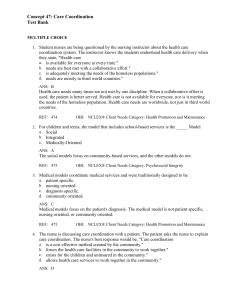
Timbys Fundamental Nursing Skills and Concepts 12th Edition Test Bank
advertisement

Timby's Fundamental Nursing Skills and Concepts 12th Edition by Moreno Timby Test Bank Chapter 1 Nursing Foundations Multiple Choice Identify the choice that best completes the statement or answers the question. ep .c om 1. The medical-surgical nurse identifies a clinical practice issue and wants to determine if there is sufficient evidence to support a change in practice. Which type of study provides the strongest evidence to support a practice change? • Randomized control study • Quasi-experimental study • Case-control study • Cohort study ng te st pr 2. The medical-surgical unit recently implemented a patient-centered care model. Which action implemented by the nurse supports this model? • Evaluating care • Assessing needs • Diagnosing problems • Providing compassion .m yn ur si 3. Which action should the nurse implement when providing patient care in order to support The Joint Commission’s (TJC) National Patient Safety Goals (NPSG)? • Silencing a cardiorespiratory monitor • Identifying each patient using one source • Determining patient safety issues upon admission • Decreasing the amount of pain medication administered w w w 4. Which interprofessional role does the nurse often assume when providing patient care in an acute care setting? • Social worker • Client advocate • Care coordinator • Massage therapist 5. The medical-surgical nurse wants to determine if a policy change is needed for an identified clinical problem. Which is the first action the nurse should implement? • Developing a question • Disseminating the findings • Conducting a review of the literature • Evaluating outcomes of practice change 6. The nurse is evaluating the level of evidence found during a recent review of the literature. Which evidence carries the lowest level of support for a practice change? • Level IV • Level V • Level VI • Level VII ep .c om 7. The nurse is reviewing evidence from a quasi-experimental research study. Which level of evidence should the nurse identify for this research study? • Level I • Level II • Level III • Level IV te st pr 8. Which level of evidence should the nurse identify when reviewing evidence from a single descriptive research study? • Level IV • Level V • Level VI • Level VII .m yn ur si ng 9. Which statement should the nurse make when communicating the “S” in the SBAR approach for effective communication? • “The patient presented to the emergency department at 0200 with lower left abdominal pain.” • “The patient rated the pain upon admission as a 9 on a 10-point numeric scale.” • “The patient has no significant issues in the medical history.” • “The patient was given a prescribed opioid analgesic at 0300.” w w w 10. The staff nurse is communicating with the change nurse about the change of status of the patient. The nurse would begin her communication with which statement if correctly using the SBAR format? • “The patient’s heartrate is 110.” • “I think this patient needs to be transferred to the critical care unit.” • “The patient is a 68-year-old male patient admitted last night.” • “The patient is complaining of chest pain.” 11. Which nursing action exemplifies the Quality and Safety Education for Nursing (QSEN) competency of safety? • Advocating for a patient who is experiencing pain • Considering the patient’s culture when planning care • Evaluating patient learning style prior to implementing discharge instructions • Assessing the right drug prior to administering a prescribed patient medication • 12. Which type of nursing is the root of all other nursing practice areas? Pediatric nursing • • • Geriatric nursing Medical-surgical nursing Mental health-psychiatric nursing 13. Which did the Nursing Executive Center of The Advisory Board identify as an academic-practice gap for new graduate nurses? • Patient advocacy • Patient education om .c st • 14. Which statement regarding the use of the nursing process in clinical practice is accurate? “The nursing process is closely related to clinical decision-making.” “The nursing process is used by all members of the interprofessional team to plan care.” “The nursing process has 4 basic steps: assessment, planning, implementation, evaluation.” “The nursing process is being replaced by the implementation of evidence-based practice.” ep • • • Disease pathophysiology Therapeutic communication pr • • ng te 15. Which is the basis of nursing care practices and protocols? Assessment Evaluation Diagnosis Research si • • • • ur yn .m • • • • 16. Which is a common theme regarding patient dissatisfaction related to care provided in the hospital setting? Space in hospital rooms Medications received to treat pain Time spent with the health-care team Poor quality food received from dietary w w w 17. The nurse manager is preparing a medical-surgical unit for The Joint Commission (TJC) visit With the nurse manager presenting staff education focusing on TJC benchmarks, which of the following topics would be most appropriate? • Implementation of evidence-based practice • Implementation of patient-centered care • Implementation of medical asepsis practices • Implementation of interprofessional care 18. Which aspect of patient-centered care should the nurse manager evaluate prior to The Joint Commission site visit for accreditation? • Visitation rights • Education level of staff • Fall prevention protocol • Infection control practices 19. The medical-surgical nurse is providing patient care. Which circumstance would necessitate the nurse verifying the patient’s identification using at least two sources? • Prior to delivering a meal tray • Prior to passive range of motion • Prior to medication administration • Prior to documenting in the medical record ep .c om 20. The nurse is providing care to several patients on a medical-surgical unit. Which situation would necessitate the nurse to use SBAR during the hand-off process? • Wound care • Discharge to home • Transfer to radiology • Medication education pr Multiple Response te st Identify one or more choices that best complete the statement or answer the question. .m yn ur si ng 21. The staff nurse is teaching a group of student nurses the situations that necessitate hand-off communication. Which student responses indicate the need for further education related to this procedure? Select all that apply. • “A hand-off is required prior to administering a medication.” • “A hand-off is required during change of shift.” • “A hand-off is required for a patient is transferred to the surgical suite.” • “A hand-off is required whenever the nurse receives a new patient assignment.” • “A hand-off is required prior to family visitation.” w w w • • • • • 22. Which actions by the nurse enhance patient safety during medication administration? Select all that apply. Answering the call bell while transporting medications for a different patient Identifying the patient using two sources prior to administering the medication Holding a medication if the patient’s diagnosis does not support its use Administering the medication two hours after the scheduled time Having another nurse verify the prescribed dose of insulin the patient is to receive 23. The medical-surgical nurse assumes care for a patient who is receiving continuous cardiopulmonary monitoring. Which actions by the nurse enhance safety for this patient? Select all that apply. • Silencing the alarm during family visitation • Assessing the alarm parameters at the start of the shift • Responding to the alarm in a timely fashion • Decreasing the alarm volume to enhance restful sleep • Adjusting alarm parameters based on specified practitioner prescription 24. The nurse is planning an interprofessional care conference for a patient who is approaching discharge from the hospital. Which members of the interprofessional team should the nurse invite to attend? Select all that apply. • Physician • Pharmacist • Unit secretary • Social worker • Home care aide pr ep .c om 25. The nurse manager wants to designate a member of the nursing team as the care coordinator for a patient who will require significant care during the hospitalization. Which skills should this nurse possess in order to assume this role? Select all that apply. • Effective clinical reasoning • Effective communication skills • Effective infection control procedures • Effective documentation • Effective intravenous skills te st Answer Section ng MULTIPLE CHOICE w w w .m yn ur si • ANS: 1 Chapter number and title: 1, Foundations for Medical Surgical Practice Chapter learning objective: Discussing the incorporation of evidence-based practices into medical-surgical nursing Chapter page reference: 003-004 Heading: Evidence-Based Nursing Care Integrated Processes: Nursing Process: Planning Client Need: Safe and Effective Care Environment/ Management of Care Cognitive level: Comprehension [Understanding] Concept: Evidence-Based Practice Difficulty: Easy 1 Feedback Systematic reviews of randomized control studies (Level I) are the highest level of evidence because they include data from selected studies that randomly assigned participants to control and experimental groups. The lower the numerical rating of the level of evidence indicates the highest level of evidence; therefore, this type of study provides the strongest evidence to support a practice change. Quasi-experimental studies are considered Feedback Systematic reviews of randomized control studies (Level I) are the highest level of evidence because they include data from selected studies that randomly assigned participants to control and experimental groups. The lower the numerical rating of the level of evidence indicates the highest level of evidence; therefore, this type of study provides the strongest evidence to support a practice change. Quasi-experimental studies are considered Level III; therefore, this study does not provide the strongest evidence to support a practice change. Case-control studies are considered Level IV; therefore, this study does not provide the strongest evidence to support a practice change. Cohort studies are considered Level IV; therefore, this study does not provide the strongest evidence to support a practice change. om 1 ep .c 2 st pr 3 ng te 4 w w w .m yn ur si PTS: 1 CON: Evidence-Based Practice • ANS: 4 Chapter number and title: 1, Foundations of Medical-Surgical Practice Chapter learning objective: Explaining the importance of patient-centered care in the management of medical- surgical patients Chapter page reference: 004-005 Heading: Patient-Centered Care in the Medical-Surgical Setting Integrated Processes: Caring Client Need: Psychosocial Integrity Cognitive level: Application [Applying] Concept: Nursing Roles Difficulty: Moderate 1 2 Feedback Evaluation is a step in the nursing process; however, this is not an action that supports the patient-centered care model. Assessment is a step in the nursing process; however, this is not an action that supports the patient-centered care model. Diagnosis is a step in the nursing process; however, this is not an action that supports the patient-centered care model. Compassion is a competency closely associated with patient-centered care; therefore, this action supports the patient-centered model of care. 3 4 w w 1 w .m yn ur si ng te st pr ep .c om PTS: 1 CON: Nursing Roles • ANS: 3 Chapter number and title: 1, Foundations of Medical-Surgical Nursing Practice Chapter learning objective: Discussing implications to medical-surgical nurses of Quality and Safety Education for Nurses (QSEN) competencies Chapter page reference: 005-006 Heading: Patient Safety Outcomes Integrated Processes: Nursing Process: Implementation Client Need: Safe and Effective Care Environment/ Management of Care Cognitive level: Application [Applying] Conce pt: Safety Diffic ulty: Mode rate 2 3 4 Feedback Safely using alarms is a NPSG identified by TJC. Silencing a cardiorespiratory monitor is not nursing action that supports this NPSG. Patient identification using two separate resources is a NPSG identified by TJC. Identifying a patient using only one source does not support this NPSG. Identification of patient safety risks is a NPSG identified by the TJC. Determining patient safety issues upon admission supports this NPSG. Safe use of medication is a NPSG identified by the TJC. Decreasing the amount of pain medication administered does not support this NPSG. does not support this NPSG. Identification of patient safety risks is a NPSG identified by the TJC. Determining patient safety issues upon admission supports this NPSG. Safe use of medication is a NPSG identified by the TJC. Decreasing the amount of pain medication administered does not support this NPSG. 3 4 te st pr ep .c om PTS: 1 CON: Safety • ANS: 3 Chapter number and title: 1, Foundations of Medical-Surgical Nursing Practice Chapter learning objective: Describing the role and competencies of medical-surgical nursing Chapter page reference: 006-007 Heading: Interprofessional Collaboration and Communication Integrated Processes: Nursing Process: Implementation Client Need: Safe and Effective Care Environment/ Management of Care Cognitive level: Comprehension [Understanding] Concept: Nursing Roles Difficult y: Easy ng ur si 1 .m yn 2 w w w 3 4 Feedback The nurse does not often assume the interprofessional role of social worker when providing patient care in an acute care setting. The nurse does not often assume the interprofessional role of client advocate role when providing patient care in an acute care setting. The nurse often assumes the interprofessional role of care coordinator when providing patient care in an acute care setting. The nurse does not often assume the interprofessional role of massage therapist when providing patient care in an acute care setting. PTS: 1 CON: Nursing Roles • ANS: 1 Chapter number and title: 1, Foundations of Medical-Surgical Practice Chapter learning objective: Discussing the incorporation of evidence-based practices into medical-surgical nursing Chapter page reference: 003 Heading: Box 1.3 Steps of Evidence- Based Practice Integrated Processes: Nursing Process: Implementation Client Need: Safe and Effective Care Environment/ Management of Care Cognitive level: Analysis [Analyzing] Concept: Evidence-Based Practice Difficulty: Difficult om Feedback The first step of evidence-based practice is to develop a question based on the clinical issue. The last step of evidence-based practice is to disseminate findings. The second step of evidence-based practice is to conduct a review of the literature, or current evidence, available. The fifth step of evidence-based practice is to evaluate the outcomes associated with the practice change. .c 1 ep 2 pr 3 te st 4 w w w .m yn ur si ng PTS: 1 CON: Evidence-Based Practice • ANS: 4 Chapter number and title: 1, Foundations of Medical-Surgical Nursing Practice Chapter learning objective: Discussing the incorporation of evidence-based practices into medical-surgical nursing Chapter page reference: 004 Heading: Box 1.4 Evaluating Levels of Evidence Integrated Processes: Nursing Process: Planning Client Need: Safe and Effective Care Environment/ Management of Care Cognitive level: Comprehension [Understanding] Concept: Evidence-Based Practice Difficulty: Easy 1 2 3 Feedback The lower the numeric value of the evidence the greater the support for a change in practice. Level IV evidence does not carry the lowest level of support for a practice change. The lower the numeric value of the evidence the greater the support for a change in practice. Level V evidence does not carry the lowest level of support for a practice change. The lower the numeric value of the evidence the greater the support for a change in The lower the numeric value of the evidence the greater the support for a change in practice. Level IV evidence does not carry the lowest level of support for a practice change. The lower the numeric value of the evidence the greater the support for a change in practice. Level V evidence does not carry the lowest level of support for a practice change. The lower the numeric value of the evidence the greater the support for a change in practice. Level VI evidence does not carry the lowest level of support for a practice change. The lower the numeric value of the evidence the greater the support for a change in practice. Level VII evidence carries the lowest level of support for a practice change. 1 2 3 om 4 w w 2 w 1 .m yn ur si ng te st pr ep .c PTS: 1 CON: Evidence-Based Practice • ANS: 3 Chapter number and title: 1, Foundations of Medical-Surgical Nursing Practice Chapter learning objective: Discussing the incorporation of evidence-based practices into medical-surgical nursing Chapter page reference: 004 Heading: Box 1.4 Evaluating Levels of Evidence Integrated Processes: Nursing Process: Implementation Client Need: Safe and Effective Care Environment/ Management of Care Cognitive level: Application [Applying] Concept: Evidence-Based Practice Difficulty: Moderate 3 4 Feedback A systemic review of randomized controlled studies, not a quasi-experimental research study, is identified as Level I. Evidence from at least one study randomized control study, not a quasi-experimental research study, is identified as Level II. A quasi-experimental research study is identified as a Level III. Evidence from case-control or cohort studies, not a quasi-experimental research study, is identified as a Level IV. PTS: 1 CON: Evidence-Based Practice • ANS: 3 Chapter number and title: 1, Foundations of Medical-Surgical Nursing Practice .c om Chapter learning objective: Discussing the incorporation of evidence-based practices into medical-surgical nursing Chapter page reference: 004 Heading: Box 1.4 Evaluating Levels of Evidence Integrated Processes: Nursing Process: Implementation Client Need: Safe and Effective Care Environment/ Management of Care Cognitive level: Application [Applying] Concept: Evidence-Based Practice Difficulty: Moderate ep Feedback Evidence from case-control or cohort studies, not a single descriptive research study, is identified as a Level IV. Evidence from systemic reviews of descriptive or qualitative studies, not a single descriptive research study, is identified as Level V. Evidence from a single descriptive research study is identified as Level VI. Evidence from expert individual authorities or committees, not a single descriptive research study, is identified as Level VII. st pr 1 te 2 si ng 3 ur 4 w w .m yn PTS: 1 CON: Evidence-Based Practice • ANS: 1 Chapter number and title: 1, Foundations of Medical-Surgical Nursing Practice Chapter learning objective: Describing the role of interprofessional collaboration and teamwork in the provision of safe, quality patient care w Chapter page reference: 005 Heading: Box 1.6 The SBAR Approach for Effective Communication Integrated Processes: Nursing Process: Implementation Client Need: Safe and Effective Care Environment/ Management of Care Cognitive level: Application [Applying] Concept: Communic ation Difficulty: Moderate Feedback The “S” reflects the patient’s current situation which is communicated by providing a brief statement of the issue. This statement by the nurse exemplifies the current situation. The “A” reflects the patient’s assessment data. This statement by the nurse exemplifies the patent’s assessment data. The “B” reflects the patient’s medical history. This statement by the nurse exemplifies communicating the patient’s history related to the current problem. The “R” reflects specific actions needed to address the situation. This statement by the nurse exemplifies the actions implemented to address current level of pain. 1 2 .c om 3 pr ep 4 w w w .m yn ur si ng te st PTS: 1 CON: Communication • ANS: 4 Chapter number and title: 1, Foundations of Medical-Surgical Nursing Practice Chapter learning objective: Describing the role of interprofessional collaboration and teamwork in the provision of safe, quality patient care Chapter page reference: 005 Heading: Box 1.6 The SBAR Approach for Effective Communication Integrated Processes: Nursing Process: Planning Client Need: Safe and Effective Care Environment/ Management of Care Cognitive level: Analysis [Analyzing] Concept: Communic ation Difficulty: Moderate 1 2 3 4 Feedback This statement is the “A” in the SBAR communication. This is an assessment finding by the staff nurse. This statement is the “R” in the SBAR communication. This is the recommendation by the staff nurse. This statement is the “B” in the SBAR communication. This is the background information. This statement is the “S” in the SBAR communication. This is the situation information. by the staff nurse. This statement is the “R” in the SBAR communication. This is the recommendation by the staff nurse. This statement is the “B” in the SBAR communication. This is the background information. This statement is the “S” in the SBAR communication. This is the situation information. 