mL) Genetic: cause of altered transport Autosomal Recessive- 25 % sa anak Gregor Mendel – father of modern genetics 23RD PAIR or 45th and 46th chromosome- there is problem in sex (reproductive issue) If there is prob in 22 pairs: autosomes daghan ng prob (physical ug sulod) Autodigestion phenomena -inflammation of pancreas (acute pancreatitis) gi digest sa pancreas iyang cells ky dili kagawas ang ALT -bile mo stock up sa gall bladder→cholelithiasis -RUQ pain sharp and colicky pain radiating to the right nipple, shoulder or scapula (Kehr’s Sign) Whipple resection (pancreaticoduodenectomy) -surgical removal of the head of the pancreas. -if gallstones motapot sa sphincter of oddii Major cause of death to patient with pancreatitis is Hemorhagic shock because of bleeding Hallmark sign of pancreatitissevere, excruciating pain, unrelieved by vomiting (increase pH→ Metabolic alkalosis: will end up to COMA), food, and antacids. Located in the Epigastric area. Bluish discoloration of the umbilicus because of bleeding (Cullen’s sign) Bluish discoloration of the Flank area/retroperitoneal area (Grey-Turner Sign) Management: 1.Bronchodilators 2.Mucolytics 3.Antitussives 4.O2-High flow 10-15 LPM during exacerbation non-rebreather mask (It has the highest accommodation of o2) 5.VIOKASE (Pancrealipase) artificial pancreatic enzyme. Effective when there is relief in steatorrhea. Becoz the fat in stool is already absorbed using the pancrealipase. 6.IVTT- ADEK Promising Mgt. 1.Pneumonectomy-removal of the entire lung 2.lobectomy-removal of a certain lobe of the lung -needs chest tube for drainage. POST-OP Positioning: LU-PA Lobectomy-unaffected (side lying) Pneumonectomy-Affected (side lying) To allow lung expansion Diagnostic Tests: Sweat chloride test-To determine if there is chloride in the sweat Chest X-ray- if there is fluid in lungs Serum Lipase- will increase if there is presence of pancreatitis (to rule out presence of pancreatitis) -normal: 0-160 u/L UTZ- to diagnose gallstones O2 Nasal prongs-1-3 LPM Face mask- 4-8 LPM Venturi mask- it has its own gauge COPD for client’s safety below 10 LPM Partial rebreather – 8-10 LPM Non-rebreather- 10-15 LPM LAST RESORT: INTUBATION Bronchiectasis (Chronic dilatation of the bronchioles) Unknown cause→ multifactorial Infectious Environment genetics -Damaged cilia Hallmark Sign: Layering of Sputum (different colors and character) Rusty: damaged bronchial wall White: sputum Foamy Yellow green: Infection Dx: bronchial CT scan Mgt: • • • CPT Mucolytics + Bronchodilators (given first before CPT) Antibiotic Prophylaxis LUNG RESECTION 1.wedge resection-pie 2.segmentectomy -half/segment of a lobe 3.lobectomy 4.pneumonectomy Before surgery: ✓ ✓ ✓ Informed consent CP clearance Withhold→ blood thinner, anticoagulants After surgery: ✓ Positioning ✓ A-B-C A • • • • Ascertain/check if the ET tube is in place using X-ray. Co2 detector Auscultate breath sound Suction at bedside Principle of suctioning: ✓ ✓ ✓ hyperoxygenate before and after suctioning 2 minutes hyperventilate using mechanical ventilator suction- during withdrawal only -circular motion -intermittent -10-15 secs PNSS use to clean the suction B • Connect to mechanical ventilator • Connect to BVM C • Check capillary refill • Check distal pulse • Check temp of the extremities (cold-poikilothermia) • Check color of the extremities • Check urine output- N: 30 mL/hr • Check vital signs : hypo,tachy,tachy Asthma -reversible hyperresponsiveness and acute inflammation of the airways -inflammation of the airways Factors: • Anaphylaxis/allergy (foods, meds, dust, dander, bee stings, weather) • Hereditary • Exercise induced • Petrichor-induced asthma (singaw sa kalsada) Inflammation - mucus production - bronchoconstriction S/sx: ✓ ✓ ✓ ✓ ✓ ✓ cough (with or without secretions) air hunger dyspnea, S.O.B. decrease LOC wheezing Cyanosis ▪ Central-late ▪ Peripheral- early Status Asthmaticus -severe form of asthma with frequent