Drug Cards: Dronabinol, Methadone, Lidocaine, Acetaminophen
advertisement
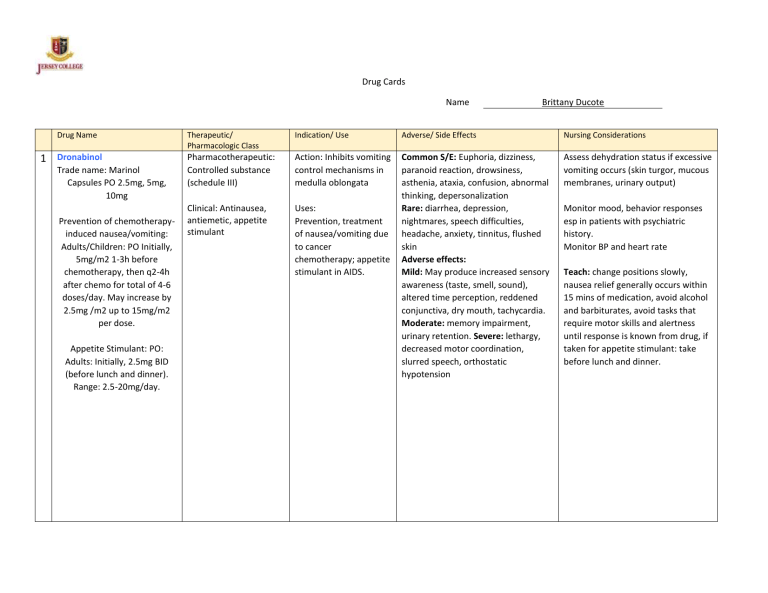
Drug Cards Name Drug Name 1 Dronabinol Trade name: Marinol Capsules PO 2.5mg, 5mg, 10mg Prevention of chemotherapyinduced nausea/vomiting: Adults/Children: PO Initially, 5mg/m2 1-3h before chemotherapy, then q2-4h after chemo for total of 4-6 doses/day. May increase by 2.5mg /m2 up to 15mg/m2 per dose. Appetite Stimulant: PO: Adults: Initially, 2.5mg BID (before lunch and dinner). Range: 2.5-20mg/day. Brittany Ducote Therapeutic/ Pharmacologic Class Indication/ Use Adverse/ Side Effects Nursing Considerations Pharmacotherapeutic: Controlled substance (schedule III) Action: Inhibits vomiting control mechanisms in medulla oblongata Assess dehydration status if excessive vomiting occurs (skin turgor, mucous membranes, urinary output) Clinical: Antinausea, antiemetic, appetite stimulant Uses: Prevention, treatment of nausea/vomiting due to cancer chemotherapy; appetite stimulant in AIDS. Common S/E: Euphoria, dizziness, paranoid reaction, drowsiness, asthenia, ataxia, confusion, abnormal thinking, depersonalization Rare: diarrhea, depression, nightmares, speech difficulties, headache, anxiety, tinnitus, flushed skin Adverse effects: Mild: May produce increased sensory awareness (taste, smell, sound), altered time perception, reddened conjunctiva, dry mouth, tachycardia. Moderate: memory impairment, urinary retention. Severe: lethargy, decreased motor coordination, slurred speech, orthostatic hypotension Monitor mood, behavior responses esp in patients with psychiatric history. Monitor BP and heart rate Teach: change positions slowly, nausea relief generally occurs within 15 mins of medication, avoid alcohol and barbiturates, avoid tasks that require motor skills and alertness until response is known from drug, if taken for appetite stimulant: take before lunch and dinner. Drug Name 2 Methadone Trade name: Dolophine, Metadol, Methadone Disket, Methadone Intensol, Methadose Dosage: PO: Adults: Initially, 2.5mg -10mg q4-12h. Children: 0.1-0.2mg/kg/dose q4-8h for 2-3 doses then q612 h as needed. Maximum dose: 10mg IV, IM, Subcutaneous: Adults: Initially, 2.5mg q8-12h, then titrate slowly to desired effect. Children: 0.1mg/kg q4-8h for 2-3 doses, then q4-12h. Maximum: 10mg/dose Therapeutic/ Pharmacologic Class Indication/ Use Adverse/ Side Effects Nursing Considerations Pharmacotherapeutic: Narcotic agonist (Schedule II) Action: Binds with opioid receptors in the CNS Assess type, location, intensity of pain. Clinical: Opioid analgesic. Uses: Relief of severe pain, detoxification, temporary maintenance treatment of narcotic abstinence syndrome Frequent S/E: Sedation, decreased BP, diaphoresis, facial flushing, constipation, dizziness, n/v. Occasional S/E: Confusion, urinary retention, palpitations, abdominal cramps, visual changes, dry mouth, headache, decreased appetite, anxiety, insomnia Rare S/E: Allergic reaction (rash, pruritis) Therapeutic effect: Alters processes affecting analgesia, emotional responses to pain; reduces withdrawal symptoms from other opioid drugs Adverse Effects: Respiratory depression, skeletal muscle flaccidity, cold/clammy skin, cyanosis, extreme drowsiness progressing to seizures, stupor, coma. Cardiac toxicity: Prolonged QT, torsade de pointes. Antidote: Nalaxone Detoxification: PO: Adults: Initial dose should not exceed 30mg. An additional 5-10mg may be added if withdrawal symptoms exist, or return in 2-4h. Total daily dose not to exceed 40mg. Maintenance range: 80-120mg/day with careful titration. Monitor VS, pain, respiratory status: rate, rhythm, depth after administration Assess adequate voiding in case of urinary retention Monitor for withdrawal symptoms, serum amylase and lipase for increases. Begin a bowel program to avoid constipation Teach: Avoid alcohol and other CNS depressants, methadone may produce drug dependence, potential for abuse, may cause dry mouth and drowsiness, avoid tasks that require motor skills until