2 3 4 yn ur pr si ng te st Integrated Processes: Nursing Process: Implementation Client Need: Safe and Effective Care Environment/ Management of Care Cognitive level: Application [Applying] Conce pt: Safety Diffic ulty: Mode rate ep .c om PTS: 1 CON: Communication • ANS: 4 Chapter number and title: 1, Foundations of Medical-Surgical Nursing Practice Chapter learning objective: Discussing implications to medical-surgical nurses of Quality and Safety Education for Nurses (QSEN) competencies Chapter page reference: 006 Heading: Box 1.8 Quality and Safety Education for Nursing (QSEN) Competencies w w w 2 .m 1 3 4 Feedback Advocating for a patient who is in pain exemplifies the QSEN competency of patientcentered care, not safety. Considering the patient’s cultural background exemplifies the QSEN competency of patient-centered care, not safety. Evaluating the patient’s learning style prior to implementing discharge instructions exemplifies the QSEN competency of patientcentered care, not safety. Assessing the right drug prior to administering a prescribed medication exemplifies the QSEN competency of safety. PTS: 1 CON: Safety • ANS: 3 Chapter number and title: 1, Foundations of Medical-Surgical Nursing Practice Chapter learning objective: Describing the role and competencies of om .c ep pr medical-surgical nursing Chapter page reference: 002 Heading: Introduction Integrated Processes: Nursing Process: Planning Client Need: Safe and Effective Care Environment/ Management of Care Cognitive level: Knowledge [Remembering] Co nce pt: Nu rsi ng Dif fic ult y: Eas y st Feedback Pediatric nursing is not the root of all nursing practice areas. Geriatric nursing is not the root of all nursing practice areas. Medical-surgical nursing is the root of all nursing practice as care provided here can be implemented in all other areas of nursing practice. Mental health-psychiatric nursing is not the root of all nursing practice areas. te 1 si ng 2 yn ur 3 .m 4 w w w PTS: 1 CON: Nursing • ANS: 3 Chapter number and title: 1, Foundations of Medical-Surgical Nursing Practice Chapter learning objective: Describing the role and competencies of medical-surgical nursing Chapter page reference: 002-003 Heading: Competencies in MedicalSurgical Nursing Integrated Processes: Teaching and Learning Client Need: Physiological Integrity/ Physiological Adaptation Cognitive level: Knowledge [Remembering] Concept: Critical Thinking Difficulty: Easy Feedback Patient advocacy is not identified as an academic-practice gap for new graduate nurses. 1 Patient education is not identified as an academic-practice gap for new graduate nurses. Knowledge of pathophysiology of patient conditions is identified as an academicpractice gap for new graduate nurses. Therapeutic communication is not identified as an academic-practice gap for new graduate nurses. om 2 .c 3 pr ep 4 w w w .m yn ur si ng te st PTS: 1 CON: Critical Thinking • ANS: 1 Chapter number and title: 1, Foundations of Medical-Surgical Nursing Practice” Chapter learning objective: Describing the role and competencies of medical-surgical nursing Chapter page reference: 003 Heading: Competencies Related to the Nursing Process Integrated Processes: Teaching and Learning Client Need: Safe and Effective Care Environment/ Management of Care Cognitive level: Comprehension [Understanding] Concept: Critical Thinking Difficulty: Easy 1 2 3 4 Feedback The nursing process is closely related to the nurse’s decision-making in the clinical environment. This statement is accurate. The nursing process is not used by all members of the interprofessional team to plan care. The nursing process has 5, not 4, basic steps: assessment, diagnosis, planning, implementation, and evaluation. The nursing process is not being replaced by the implementation of evidence-based practice. 2 members of the interprofessional team to plan care. The nursing process has 5, not 4, basic steps: assessment, diagnosis, planning, implementation, and evaluation. The nursing process is not being replaced by the implementation of evidence-based practice. 3 4 te st pr ep .c om PTS: 1 CON: Critical Thinking • ANS: 4 Chapter number and title: 1, Foundations for Medical-Surgical Nursing Practice Chapter learning objective: Discussing the incorporation of evidence-based practices into medical-surgical nursing Chapter page reference: 003-004 Heading: Evidence-Based Nursing Care Integrated Processes: Teaching and Learning Client Need: Safe and Effective Care Environment/ Management of Care Cognitive level: Knowledge [Remembering] Concept: Evidence-Based Practice Difficulty: Easy ng ur si 1 yn 2 w w w .m 3 4 Feedback Assessment is a step in the nursing process; however, this is not the basis for nursing care practices and protocols. Evaluation is a step in the nursing process; however, this is not the basis for nursing care practices and protocols. Diagnosis is a step in the nursing process; however, this is not the basis for nursing care practices and protocols. Evidence that is obtained through research is the basis for nursing care practices and protocols. PTS: 1 CON: Evidence-Based Practice • ANS: 3 Chapter number and title: 1, Foundations of Medical-Surgical Nursing Practice Chapter learning objective: Explaining the importance of patient-centered care in the management of medical- surgical patients Chapter page reference: 004-005 Heading: Patient-Centered Care in the Medical-Surgical Setting Integrated Processes: Teaching and Learning Client Need: Safe and Effective Care Environment/ Management of Care Cognitive level: Knowledge [Remembering] Concept: Communic ation Difficulty: Easy Feedback Space in each hospital room is not a common theme of patient dissatisfaction. Medications received for pain management is not a common theme of patient dissatisfaction. A lack of time with members of the health care team is a common theme of patient dissatisfaction. Poor food quality is not a common theme of patient dissatisfaction. om 1 ep .c 2 pr 3 te st 4 w w w .m yn ur si ng PTS: 1 CON: Communication • ANS: 2 Chapter number and title: 1, Foundations of Medical-Surgical Nursing Practice Chapter learning objective: Explaining the importance of patient-centered care in the management of medical- surgical patients Chapter page reference: 004-005 Heading: Patient-Centered Care in the Medical-Surgical Setting Integrated Processes: Teaching and Learning Client Need: Safe and Effective Care Environment/ Management of Care Cognitive level: Application [Applying] Concept: Quality Improvement Difficulty: Moderate 1 2 3 4 Feedback Implementation of evidence-based practice is not the benchmark in which acute care facilities are evaluated against. Implementation of patient-centered care is the benchmark in which acute care facilities are evaluated against. Implementation of medical asepsis practices is not the benchmark in which acute care facilities are evaluated against. Implementation of interprofessional care is not the benchmark in which acute care facilities are evaluated against. 1 not the benchmark in which acute care facilities are evaluated against. Implementation of patient-centered care is the benchmark in which acute care facilities are evaluated against. Implementation of medical asepsis practices is not the benchmark in which acute care facilities are evaluated against. Implementation of interprofessional care is not the benchmark in which acute care facilities are evaluated against. 2 3 4 PTS: 1 CON: Quality Improvement • ANS: 1 yn ur si ng te st pr ep .c om Chapter number and title: 1, Foundations of Medical-Surgical Nursing Practice Chapter learning objective: Explaining the importance of patient-centered care in the management of medical- surgical patients Chapter page reference: 004-005 Heading: Patient-Centered Care in the Medical-Surgical Setting Integrated Processes: Nursing Process: Planning Client Need: Safe and Effective Care Environment/ Management of Care Cognitive level: Application [Applying] Concept: Quality Improvement Difficulty: Moderate w w 2 w .m 1 3 4 Feedback Visitation rights should be evaluated prior to a TJC accreditation site visit as this aspect of patient-centered care is incorporated into the site evaluation. The education level of staff is not evaluated prior to a TJC accreditation visit. This information should be evaluated for a hospital that is attempting to earn Magnet status. While the fall prevention program will be reviewed during a TJC accreditation site visit this is not an aspect of patient-centered care. While infection control practices will be reviewed during a TJC accreditation site visit this is not an aspect of patient-centered care. PTS: 1 CON: Quality Improvement • ANS: 3 Chapter number and title: 1, Foundations of Medical-Surgical Practice Chapter learning objective: Discussing implications to medical-surgical nurses om .c ep of Quality and Safety Education for Nurses (QSEN) competencies Chapter page reference: 005-006 Heading: Patient Safety Outcomes Integrated Processes: Nursing Process: Planning Client Need: Safe and Effective Care Environment/Safety and Infection Control Cognitive level: Application [Applying] Conce pt: Safety Diffic ulty: Mode rate st pr Feedback While the nurse should take care to deliver the meal tray to the correct patient this circumstance does not require verification of patient identity through two sources. While the nurse should take care to implement passive range of motion on the correct patient this circumstance does not require verification of patient identity through two sources. The nurse should identify a patient using two sources prior to medication administration. While the nurse should take care to document patient care in the correct medical record this circumstance does not require verification of patient identity through two sources. ng te 1 yn ur si 2 .m 3 w w 4 w PTS: 1 CON: Safety • ANS: 3 Chapter number and title: 1, Foundations of Medical-Surgical Nursing Practice Chapter learning objective: Describing the role of interprofessional collaboration and teamwork in the provision of safe, quality patient care Chapter page reference: 005-006 Heading: Patient Safety Outcomes Integrated Processes: Nursing Process: Implementation Client Need: Safe and Effective Care Environment/ Management of Care Cognitive level: Application [Applying] Concept: Communication, Safety Difficulty: Moderate .c om 1 Feedback Effective staff communication is essential to safe patient care, especially during hand- offs. Implementation of wound care is not an example of a hand-off situation. Effective staff communication is essential to safe patient care, especially during hand- offs. Discharge to home is not an example of a hand-off situation. Effective staff communication is essential to safe patient care, especially during hand- offs. Patient transfer to another unit of the hospital necessitate a change in who is responsible for direct patient care; therefore, this situation would necessitate the need for SBAR during the hand-off process. Effective staff communication is essential to safe patient care, especially during hand- offs. Medication education is not an example of a hand-off situation. st pr ep 2 si ng te 3 yn ur 4 CON: Communication | Safety .m PTS: 1 w MULTIPLE RESPONSE w w 21. ANS: 2, 3, 4 Chapter number and title: 1, Foundations of Medical-Surgical Nursing Practice Chapter learning objective: Describing the role of interprofessional collaboration and teamwork in the provision of safe, quality patient care Chapter page reference: 005-006 Heading: Patient Safety Outcomes Integrated Processes: Teaching and Learning Client Need: Safe and Effective Care Environment/ Management of Care Cognitive level: Analysis [Analyzing] Concept: Communic ation Difficulty: Difficult om 1. Feedback This is incorrect. Hand-off communication is not required prior to the administration of medication. The nurse would, however, verify the patient’s identity using two sources. This is correct. Hand-off communication is required when patient care is transferred from one provider to another, such as during the change of shift. This is correct. Hand-off communication is required when patient care is transferred from one provider to another, such as when a patient is transferred to the surgical suite. This is correct. Hand-off communication is required when patient care is transferred from one provider to another, such as anytime the nurse receives a new patient assignment. This is incorrect. Hand-off communication is not required prior to family visitation. ep .c 2. st pr 3. ng te 4. ur si 5. w w w .m yn PTS: 1 CON: Communication 22. ANS: 2, 3, 5 Chapter number and title: 1, Foundations of Medical-Surgical Nursing Practice Chapter learning objective: Discussing implications to medical-surgical nurses of Quality and Safety Education for Nurses (QSEN) competencies Chapter page reference: 005-006 Heading: Patient Safety Outcomes Integrated Processes: Nursing Process: Implementation Client Need: Safe and Effective Care Environment/Safety and Infection Control Cognitive level: Application [Applying] Conce pt: Safety Diffic ulty: Mode rate om 1. Feedback This is incorrect. Interruptions should be minimized during the medication administration process; therefore, the nurse should not answer the call bell for another patient while transporting medications for administration. This is correct. Verification of the right patient is one of the rights of medication administration; therefore, the nurse would identify the patient using two sources prior to the administration of medication. This is correct. The nurse should ensure that the rationale for all medications are associated with the patient condition; therefore, this action enhances patient safety during medication administration. This is incorrect. One of the rights of medication administration is the right time, which correlates to 30 minutes before or 30 minutes after the scheduled time. This nursing action would not enhance patient safety during medication administration. This is correct. Verifying the dose of a highrisk medication, such as insulin, enhances patient safety during medication administration. pr ep .c 2. ng te st 3. yn ur si 4. w .m 5. w PTS: 1 w CON: Safety 23. ANS: 2, 3, 5 Chapter number and title: 1, Foundations of Medical-Surgical Nursing Practice Chapter learning objective: Discussing implications to medical-surgical nurses of Quality and Safety Education for Nurses (QSEN) competencies Chapter page reference: 005-006 Heading: Patient Safety om Outcomes Integrated Processes: Nursing Process: Implementation Client Need: Safe and Effective Care Environment/Safety and Infection Control Cognitive level: Analysis [Analyzing] Conce pt: Safety Diffic ulty: Diffic ult .c Feedback This is incorrect. Monitor alarms should be audible even during family visitation. Inaudible alarms may impede patient safety. This is correct. The nurse should assess the alarm parameters, comparing to the prescribed settings, at the start of each shift. This action enhanced patient safety. pr ep 1. te st 2. This is correct. The nurse should respond to all alarms in a timely fashion, which enhances patient safety. This is incorrect. Monitor alarms should be audible at all times, even when the patient is asleep to enhance patient safety. This is correct. The nurse should adjust alarm parameters based on specific practitioner prescriptions. This action enhances safety. ng si 3. yn ur 4. .m 5. w w PTS: 1 w CON: Safety 24. ANS: 1, 2, 4 Chapter number and title: 1, Foundations of Medical-Surgical Nursing Practice Chapter learning objective: Describing the role of interprofessional collaboration and teamwork in the provision of safe, quality patient care Chapter page reference: 006-007 Heading: Interprofessional Collaboration and Communication Integrated Processes: Nursing Process: Planning om Client Need: Safe and Effective Care Environment/ Management of Care Cognitive level: Application [Applying] Concept : Collabor ation Difficult y: Moderat e .c Feedback This is correct. The physician is a member of the interprofessional team and should be invited to participate in the care conference. This is correct. The pharmacist is a member of the interprofessional team and should be invited to participate in the care conference. This is incorrect. The unit secretary is not a member of the interprofssional team; therefore, would not require an invitation to attend the care conference. This is correct. The social worker is a member of the interprofessional team; therefore, should be invited to participate in the care conference. This is incorrect. The home care aide, while a member of the interprofessional team, would not benefit from attending a care conference while the patient is hospitalized. ep 1. st pr 2. si ng te 3. yn ur 4. w .m 5. w w PTS: 1 CON: Collaboration 25. ANS: 1, 2, 4 Chapter number and title: 1, Foundation of Medical-Surgical Nursing Practice Chapter learning objective: Describing the role of interprofessional collaboration and teamwork in the provision of safe, quality patient care Chapter page reference: 006-007 Heading: Interprofessional Collaboration and Communication Integrated Processes: Nursing Process: Planning Client Need: Safe and Effective Care Environment/ Management of Care Cognitive level: Analysis [Analyzing] Concept : Collabor ation Difficult y: Difficult om Feedback This is correct. Effective clinical reasoning is a skill required for the nurse to assume the role of care coordinator. .c 1. ep This is correct. Effective communication is a skill required for the nurse to assume the role of care coordinator. This is incorrect. Effective infection control procedures are expected to meet the standard of care; however, this skill is not required for the nurse to assume the role of care coordinator. This is correct. Effective documentation, a form of communication, is a skill required for the nurse to assume the role of care coordinator. This is incorrect. Effective intravenous skills are not required for the nurse to assume the role of care coordinator. st pr 2. ng te 3. ur si 4. .m yn 5. CON: Collaboration w w w PTS: 1 Chapter 2: Nursing Process Multiple Choice Identify the choice that best completes the statement or answers the question. 