episodes Dx test: • CBC → WBC→ eosinophil: ELEVATED (eosinophilia) Eosinophil→ 1%-2% WBC: 4,000-11,000 Histamine mediator/anti-histamine 5 WBC: NEBML-neutrophils,eosinophil,basophil,monocyte,Lymphocytes • • X-ray PFM (Peak Flow Meter): measures the force of expiration Green - Yellow red Green-normal Yellow-mild to moderate asthma Red-severe Incentive Spirometry-promotes deep breathing DOC-bronchodilator Histamine-primary chemical mediator Leukotriene-secondary chemical mediator; 3x most potent than histamine Severe: - Epinephrine (long acting) -theophylline (+)toxicity (palpitation, chest pain) aminohylline - Quick acting (albuterol) Mild-moderate: - Ipratropium - Corticosteroids-hydrocortisone - Theophylline - Montelukast, Zafirlukast (Leukotriene Modifiers)- given 9 pm-extreme drowsiness Hora Somni-hours of sleep - Antihistamine Sedating: hangover effect (cetirizine) Non-sedating: Loratadine (Alerta) Infectious Disorders PTB(Pulmonary Tuberculosis Bacteria) C/A: Tubercle Bacilli (Mycobacterium Tubercle) MOT: Airborne Droplet Form of Pneumonia: bronchopneumonia → IP: 2-10 weeks Complication: Pulmonary Fibrosis Pleural Effusion Process with (COI-Chain of Infection): 1. Infected Host -full blown -Active disease 2. Portal of Exit 3. -cough -sneeze C/A 4. Susceptible Host 5. -inhale: PO entry -IP: 2-10 weeks -Bronchopneumonia (cough, fever (low grade), fatigue, may not have hemoptysis WBC activation ▪ Neutrophils Phagocytosis ▪ Antibodies ▪ macrophages 6. 7. 8. 9. Granuloma Formation (scarring) Normal disappears in 6 months In the middle of scar there is Ghon tubercle dormant phase active phase (makagawas ang infection) -reinfection -immunosuppression (WOF: WBC) 10. ulceration of the granuloma 11. pulmonary fibrosis (hardening of the lungs) 12. TB transmitted to bloodstream: Miliary TB (Extrapulmonary TB) Extrapulmonary TB once it gets to the: • Brain-encephalitis • CNS covering- meningitis • Bones- Pott’s Disease (causes degeneration and demineralization) -diet high in calcium (e.g., dairy, seaweed) • Liver-liver failure (EARLIEST SIGN: Jaundice) • Kidneys- renal failure • Adrenal cortex- Addison’s Disease • Testicles – • Lymphnodes-lymphadenopathy HIV/AIDS • <200 cells/mm³ (WBC count) • Target CD4 (helper cells) • Common to sodomy (“luvey”) because blood is the fastest way of transport. Leading cause of Mortality: United States: PCP • Pneumocystic • Carinii • Pneumonia Philippines • PTB S/sx: C-cough; 3 weeks; productive H-hemoptysis; blood-tinged sputum; sudden onset A-afternoon fever (low grade fever: 37.6-37.9) N-night sweats A-anorexia leading to weight loss (unintentional) K-kapoy (Fatigue secondary to hypoxia) Diagnostic tests: Confirmatory exams: 1.X-ray -detects presence of granuloma 2 Sputum exam- use to confirm active PTB • AFB (Acid Fast Bacilli) • GeneXpert test: AFB + Detects Drug Resistance Rifampicin-daghan ng na immune ani Nursing Consideration: • 2 sputums exams -Collected at 6AM & 7AM consecutively -Container: must be sterile Instruct patient to: ➔ Gargle with water (salt water, warm water) to minimize the contamination of the sample normal flora of the mouth. ➔ Do not use mouthwash because it contains antiseptics (chlorhexidine). ➔ do not spit the surface saliva ➔ deep breath 3x and cough forcefully -once obtained ihatod ang sample sa lab. -2 hours life span Brain threshold sa hypoxia- lethargy Earliest s/sx- restlessness, confusion Wernicke’s korsakoff’s psychosis Huntington’s Management of PTB 1.Mgt. Program: NTCP (National Tuberculosis Control Program) 2. Therapy: DOTS (Directly-Observed Treatment Shortcourse) or “Tutok Gamutan” • given for 6 mos : ✓ 2 mos: intensive phase (R-I-P-E) + S [IM—MDR TB] ✓ 4 mos: Maintenance Phase (R-I-P/R-I) S-only given if pt is already MDR TB R-rifampicin (R) → S/E (expected): Red orange urine discoloration → A/E (report): abdominal pain, jaundice, oliguria → this indicates hepatorenal failure hepatorenal failure (liver & kidney