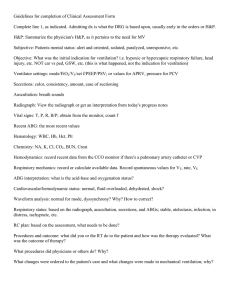
Signs and symptoms of Hypoxemia headache breathlessness or severe dyspnea palpitations angina restlessness tremors Severe Hypoxemia impaired judgement progressive loss of cognition loss of motor function that worsens loss of consciousness Signs of impending respiratory failure ↑ RR, SOB, tachypnea ↑ HR Dizziness Cyanosis flaring of nostrils intercostal, suprasternal or supraclavicular retraction ↑ accessory muscle recruitment paradoxical breathing diaphoresis anxiety, confusion, impaired consciousness Type types: hypoemix +++ (Impaired gas exchange causing inability to maintain adequate oxygen saturation.) - high altitudes - CHF Shunt: perfusion of lung regions that have low ventilation - mucus plug, bronchospasm,inflammation, pneumonia, chronic bronchitis, bronchiectasis Dead Space: ventilation of lung regions that have low perfusion - PE, emphysema, cardiogenic shock Hypercapnic: inadequate elimination of CO2 by lungs - hyperventilation - impaire ventilatory drive Indications for Mechanical Ventilation - - General anesthesia, Shock, Life support during Cardiac or Respiratory arrest Management of ↑ ICP Pulmonary diseases – obstructive & restrictive Neurological diseases – ALS, Guillain-Barre, Myasthenia gravis Increased WOB unrelieved by other interventions Respiratory muscle fatigue Impending respiratory arrest o Apnea or hypopnea o Severe hypoxia or hypercapnia Respiratory distress with altered mentation/ obtundation e.g. poisoning, ETOH intoxication, brain injury, drug overdose, stroke o GCS of ≤8 should undergo tracheal intubation in order to prevent possible airway obstruction, aspiration or respiratory compromise leading to secondary brain injury o Intact cough and gag reflex? - Airway issue – obstruction, edema, inability to mobilize secretions Types of Mechanical Ventilation Negative Pressure Mechanical Ventilation (Iron Lung, Chest Cuirass) Positive pressure ventilation(NPPV, IPPV) (CPAP, BiPAP) Noninvasive Positive Pressure Ventilation (NPPV) Continuous passive airway pressure (CPAP) pt spontaneously breathes air delivered at steady, pre-set, continuous pressure during inspiration and expiration to keep airways open Airway Pressure Release Ventilation (APRV) pt spontaneously breathes with a set amount of CPAP CPAP can be dropped allowing the pt to exhale CPAP is restored Benefits Indications Precautions & contraindications short term use reduces need for sedation more cost effective decreased complications decreased infections decreased airway trauma decreased LOS decreased Mortality Respiratory drive must be intact Obstructive Sleep Apnea Hypoxic respiratory failure Neuromuscular diseases pediatric pt with acute resp. failure COPD exacerbation Cardiogenic pulmonary edema if pt able to protect impending cardiac or respiratory arrest hemodynamically unstable severe hypoxemia unconscious/uncoo perative UGIB risk for aspiration unstable upper airwayobstruction/secreti on/protection once exhalation is complete Allows more pt control than traditional CPAP Bilevel positive airway pressure (BiPAP) airway pneumonia facial trauma Disadvantages skin breakdown gastric distention claustrophobia Rhinitis Eye irritation headache sinus pain IPAP EPAP both levels above atmospheric pressure often used after CPAP has failed/not tolerated Invasive PPV used to deliver room air or it can deliver oxygen enriched air in concentrations up to 100% Advantages allows better control of minute ventilation better pt synchrony and monitoring better secretion management and airway prt=otection extensive monitoring capability decrease work of breathing mechanical bronchodilation reversal of respiratory failure - dec. SpO2 despite supplemental O2 - increases CO2 - respiratory acidosis Disadvantages discomfort and limitations of artificial airway ventilatory associated lung injury and infection increased intrathoracic pressure - decrease venous return and CO - decrease systemic BP increase cost decreased urine output increased ICP muscle