1. The home care nurse is planning care for a diabetic patient requiring an extensive dressing change twice a day, assistance with activities of daily living (ADLs), and comprehensive education. Which role is the nurse assuming by coordinating the care this patient requires? • • • • Collaborator Case manager Health educator Health promoter om 2. The nurse is discussing follow-up care with a patient who is being discharged. The patient and family cross their arms and state angrily that the team's suggestions are not acceptable. Which response by the nurse is appropriate? • “We only want what's best for you.” • “We will leave you alone to discuss your options.” • “Perhaps you did not understand the recommendations.” • “Let's discuss other options that might work well for you and your family.” st pr ep .c 3. The nurse is preparing a patient for discharge who will be requiring physical therapy (PT) to rehabilitate after a total knee replacement. After reading the health-care provider’s order for PT, which would be the nurse's initial action? • Teach the family the exercises needed for the patient. • Call home health and schedule a therapist to visit the home for therapy. • Set up appointments according to the order with the hospital PT department. • Discuss the various types of settings for therapy and have the patient choose the venue. ur si ng te 4. The nurse is caring for a patient with rheumatoid arthritis who expresses the desire to remain active as long as possible. In order for the patient to meet this goal, what should the nurse prepare to do? • Tell the patient there is no hope. • Ask the patient the reason for the decision. • Teach the patient nutrition and joint exercises. • Refer the patient to the appropriate professionals. w w w .m yn 5. A nurse is working as the designated leader of a group of health-care providers in a community clinic setting. The team members are working to decrease the number of adolescent pregnancies in the community. They have defined the problem and are now focusing on objectives and considering various viewpoints presented by the group. The nurse is tasked with helping the team to stay focused in order to address the defined problem. Which competency of collaboration does this describe? • Trust • Mutual respect • Communication • Decision making 6. The nurse managers in a community hospital have been charged with reviewing job descriptions of unlicensed assistive personnel (UAPs) and have questions about the delegation of certain patient care activities to UAPs by nurses. To which group, organization, or individual would committee members direct their questions to obtain definitive answers about the parameters of nurse delegation to UAPs? • The state board of nursing • The American Nurses Association • • The hospital's Chief Nursing Officer The hospital's Chief Executive Officer ep .c om 7. Which statement is a primary and historical barrier to effective nurse-physician collaboration that has persisted over time? • The view among the general population that nurses’ contributions to patients’ care is less important to their health and well-being compared to the contribution of physicians • The nurses’ and physicians’ perceptions of inequity in their roles, with nurses assuming a subservient role and physicians assuming leadership and superior role in health-care settings • A general lack of education provided in schools for health professionals about the benefits on health-care quality linked • A lack of published evidence about the effectiveness of collaborative efforts among and between nurses and physicians to nurse-physician collaboration ng te st pr 8. A patient with Type 1 diabetes mellitus has developed an open sore on the shin and is having trouble meeting daily goals for exercising. The patient is scheduled for discharge in a couple of days. When planning for this patient’s continued care, who will the nurse notify regarding the patient’s needs after discharge? • The pharmacy • The case manager • The physical therapist • The occupational therapist .m yn ur si 9. A patient who is recovering from coronary bypass surgery is placed on a critical pathway for extended care. Which patient statement indicates appropriate understanding of the plan of care? • “I cannot alter the critical pathway plan.” • “I must be able to meet goals that are set for me.” • “My insurance plan can deny payment if I do not meet goals.” • “The chosen critical pathway can be altered to meet my needs.” w w w 10. The case manager interviews an older adult patient hospitalized after hip replacement surgery. The patient requires in-patient rehabilitation prior to being discharged home. The case manager works with the hospital nursing staff, the rehabilitation center, the patient’s family members, and other care providers to assist with a smooth transition. Which is the primary goal of the care management model described here? • To provide greater peace of mind for the patient and his or her family members • • • To track a patient’s progress to ensure that appropriate care is provided until discharge To manage concerns that are related to the patient’s medical care and treatment regimen only To provide a continuum of clinical services in order to help contain costs and improve patient outcomes 11. The patient’s case manager, diabetes educator, and dietician meet to discuss the patient’s needs in preparation for discharge to home. The patient’s primary health-care provider arrives and states, “I will be making all decisions regarding the patient’s discharge care.” With the primary health-care provider’s decision to lead the team, the dynamic has shifted between which two types of teams? • Intradisciplinary to interdisciplinary team • Multidisciplinary to intradisciplinary team • Interprofessional to interdisciplinary team • Interdisciplinary to multidisciplinary team ng te st pr ep .c om 12. A school-age patient is admitted to the pediatric intensive care unit (PICU), unconscious and with multiple traumatic injuries, after a skateboard accident that included a closed head injury. Many health professionals are involved in the patient’s care and the scene is chaotic. The parents are extremely anxious and want to know what is happening. The case manager asks for an interdisciplinary team meeting to speak with the patient’s parents. Which is the rationale for this meeting? • To allow for each specialty to practice independently • To share and evaluate information for care planning and implementation, and prevent priority conflicts, redundancy, and omissions in care • To all the primary health-care provider to make all the decision regarding the patient’s care • To prevent the parents from trying to change the plan of care w .m yn ur si 13. The Chief Nursing Officer and Chief Medical Officer in an urban teaching hospital are leading a series of meetings with nurses, physicians, hospital lawyers, and risk managers to review and update hospital privileging procedures and requirements for advanced practice RNs and physicians new to the hospital. This is an example of which type of collaborative team? • Intradisciplinary • Interdisciplinary • Multidisciplinary • Complementary w w 14. A local hospital formed a neurotrauma (NT) team with the following members: acute care nurses, physicians, other care partners (e.g., physical therapists, social workers, case managers, dieticians), and representatives from the NT outpatient clinic. This team is led by a physician who makes treatment decisions based on the treatment plans developed by individual team members who each communicate with the patients, asking the same or similar questions to obtain data needed for their treatment plan. Which type of communication and action is represented in the scenario described? • Parallel communication • Parallel functioning • Information exchange • Coordination and consultation 15. The nurse is caring for a patient who is reporting pain of 8/10 on a 1 to 10 numeric pain scale. The nurse administers the prescribed pain medication. When the nurse re-evaluates the patient one hour later, the patient is still reporting pain of 8/10. Which action by the nurse is appropriate at this time? • Wait for the health-care provider to make rounds to report the problem. • • • Report to the health-care provider by telephone. Increase the dosage of the medication. Include in the nursing report that the medication is ineffective. pr ep .c om 16. Handoff communication, the transfer of information during transitions in care such as during change-of-shift report, includes an opportunity to ask questions, clarify, and confirm the information between sender and receiver. Which is the main objective for ensuring effective communication during a patient handoff? • To avoid lawsuits • To ensure patient safety • To facilitate quality improvement • To make sure all documentation is done ur si ng te st 17. The nurse is providing care to a patient diagnosed with end-stage renal disease. When planning a care plan conference for this patient, who does the nurse invite to participate? • The oncologist • The psychiatrist • The hospital CEO • The family members w w .m yn 18. Which should be the focus of an educational session for nurses and other members of the interdisciplinary team when addressing high rates of patient readmission to the health system? • Medication errors • Coordination of care • Adverse clinical events • Roles of each member providing care w 19. Which patient population should the nurse focus on to increase access to care that is coordinated, safe, and focused on the patient’s unique needs across all care settings? • Pediatric patients • Older adult patients • Young adult patients • Acute needs patients 20. Which is a basic principle of the Patient Protection and Affordable Care Act of 2010 that the nurse should include in a teaching session for members of the health-care team? • Decreased access • Decreased cost of care • • Decreased quality of care Decreased safety Multiple Response Identify one or more choices that best complete the statement or answer the question. st Increased overall cost of health-care services Decreased patient morbidity and mortality Decreased level of job satisfaction te • • • pr ep .c om 21. The hospital’s nurse case manager has been extensively involved with a shooting victim and members of the patient’s family in coordinating care of providers from many disciplines as the patient progressed from the emergency department (ED) to the intensive care unit (ICU), and then onto the medical-surgical unit. After three weeks of hospitalization, the case manager is helping to prepare the patient for discharge to a rehabilitation center where treatment will continue. Which outcomes have been documented in the literature as benefits of such collaboration? Select all that apply. • Improved patient outcomes • Decreased duplication of health-care services .m yn ur si ng 22. The case manager assembles a team of health-care professionals, including the patient’s primary health-care provider, physical therapist, and social worker, for the purpose of collaborative discharge planning and decision making. Which type of team did the case manager assemble? Select all that apply. • Management • Intradisciplinary • Interdisciplinary • Interprofessional • Primary nursing care w w w 23. The nurse is preparing to document care provided to the patient during the day shift. The nurse documents that the patient experienced an increased pain level while ambulating which required an extra dose of pain medication; took a shower; visited with family; and ate a small lunch. Which information is important to include during the oral end-of-shift reporting? Select all that apply. • The last antibiotics given • The patient’s taking a shower • The patient’s visit with family • The extra dose of pain medication • The patient’s response to ambulation 24. When the nurse receives a telephone order from the health-care provider's office, which guidelines are used to ensure the order is correct? Select all that apply. • Ask the prescriber to speak slowly. • Read the order back to the prescriber. • Know agency policy for telephone orders. • • Sign the prescriber’s name and credentials. Ask the prescriber to repeat or spell out medication. .c om 25. When discussing the importance of interprofessional collaboration, which advantages should the nurse include? Select all that apply. • Improved team member satisfaction • Increased division among team members • Increased safety with medication administration • Enhanced communication among team members • Increased patient satisfaction with discharge transition process Chapter 2 Nursing Process Multiple Choice Identify the choice that best completes the statement or answers the question. te st pr ep 1. The home care nurse is planning care for a diabetic patient requiring an extensive dressing change twice a day, assistance with activities of daily living (ADLs), and comprehensive education. Which role is the nurse assuming by coordinating the care this patient requires? • Collaborator • Case manager • Health educator • Health promoter yn ur si ng 2. The nurse is discussing follow-up care with a patient who is being discharged. The patient and family cross their arms and state angrily that the team's suggestions are not acceptable. Which response by the nurse is appropriate? • “We only want what's best for you.” • “We will leave you alone to discuss your options.” • “Perhaps you did not understand the recommendations.” • “Let's discuss other options that might work well for you and your family.” w w w .m 3. The nurse is preparing a patient for discharge who will be requiring physical therapy (PT) to rehabilitate after a total knee replacement. After reading the health-care provider’s order for PT, which would be the nurse's initial action? • Teach the family the exercises needed for the patient. • Call home health and schedule a therapist to visit the home for therapy. • Set up appointments according to the order with the hospital PT department. • Discuss the various types of settings for therapy and have the patient choose the venue. 4. The nurse is caring for a patient with rheumatoid arthritis who expresses the desire to remain active as long as possible. In order for the patient to meet this goal, what should the nurse prepare to do? • Tell the patient there is no hope. • Ask the patient the reason for the decision. • Teach the patient nutrition and joint exercises. • Refer the patient to the appropriate professionals. om 5. A nurse is working as the designated leader of a group of health-care providers in a community clinic setting. The team members are working to decrease the number of adolescent pregnancies in the community. They have defined the problem and are now focusing on objectives and considering various viewpoints presented by the group. The nurse is tasked with helping the team to stay focused in order to address the defined problem. Which competency of collaboration does this describe? • Trust • Mutual respect • Communication • Decision making te st pr ep .c 6. The nurse managers in a community hospital have been charged with reviewing job descriptions of unlicensed assistive personnel (UAPs) and have questions about the delegation of certain patient care activities to UAPs by nurses. To which group, organization, or individual would committee members direct their questions to obtain definitive answers about the parameters of nurse delegation to UAPs? • The state board of nursing • The American Nurses Association • The hospital's Chief Nursing Officer • The hospital's Chief Executive Officer w w .m yn ur si ng 7. Which statement is a primary and historical barrier to effective nurse-physician collaboration that has persisted over time? • The view among the general population that nurses’ contributions to patients’ care is less important to their health and well-being compared to the contribution of physicians • The nurses’ and physicians’ perceptions of inequity in their roles, with nurses assuming a subservient role and physicians assuming leadership and superior role in health-care settings • A general lack of education provided in schools for health professionals about the benefits on health-care quality linked • A lack of published evidence about the effectiveness of collaborative efforts among and between nurses and physicians to nurse-physician collaboration w 8. A patient with Type 1 diabetes mellitus has developed an open sore on the shin and is having trouble meeting daily goals for exercising. The patient is scheduled for discharge in a couple of days. When planning for this patient’s continued care, who will the nurse notify regarding the patient’s needs after discharge? • The pharmacy • The case manager • The physical therapist • The occupational therapist 9. A patient who is recovering from coronary bypass surgery is placed on a critical pathway for extended care. Which patient statement indicates appropriate understanding of the plan of care? • • • • “I cannot alter the critical pathway plan.” “I must be able to meet goals that are set for me.” “My insurance plan can deny payment if I do not meet goals.” “The chosen critical pathway can be altered to meet my needs.” .c pr • To track a patient’s progress to ensure that appropriate care is provided until discharge To manage concerns that are related to the patient’s medical care and treatment regimen only To provide a continuum of clinical services in order to help contain costs and improve patient outcomes ep • • om 10. The case manager interviews an older adult patient hospitalized after hip replacement surgery. The patient requires in-patient rehabilitation prior to being discharged home. The case manager works with the hospital nursing staff, the rehabilitation center, the patient’s family members, and other care providers to assist with a smooth transition. Which is the primary goal of the care management model described here? • To provide greater peace of mind for the patient and his or her family members ur si ng te st 11. The patient’s case manager, diabetes educator, and dietician meet to discuss the patient’s needs in preparation for discharge to home. The patient’s primary health-care provider arrives and states, “I will be making all decisions regarding the patient’s discharge care.” With the primary health-care provider’s decision to lead the team, the dynamic has shifted between which two types of teams? • Intradisciplinary to interdisciplinary team • Multidisciplinary to intradisciplinary team • Interprofessional to interdisciplinary team • Interdisciplinary to multidisciplinary team w w w .m yn 12. A school-age patient is admitted to the pediatric intensive care unit (PICU), unconscious and with multiple traumatic injuries, after a skateboard accident that included a closed head injury. Many