affected): • Kidney Function test (indicates if the kidney is functioning well) → blood specimen ✓ Blood Urea Nitrogen (BUN) from protein→ n: 10-20 mg/dL ✓ Creatinine – most specific indicator → n: 0.6-1.2 mg/dL Caloric Intake: Carbs: 1gm x 4 Protein: 1gm x 4 Fats: 1 gm x 9 Duodenum-pepsin Amino acid→ nutrient→waste: ammonia (NH4)→ liver→urea→ kidney→urine • Liver function Test: Glutamic Acid (waste): ✓ SGPT/ALT :7-56 u/L ✓ SGOT/AST: 10-40 u/L Hepatic encephalopathy-complication of liver failure Can lead to coma Azotemia/uremia- complication of kidney failure HRZE old name sa RIPE sa health center ( H or INH, R for Rifampicin, Z for pyrazeenamide I-isoniazid (H) – other name INH →S/E: numbness (Temporary) → A/E: Painful digits + paresthesia (peripheral neuritis) Neuropathy-loss of sensation (DM) INH-Neuritis (inflammed neurons)—mgt: give B6 (pyridoxine) or any B complex P-pyrazenamide (Z)→ A/E: Hyperuricemia ( uric acid > 6mg/dl) WOF: ✓ joints: Gouty→ tophi ✓ kidneys: stones (nephrolithiasis Uric acid- by product of Purine Uricosoric Drug: Zyloprim (Allopurinol), Probenecid, ulasimang bato -ipa-ihi ang uric acid E-Ethambutol (E)→ A/E: Optic Neuritis (WOF: blurring vision, eye pain)→mgt: Vit. A, B complex (B1, B6, B12) 6 yo- 20/20 vision fully developed. Do not give ethambutol to pt <6yo.--> becoz dili mabantayan ang early sign of optic neuritis or blurring of vision ky dili sab ka verbalize ang mga bata. B1-thiamine B2-riboflavin B6-pyridoxine B12-cyanocobalamine DOTS- oral (Red-orange tablet)→ FixCom4 (RIPE/HRZE), Quadtab → 6 AM → after 2-3 weeks of taking DOTS continuous pt. is not contagious anymore. Isoniazid-prophylactic medication 4-6 months If TB is MDR diri na ang IM injections or the Streptomycin/vancomycin/ (Amino glycosides) A/E: damages organs in beanshaped organs which are the: • Kidneys: WOF: urine output, KFT ( BUN, crea) • Ears: hearing loss, tinnitus (ototoxic) TYPES OF PNEUMONIA BASES ON LOCATION: Pneumonia -inflammation of lung parenchyma • Bronchi, bronchioles – broncho pneumonia • Alveoli- alveolar pneumonia • Pleura-pleural pneumonia Causes of Pneumonia: • Bacteria – staphylococcus, strep, acinetobacter, pseudomonas • Viral• Fungal- immunocompromised pts. Diagnotic Exams: • Chest X-ray • Sputum exam → GSCS (for bacteria only) ✓ Gram Staining- to determine tx; ✓ Culture & Sensitivity- to determine C/A and resistance of a certain bacteria • ELISA- Enzyme-Linked immunosorbent assay → SCREENING TEST ✓ Antibodies • PCR- polymerase chain reaction → CONFIMATORY FOR VIRAL PNEUMONIA • For covid RTPCR (Reverse Transcriptase Polemerase Chain Reaction) – CONFIRMATORY TEST FOR COVID • Western Blot – CONFIRMATORY TEST FOR HIV • Bronchoscopy • CBC ✓ Neutrophils: Bacterial ✓ T Lymphocytes: Viral ✓ Monocytes: fungal infection Bronchopneumonia 1. If the cough sputum is: • Rusty: Bacterial • Greenish: streptococcus, staph • Yellowish: acinitobacter, pseudomonas o o o o o If the sputum is pink frothy sputum (hallmark sign): pulmonary edema (Manifest in Heart and respiratory Failure) If the sputum is red (hemoptysis): PTB If the sputum is whitish, sticky (dry cough)→ virus If the sputum is greenish: fungal If the cough (sputum) is mucoid: allergy, itchy 2. 3. 4. 5. Low-grade fever Night sweats Mild chest tightness Adventitious Sounds: • crackles (popping sound during inspiration – ky ang hangin mo bangga sa sputum) ✓ Course crackles- early inspiration 6. Rhonhi Alveolar Pneumonia 1. Cough 2. High-grade fever 3. Chest pain after coughing 4. Adventitious Sounds (Fine crackles- late inspiration) 5. Rhonchi 6. Chest retractions 7. See-saw-respiration (chest indrawing) → happens when there is retractions Pleural Pneumonia 1. Cough 2. High-grade fever 3. Sharp chest pain: worsen during inspiration 4. Pleurisy- if this is presence there will be: ✓ Friction: friction rub→ harsh grating sound like rubbing your hair together (High pitch). Auscultate using diagphram. Pericardial friction rub-heart