weakness Artificial/adjust airways Upper airway obstruction Inability to protect the lower airway from aspiration Inability to clear secretions from lower airways Need for intubation/mechanical ventilation Drawbacks Endotracheal tube (ETT) uncomfortable for conscious pt prevents speech bypasses normal respiratory defenses T3-T4 level 5 cm above carina (T6) cuffed conduits placed in the trachea via nose/mouth to maintain airway patency and allow Benefits prevention of complications humidify to prevent drying of mucosa and secretions cuff pressures avoid over humidify to prevent drying of mucosa and secretions cuff pressures avoid over inflation maintain adequate if misplaced into R. main bronchus… collapse of the left lung decrease in SpO2 and low PaO2 lead to atelectasis of L. lung and hyperinflation R. lung for mechanical ventilation for pt with respiratory failure Communication board, Call bell Tracheostomy inserted into the trachea below vocal pt usually unable to cords speak performed in pt who are intubated no oral feeding for longer than 1-3 until cleared for weeks or who have swallow-NGT upper airway obstruction If patient weaned communication from ventilator board, iPad, pen humidified oxygen and paper, call bell delivered via trach mask Passy Muir Valves one way valve placed over trach that opens to allow inspiration via trach then closes air is exhaled up thru the vocal cords, mouth and nose allowing for speech reduced cough effectiveness nosocomial infection broncho/laryngosp asm aspiration tooth damages injury to lips, tongue, VC, pharynx tracheal stenosis, erosion, necrosis cardiac arrhythmias Hemorrhage surgical emphysema pneumo/hemothor ax cricoid cartilage damage fistula infection dysphagia stenosis sinus aphonia/dysphonia inflation to prevent aspiration and achieve good tidal volume reduces laryngeal injury improved comfort decreased airflow resistance improved airway care may allow for oral feeding with cuff deflated allows for vocalization with a cap/plug Speak with a Trach fenestrated trach allows for vocalization normal breathing with trach in situ coughing thru mouth improves swallowing step prior to decannulation indicated for pt: alert and attempting to communicate able to exhale around the trach rube able to tolerate cuff deflation have minimal secretions can be used for vent dependent pt doesnt require a fenestrated trach contrainditons inflated trach cuff absence of a cuff leak thick uncontrolled trach secretions think uncontrolled oral secrtions severe respiratory weakness unconscious gas trapping with auto PEEP Ventilator Parameters Peak Pressure if set limits exceeded ventilation if peak pressure exceeded because → alarm of decreased lung compliance or increased airway resistance pressure will be decreased… pressure alarm will go off - chronic bronchitis - CF - increased mucus production peak inspiratory pressure: pressure only while flow is occurring - dynamic measure - normal -60cmH20 plateau pressure: pressure in the lung after all flow has stopped -static measure peak expiratory pressure: max pressure achieved during expiration - norm: >80-100cmH20 Respiratory rate (RR, f) Clinical Situations where RR may be increased Hypoxemia good indicator of pt’s stimulus to minimum number of breaths/min vent delivered intiral RR set b/w 10-20 b/m breathe and normal vs. abnormal ventilation status can provide all pt’s ventilation, or pt may be able to breathe spontaneously b/w vent breathes may adjust RR to control CO2 levels Tidal Volume (Vt) calculated based on pt age, gender, and height volume of gas vent delivers with each breathe Hypercapnia Acidosis Increased dead space vent anxiety decreased lung compliance RR decreased in respiratory center depression CO2 narcosis Vti = Inspiratory Tidal Volume. Vte = Expiratory Tidal Volume helps to enhance ventilation Vti – Vte = Leak usual 6 to 8 ml/kg (ideal body weight ) Minute Ventilation (Ve) total volume of gas delivered in 1 minute used in conjunction with ABGs normal= 5-10 L/min Fraction