health professionals are involved in the patient’s care and the scene is chaotic. The parents are extremely anxious and want to know what is happening. The case manager asks for an interdisciplinary team meeting to speak with the patient’s parents. Which is the rationale for this meeting? • To allow for each specialty to practice independently • To share and evaluate information for care planning and implementation, and prevent priority conflicts, redundancy, and omissions in care • To all the primary health-care provider to make all the decision regarding the patient’s care • To prevent the parents from trying to change the plan of care 13. The Chief Nursing Officer and Chief Medical Officer in an urban teaching hospital are leading a series of meetings with nurses, physicians, hospital lawyers, and risk managers to review and update hospital privileging procedures and requirements for advanced practice RNs and physicians new to the hospital. This is an example of which type of collaborative team? • • • • Intradisciplinary Interdisciplinary Multidisciplinary Complementary ep .c om 14. A local hospital formed a neurotrauma (NT) team with the following members: acute care nurses, physicians, other care partners (e.g., physical therapists, social workers, case managers, dieticians), and representatives from the NT outpatient clinic. This team is led by a physician who makes treatment decisions based on the treatment plans developed by individual team members who each communicate with the patients, asking the same or similar questions to obtain data needed for their treatment plan. Which type of communication and action is represented in the scenario described? • Parallel communication • Parallel functioning • Information exchange • Coordination and consultation si Report to the health-care provider by telephone. Increase the dosage of the medication. Include in the nursing report that the medication is ineffective. ur • • • ng te st pr 15. The nurse is caring for a patient who is reporting pain of 8/10 on a 1 to 10 numeric pain scale. The nurse administers the prescribed pain medication. When the nurse re-evaluates the patient one hour later, the patient is still reporting pain of 8/10. Which action by the nurse is appropriate at this time? • Wait for the health-care provider to make rounds to report the problem. w w .m yn 16. Handoff communication, the transfer of information during transitions in care such as during change-of-shift report, includes an opportunity to ask questions, clarify, and confirm the information between sender and receiver. Which is the main objective for ensuring effective communication during a patient handoff? • To avoid lawsuits • To ensure patient safety • To facilitate quality improvement • To make sure all documentation is done w 17. The nurse is providing care to a patient diagnosed with end-stage renal disease. When planning a care plan conference for this patient, who does the nurse invite to participate? • The oncologist • The psychiatrist • The hospital CEO • The family members 18. Which should be the focus of an educational session for nurses and other members of the interdisciplinary team when addressing high rates of patient readmission to the health system? • • • • Medication errors Coordination of care Adverse clinical events Roles of each member providing care om 19. Which patient population should the nurse focus on to increase access to care that is coordinated, safe, and focused on the patient’s unique needs across all care settings? • Pediatric patients • Older adult patients • Young adult patients • Acute needs patients st pr ep .c 20. Which is a basic principle of the Patient Protection and Affordable Care Act of 2010 that the nurse should include in a teaching session for members of the health-care team? • Decreased access • Decreased cost of care • Decreased quality of care • Decreased safety ng te Multiple Response Identify one or more choices that best complete the statement or answer the question. Increased overall cost of health-care services Decreased patient morbidity and mortality Decreased level of job satisfaction w • • • w w .m yn ur si 21. The hospital’s nurse case manager has been extensively involved with a shooting victim and members of the patient’s family in coordinating care of providers from many disciplines as the patient progressed from the emergency department (ED) to the intensive care unit (ICU), and then onto the medical-surgical unit. After three weeks of hospitalization, the case manager is helping to prepare the patient for discharge to a rehabilitation center where treatment will continue. Which outcomes have been documented in the literature as benefits of such collaboration? Select all that apply. • Improved patient outcomes • Decreased duplication of health-care services 22. The case manager assembles a team of health-care professionals, including the patient’s primary health-care provider, physical therapist, and social worker, for the purpose of collaborative discharge planning and decision making. Which type of team did the case manager assemble? Select all that apply. • Management • Intradisciplinary • Interdisciplinary • Interprofessional • Primary nursing care om 23. The nurse is preparing to document care provided to the patient during the day shift. The nurse documents that the patient experienced an increased pain level while ambulating which required an extra dose of pain medication; took a shower; visited with family; and ate a small lunch. Which information is important to include during the oral end-of-shift reporting? Select all that apply. • The last antibiotics given • The patient’s taking a shower • The patient’s visit with family • The extra dose of pain medication • The patient’s response to ambulation st pr ep .c 24. When the nurse receives a telephone order from the health-care provider's office, which guidelines are used to ensure the order is correct? Select all that apply. • Ask the prescriber to speak slowly. • Read the order back to the prescriber. • Know agency policy for telephone orders. • Sign the prescriber’s name and credentials. • Ask the prescriber to repeat or spell out medication. .m MULTIPLE CHOICE yn ur si ng te 25. When discussing the importance of interprofessional collaboration, which advantages should the nurse include? Select all that apply. • Improved team member satisfaction • Increased division among team members • Increased safety with medication administration • Enhanced communication among team members • Increased patient satisfaction with discharge transition process w w w • ANS: 2 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Exploring the role of the registered nurse in patientcentered transitional care programs Chapter page reference: 017 Heading: Case Manager Integrated Processes: Nursing Process Client Need: Safe and Effective Care Environment – Management of Care Cognitive level: Comprehension [Understanding] Concept : Collabor ation Difficult y: Easy om 1 Feedback Collaboration means a collegial working relationship with other health-care providers to supply patient care. Collaborative practice requires the discussion of diagnoses and management in the delivery of care. Case management involves one or more individuals overseeing the needs and requirements of a particular individual's health. Health promotion activities include disease prevention and healthy lifestyle interventions. Health education would be included in this particular situation, but collaboration is a more inclusive definition of what is occurring with these individuals and the care they require. Health promotion activities include disease prevention and healthy lifestyle interventions. Health education would be included in this particular situation, but collaboration is a more inclusive definition of what is occurring with these individuals and the care they require. ep .c 2 ng te st pr 3 yn ur si 4 w w w .m PTS: 1 CON: Collaboration • ANS: 4 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Defining interprofessional collaboration in the health-care setting Chapter page reference: 010-011 Heading: The Care Transitions Program Integrated Processes: Communication and Documentation Client Need: Psychosocial Integrity Cognitive level: Application [Applying] Concept: Communication Difficulty: Moderate Feedback Telling the patient that the doctor only wants what is best sends the message that the patient does not know what is best, when, in 1 fact, a well-informed patient does know what is best and should be able to make the correct choice. By leaving the room, the nurse and doctor 2 have turned their backs on the patient. Feedback Telling the patient that the doctor only wants what is best sends the message that the patient does not know what is best, when, in fact, a well-informed patient does know what is best and should be able to make the correct choice. By leaving the room, the nurse and doctor have turned their backs on the patient. 1 2 The patient may not understand the recommendations, but pointing that out can be seen as demeaning. The patient is the center of the team, and the goal is to facilitate healing. There are always other options to consider to reach that goal. The nurse would discuss other options with the patient, which will most likely increase cooperation by the patient, who will feel in control as the decision is made. ep .c om 3 te st pr 4 w w w .m yn ur si ng PTS: 1 CON: Communication • ANS: 4 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Exploring the role of the registered nurse in patientcentered transitional care programs Chapter page reference: 011 Heading: The Care Transitions Program Integrated Processes: Nursing Process Client Need: Safe and Effective Care Environment – Management of Care Cognitive level: Application [Applying] Concept : Collabor ation Difficult y: Moderat e Feedback The therapy that the patient requires must be performed by a professional physical therapist. To teach the family exercises 1 encroaches upon the expertise of the professional who will be performing the service. Scheduling home PT is leaving the patient out 2 of the decision-making process. Feedback The therapy that the patient requires must be performed by a professional physical therapist. To teach the family exercises encroaches upon the expertise of the professional who will be performing the service. Scheduling home PT is leaving the patient out of the decision-making process. The nurse would not refer the patient for outpatient therapy unless the patient requests that form of therapy. The nurse best exhibits the characteristic that the patient has a right to self- determination by presenting the methods available for PT and answering the patient's questions about each so the patient can make an informed decision. 1 2 .c om 3 pr ep 4 w w w .m yn ur si ng te st PTS: 1 CON: Collaboration • ANS: 4 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Identifying the roles of health-care professionals coordinating care for patients Chapter page reference: 015-019 Heading: Providers Integrated Processes: Nursing Process Client Need: Safe and Effective Care Environment – Management of Care Cognitive level: Analysis [Analyzing] Concept : Collabor ation Difficult y: Hard Feedback The patient with a chronic disease should not 1 be told there is no hope but should be helped toward reaching desired goals. Asking the patient the reason for the decision 2 is irrelevant to the situation. The nurse can teach some nutrition and 3 exercise but cannot go into the depth that this patient would need. The number of patients with chronic diseases with health-care needs is increasing rapidly, and nurses and primary health-care providers cannot meet all of these patients’ needs. When a patient expresses the desire to live as normally as possible, the nurse should refer the patient to professionals who can help the patient meet that goal. 4 w w w .m yn ur si ng te st pr ep .c om PTS: 1 CON: Collaboration • ANS: 4 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Defining interprofessional collaboration in the health-care setting Chapter page reference: 013-015 Heading: Interprofessional Collaboration Integrated Processes: Nursing Process Client Need: Safe and Effective Care Environment – Management of Care Cognitive level: Comprehension [Understanding] Concept : Collabor ation Difficult y: Easy Feedback Trust occurs when an individual is confident in the actions of another individual. Both 1 mutual respect and trust imply mutual process and outcome and may be expressed verbally or nonverbally. Mutual respect occurs when two or more 2 people show or feel honor or esteem toward one another. Communication is necessary in effective collaboration; it occurs only if the involved 3 parties are committed to understanding each other's professional roles and appreciating each other as individuals. Decision making involves shared responsibility for the outcome. The team must follow specific steps of the decision-making process, beginning with a clear definition of the problem. Team decision making must be 4 directed at the objectives of the effort and requires full consideration and respect for various and diverse viewpoints, and often requires guidance and direction from a group leader. Communication is necessary in effective collaboration; it occurs only if the involved parties are committed to understanding each other's professional roles and appreciating each other as individuals. Decision making involves shared responsibility for the outcome. The team must follow specific steps of the decision-making process, beginning with a clear definition of the problem. Team decision making must be directed at the objectives of the effort and requires full consideration and respect for various and diverse viewpoints, and often requires guidance and direction from a group leader. 3 om 4 w w w .m yn ur si ng te st pr ep .c PTS: 1 CON: Collaboration • ANS: 1 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Identifying the roles of health-care professionals coordinating care for patients Chapter page reference: 014-015 Heading: Interprofessional Education Integrated Processes: Nursing Process Client Need: Safe and Effective Care Environment – Management of Care Cognitive level: Comprehension [Understanding] C o n c e pt : L e g al D if fi c ul ty : E as y Feedback Parameters for the delegation of patient care 1 tasks by nurses to UAPs are established by each state's board of nursing. This organization does not provide definitive 2 answers regarding tasks that nurses can delegate to UAPs. Feedback Parameters for the delegation of patient care tasks by nurses to UAPs are established by each state's board of nursing. This organization does not provide definitive answers regarding tasks that nurses can delegate to UAPs. This individual does not provide definitive answers regarding tasks that nurses can delegate to UAPs. 1 2 3 om This individual does not provide definitive answers regarding tasks that nurses can delegate to UAPs. .c 4 w w w .m yn ur si ng te st pr ep PTS: 1 CON: Legal • ANS: 2 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Defining interprofessional collaboration in the health-care setting Chapter page reference: 013-015 Heading: Interprofessional Collaboration Integrated Processes: Teaching and Learning Client Need: Safe and Effective Care Environment – Management of Care Cognitive level: Comprehension [Understanding] Concept : Collabor ation Difficult y: Easy Feedback Evidence does not suggest that the general population views nurses’ contributions to the 1 care of patients as less important, thus this is not considered a primary barrier to nursephysician collaboration. A primary and historical barrier to effective nurse-physician collaboration has been nurses’ and physicians’ perceptions of 2 inequity in their roles, with nurses assuming a subservient role and medical providers perceiving their role to be superior in the provision of health-care services. Likewise, because health professional students are in fact educated about the benefits of collaborative practice and 3 published evidence has documented the effectiveness of collaboration in improving patient outcomes, these are not barriers to nurse-physician collaboration has been nurses’ and physicians’ perceptions of inequity in their roles, with nurses assuming a subservient role and medical providers perceiving their role to be superior in the provision of health-care services. Likewise, because health professional students are in fact educated about the benefits of collaborative practice and published evidence has documented the effectiveness of collaboration in improving patient outcomes, these are not barriers to collaboration. In addition, the federal government, as evidenced in particular by the Healthy People initiative, has promoted collaborative efforts among patients, nurses, physicians, other health-care providers, and the larger community to improve the health of the U.S. population. 2 3 .c om 4 w w w .m yn ur si ng te st pr ep PTS: 1 CON: Collaboration • ANS: 2 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Identifying the roles of health-care professionals coordinating care for patients Chapter page reference: 017-018 Heading: Case Manager Integrated Processes: Nursing Process Client Need: Safe and Effective Care Environment – Management of Care Cognitive level: Application [Applying] Concept : Collabor ation Difficult y: Moderat e Feedback The pharmacy is not needed as part of the 1 team at this time. The patient’s needs and progress have changed. The nurse notifies the case manager to 2 coordinate changes in care needed after discharge. This patient’s exercise program needs to be revamped, and the case manager is the individual to coordinate this change. A physical therapist may be needed, but the 3 nurse would coordinate care best by notifying the case manager. The occupational therapist mainly deals with the upper body areas needing rehabilitation. 