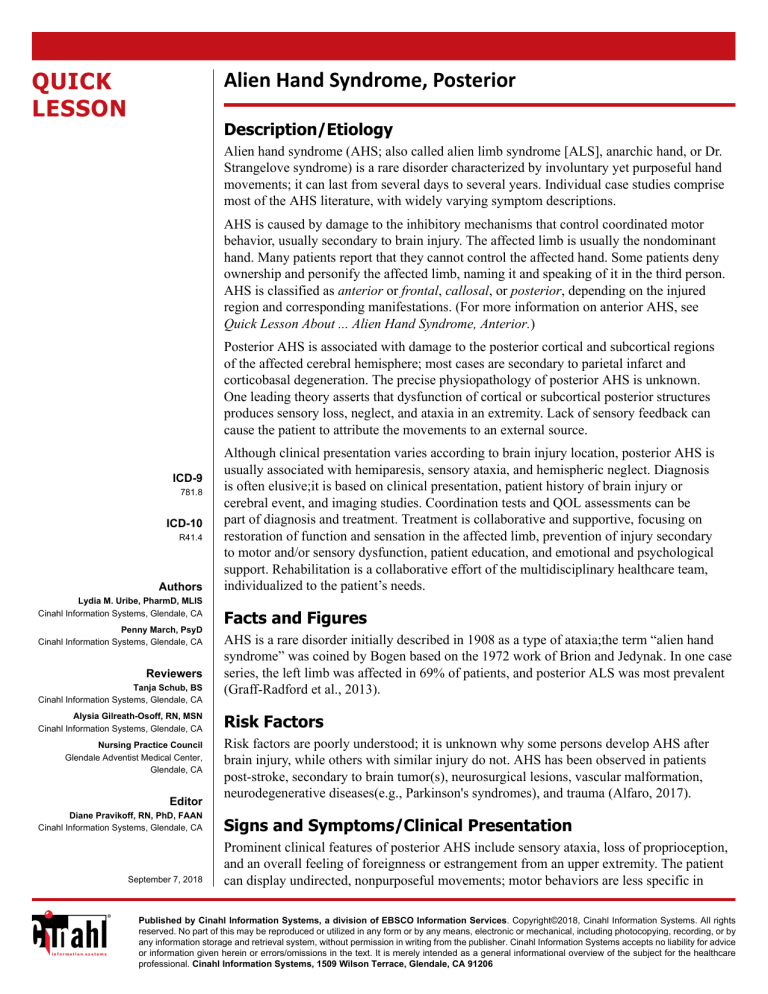
QUICK LESSON Alien Hand Syndrome, Posterior Description/Etiology Alien hand syndrome (AHS; also called alien limb syndrome [ALS], anarchic hand, or Dr. Strangelove syndrome) is a rare disorder characterized by involuntary yet purposeful hand movements; it can last from several days to several years. Individual case studies comprise most of the AHS literature, with widely varying symptom descriptions. AHS is caused by damage to the inhibitory mechanisms that control coordinated motor behavior, usually secondary to brain injury. The affected limb is usually the nondominant hand. Many patients report that they cannot control the affected hand. Some patients deny ownership and personify the affected limb, naming it and speaking of it in the third person. AHS is classified as anterior or frontal, callosal, or posterior, depending on the injured region and corresponding manifestations. (For more information on anterior AHS, see Quick Lesson About ... Alien Hand Syndrome, Anterior.) Posterior AHS is associated with damage to the posterior cortical and subcortical regions of the affected cerebral hemisphere; most cases are secondary to parietal infarct and corticobasal degeneration. The precise physiopathology of posterior AHS is unknown. One leading theory asserts that dysfunction of cortical or subcortical posterior structures produces sensory loss, neglect, and ataxia in an extremity. Lack of sensory feedback can cause the patient to attribute the movements to an external source. ICD-9 781.8 ICD-10 R41.4 Authors Lydia M. Uribe, PharmD, MLIS Cinahl Information Systems, Glendale, CA Penny March, PsyD Cinahl Information Systems, Glendale, CA Reviewers Tanja Schub, BS Cinahl Information Systems, Glendale, CA Alysia Gilreath-Osoff, RN, MSN Cinahl Information Systems, Glendale, CA Nursing Practice Council Glendale Adventist Medical Center, Glendale, CA Editor Diane Pravikoff, RN, PhD, FAAN Cinahl Information Systems, Glendale, CA September 7, 2018 Although clinical presentation varies according to brain injury location, posterior AHS is usually associated with hemiparesis, sensory ataxia, and hemispheric neglect. Diagnosis is often elusive;it is based on clinical presentation, patient history of brain injury or cerebral event, and imaging studies. Coordination tests and QOL assessments can be part of diagnosis and treatment. Treatment is collaborative and supportive, focusing on restoration of function and sensation in the affected limb, prevention of injury secondary to motor and/or sensory dysfunction, patient education, and emotional and psychological support. Rehabilitation is a collaborative effort of the multidisciplinary healthcare team, individualized to the patient’s needs. Facts and Figures AHS is a rare disorder initially described in 1908 as a type of ataxia;the term “alien hand syndrome” was coined by Bogen based on the 1972 work of Brion and Jedynak. In one case series, the left limb was affected in 69% of patients, and posterior ALS was most prevalent (Graff-Radford et al., 2013). Risk Factors Risk factors are poorly understood; it is unknown why some persons develop AHS after brain injury, while others with similar injury do not. AHS has been observed in patients post-stroke, secondary to brain tumor(s), neurosurgical lesions, vascular malformation, neurodegenerative diseases(e.g., Parkinson's syndromes), and trauma (Alfaro, 2017). Signs and Symptoms/Clinical Presentation Prominent clinical features of posterior AHS include sensory ataxia, loss of proprioception, and an overall feeling of foreignness or estrangement from