of inspired oxygen (FiO2) Hypoventilation – inadequate ventilation to eliminate CO₂, respiratory acidosis Hyperventilation: ventilation in xs of that needed to maintain adequate CO₂ levels –produces hypocapnia and respiratory alkalosis concentration of O2 in inspired gas range is 21% to 100% varies depending on pt condition, SpO2, ABG Titrate to keep SpO2 >95% Positive end expiratory pressure (PEEP) range from 0-50 cmH20 on vent initial settings 5ml maintains volume in alveoli to prevent collapse at end expiration ↑ oxygenation ↓ WOB adjust with ABG results and clinical status Clinically indicated for: low volume vent cycles FiO2 requirements >0.60 ARDS obstructive lung disease DO NOT use in pneumonia Types of Breathes Controlled Breathe each breath delivered to pt is initiated and ended by the How Breath is initiated/Triggered machine according to present pressure/volume Assisted Supported Breathe No spontaneous breaths - elapsed present time is the trigger - provides RR 14-20bpm Presence of spontaneous breath - negative pressure or inspiratory flow is triggered - sensitivity set to determine how easy for pt to trigger the vent to deliver a breath every breathe is spontaneous (ie. Limit -Size of Breaths pt triggered) but supported by vent. which delivered present tidal Volume controlled volume/pressure level -present volume of gas delivered -the larger the volume the greater pressure support the expiratory time required volume support - RR and I:E ratio Pressure Controlled -preset inflation pressure of gas delivered -decrease risk of barotrauma Pressure Regulated Volume Control (PRVC) pre-set/backup vent added to pressure control mode - pressures and flow regulated based on changing lung compliance Spontaneous Breaths initiated, controlled and cycled by pt Modes of mechanical ventilation how the vent is programmed to control… time, pressure, volume and flow of breaths delivered to a pt cycling mechanism describes how the vent is programmed to switch from inspiration to expiration Combination modes combination of both controlled and supported Inspiratory and Expiratory times (Ti: Te) Ti: time over which the tidal volume/pressure is delivered (3-5 seconds) may include pause Te: time remaining before next breath I:E ratio- usually set to 1:2 to mimic usual pattern of breathing Volume controlled/cycle ventilation Inspiration ends when machine delivers a preset tidal volume at which point flow stops and the ventilator cycles to expiration trigger is time most used initial vent setting Provides stable minute ventilation with known tidal volume Pressure controlled/cycled ventilation Inspiration ends when machine delivers a preset inflation pressure at which point flow stops to allows for expiration Volumes vary with each breath according to resistance and compliance If a patient becomes extremely asynchronous or coughs, the highpressure alarm may be triggered and the inspiratory phase ends, resulting in exhalation. Safety feature to avoid elevated and sustained inspiratory pressure that can cause barotrauma. Ventilator flow rate initial setting 40-60 L/min rate that a volume of gas is delivered to the pt per unit of time can be adjusted to deliver vent in set time ↑ flow results in ↑RR and VE Assist Control (AC) aka Controlled Mandatory Ventilation (CMV) vent delivers mechanical breathes non weaning mode volume control - rate preset to maintain a pressure control min. minute ventilation pressure regulated volume control - pt may have no control over vent requires pt or time can trigger breath sedation → full paralysis flow is constant during mechanical breath pt may have increased tolerance Supported Modes works on spontaneous breaths pt must have intact respiratory drive to control RR and inspiratory time pt effort and Vt may vary so machine provides a boost to spontaneous breath to ↑ Vt or overcome airway resistance Synchronized intermittent mandatory ventilation (SIMV) Synchronizes machine’s mandatory breaths with spontaneous patient breaths. ↑ pt comfort & may↓ WOB popular weaning mode pt fatigue vent will alarm back up rate and Vt may be set to deliver a min. Ve good mode for respiratory muscle exercises Disadvantage: ↑ WOB, may reduce cardiac output which may prolong ventilator dependency. CPAP mode weaning mode reduces WOB pt takes spontaneous breaths machine supports effort by delivering small amounts of continuous positive pressure during inspiration addition pressure support above PEEP may be added to augment pt Vt Ventilator Alarms - High RR High pressure Low tidal volume Circuit disconnect!! Apnea!! NEVER TURN OFF ALARMS!! ASSESS THE PATIENT, NOT THE ALARM High Pressure Alarm occlusion: biting the ETT secretion in the airway WHEN IN DOUBT & PT IN DISTRESS – secretions mucus plug bronchospasm tube kinked water in tube the head and moisture exchanger being waterlogged USE MANUAL RESUSCITATOR and 100% FiO2 TO PROVIDE PPV AND PAGE THE RT displacement: has the tube slipped into the right main stem pt vent asynchrony: pt bucking coughing gagging talking laughing anxious restless ARDs, pulmonary edema, pneumothorax Low Pressure or Low Exhaled Volume Alarm is the pt connected to the vent - accidental extubation quickly check for leaks in the system did vent malfunction ETT position, is cuff properly inflated did the pt condition change WHEN IN DOUBT & PT IN DISTRESS USE MANUAL RESUSCITATOR TO PROVIDE PPV AND PAGE THE RESPIRATORY THERAPIST Weaning Protocols Weaning Monitor patients for exercise intolerance during weaning trials!! ↑ RR ↓ Vt ↑ use of accessory breathing muscles Stop and rest!! Criteria for successful SBT - Management of underlying respiratory condition Respiratory rate < 35 breaths/minute Heart rate < 140 /minute Stable pulmonary function measures Arterial oxygen saturation >90% on FiO₂<0.4 Stable systolic blood pressure Good tolerance to SBT No signs of respiratory distress (Accessory muscle use, paradoxical breathing, intercostal retractions, nasal flaring, profuse diaphoresis, agitation) - - Primary Secondary First point of entry into the health care system Routine health care services provided to pt with acute and chronic conditions PCP, OB/GYN,PA, NP Provided in outpatient settings More complex/advanced care usually provided in hospital setting First referral level for more advanced interventions not available from PCP Surgeons, cardiologist, orthopedist May require in patient hospitalization or same day surgery Tertiary Very specialized care for conditions that are relatively rare Complex technology or major surgical procedures Specialized physicians in hospitals • A self referred patient seeks the services of a physical therapist for new onset of low back pain • A physician assistant treats a patient in the emergency department of a hospital for injuries resulting from a fall • A neurosurgeon completes a consultation for a patient requiring resection of a brain tumor Acute Care Hospital Short term hospitalization Rapid discharge to next level of care Pt. is medically unstable and requires constant medical/nursing care LOS 3-5 days in hospital Diagnosis MD, PA, RN,PT,OT Long term acute care hospital (LTACH) Long term medical intervention or hospital Pt. require specialized care including 24 hour medical, nursing and respiratory therapy >25 days mechanical vent dependence and weaning. sepsis and non-healing wounds Acute Rehab In-patient rehabilitation, Social and vocational services to disabled individuals after discharge from hospital Intermediate health care Must be able to participate in minimum of 3 hours of intense daily rehab per day 15 days Subacute Rehab Pt should be able to tolerate stroke, SCI, TBI, PD, MS, amputation Pt. medically fragile Medical, nursing, and rehab staff Provided in skilled nursing facility or hospital at least 1 hour therapy/day Extended care facility or Skilled Nursing Facility (SNF) Facilities can be free standing or part of a hospital transitional care unit Nursing home/LT C Residential facility that provides care for patients with chronic illness or