4 w w w .m yn ur si ng te st pr ep .c om PTS: 1 CON: Collaboration • ANS: 4 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Exploring unique patient situations requiring or enhanced by interprofessional collaboration Chapter page reference: 019-020 Heading: Unique Patient Situations Requiring or Enhanced by Interprofessional Collaboration Integrated Processes: Teaching and Learning Client Need: Safe and Effective Care Environment – Management of Care Cognitive level: Analysis [Analyzing] Concep t: Manage ment Difficul ty: Difficul t Feedback The patient is included in the discussion of 1 meeting goals. The case manager monitors and works with 2 the patient to alter the pathway as needed during the recovery process. It is possible to have variances in a critical 3 pathway that, if documented properly, should be paid for by insurance. Care maps, or critical pathways, are flexible 4 enough to be adjusted and tailored to the patient's needs and wishes. PTS: 1 CON: Management • ANS: 4 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Describing models of transitional care Chapter page reference: 010-012 Heading: Evidence-Based Models of Transitional Care Integrated Processes: Teaching and Learning Client Need: Safe and Effective Care Environment – ur si ng te st pr ep .c om Management of Care Cognitive level: Comprehensive [Understanding] Concep t: Manage ment Difficul ty: Easy Feedback Although the involvement of case managers in care typically provides greater peace of 1 mind for patients and family members, this is not the primary goal of this service. Toward this end, case managers not only with help to coordinate care and treatment during 2 hospitalization, but also assist with planning for care following discharge. Their focus includes not only medical care, but issues related to health promotion and 3 disease prevention, the cost of health care received, and planning for the efficient use of resources. Case managers coordinate patient care to help ensure that a continuum of clinical 4 services is provided. The goal of case management is to improve patient outcomes and to help contain costs. .m yn PTS: 1 CON: Management • ANS: 4 w w w Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Describing models of transitional care Chapter page reference: 010-011 Heading: The Transitional Care Model Integrated Processes: Nursing Process Client Need: Safe and Effective Care Environment – Management of Care Cognitive level: Comprehension [Understanding] Concept : Collabor ation Difficult y: Easy Feedback Intradisciplinary teams include members of the same profession. Interdisciplinary teams include professionals of varied backgrounds who share in decision making. Multidisciplinary teams include members of varied backgrounds, but treatment decisions are made by one member–usually the primary health-care provider. Intradisciplinary teams include members of the same profession. The term interprofessional team is synonymous with interdisciplinary team. Interdisciplinary teams include professionals of varied backgrounds who share in decision making. Multidisciplinary teams include members of varied backgrounds, but treatment decisions are made by one member–usually the primary health-care provider. om 1 .c 2 pr ep 3 ng te st 4 w w w .m yn ur si PTS: 1 CON: Collaboration • ANS: 2 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Exploring unique patient situations requiring or enhanced by interprofessional collaboration Chapter page reference: 019-020 Heading: Unique Patient Situations Requiring or Enhanced by Interprofessional Collaboration Integrated Processes: Nursing Process Client Need: Safe and Effective Care Environment – Management of Care Cognitive level: Comprehension [Understanding] Concept : Collabor ation Difficult y: Easy Feedback Interdisciplinary collaboration engages each professional’s contribution to joint care planning, implementation, and accomplishment of patient goals, with 1 possibly less redundancy, more efficiency, and fewer care omissions. The parents of a minor child should be involved in all aspects of care and decision making. Interdisciplinary collaboration engages each om 1 Feedback Interdisciplinary collaboration engages each professional’s contribution to joint care planning, implementation, and accomplishment of patient goals, with possibly less redundancy, more efficiency, and fewer care omissions. The parents of a minor child should be involved in all aspects of care and decision making. Interdisciplinary collaboration engages each professional’s contribution to joint care planning, implementation, and accomplishment of patient goals, with possibly less redundancy, more efficiency, and fewer care omissions. The parents of a minor child should be involved in all aspects of care and decision making. Interdisciplinary collaboration engages each professional’s contribution to joint care planning, implementation, and accomplishment of patient goals, with possibly less redundancy, more efficiency, and fewer care omissions. The parents of a minor child should be involved in all aspects of care and decision making. te st pr ep .c 2 .m yn ur si ng 3 w w w 4 Interdisciplinary collaboration engages each professional’s contribution to joint care planning, implementation, and accomplishment of patient goals, with possibly less redundancy, more efficiency, and fewer care omissions. The parents of a minor child should be involved in all aspects of care and decision making. PTS: 1 CON: Collaboration • ANS: 2 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Describing models of transitional care Chapter page reference: 010-011 Heading: The Transitional Care Model Integrated Processes: Nursing om Process Client Need: Safe and Effective Care Environment – Management of Care Cognitive level: Comprehension [Understanding] Concept : Collabor ation Difficult y: Easy pr ep .c 1 Feedback Intradisciplinary teams comprise members of the same profession working to achieve a common goal. A team comprising members from different disciplines that is focused on achieving a common goal is an interdisciplinary team. Their varying professional backgrounds helps to ensure that other perspectives are represented as the issue is considered. Multidisciplinary teams are more commonly teams whose members work more autonomously toward the common goal. Complementary is not a type of team, although team members’ efforts can be complementary and provide a broader perspective of issues. te st 2 si ng 3 yn ur 4 w w w .m PTS: 1 CON: Collaboration • ANS: 1 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Defining interprofessional collaboration in the health-care setting Chapter page reference: 013-014 Heading: Interprofessional Communication Integrated Processes: Communication and Documentation Client Need: Safe and Effective Care Environment – Management of Care Cognitive level: Comprehension [Understanding] Concept: Communic ation Difficulty: Easy Feedback The type of communication and action used by this health-care team is parallel communication. It is at the lowest level along the continuum of communication and collaboration among health team members 1 and is characterized by each professional communicating with the patient Feedback The type of communication and action used by this health-care team is parallel communication. It is at the lowest level along the continuum of communication and collaboration among health team members and is characterized by each professional communicating with the patient independently, asking the same or similar questions needed to develop their plan of care. om 1 ep .c The next level up on the continuum of communication and collaboration, but not described in this scenario, is parallel functioning. Here, communication is more coordinated, but each professional still develops separate interventions and care plans. In parallel functioning, the exchange of information among team members is more structured and planned, but decision making is unilateral and does not involve much collegiality. While there is an information exchange occurring, this is not the best description of the scenario. The actions of this NT team do not demonstrate coordination and consultation or comanagement and referral, the two highest levels of communication and collaborative action. ng te st pr 2 ur si 3 .m yn 4 w w w PTS: 1 CON: Communication • ANS: 2 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Defining interprofessional collaboration in the health-care setting Chapter page reference: 013-014 Heading: Interprofessional Communication Integrated Processes: Communication and Documentation Client Need: Safe and Effective Care Environment – Management of Care Cognitive level: Application [Applying] Concept: Communic ation Difficulty: Moderate Feedback Waiting for the physician to arrive could cause the patient to experience a great deal of pain in the interim. In this case reporting to the physician by telephone is appropriate. The nurse cannot alter the dose of medication. The nurse would address the patient's distress immediately and later include the event in the end-of-shift report to the oncoming nurse. 1 2 3 om 4 w w w .m yn ur si ng te st pr ep .c PTS: 1 CON: Communication • ANS: 2 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Defining interprofessional collaboration in the health-care setting Chapter page reference: 013-014 Heading: Interprofessional Communication Integrated Processes: Communication and Documentation Client Need: Safe and Effective Care Environment – Safety and Infection Control Cognitive level: Comprehension [Understanding] Concept: Communication; Safety Difficulty: Easy Feedback Handoff communication may be scrutinized 1 during a lawsuit, but avoiding litigation is not a primary objective. Ineffective communication is the primary cause of sentinel events, making patient 2 safety the primary objective of the handoff communication process. Analysis of handoff communication may be a 3 quality improvement criterion, not a primary objective. 4 Handoff communication may be verbal or written. PTS: 1 CON: Communication | Safety • ANS: 4 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Defining interprofessional collaboration in .m yn ur si ng te st pr ep .c om the health-care setting Chapter page reference: 013-014 Heading: Interprofessional Communication Integrated Processes: Communication and Documentation Client Need: Safe and Effective Care Environment – Management of Care Cognitive level: Application [Applying] Concep t: Manage ment Difficul ty: Modera te Feedback The choice of health-care professionals who 1 are invited to attend the conference is based on the needs of the patient. The choice of health-care professionals who 2 are invited to attend the conference is based on the needs of the patient. The choice of health-care professionals who 3 are invited to attend the conference is based on the needs of the patient. The choice of health-care professionals who are invited to attend the conference is based on the needs of the patient. Family 4 members are an important part of the care plan conference, especially for patients who are unable to advocate for themselves. w w w PTS: 1 CON: Management • ANS: 2 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Discussing the importance of successful transitions for medical-surgical patients Chapter page reference: 009-010 Heading: Overview of Transitional Care Integrated Processes: Teaching and Learning Client Need: Safe and Effective Care Environment – Management of Care Cognitive level: Comprehension [Understanding] Concep t: Manage ment Difficul ty: Easy om 1 Feedback The safety of the patient is at risk during transitions between care settings, particularly following an acute hospitalization. The patient’s needs may go unmet, and there is the risk for medication errors and adverse clinical events; however, these are not the focus of an education session regarding readmission rates. Hospital readmission rates are often attributed to a lack of coordination of care as patients are discharged to rehabilitation facilities, long-term care agencies, or back to their homes; therefore, this should be the focus of the educational session. The safety of the patient is at risk during transitions between care settings, particularly following an acute hospitalization. The patient’s needs may go unmet, and there is the risk for medication errors and adverse clinical events; however, these are not the focus of an education session regarding readmission rates. The role of each member of the interdisciplinary team should not be the focus of an educational session to decrease hospital readmission rates. st pr ep .c 2 si ng te 3 .m yn ur 4 w w w PTS: 1 CON: Management • ANS: 2 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Discussing the importance of successful transitions for medical-surgical patient Chapter page reference: 009 Heading: Introduction Integrated Processes: Nursing Process Client Need: Safe and Effective Care Environment – Management of Care Cognitive level: Application [Applying] Concep t: Manage ment Difficul ty: Modera te Feedback The pediatric patient population is not identified as a group where access to coordinated, safe, and focused care is lacking across care settings. Access to care that is coordinated, safe, and focused on the patient’s unique needs across all care settings has eluded many patients, particularly the elderly and chronically ill. The young adult patient population is not identified as a group where access to coordinated, safe, and focused care is lacking across care settings. Patients requiring acute care is not identified as a group where access to coordinated, safe, and focused care is lacking across care settings. 1 .c om 2 pr ep 3 te st 4 w w w .m yn ur si ng PTS: 1 CON: Management • ANS: 2 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Describing changes in the health-care landscape Chapter page reference: 009-010 Heading: Overview of Transitional Care Integrated Processes: Teaching and Learning Client Need: Safe and Effective Care Environment – Management of Care Cognitive level: Application [Applying] Concept: Healthcare System Difficulty: Moderate 1 2 3 Feedback Increased, not decreased, access is a basic principle of the Patient Protection and Affordable Care Act of 2010. Decreased cost of care is a basic principle of the Patient Protection and Affordable Care Act of 2010. Increased, not decreased, quality of care is a basic principle of the Patient Protection and Affordable Care Act of 2010. Feedback Increased, not decreased, access is a basic principle of the Patient Protection and Affordable Care Act of 2010. Decreased cost of care is a basic principle of the Patient Protection and Affordable Care Act of 2010. Increased, not decreased, quality of care is a basic principle of the Patient Protection and Affordable Care Act of 2010. Increased, not decreased, safety is a basic principle of the Patient Protection and Affordable Care Act of 2010. 1 2 3 4 CON: Healthcare System om PTS: 1 ep .c MULTIPLE RESPONSE w w w .m yn ur si ng te st pr 21. ANS: 1, 2, 4 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Describing models of transitional care Chapter page reference: 009-010 Heading: Overview of Transitional Care Integrated Processes: Nursing Process Client Need: Safe and Effective Care Environment – Management of Care Cognitive level: Comprehension [Understanding] Concep t: Manage ment Difficul ty: Easy 1. 2. Feedback This is correct. Research findings suggest that collaboration in health care among patients, family members, caregivers, and communities leads to improved patient outcomes, a reduction in duplicated health-care services, and a decrease in patient morbidity and mortality. This is correct. Research findings suggest that collaboration in health care among patients, family members, caregivers, and communities leads to improved patient outcomes, a reduction in duplicated health-care services, and a decrease in patient morbidity and mortality. This is incorrect. Research findings suggest collaboration in health care among patients, family members, caregivers, and communities leads to improved patient outcomes, a reduction in duplicated health-care services, and a decrease in patient morbidity and mortality. This is correct. Research findings suggest that collaboration in health care among patients, family members, caregivers, and communities leads to improved patient outcomes, a reduction in duplicated health-care services, and a decrease in patient morbidity and mortality. This is incorrect. Research findings suggest that collaboration in health care among patients, family members, caregivers, and communities leads to a decreased, not increased, cost of care. This is in correct. Research findings suggest that collaboration in health care among patients, family members, caregivers, and communities leads to improved patient outcomes, a reduction in duplicated health-care services, and a decrease in patient morbidity and mortality. This is incorrect. Collaborative efforts have also been found to contribute to an enhanced sense of autonomy. This increase in sense of autonomy has been linked to nurses’ greater job satisfaction. 1. 2. .c om 3. te st pr ep 4. si ng 5. CON: Management 22. ANS: 3, 4 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Describing models of transitional care Chapter page reference: 010-011 Heading: The Transitional Care Model Integrated Processes: Nursing Process Client Need: Safe and Effective Care Environment – Management of Care Cognitive level: Comprehension [Understanding] Concept : Collabor ation Difficult y: Easy w w w .m yn ur PTS: 1 Feedback This is incorrect. Management teams are executive-level teams that run the day-to-day operations of a corporation. This is incorrect. Intradisciplinary teams include members of the same profession. This is correct. Interdisciplinary teams include professionals of varied backgrounds who share decision making. The terms interprofessional team and interdisciplinary team are synonymous. 1. 2. om 3. .c This is correct. Interdisciplinary teams include professionals of varied backgrounds who share decision making. The terms interprofessional team and interdisciplinary team are synonymous. This is incorrect. A primary nursing care team includes a primary nurse and associate nurses who will provide care to a patient during a hospital stay. pr ep 4. te st 5. CON: Collaboration 23. ANS: 4, 5 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Defining interprofessional collaboration in the health-care setting Chapter page reference: 013-014 Heading: Interprofessional Communication Integrated Processes: Communication and Documentation Client Need: Safe and Effective Care Environment – Management of Care Cognitive level: Analysis [Analyzing] Concept: Communic ation Difficulty: Difficult w w w .m yn ur si ng PTS: 1 1. 2. 3. 4. Feedback This is incorrect. Antibiotics are reflected on the medication administration record (MAR). This is incorrect. Taking a shower does not need to be reported, only documented. This is incorrect. Visiting with the family need not be mentioned at change of shift but should be documented. This is correct. The nurse would also report any as-needed medications given and when they were last given. This is correct. In order to provide for the patient’s safety, the nurse would pass on the This is incorrect. Taking a shower does not need to be reported, only documented. This is incorrect. Visiting with the family need not be mentioned at change of shift but should be documented. This is correct. The nurse would also report any as-needed medications given and when they were last given. This is correct. In order to provide for the patient’s safety, the nurse would pass on the patient’s response to ambulation so that the oncoming staff can take fall precautions. 2. 3. 4. 5. yn ur si ng te st pr ep .c om PTS: 1 CON: Communication 24. ANS: 1, 2, 3, 5 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Defining interprofessional collaboration in the health-care setting Chapter page reference: 013-014 Heading: Interprofessional Communication Integrated Processes: Communication and Documentation Client Need: Safe and Effective Care Environment – Management of Care Cognitive level: Application [Applying] Concept: Communic ation Difficulty: Moderate w 2. w w .m 1. 