response to drug is established. Avoid CYP3A4 inducers and inhibitors that may reduce or increase methadone effects. (phenobarbital, charithromycin, etc) Report severe drowsiness, respiratory depression. Drug Name Therapeutic/ Pharmacologic Class 3 Lidocaine (Topical) Trade name: Lidoderm, Xylocaine Topical: Adults: Apply to affected areas as needed Topical (dermal patch): Adults: Apply to intact skin over most painful area (up to 3 applications once for up to 12 hours in a 24h period) Pharmacotherapeutic: Amide anesthetic. Clinical: Antiarrhythmic, anesthetic. Therapeutic effect: Causes temporary loss of feeling/sensation Inhibits ventricular arrhythmias. Indication/ Use Adverse/ Side Effects Nursing Considerations Action: Inhibits conduction of nerve impulses Occasional S/E: Burning, stinging, tenderness at application site. Rare S/E: Generally associated with high dose: Drowsiness, dizziness, disorientation, light-headedness, tremors, apprehension, euphoria, sensation of heat/cold/numbness, blurred/double vision, tinnitus, nausea. Obtain baseline VS, EKG, serum electrolytes. Monitor LOC. Monitor EKG, VS for cardiac performance. -If EKG shows arrhythmias, prolongation of PR interval or QRS complex, inform physician immediately. Adverse Effects: Cardiovascular depression, bradycardia, hypotension, arrhythmias, heart block, CV collapse, cardiac arrest. Assess HR for rate, rhythm, quality. BP for hypotension. Uses: Topical Anesthetic: local skin disorders (minor burns, insect bites, prickly heat, skin manifestations of chickenpox, abrasions). Mucous membranes (local anesthesia of oral, nasal, laryngeal mucous membranes; local anesthesia of respiratory, urinary tracts; relief of discomfort pruritis ani, hemorrhoids, pruritis vulvae. Dermal patch: relief of chronic pain in postherpetic neuralgia, allodynia (painful hypersensitivity) Teach: Report irritation, pain, numbness, swelling, blurred vision, tinnitus, respiratory difficulty. Drug Name 4 Acetaminophen Trade name: Abenol, Acephen, Atasol, Feverall, Mapap, Ofirmev, Tempra, Tylenol IV: Adults, adolescents weighing 50kg or more: 1000mg q6h or 650mg q4h. Adults, adolescents weighing less than 50kg: 15mg/kg q6h or 12.5mg/kg q4h. Children 2-12: 15mg/kg q6h or 12.5mg/kg q4h. Infants/children less than 2: 7.5-15mg/kg q6h. PO: Adults, children 13 and older: 325-650mg q4-6h or 1g 3-4 times a day. Children 12 and younger: 1015mg/kg/dose q8h. Neonates: 30mg/kg/once, then 20mg/kg/day. Rectal: Adults: 325-650mg q4-6h. Children: 10-20mg/kg/dose q4-6h. Neonates: 30mg/kg/once, then 20mg/kg/dose q6-8h. Therapeutic/ Pharmacologic Class Indication/ Use Adverse/ Side Effects Nursing Considerations Pharmacotherapeutic: Central analgesic. Clinical: Non-narcotic analgesic, antipyretic. Action: Appears to inhibit prostaglandin synthesis in the CNS and block pain impulses through peripheral action. Acts centrally o hypothalamic heatregulating center, producing peripheral vasodilation (heat loss, skin erythema, diaphoresis) Rare S/E: Hypersensitivity reaction. Assess onset, location, duration, type of pain. Assess for fever. Assess alcohol usage. Adverse Effects: Early signs of toxicity: Anorexia, nausea, diaphoresis, fatigue within first 12-24 hours. Later signs of toxicity: Vomiting, right upper quadrant tenderness, elevated hepatic function tests within 48-72 hours after ingestion. Assess for relief of pain, fever. Assess risk for bleeding if also taking Warfarin or St. John’s wort. Monitor AST, ALT, bilirubin, prothrombin levels for indication of hepatotoxicity Antidote: Acetylcysteine Uses: Relief of mild to moderate pain, fever. IV Use: management of moderate to severe pain when combined with opioid analgesia. Report to physician if use is longer than 5 days in children and longer than 10 days in adults. Report fever lasting longer than 3 days to physician Teach: Not to exceed more than 4g in 24 hour period. Be aware of other over the counter meds that may contain acetaminophen. Avoid alcohol. Take with a full glass of water.