disabilities Services include medical, specialized services and rehabilitation Hospice/ palliative care Services provided at home, free standing facilities or inpatient setting Emphasis is on spiritual, emotional, psychological and legal needs Home Care Who no on a reg. longer basis qualify for require acute care Provides care to patients who are no longer acute but still require skilled care on an inpatient basis Continuous care provided by nursing, rehab, and other health care services… as 24 hr. 7 days/week nursing coverage Skilled therapy (OT,PT,SLP) available 5 days/week Provides services for 60 days or more chronic illness or disabilities Skilled nursing and aides are available 24 hours Reimbur sement requires certifica tion of terminal illness i.e. ≤ 6 mos. life expecta ncy Supportive care for terminal patients Nurses, SW, clergy, volunteers, physicians SNFs must be certified by Medicare and meet qualifications Health care provided to patients in their homes Provided by home health agency Eligible patients: Home bound or have great difficulty leaving Rehab services are consulted as needed Pt. must be certifiec by an MD to require skilled care from (HHA) which may be governmental, private, non-profit or for-profit home without assistance Would experience a health risk leaving the home RN, PT,OT,SLP, aide Require skilled care from RN, PT, OT, SLP Must have reasonable potential for improvement Requires skilled services (not housekeeping) Out patient or ambulat ory care Outpatient basis Stable patients Pt. no confined to an intuitional bed Outpatient clinics, surgical centers, or private practices Decision tree for making referrals Infection Control Airborne Contact Protect against germs that are spread through the air Protect against skin contact with infectious organisms Diseases TB, SARS, smallpox, chickenpox, disseminated shingles (Herpes zoster) Precautions Patient placement in negative pressure isolation room Airborne Disease Precaution (STOP) sign on door Protective Gear N95 respirator for staff use Resistant organisms – Methicillin Resistant S. aureus (MRSA), Vancomycin Resistant Enterococcus (VRE), Extended Spectrum Beta-lactamase positive (ESBL) bacteria, Clostridium difficile (C. diff), Patient placement in private room Gown for staff and visitor use Contact Precaution (STOP) sign on door Gloves for staff use Wear PPE when direct/indirect contact with patient/environment anticipated e.g., taking vital signs, touching Surgical procedure mask for patient use Droplet Protect against large respiratory droplets when the patient coughs or undergoes respiratory procedures communicable skin conditions (ring worm, scabies) bed rail, bedside and bedside tables etc. Respiratory Syncytial Virus (RSV), Mumps, Meningococcal meningitis, Pertussis (whooping cough “STOP” contact isolation sign Patient placement in private room Droplet Precautions (STOP) sign on door Gowns, gloves & mask for staff and visitor use Face protection (goggles/face shield) for staff use Hand hygiene by all persons before leaving room Universal Standard Precautions Activity Restrictions Bed rest DO NOT get pt OOB if last activity order was bed rest Cardiac A fib -> hold PT if new onset or HR >120 @ rest MAP <60 Cardiac cath/PCI � bed rest with pressure to femoral artery access site 4-5 hours after Hold PT for chest pain until R/O MI Use Rolling walker vs standard walker No PT if pt on IABP Precautions and Contraindications Sternal Pulmonary Pace Makers CABG Pulse ox: >90Transcutaneous pacing Valve 92% normally → do not move pt replacements 88-90% if end Transvenous/epicardial stage pulmonary - Avoid tension disease on leads - PPM Signs and - Sling Symptoms: - No shoulder flex >90 SOB (dyspnea) - Minimize use of cyanosis shoulder unil dizziness(syncop wire insertion e) heal fatigue - Hold PT if pacer edema is not capturing chest pains until readjusted - ICD Contact MD if ICD fires Pt may become dizzy or syncopal Low battery tone Know pt tachycardia detention rate Don’t use ESTIM over ICD