3. Feedback This is correct. When receiving a telephone order from a provider, the nurse should ask the prescriber to repeat or spell out the medication, to speak slowly, and read the order back to the prescriber once the prescription is complete. This is correct. When receiving a telephone order from a provider, the nurse should ask the prescriber to repeat or spell out the medication, to speak slowly, and read the order back to the prescriber once the prescription is complete. This is correct. It is also important for the nurse to know the agency’s policy regarding telephone orders. This is incorrect. The nurse does not sign the prescriber’s name and credentials; the nurse only transcribed the prescription and the prescriber countersigns it within a time period prescribed by the agency’s policy. This is correct. When receiving a telephone order from a provider, the nurse should ask the prescriber to repeat or spell out the medication, to speak slowly, and read the order back to the prescriber once the prescription is complete. 4. om 5. w w w .m yn ur si ng te st pr ep .c PTS: 1 CON: Communication 25. ANS: 1, 4, 5 Chapter number and title: 2, Interprofessional Collaboration and Care Coordination Chapter learning objective: Exploring unique patient situations requiring or enhanced by interprofessional collaboration Chapter page reference: 019-020 Heading: Unique Patient Situations Requiring or Enhanced By Interprofessional Collaboration Integrated Processes: Teaching and Learning Client Need: Safe and Effective Care Environment – Management of Care Cognitive level: Application [Applying] Concept : Collabor ation Difficult y: Moderat e 1. 2. 3. 4. 5. Feedback This is correct. Improved team member satisfaction is an advantage of interprofessional collaboration. This is incorrect. There is a decreased, not increased, division among team members with interprofessional collaboration. This is incorrect. There is increased safety with the discharge transition process, not medication administration, with interprofessional collaboration. This is correct. Enhanced communication among team members is an advantage of interprofessional collaboration. This is correct. Increased patient satisfaction with the discharge transition process is an with interprofessional collaboration. This is incorrect. There is increased safety with the discharge transition process, not medication administration, with interprofessional collaboration. This is correct. Enhanced communication among team members is an advantage of interprofessional collaboration. This is correct. Increased patient satisfaction with the discharge transition process is an advantage of interprofessional collaboration. 3. 4. 5. PTS: 1 CON: Collaboration om Chapter 3 Laws and Ethics ep .c MULTIPLE CHOICE • A student nurse who is not yet licensed: • may not perform nursing actions until he or she has passed the licensing examination. is not responsible for his or her actions as a student under the state licensing law. • may perform nursing actions only under the supervision of a licensed nurse. • must apply for a temporary student nurse permit to practice as a student. ANS: C te st pr • I dont know, but I would be willing to be tested. w • w .m yn ur si ng Students may perform nursing actions before they are licensed but only under the supervision of a licensed nurse. The student is responsible for his or her own actions; however, the supervising nurse may also be responsible, depending on the situation. No special permit is required to practice as a student in an approved school of nursing. DIF: Cognitive Level: Knowledge REF: dm 30 OBJ: Theory #1 TOP: Practice Regulations for the Student Nurse KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • During an employment interview, the interviewer asks the nurse applicant about HIV status. The nurse applicant can legally respond: • No, even though he or she has a positive HIV test. w • • I dont know, and I refuse to be tested. You do not have a right to ask me that question. ANS: D In employment practice, it is illegal to discriminate against people with certain diseases or conditions. Asking a question about health status, especially HIV or AIDS infection, is illegal. DIF: Cognitive Level: Application REF: dm 31 OBJ: Clinical Practice #1 TOP: Discrimination KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • An example of a violation of criminal law by a nurse is: • taking a controlled substance from agency supply for personal use. • accidentally administering a drug to the wrong patient, who then has a serious reaction. • advising a patient to sue the doctor for a supposed mistake the doctor made. writing a letter to the newspaper outlining questionable or unsafe hospital practices. ANS: A Theft of a controlled substance is a federal crime and consequently a crime against society. DIF: Cognitive Level: Application REF: dm 30 OBJ: Theory #2 TOP: Criminal Law KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The LPN (LVN) assigns part of the care for her patients to a nursing assistant. The LPN is legally required to perform which of the following for the residents assigned to the assistant? • Toilet the residents every 2 hours and as needed. st pr ep .c om • Feed breakfast to one of the residents who needs assistance. • Give medications to the residents at the prescribed times. te • Transport the residents to the physical therapy department. ANS: C Toileting, feeding, and transporting residents or patients are tasks that can be legally assigned to a nurses aide. Administering medications is a nursing act that can be performed only by a licensed nurse or by a student nurse under the supervision of a licensed nurse. DIF: Cognitive Level: Application REF: dm 31 OBJ: Theory #3 TOP: Delegation KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care • w w w .m yn ur si ng • If a nurse is reported to a state board of nursing for repeatedly making medication errors, it is most likely that: • the nurse will immediately have his or her license revoked. • the nurse will have to take the licensing examination again. • a course in legal aspects of nursing care will be required. • there will be a hearing to determine whether the charges are true. ANS: D The nurse may have his or her license revoked or be required to take a refresher course, but this would be based on the evidence presented at a hearing. The licensing examination is not usually required as a correction of the situation as described. DIF: Cognitive Level: Knowledge REF: dm 31 OBJ: Theory #3 TOP: Professional Discipline KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A nurse co-worker arrives at work 30 minutes late, smelling strongly of alcohol. The fellow nurses legal course of action is to: • have the nurse lie down in the nurses lounge and sleep while others do the work. state that, if this happens again, it will be reported. • report the condition of the nurse to the nursing supervisor. offer a breath mint and instruct the nurse co-worker to work. ANS: C Nurses must report the condition. It is a nurses legal and ethical duty to protect patients from impaired or incompetent workers. Allowing the impaired nurse to sleep enables the impaired nurse to avoid the consequences of his or her actions and to continue the risky behavior. Threatening to report the next time continues to place patients at risk, as does masking the signs of impairment with breath mints. DIF: Cognitive Level: Application REF: dm 31 OBJ: Theory #3 TOP: Professional Discipline KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • When a student nurse performs a nursing skill, it is expected that the student: • perform the skill as quickly as the licensed nurse. ur si ng te st pr ep .c • om • achieve the same result as the licensed nurse. • not be held to the same standard as the licensed nurse. .m yn • always be directly supervised by an instructor. ANS: B Students are not expected to perform skills as quickly or as smoothly as experienced nurses, but students must achieve the same result in a safe manner. DIF: Cognitive Level: Comprehension REF: dm 30 OBJ: Theory #1 TOP: Practice Regulations for the Student Nurse KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • If a nurse receives unwelcome sexual advances from a nursing supervisor, the first step the nurse should take is to: w w w • • send an anonymous letter to the nursing administration to alert them to the situation. tell the nursing supervisor that she is uncomfortable with the sexual advances and ask the superviso • behavior. • report the nursing supervisor to the state board for nursing. resign and seek employment in a more comfortable environment. ANS: B The first step in dealing with sexual harassment in the workplace is to indicate to the person that the actions or conversations are offensive and ask the person to stop. If the actions continue, then reporting the occurrence to the supervisor or the offenders supervisor is indicated. DIF: Cognitive Level: Application REF: dm 32 OBJ: Clinical Practice #1 TOP: Sexual Harassment KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A person who has been brought to the emergency room after being struck by a car insists on leaving, although the doctor has advised him to be hospitalized overnight. The nurse caring for this patient should: • have him sign a Leave Against Medical Advice (AMA) form. pr ep .c om • tell him that he cannot leave until the doctor releases him. • immediately begin the process of involuntary committal. te st • contact the persons health care proxy to assist in the decision-making process. ANS: A A person has the right to refuse medical care, and agencies use the Leave AMA to document the medical advice given and the patients informed choice to leave against that advice. DIF: Cognitive Level: Application REF: dm 38 OBJ: Clinical Practice #3 TOP: Patients Rights KEY: Nursing Process Step: Implementation MSC: NCLEX: N/A • The information in a patients chart may legally be: • copied by students for use in school reports or case studies. .m yn ur si ng • shared with other health care providers at the patients request. w • provided to lawyers or insurers without the patients permission. w • withheld from the patient, because it is the property of the doctor or agency. ANS: C A release or consent is required to provide information from a patients chart to anyone not directly caring for that patient. The patient must provide consent to provide information to insurers, lawyers, or other health care agencies or providers. The patient has the right to access the information in his or her chart (copies), but the agency or doctor retains ownership of the document. DIF: Cognitive Level: Application REF: dm 34 OBJ: Theory #5 TOP: Legal Documents KEY: Nursing Process Step: N/A MSC: NCLEX: N/A w • • If a patient indicates that he is unsure if he needs the surgery he is scheduled for later that morning, the nurse would best reply: • Your doctor explained all of that yesterday when you signed the consent. • Your doctor is in the operating room; she cant talk to you now. • You should have the surgery; your doctor recommended that you have it. I will call the doctor to speak with you before you go to the operating room. ANS: D A consent can be withdrawn at any time before the treatment or procedure has been started. The physician should be notified by the supervising nursing staff of the unit. DIF: Cognitive Level: Application REF: dm 36 OBJ: Clinical Practice #4 TOP: Informed Consent KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A 16-year-old boy is admitted to the emergency room after fracturing his arm from falling off his bike while visiting with his stepfather who is not the custodial parent. The nurse is preparing him to go to the operating room but must obtain a valid informed consent by: • having the patient sign the consent for surgery. ng te st pr ep .c om • obtaining the signature of his stepfather for the surgery. • declaring the patient to be an emancipated minor. ur si • obtaining permission of the custodial parent for the surgery. ANS: D The patient is a minor and cannot legally sign his own consent unless he is an emancipated minor; the guardian for this patient is the custodial parent. A step-parent is not a legal guardian for a minor unless the child has been adopted by the step-parent. The hospital does not have the authority to declare the patient an emancipated minor. DIF: Cognitive Level: Application REF: dm 36 OBJ: Clinical Practice #3 TOP: Consent KEY: Nursing Process Step: Intervention MSC: NCLEX: Safe Effective Care Environment: coordinated care • A patient has advance directives spelled out in a durable power of attorney, with the appointment of his daughter as his health care agent. The daughter will be responsible for: • paying all the medical bills associated with the fathers illness. w w w .m yn • • making all informed consent decisions for her father. • making all choices about her fathers health care if the father is unable. • paying only for those health care decisions based om on the advance directives. ANS: C A health care agent makes decisions for the patient only when a patient is unable, according to the wishes made known by the patient in advance directives. A health care agent is not responsible for financial decisions or payments. DIF: Cognitive Level: Application REF: dm 36 OBJ: Clinical Practice #5 TOP: Advance Directives KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A patient has signed a do-not-resuscitate (DNR) order. If a nurse performs cardiopulmonary resuscitation (CPR) when the patient stops breathing and then successfully revives the patient, the: nurse could be found guilty of battery. • patient would have no grounds for legal action. • patient could charge the nurse with false imprisonment. ep .c • nurse could be found guilty of assault. ANS: A A nurse who attempts CPR on a patient who had a doctors order for a DNR could be found guilty of battery. DIF: Cognitive Level: Comprehension REF: dm 9 | dm 36 OBJ: Clinical Practice #3 TOP: DNR KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A patient refuses to take his medications or to eat his breakfast. He is alert, mentally competent, and fairly comfortable. The nurse should: • give the medications by injection if the patient will not take them orally. .m yn ur si ng te st pr • tell the patient that he must cooperate with his care. w • respect the patients right to refuse medications or food, because he is competent. w • contact the doctor to insert a feeding tube to supply both medicine and food. ANS: B The competent patient has the right to refuse medicine, food, treatments, and procedures. Giving (or threatening to give) medications by injection over the patients objections is considered battery. Threatening the patient or overriding the patients wishes is a violation of the patients bill of rights and constitutes assault or battery. DIF: Cognitive Level: Application REF: dm 38 OBJ: Clinical Practice #3 TOP: Patients Rights KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A nurse remarks to several people that Dr. X must be getting w • senile because she makes so many mistakes. If that remark results in some of Dr. Xs patients changing to another doctor, Dr. X would have grounds to sue the nurse for: • slander. • libel. • invasion of privacy. • w w .m yn ur si ng te st pr ep .c om n e g l i g e n c e . A N S : A A person who makes untrue, malicious, or harmful remarks that damage a persons reputation and cause injury (loss of business) is guilty of defamation and slander. Libel is defamation that is written. DIF: Cognitive Level: Application REF: dm 38 OBJ: Clinical Practice #5 TOP: Defamation/ Slander KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A licensed nurse is liable for charges of malpractice when she: • does not show up for work and fails to call to notify the agency. clocks in for another nurse to prevent that nurse from having pay docked. • falsifies data, causing the patient to suffer problems resulting in death. w • • assists in performing CPR that is unsuccessful, and the patient dies. ANS: C Malpractice is professional negligence or, in this case, doing (falsifying) something the reasonable and prudent nurse would not do. It is the proximate cause of the patient injury. This is a case of causation. DIF: Cognitive Level: Application REF: dm 37, Box 3-6 OBJ: Theory #5 TOP: Negligence and Malpractice KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A postoperative patient in the intensive care unit (ICU) is so confused and agitated that staff have not been able to safely care for him. He has pulled out his central line once, and he slides to the bottom of the bed, where he attempts to climb out, pulling and disrupting the various tubes and monitors. The nurses best course of action is to: • place him in a protective vest device. use a sheet to tie him in a chair at the nurses station. • request that the doctor write an order for a protective device and/or medication. om • call a family member to stay with the patient. ANS: C A protective device may not be used (except in an emergency) without a doctors order, and it is used only when other less restrictive means do not provide safety for the patient. DIF: Cognitive Level: Application REF: dm 39 OBJ: Clinical Practice #3 TOP: False Imprisonment KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • An elderly, slightly confused patient sustains an injury from a heating pad that was wrongly applied by the nurse. The nurse should: • pretend to be unaware of the injury to the patient. ng te st pr ep .c • report the incident to the risk management team via an incident report. • document in the patients chart that an incident report was filled out. ur si • not chart anything about the injury in the patients chart. ANS: B When an incident occurs that has potential for a future lawsuit, the risk management team should be aware of it as soon as possible. An incident report should be filled out, and the patient chart should be documented to describe the injury. No mention of the incident report is usually made in the patient chart. Honesty and a forthright explanation to the patient reduce the risk of lawsuits. DIF: Cognitive Level: Application REF: dm 40 OBJ: Theory #5 TOP: Incident Reports KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • Nursing liability insurance is a policy purchased and put into effect by the nurse for the purpose of: • providing protection against being sued. w w w .m yn • • reducing the chance of litigation. • paying attorney fees and any award won by the plaintiff. • are voluntary. • rarely change. .c providing the hospital with added protection. ANS: C Nursing liability pays attorney fees and any award won by the plaintiff. DIF: Cognitive Level: Comprehension REF: dm 40 OBJ: Theory #5 TOP: Nursing Ethics KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • Ethics and law are different from each other in that ethics: • bear a penalty if violated. om • can alway s direct all decisi ons. ANS: B Ethics are voluntary and are based on values. Ethics may change as parameters of health care change. There is no penalty for violation. DIF: Cognitive Level: Analysis REF: dm 40 OBJ: Theory #6 TOP: Nursing Ethics KEY: Nursing Process Step: N/ A MSC: NCLEX: N/A • To best protect himself or herself from being sued, the nurse should: • continue to do procedures as taught in school. maintain competency. w • purchase malpractice insurance. w • .m yn ur si ng te st pr ep • w • use evi den cebas ed pra ctic e. AN S: patient information in a secure office area. • medications in a locked area. .c • om C Keeping up with continuing education, maintaining competency, and seeking to improve ones own practice by self-evaluation will best protect the nurse. DIF: Cognitive Level: Comprehension REF: dm 39, Box 3-7 OBJ: Theory #5 TOP: Avoiding Lawsuits KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The Health Insurance Portability and Accountability Acts (HIPAA) main focus is in keeping: • patients safe from harm. hospital infectio ns under control. ANS: B HIPAA regulates the way patient information is conveyed and stored. DIF: Cognitive Level: Comprehension REF: dm 34, Box 3-4 OBJ: Clinical Practice #1 TOP: HIPAA KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • When a patient asks a nurse to witness the signing of a will, the nurse should refer the request to the: nurse supervisor. • hospital legal department. • notary public for the hospital. .m yn ur • w w w • n u r s e s a t t o r n e si ng te st pr ep • st pr ep .c om y . A N S : C Although witnessing a legal document for a patient is not illegal, most agencies have a policy regarding the proper course of action by referring the patient to the notary public. DIF: Cognitive Level: Application REF: dm 36 OBJ: Theory #1 TOP: Witnessing Wills and Other Legal Documents KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • Criteria that justify becoming an emancipated minor and able to sign a medical consent include all of the following except: • independence established through a court order. service in the armed forces. • a 14-year-old whose parents are dead. ng te • a 17yearold pregn ant femal e. ANS: C Criteria are that the minor be independent by court order, be a member of the military, be pregnant, or be married. DIF: Cognitive Level: Application REF: dm 36 OBJ: Clinical Practice #33 TOP: Emancipated Minor KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A written statement expressing the wishes of a patient regarding future consent for or refusal of treatment in case the patient is incapable of participating in decision making is an example of: • a privileged relationship. w w w .m yn ur si • • a health care agent. • an advance directive. • .m yn ur si ng te st pr ep .c om w i t n e s s e d w i l l . A N S : C An advance directive makes the patients wishes known regarding medical decisions and consent in the event that he or she is unable to participate in decision making. DIF: Cognitive Level: Knowledge REF: dm 36 OBJ: Clinical Practice #5 TOP: Legal Terms KEY: Nursing Process Step: N/ A MSC: NCLEX: N/A • A nurse is caring for an unmarried 16-year-old patient who has just given birth to a baby boy. The nurse will get the consent to perform a circumcision on the patients son from the: • patients father. patients physician. • patients mother. 