Pleural friction rub- lungs According to Acquisition: CAP (Community Acquired Pneumonia) HAP (Hospital Acquired Pneumonia) or Nosocomial pneumonia ✓ occurs after 48-72 hours of hospitalization ✓ ventilator-assisted pneumonia ✓ there should be no respi sx upon admission Tx of pneumonia: 1.Antibacterials- Penicillins/Pen G, Methicillin→ Class: Cephalosphorins S/E: tinnitus (sensorineural) -Class: Fluroquinolones – best for pts w/ cardiac problems ; ciprofloxacin, ofloxacin -Betalactams (IVTT): Cefuroxime, cefixime -Aminoglycosides: “mycin”→ gentamycin, azithromycin -First-Line of Drugs in the Community: amoxicillin, cotrimoxazole Staphylococcus- DOC: Cephalosporins (methicillin, penicillin) -once evolve becomes: • MRSA (methicillin-resistant staphylococcus aureus) ❖ DOC: Aminoglycoside: Vancomycin • VRSA (vancomycin resistant staphylococcus aureus) ❖ Trimethoprim-sulfamethoxazole (TMP-SMZ)/ Cotrimoxazole Antibacterial + If IVTT (give H2 Blocker) ✓ Ranitidine- common S/E drowsiness ✓ Cimetidine : most cheapest but have lots of S/E ✓ Famotidine : S/E, D-D interaction BID-8am-6pm TID-8am-1pm-6pm 4. 5. 6. 7. 8. 9. Antivirals Antifungals Mucolytics Antitussives Bronchodilator Hydrocortisone (steroids) Pneumothorax ✓ presence of air in the thoracic cavity ✓ enclosed- negative pressure ✓ once there is an opening there will be a vacuum/sucking effect Dx test: X-ray pleural cavity-outside visceral cavity- inside A. Open pneumothorax -puncture injuries, penetration (sucking-chest wound) -it will result to an air in the thoracic cavity. -S/sx: dyspnea, air hunger, feeling of impending doom, restlessness, shortness of breath -Mgt. cover using anything (community), vaselinized gauze (gauze soaked in PNSS) -hospital B. Close pneumothorax -it will result to an air in the thoracic cavity, which could pressure on the thoracic cavity, and tension on the thoracic cavity called TENSION PNEUMOTHORAX (mediastinal shift- organs will be pushed to the unaffected side) TENSION PNEUMOTHORAX: ✓ Mediastinal Shift: ✓ lung collapse ✓ D.O.B, air hunger ✓ PMI/Apex→ Left 5th ICS MCL Change in position ✓ tracheal deviation ✓ absence of breath sound ✓ percussion: hyperresonance to tympany (there is amount of air in the lungs) same as chronic emphysema, pneumothorax ✓ -caused by: • Rupture of bleb • Central line insertion-subclavian vein • Thoracentesis-(tripod/orthopneic) presence of lung puncture -Mgt: giving antitussive and instruct not to cough forcefully • Flail chest- rib fracture MGT: Thoracostomy- surgical opening of thoracic cavity 3-way bottle system: Bottle A: Drainage Bottle/Drainage chamber • n: 100 mL/hr for the first 2 hrs & gradually decreasing in amount • bright red:24 hours • active bleeding > 24 hours bright red bleeding Bottle B: Water Seal Bottle/ Chamber • 20 ml water • Fxn: to maintain the negative pressure of the thoracic cavity • N: bubbling/ oscillations (rise and fall of water) during inhalation; intermittent • If continuous: air leak • If absence of bubbling: 1. Obstruction- due to kinks (unkink) or clots (refer to doctor: milk the clot towards the bottle 2.lung re-expansion – naulian na and pt; (+) breath sounds; to CONFIRM: X-ray Bottle C: Suction Bottle • Low and continuous suctioning → 20mmHg Things at Bedside: 1.Vaselinized Gauze (if natangtang sa patient nga part) 2. clamps (If natangtang sa bottle) ✓ RULE: do not clamp for more than 30 minutes: becoz PROLONG clamping can lead to tension pneumothorax ✓ Extra bottle w/ NSS Procedure if nabuak: clamp, transfer to extra bottle, document MED MGT: 1. Pain medication-to prevent respiratory acidosis 2. If severe injury: provide artificial airway and connect to mechanical ventilator REMOVAL of CHEST TUBE: -Instruct to take a deep breath and slowly exhale while the doctor removes the tube -palpate site for HALLMARK: crepitus (crackling sensation) – presence of air inside the skin (Subcutaneous Emphysema) assure pt that it will resolved in days to weeks.