an upper extremity. The patient can display undirected, nonpurposeful movements; motor behaviors are less specific in Published by Cinahl Information Systems, a division of EBSCO Information Services. Copyright©2018, Cinahl Information Systems. All rights reserved. No part of this may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the publisher. Cinahl Information Systems accepts no liability for advice or information given herein or errors/omissions in the text. It is merely intended as a general informational overview of the subject for the healthcare professional. Cinahl Information Systems, 1509 Wilson Terrace, Glendale, CA 91206 posterior AHS than in the anterior variant. Symptoms of posterior AHS reportedly diminish more quickly than those of anterior AHS, sometimes within days. Assessment › Patient History • Assess symptom onset, duration, and severity; assess social impact of symptoms (e.g., ability to work, perform ADLs, maintain social relationships) • Obtain medical and surgical history, with attention to history of traumatic brain injury, infarct, surgery, tumor(s), or degenerative disease › Physical Findings of Particular Interest • Patient might report absence of sensation on tactile stimulation › Laboratory Tests • There are no laboratory tests to diagnose AHS › Diagnostic Tests/Studies • CT scan or MRI can identify changes consistent with hemispheric lesions secondary to infarction, ischemia, tumor, or neurodegenerative disease • Tests of motor functioning (e.g., Functional Independence Measure [FIM], Jebsen-Taylor Hand Function Test, Minnesota Rate of Manipulation Test)can identify reduced coordination and control in the affected limb Treatment Goals › Promote Rehabilitation and Progressive Independence with ADLs • Provide initial and ongoing assessment of patient’s functional ability using standardized assessment tools, if available; immediately report worsening of physical, neurologic, psychological, or emotional signs/symptoms to the treating clinician and provide prescribed treatment • Assess fall risk , and provide individualized supervision to reduce risk for injury; immediately report injuries to the clinician and provide prescribed treatment • Encourage/assist with careful positioning and good hygiene of the affected hand to reduce risk for skin compromise and musculoskeletal injury • Request referral to physical and/or occupational therapy to increase strength, endurance, transfer ability, balance, fine motor skills, and sensory-motor integration –Encourage/assist patient with weight-bearing activities to improve neuromuscular function –Provide necessary retraining and assistance to complete ADLs, supporting reduction of intermanual conflict and return to self-sufficiency › Provide Emotional Support and Educate • Assess anxiety level and coping ability; provide emotional support; educate and encourage discussion about frustration and embarrassment caused by lack of extremity control; be patient and empathetic, showing concern for the patient’s overall well-being rather than localized symptom alleviation • Assist the patient in setting achievable short- and long-term goals to increase self-worth and self-esteem; request referral, if appropriate, to a –mental health clinician for counseling on strategies for coping with AHS-associated frustration and anger –social worker for identification of local resources for support groups, outpatient physical/occupational therapy, transportation, and in-home services Food for Thought › Researchers analyzed a cohort of 150 patients with AHS and found the most common cause to be corticobasal syndrome (n = 108), the most common manifestation was isolated upper extremity AHS (n = 122), and consistent contralateral parietal lobe damage regardless of AHS etiology (Graff-Radford, 2013) › Researchers in India described a case of a person with progressive, simultaneous alien hand and leg syndrome as the sole presenting feature of sporadic Creutzfeldt-Jakob disease (sCJD), suggesting that CJD should be part of differential diagnosis in cases of isolated alien hand symptoms (Kumawat et al., 2015) › Researchers report on the case of a 65-year-old female classical pianist, who presented with uncontrollable levitation of the right arm while playing the piano. Assessing the patient with Diffusion-Tensor magnetic resonance imaging (DT-MRI), extensive damage was observed to the left frontotemporal cortex and into the ipsilateral parietal cortex, causing a disruption of corpus callosum projections (Alfaro, 2017) › Researchers conducting a study assessing multisensory integration and visual self-recognition of body parts in patients post right-hemisphere stroke with AHS reported that participants with AHS were unable to access a reliable multisensory representation of their alien hand, as compared to the control group (Olgiati, 2017) Red Flags › Affected-limb personification might be mistaken as a symptom of psychosis What Do I Need to Tell the Patient/Patient’s Family? › Advise family members to remain neutral (i.e., do not blame the person for their behavior and remain calm) during episodes and to focus on the person rather than on behavior › There is no cure for AHS; treatment is supportive, and recovery can be slow › Educate the patient and family about home safety precautions; extremity sensory loss increases risk for burns and skin breaks; extremity motor dysfunction increases risk for musculoskeletal injury References 1. Alfaro, A., Bernabeu, Á, Badesa, F. J., García, N., & Fernández, E. (2017). When playing is a problem: An atypical case of alien hand syndrome in a professional pianist. Frontiers in Human Neuroscience, 11, 198. doi:10.3389/fnhum.2017.00198 (C) 2. Bartolo, M., Zucchella, C., Pichiecchio, A., Pucci, E., Sandrini, G., & Sinforiani, E. (2011). Alien hand syndrome in left posterior stroke. Neurological Sciences, 32(3), 483-486. doi:10.1007/s10072-011-0490-y (C) 3. Graff-Radford, J., Rubin, M. N., Jones, D. T., Aksamit, A. J., Ahlskog, J. E., Knopman, D. S., ... Josephs, K. A. (2013). The alien limb phenomenon. Journal of Neurology, 260(7), 1880-1888. doi:10.1007/s00415-013-6898-y (R) 4. Kumawat, B. L., Sharma, C. M., Nath, K., Acharya, M., Khandelwat, D., & Jain, D. (2015). Alien hand and leg as the presenting feature of probably sporadic Cruetzfeldt-Jakob disease: A rare presentation of a rare disease. Annals of Indian Academy of Neurology, 18(1), 99-102. doi:10.4103/0972-2327.144278 (R) 5. Mark, V. W. (2017, May 2). Alien hand syndrome. Medlink Neurology. Retrieved August 30, 2018, from http://www.medlink.com/article/alien_hand_syndrome (RV) 6. Olgiati, E., Maravita, A., Spandri, V., Casati, R., Ferraro, F., Tedesco, L., ... Bolognini, N. (2017). Body schema and corporeal self-recognition in the alien hand syndrome. Neuropsychology, 31(5), 575-584. doi:10.1037/neu0000359 (RCT) 7. Panikkath, R., Panikkath, D., Mojumder, D., & Nugent, K. (2014). The alien hand syndrome. Proceedings (Baylor University. Medical Center), 27(3), 219-220. (C) 8. Shereef, H., & Cavanna, A. E. (2013). The "brother's arm:" Alien hand syndrome after right posterior parietal lesion. Journal of Neuropsychiatry and Clinical Neurosciences, 25(4), E02. doi:10.1176/appi.neuropsych.12080193 (C)