16-year-old patient. w w • w • ANS: D Pregnancy qualifies as the basis for the 16-year-old to be treated as an emancipated minor. DIF: Cognitive Level: Application REF: dm 36 OBJ: Clinical Practice #3 TOP: Patients Rights KEY: Nursing Process Step: Implementation MSC: NCLEX: N/A • A 48-year-old man refuses to take a medication ordered for the control of his blood pressure. The nurses most effective response would be: • Your doctor expects you to be compliant. • You have the right to refuse. This medication keeps your blood pressure under control. • Fine. I will document that you are refusing this drug. Are you aware that you could have a stroke? ANS: B Patients have the right to refuse medication, but it is the nurses responsibility to explain the reason for the particular drug. DIF: Cognitive Level: Application REF: dm 37 OBJ: Theory #1 TOP: Legal Standards KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • The Occupational Safety and Health Act includes all of the following except: • regulations for handling infectious materials. radiation and electrical equipment safeguards. • staffing ratios and delegation criteria. regulations for handling toxic materials. ANS: C The Occupational Safety and Health Act was passed in 1970 to improve the work environment in areas that affect workers health or safety. It includes regulations for handling infectious or toxic materials, radiation safeguards, and the use of electrical equipment. DIF: Cognitive Level: Comprehension REF: dm 31 OBJ: N/A TOP: OSHA KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The most frequently cited cause of a sentinel event by the Joint Commission is a problem in: • applying physical restraints. methods of patient transportation. w • w .m yn ur si ng te st • pr • ep .c om • • medication errors. w • ina de qu ate co m mu nic ati on. .c om A N S: D The most frequently cited cause of a sentinel event by the Joint Commission is communication. During handoff communication, there is a risk that critical patient care information might be lost due to lack of communication. DIF: Cognitive Level: Knowledge REF: dm 33 OBJ: Clinical Practice #2 TOP: Communication KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The acronym SBAR is a method to communicate with a physician that clarifies a situation that may result in litigation. The acronym stands for: situation, background, alterations, results. • subjective, believable, actual, recommendation. • situation, background, assessment, recommendation. pr ep • situation, basis, assessment, recommendation. ANS: C SBAR is an acronym that stands for situation, background, assessment, and recommendation. This undetailed analysis clarifies the situation in a manner that is concise yet complete. DIF: Cognitive Level: Knowledge REF: dm 33 OBJ: Theory #5 TOP: SBAR Reporting KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The patient who cannot legally sign his or her own surgical consent is a(n): • 17-year-old who is serving in the armed forces. 17-year-old emancipated minor. w • 16-year-old who is legally married. w • .m yn ur si ng te st • 18-year-old who received a narcotic 30 minutes ago. ANS: D The person giving the consent must be able to take part in the decision making. A sedated person does not have this ability. DIF: Cognitive Level: Application REF: dm 36 OBJ: Clinical Practice #3 TOP: Patients Rights KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The nurse who may be liable for invasion of privacy would be the nurse who is: • refusing to give patient information to a relative over the phone. w • • firmly closing the door prior to bathing the patient. • discussing her patients with a fellow nurse. reporting the patient as a possible victim of elder abuse. ANS: C Discussing a patient with anyone, even another health professional, who is not involved in the patients care can put a nurse at risk for invasion of privacy. DIF: Cognitive Level: Application REF: dm 38 OBJ: Clinical Practice #3 TOP: Patients Rights KEY: Nursing Process Step: Implementation MSC: NCLEX: N/A • A characteristic of an advance directive is that: • advance directives do not expire. only some states recognize advance directives. • advance directives can be non-verbal. advance directives from one state are recognized by another. ANS: A An advance directive is a written statement expressing the wishes of the patient regarding future consent for or refusal of treatment if the patient is incapable of participating in decision making, ng te st pr • ep • .c om • defamation. w • w .m yn ur si and they do not expire. All states recognize advance directives, but each state regulates advance directives differently, and an advance directive from one state may not be recognized in another. DIF: Cognitive Level: Comprehension REF: dm 36 OBJ: Clinical Practice #5 TOP: Advance Directives KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A patient who is refusing to take his medication is threatened that he will be held down and forced to take the dose. This is an example of: • battery. w • • i n v a s i assault. is accidentally exposed. • leaves the hospital against medical advice. ur si • w w w .m yn • c o m e s t o h a r m . A N S : ng te st pr ep .c om o n o f p r i v a c y . A N S : C Assault is the threat to harm another or even to touch another without that persons permission. The person being threatened must believe that the nurse has the ability to carry out the threat. DIF: Cognitive Level: Comprehension REF: dm 37 OBJ: Theory #3 TOP: Legal Terms KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The nurse explains that a sentinel event is a situation in which a patient: • refuses care. and ur si ng te st pr ep .c om D A sentinel event is an unexpected situation in which the patient comes to harm. DIF: Cognitive Level: Comprehension REF: dm 33 OBJ: Theory #5 TOP: Legal Terms KEY: Nursing Process Step: N/A MSC: NCLEX: N/A COMPLETION • In 2003, the Patients Bill of Rights was revised to become the : Understanding Expectations, Rights, and Responsibilities. ANS: Patient Care Partnership The Patient Care Partnership addresses patient rights and the responsibility of health care facilities. DIF: Cognitive Level: Knowledge REF: dm 32 OBJ: Clinical Practice #3 TOP: Patients Rights KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • CAPTA, passed in 1973, is a law regarding the safety of minors. It is the . ANS: Child Abuse Prevention; Treatment Act This is a law that requires mandated reporting and defines who is a mandated reporter. DIF: Cognitive Level: Knowledge REF: dm 32 OBJ: Theory #1 TOP: Professional Accountability KEY: Nursing Process Step: N/A MSC: NCLEX: N/ A .m yn MULTIPLE RESPONSE • Professional accountability includes: (Select all that apply.) • understanding theory. adhering to the dress code of the facility. • asking for assistance when unsure of a procedure or physician order. participating in continuing education classes. w • w • w • • meeting the health care needs of the patient. reporting patient health status changes to all family members. ANS: A, C, D, E Professional accountability is a nurses responsibility to meet the health care needs of the patient in a safe and caring application of nursing skills and understanding of human needs. DIF: Cognitive Level: Analysis REF: dm 39 OBJ: Theory #3 TOP: Professional Accountability KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A nurse arrives at the scene of a motor vehicle accident. A person in the vehicle mumbles incoherently when asked his name. Which actions are not covered by the Good Samaritan Act? (Select all that apply.) • Using two magazines and a bandana to splint a broken arm • Applying a tourniquet to a lacerated leg while awaiting emergency personnel • Pulling the individual from the surface of the highway • Initiating an emergency tracheotomy when the individual goes into respiratory arrest Compressing a bleeding wound with a soiled shirt ANS: D The Good Samaritan Act covers care given in an emergency, but only within the scope of ones practice, and care that does not cause harm resulting from negligence. DIF: Cognitive Level: Comprehension REF: dm 32 OBJ: Theory #5 TOP: Legal Scope of Practice KEY: Nursing Process Step: N/A MSC: NCLEX: Safe Effective Care Environment • The Ethics Committee of a facility has the responsibility to: (Select all that apply.) • develop policies. ng te st pr ep .c om • address issues in their facility. • modify the established codes of ethics as suits the situation. • create a master plan for decision making to be followed in ethical dilemmas. yn ur si • help to find a better understanding of ethical dilemmas from different standpoints. ANS: A, B, E An Ethics Committee of an institution has representatives from various fields to formulate, address, and help clarify ethical problems that present themselves in their facility. DIF: Cognitive Level: Comprehension REF: dm 42 OBJ: Theory #6 TOP: Ethics KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • w w w .m • The commonalities of The Codes of Ethics of the National Association for Practical Education and Service (NAPNES) and The National Federation of Licensed Practical Nurses (NFLPN) include: (Select all that apply.) • commitment to continuing education. • respect for human dignity. • maintenance of competence. • requirement for membership in a national organization. preserving the confidentiality of the nursepatient relationship. ANS: A, B, C, E Both Codes of Ethics support maintenance of competency, preservation of confidentiality of the nursepatient relationship, commitment to continuing education, and respect for human dignity. • handicapped. ep disabled. pr • .c Chapter 4 Health and Illness MULTIPLE CHOICE • The rehabilitation nurse describes a patient who is blind, works full time as a Spanish interpreter, and lives with his wife in a downtown apartment. The nurse classifies this person as: • impaired. om • st • w w w .m yn ur si ng te d e p e n d e n t . A N S : A The blindness is an impairment of vision that does not inhibit the patient from performing his job or enjoying a normal life. DIF: Cognitive Level: Application REF: 177 OBJ: 1 (theory) TOP: Concepts of Rehabilitation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation • A resident with advanced Parkinsons disease stays in his wheelchair all day because it is too tiring to walk and he is fearful of falling. In order to increase mobility, the best intervention would be to: • instruct the resident in crutch walking. • assist the resident to walk in the hallway with a gait belt. • encourage the resident to rock back and forth in his wheelchair to off load weight. • The obese resident who lies on her back because it is difficult to turn due to her weight has a pressure ulcer on her coccyx that is covered with a dressing. The most effective intervention to encourage independence is: • have staff turn the resident every 2 hours. w w .m • yn ur si ng te st pr ep .c om arr an ge fo ra w al ki ng ca ne . A N S: B Walking is the best exercise to prevent problems associated with immobility. The gait belt will make the resident more secure. Canes and crutches do not diminish the weakness or the fear of falling. DIF: Cognitive Level: Application REF: 184 | Box 9-5 OBJ: 2 (theory) TOP: Preventing Problems of Immobility KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance w • • • turn the patient on her side and use pillows to stabilize her. arrange for short side rails to be used for positioning. arrange for a trapeze so the patient can assist with positioning. ANS: D The trapeze allows for self-positioning and is less confining than are bed rails. The other options do not foster independence. DIF: Cognitive Level: Application REF: 186-187 OBJ: 2 (theory) TOP: Preventing Problems of Immobility KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance • When the nurse assesses reddened heels on the bed-bound stroke patient, the nurse modifies the care plan to include which intervention? • Massage heels briskly. • Apply socks to feet. • Swab heels with alcohol. • w w w .m yn ur si ng te st pr ep .c om E l e v a t e f e e t o n p i l l o w s . A N S : D Elevation of the feet gets the weight off the heels and will allow them to heal. All other options are not helpful to damaged skin. Brisk massage may promote damage to the skin. Alcohol can be irritating and may further damage heel skin. DIF: Cognitive Level: Application REF: 180 | Nursing Care Plan 9-1 OBJ: 2 (theory) TOP: Preventing Problems of Immobility KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance • The nurse cautions the 70-year-old patient who just had the cast removed from a broken arm that the immobility during the time he was in a cast can cause: • arthritis. • phlebitis. • frozen shoulder. • w w w .m yn ur si ng te st pr ep .c om p a i n f u l s w e l l i n g . A N S : C Immobility can cause loss of strength and flexibility in the older adult. DIF: Cognitive Level: Knowledge REF: 178 | 180 | Table 9-1 OBJ: 3 (theory) TOP: Effects of Immobility: Joint Stiffness KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance • The nurse assessing an 85-year-old patient who has been on bed rest for a fractured hip finds the patient flushed with a temperature of 100 F, pulse of 100, and respiration rate of 24. The next intervention should be to assess: • BP. • breath sounds. • abdominal distention. • a m o u w w w .m yn ur si ng te st pr ep .c om n t o f u r i n a r y o u t p u t . A N S : B The initial assessments are the cardinal signs of pneumonia. The breath sounds should be assessed next to determine the presence of any adventitious breath sounds. BP will also need to be assessed, but the breath sounds are more important with the signs and symptoms present. Abdominal distention is indicative of a gastrointestinal problem. Amount of urinary output is important to an ongoing assessment but not a priority in the present circumstances. DIF: Cognitive Level: Analysis REF: 179 | Table 9-1 OBJ: 3 (theory) TOP: Effects of Immobility: Hypostatic Pneumonia KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance • The 76-year-old stroke patient in a long-term care facility has sent his food tray back to the kitchen untouched for the second time today. The most effective intervention to increase nutrition would be to: • take the tray back and offer to feed the patient. • request the dietitian to talk with the patient about food preferences. • take a high-protein drink to the patient. • sit with the patient during meals. apply warm compress. • turn the patient every 2 hours. ep • .c om ANS: C Taking the high-energy drink meets the immediate challenge of inadequate nutritional intake. Referral to the dietitian and sitting with the patient may be helpful. Offering to feed from a rejected tray is not supportive. DIF: Cognitive Level: Analysis REF: 190-191 OBJ: 2 (theory) TOP: Effects of Immobility: Anorexia KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance • When the nurse is assessing a bed-bound resident, a reddened area over the coccyx that does not blanch is discovered. The best intervention to prevent further skin damage is to: • cover with a transparent film dressing. • w w w .m yn ur si ng te st pr cont inue to mo nito r the area . AN S: A Since this appears to be a stage 1 pressure area, the transparent film ensures the proper amount of moisture is present for healing while allowing monitoring of the area. A warm compress is not warranted. This patient will need to be turned every hour. Monitoring of the area should continue but does not meet the immediate need. DIF: Cognitive Level: Analysis REF: 180 | Nursing Care Plan 9-1 OBJ: 3 (theory) TOP: Effects of Immobility: Impaired Circulation KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance • The LPN/LVN making care assignments to nursing assistants would not assign a patient who has: • manipulative behavior. • an unstable condition. • a draining wound. • w w .m yn ur si ng te st pr ep .c om a c o m m u n i c a b l e d i s e a s e . A N S : B Nursing assistants are not assigned to patients who have an unstable condition. Care of an unstable patient does not fall into the scope of practice of the unlicensed personnel. DIF: Cognitive Level: Comprehension REF: 183 | Assignment Considerations OBJ: 5 (theory) TOP: Assigning Personnel KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care • The chief goal of a long-term care facility is to: • offer restorative services. promote individual independence. • facilitate achievement of complete autonomy. w • • mana ge medi catio n proto cols. keep patient in a position at a table or bedside. • prevent falls. .c • om ANS :B Promotion of independence is