Resting HR Resting SBP Resting DBP Oxygen Saturation ECG Other HR SBP DBP Oxygen Saturation Other Contraindications for Exercise or Physical Activity >120 bpm or <50bpm >200 mmHg or <90mHg SBP <90 after MI >110 mmHg <90% Serious arrhythmias: a flutter, a fib, sustained SVT V fib, V tach, 2nd or 3rd degree AV block Cyanosis, diaphoresis, bilateral edema in a patient with CHF, pallor, fever, weight gain > 4–6 lbs./day, abnormal change in breath sounds or heart sounds, acute systemic infection w fever Indications to terminate Exercise or Physical Activity >sudden drop >15 bpm, change from regular to irregular rhythm or exceeds HR max >200 mmHg, decrease to <90mHg Drop >10 mmHg from resting or with increasing exercise >110 mmHg <90% cyanosis, diaphoresis, bilateral edema in a patient with CHF, pallor, abnormal change in breath sounds or heart sounds, ataxia SOB, angina, dizziness Prior to leaving patients room - - Call bell & pt’s needs within reach Side rails up (know institution policy) Restraints reapplied Lines and tubes intact Ensure pt safe and comfortable Communicate with RN Document response to tx VS at rest, during activity, recovery (monitor until stabilized) • Assess if normal/abnormal response • Sx - shortness of breath, chest pain, faintness, clamminess Communicate with team regarding concerns Treatment Guidelines Cardiac/Sternal Precautions No UE overhead activity, past 90 No UE WC propulsion No pushing/pulling No bending forward No lifting over 5-10lbs No crossing legs or ankles sit in the back seat of the car push off with your legs when standing use the log roll technique when getting out of bed CABG No lifting over 5-10lbs Avoid overhead reaching avoid standing for long periods of time Light ADL activities Monitor HR, BP, RR,O2 sat teach self monitoring endurance/functional mobility activities avoid excessive behind and encourage use of DME avoid isometric exercise no AROM of shoulder flex/abd above shoulder level Valve Replacement avoid pushing/pulling objects over 5-7 lbs prevent infection energy conservation/work simplification technique education Monitor HR, BP, RR,O2 sat incorporate rest, relaxation, and pursed-lip breathing Pacemakers 4-6 weeks, patient unable to raise left arm overhead Monitor HR, BP, RR, O2 Sat Avoid contact with strong electric or magnetic equipment No UltraSound or E-stim over surgical site Energy conservation/work simplification techniques LVAD (implanted device to help pump blood from the lower chambers of the heart to the rest of the body) Traditional OT/PT treatment for any cardiac patient with thoracotomy Follows sternal/cardiac precautions NO CPR!!!!! Use doppler to monitor BP Train patient on independently performing device connections/ donning/doffing vest Fine motor coordination/ hand strengthening Borg Scale of Exertion BP can only be taken using doppler assess Mean Arterial pressure 70-90 MAP Heart Transplant - - Prevent infection/reverse isolation General reconditioning HR will be higher secondary to denervated Vagus Nerve Chronotropic incompetence Borg Scale of perceived exertion Signs and Symptoms of Cardiac Dysfunction During Treatment marked fatigue/dyspnea drop in BP - >20mmHg drop in SBP - >10mmHg drop in SBP and DBP dizziness RR >40 bpm diaphoresis confusion syncope increased or onset of crackles in lungs presence of S3 heart sound pallor Signs of Activity Intolerance After Treatment - Peripheral edema - 2-3 hours after activity increased crackles in lungs - 0-30 min after activity occurrence of S3 heart sound Weight gain of 2-3 lbs - 12-24 hours after activity Nordon-Craft Article: Intensive Care Unit-Acquired Weakness: Implications for Physical Therapist Management physical rehab for individuals with ICU acquired weakness can begin as soon as they have sufficient medical stability to accommodate the increased vascular and oxygen demands - can pt tolerate rehab from a physiological perspective 15-30 minutes, 1 to 2 times daily Supplemental Oxygen Utilization During Physical Therapy Interventions