the chief goal, not complete autonomy. Other options are services directed at achieving increased independence. DIF: Cognitive Level: Comprehension REF: 183 OBJ: 4 (theory) TOP: Goal of Long-Term Care Facilities KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance • The nurse reminds the nursing assistant that the purpose of locking the wheels of a wheelchair is to: • supply a stable support for a patient to lift self. keep the patient from moving self. ANS: C Fall prevention is the purpose of locking the wheels of a wheelchair. DIF: Cognitive Level: Comprehension REF: 184 | Box 9-5 OBJ: 2 (clinical) TOP: Fall Prevention KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control • To decrease the incidence of falls, the nurse will arrange for the replacement of: • canes with 4 feet with a single-footed cane. yn ur si ng te st pr ep • hard-soled shoes with soft-soled bedroom slippers. • area rugs with a nonslip pad. w plain carpet with a highly patterned carpet. ANS: C Loose area rugs should be replaced with nonslip carpets. DIF: Cognitive Level: Knowledge REF: 184 | Box 9-5 OBJ: 2 (clinical) TOP: Fall Prevention KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control • The nurse instructing a family in the selection of a chair for an older adult with Parkinsons disease would stress selecting a chair that: w w • .m • • is very wide to allow for position changes. • has sturdy arms to aid in rising. • is low to prevent falls. is soft and deep for added comfort. ANS: B Sturdy arms assist in rising and sitting. Soft, low, and wide chairs cause a person to lean forward to rise and to fall into the chair to be seated. DIF: Cognitive Level: Comprehension REF: 184 | Box 9-5 OBJ: 2 (clinical) TOP: Fall Prevention KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control • The charge nurse instructs the nursing assistants to answer the call lights promptly, especially for patients who are receiving: • diuretics for fluid reduction. st pr ep .c om • antibiotics for infection. • proton pump medications for gastric reflux. ng te • w ur yn .m w w N S A I D s f o r a r t h r i t i s . A N si • Turn and reposition the resident every hour. • Assess condition of the skin every 4 hours. • Reassess the need for the security device every 4 to 8 hours. ANS: D ng te st pr • ep .c om S : A People taking diuretics need to go to the bathroom frequently, and oftentimes urgently. Prompt attention to call lights will reduce the probability of the patient getting up unassisted. Diuretics may also cause orthostatic hypotension, which increases the risk for falling. DIF: Cognitive Level: Comprehension REF: 184 | Box 9-5 OBJ: 2 (clinical) TOP: Fall Prevention KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control • The nurse is caring for a resident who has a security device for safety purposes. What intervention must the nurse include in the plan of care? • Visually check the resident every hour. w w .m yn ur si The need for continuing the use of the security device must be assessed every 4 to 8 hours. The patient should be visually checked every 30 minutes, and turned and skin assessed every 2 hours. DIF: Cognitive Level: Application REF: 184 | Box 9-5 OBJ: 2 (clinical) TOP: Use of Security Devices KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control • When the confused resident pours his cereal in a cup and drinks it, the nurse should: • put his cereal back in the bowl and hand the resident a spoon. discard the cup with his cereal and bring fresh cereal in a bowl. • calmly instruct the resident that cereal is to be eaten from a bowl. w • • n o t i n t e r dramatic two-part mini-series. w w • travel documentary. w • .m yn ur si ng te st pr ep .c om r u p t t h e b e h a v i o r. A N S : D The nurse should leave the resident alone to feed himself independently. Staff should refrain from doing what the resident can do for himself. DIF: Cognitive Level: Application REF: 186 OBJ: 4 (theory) TOP: LongTerm Care Facility Goals: Autonomy KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity • The nurse planning a group TV activity in a long-term care facility would choose a channel that offers a(n): • cartoon. • o p e r a p e r si ng te st pr ep .c om f o r m a n c e . A N S : B Travel documentaries are colorful and do not have a plot to follow. Cartoons are juvenile, opera does not have universal appeal, and the two-part drama would require long attention spans and good short-term memory. DIF: Cognitive Level: Application REF: 187 OBJ: 4 (theory) TOP: LongTerm Care Facility Goals: Autonomy KEY: Nursing Process Step: Planning MSC: NCLEX: Psychosocial Integrity • To motivate a frustrated stroke patient who is learning to walk again, the most effective motivational intervention the rehabilitation nurse could make is to: • show short movies on ambulation techniques. observe the patient while in physical therapy. • arrange a visit with another stroke victim who has learned to ambulate. ur • encourage a 1-week break from therapy, which will help the resident come back refreshed. ANS: C Talking with someone who can truly understand the frustration is helpful. Showing a short movie on ambulation techniques may be an effective teaching tool, but it is not a motivational tool. Observing the resident is necessary but does not provide motivation. A 1-week break will interrupt progress that has been made, thus decreasing motivation. w w w .m yn • DIF: Cognitive Level: Application REF: 188 | Elder Care Points OBJ: 4 (theory) TOP: Goals for Rehabilitation: Motivation KEY: Nursing Process Step: Planning MSC: NCLEX: Psychosocial Integrity • The nurse caring for the resident who is disoriented can provide the best care with which intervention? • Ensuring activities are scheduled for the same time each day • Changing care assignments for assistive personnel frequently to prevent burnout • Encouraging autonomy by allowing the resident to choose clothes from the closet Administering sedatives to calm the patient ANS: A Keeping a routine leads to less confusion. Changing assistive personnel care assignments frequently is confusing for the resident. Choosing clothing from an entire closet is overwhelming for the confused resident; rather, giving the resident a few items to choose from encourages autonomy without increasing confusion. Sedatives should not be given to treat confusion. DIF: Cognitive Level: Application REF: 185-186 OBJ: 4 (theory) TOP: Managing Confusion and Disorientation KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity MULTIPLE RESPONSE • Treatment resources that focus on restorative care for people with chronic illness and disabilities are: (Select all that apply.) • outpatient clinics. long-term health care facilities. • home care. • rehabilitation agencies. yn ur si • w w w .m • h o s p i c e a g e n c i e s . ng te st pr ep .c om • te st pr ep .c om A N S : A , B , C , D Outpatient clinics, long-term care facilities, home care, and rehabilitation agencies are sources of rehabilitation for people with chronic illness or disability. Hospice agencies focus on care of the dying patient. DIF: Cognitive Level: Knowledge REF: 179 OBJ: 1 (theory) TOP: Locus of Treatment for Chronic Illness KEY: Nursing Process Step: NA MSC: NCLEX: Health Promotion and Maintenance • The nurse reinforces that the multifocused goal of rehabilitation is to: (Select all that apply.) • promote new coping skills. teach adaptive living skills. • focus on self-care for increased independence. • improve quality of life. • restore former level of functio n. ANS: A, B, C, D w w w .m yn ur si ng • Restoring former level of function is not a goal of rehabilitation because this may an impossible goal. New coping and adaptive skills, and selfcare skills that improve the quality of life are all goals of rehabilitation. DIF: Cognitive Level: Application REF: 187 OBJ: 7 (theory) TOP: Goals of Rehabilitation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation • The patient who has been in traction for bilateral femur fractures complains of constipation. To stimulate bowel action, the nurse will: (Select all that apply.) • provide prune juice from the snack cart. • increase fluid intake. • arrange for high-fiber foods such as cauliflower and broccoli. • give prescribed stool softeners. • w w w .m yn ur si ng te st pr ep .c om e n c o u r a g e m i l k p r o d u c t s . A N S : A , B , C , D Milk products are constipating. Prune juice, extra fluid, high-fiber foods, and stool softeners will combat constipation. DIF: Cognitive Level: Application REF: 180-181 OBJ: 2 (theory) TOP: Preventing Problems of Immobility KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance • The rehabilitation nurse outlines the impact of disability, which includes: (Select all that apply.) • unchanged family roles. • life patterns centered around treatment or rehabilitation. • grief over what has been lost. • spiritual distress. • w w w .m yn ur si ng te st pr ep .c om s e n s e o f p o w e r l e s s n e s s . A N S : B , C , D , E Family roles often change as a result of a disability. Life patterns will center around treatment and rehabilitation for at least the initial phase of incurring the disability, as well as grief, spiritual distress, and powerlessness. DIF: Cognitive Level: Application REF: 177-178 OBJ: 4 (theory) TOP: Impact of Disability KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity • Long-term health care facilities are the center of treatment for people who are: (Select all that apply.) • recovering after the most acute phase of their illness is over. receiving rehabilitation after a joint replacement. • too weak from primary illness to care for themselves presently. • in need of a permanent home because of effects of a chronic condition. • under treatment for substance abuse. si ng te st pr ep .c ANS: A, B, C, D Long-term health care facilities do not offer active treatment to substance abusers. Recovery from an acute illness, joint replacement rehabilitation, weakness from illness, and a permanent home for a chronic illness are common reasons individuals seek care from longterm care facilities. DIF: Cognitive Level: Application REF: 179 | 183 OBJ: 4 (theory) TOP: Purpose of Long-Term Health Care Facilities KEY: Nursing Process Step: NA MSC: NCLEX: Health Promotion and Maintenance • The LPN/LVN in a long-term health care facility may perform in the roles of: (Select all that apply.) • charge nurse. om • designer of nursing care plans. • administrator of medications. • administrator of wound care. • w w w a s s i g n m e n t d e l e g .m yn ur • ur si ng te st pr ep .c om a t o r . A N S : A , C , D , E The LPN/LVN does not design the nursing care plan but may contribute to the care plan. This is the responsibility of the RN. The LPN/LVN may act in the role of charge nurse while under the supervision of an RN. Administration of medications and wound care and delegation of care are commonly the LPN/LVNs responsibility. DIF: Cognitive Level: Comprehension REF: 189 OBJ: 5 (theory) TOP: LPN/LVN Role in Long-Term Health Care Facility KEY: Nursing Process Step: NA MSC: NCLEX: Health Promotion and Maintenance • When delegating care to a nursing assistant, the LPN/LVN should: (Select all that apply.) • give specific instruction as to what is to be done. instruct how the task is to be done. • list information that needs to be reported. • be aware that the nurse is responsible for outcome of delegated care. .m yn • insist that the nursing assistant accept the responsibility. ANS: A, B, C, D In delegating to unlicensed assistive personnel, the LPN/LVN should first inquire if the nursing assistant is willing to take responsibility for the care assigned. DIF: Cognitive Level: Comprehension REF: 183 | Assignment Considerations OBJ: 5 (theory) TOP: Delegation KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care • The LPN/LVN can apply a physical restraint to a resident in a long-term care facility when: (Select all that apply.) • an order for the restraint is obtained within 12 hours of application. w w w • • all other measures have been attempted and failed. • documentation is made on all failed attempts. • the family is unable to stay with the resident. the least restrictive device is chosen. ANS: B, C, D, E The order for the restraint must be obtained within 24 to 48 hours after application of the device. The LPN/LVN who applies a physical restraint must have satisfied all of the other options. DIF: Cognitive Level: Application REF: 184-185 OBJ: 2 (clinical) TOP: Use of Restraints KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control • The student nurse is becoming familiar with Healthy People 2020 goals related to rehabilitation. The student nurse demonstrates an understanding of the goals when identifying which of the following as goals? (Select all that apply.) • Increase the proportion of adults with disabilities who participate in social activities. te st pr ep .c om • Increase the proportion of adults with disabilities who report satisfaction with life. Increase the proportion of people with disabilities who report not having the assistive devices and te Reduce the proportion of adults with disabilities who report feelings such as sadness, unhappiness, prevent them from being active. si ng • • ur • w w w .m yn Reduce the proportion of people with disabilities who report environmental barriers to participation • work, or community activities. ANS: A, B, D, E One of the goals of Healthy People 2020 is to reduce rather than increase the proportion of people with disabilities who report not having the assistive devices and technology needed. All other options are included as goals. DIF: Cognitive Level: Comprehension REF: 187 OBJ: 7 (theory) TOP: Healthy People 2020 Goals KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance COMPLETION • The rehabilitation nurse makes the point that a dysfunction of a specific body part is termed . ANS: impairment An impairment is a dysfunction of an organ or body part. DIF: Cognitive Level: Comprehension REF: 177 OBJ: 1 (theory) om TOP: Concepts of Rehabilitation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation • The nurse working in a long-term care facility is aware that in order to comply with Medicare guidelines, documentation of assessment findings which measure physical, psychological, and . psychosocial functioning are necessary using the ANS: Minimum Data Set minimum data set MDS The Minimum Data Set (MDS) is a primary screening and assessment tool that is standard for all Medicare and Medicaid residents in a long-term care facility. ng te st pr ep .c Chapter 5 Homeostasis, Adaptation, and Stress MULTIPLE CHOICE • An 82-year-old man is alert and oriented and in good physical health except for some arthritic pain that slows me down, but I just keep moving. He lives alone in an apartment in a senior citizen complex but enjoys the company of other residents and takes part in the social activities there. His lifestyle is an example of: • an exception to the expected norm. the disengagement theory. • the activity theory. ur w w w .m yn • t h e b i o l o g i c t h e o r y . si • ep .c om A N S : C The activity theory states that persons who remain active and interested in outside activities live longer. DIF: Cognitive Level: Analysis REF: dm 165 OBJ: Theory #3 TOP: Theories of Aging KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity: psychosocial adaptation • The nurse understands that the best explanation of why a particular person lives into his 90s in relatively good health is that the person: • had healthy parents who passed on to him good genes and no hereditary diseases. has lived a healthful lifestyle, which has included preventative care, good nutrition, exercise, and a • has treated illness with old-fashioned home remedies while avoiding the use of many prescription d te st pr • reads a lot about the newest advances in health care and tries these approaches as soon as they are p ANS: B Lifestyle and personality together probably contribute to longevity more than genetics, new medical approaches, or old-fashioned home remedies, although those may contribute in important ways. A healthy lifestyle decreases the risk of disease and its sequelae. DIF: Cognitive Level: Comprehension REF: dm 165 OBJ: Theory #3 TOP: Longevity KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • An 85-year-old widow who lives alone has fallen several times in the last month and has been noted by her children to be confused about her medications and to frequently forget what is cooking on the stove until it is burned. These observations indicate that: • she needs to be hospitalized to determine the cause of her confusion and falls. w w w .m yn ur si ng • • home delivery of a hot meal each day would solve her cooking risk. • nursing home placement would be the best solution to her problems of aging. • further assessment is needed to evaluate an increased level of assistance. ANS: D The widow is showing signs of needing additional assistance. It might include home- delivered meals or nursing home-placement, but further assessment needs to be performed. Acute care hospitalization is not indicated in this situation. DIF: Cognitive Level: Analysis REF: dm 172 OBJ: Clinical Practice #5 TOP: Aging Parents KEY: Nursing Process Step: Planning MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse clarifies that the immune system failure theory states that: • the elderly lose their ability to effectively respond to infections and are more likely to die from them the body no longer recognizes itself and begins to attack itself, causing illness. • toxins and harmful chemicals (free radicals) in the environment cause damage to body cells. om • the diminished activity of the elderly make them susceptible to illness. ANS: A With advancing age, the immune system of the elderly has less ability to fight infections. DIF: Cognitive Level: Knowledge REF: dm 165 OBJ: Theory #1 TOP: Theories of Aging KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse seeks out residents with whom they reminisce in an interview regarding the residents life story. The value of this activity is that: • it gives the staff more time to care for other residents and perform routine care. ng te st pr ep .c • it can affirm the positives of the residents life and lead to ego integrity for the resident. • nursing home residents have long days to pass, and any activity helps the time pass more quickly. yn ur si • students learn about the good old days and better appreciate the modern conveniences available tod ANS: B Eriksons psychosocial task for older adults is ego integrity, which can be assisted by life review and reminiscence. DIF: Cognitive Level: Comprehension REF: dm 170 OBJ: Theory #6 TOP: Psychological Aspects of Aging KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: psychosocial adaptation • The home health aide who visits an older adult reports to the nurse that the patient has many new bruises on her arms and face. The patient states that her daughter has a temper and got mad when she visited the day before. The nurse should: • call the daughter for clarification. w w w .m • • notify her nursing supervisor to report the incident to the authorities. • tell the aide to report it to the nursing supervisor. • plan to visit the patient when the .c om daughter will be present. ANS: B It is a legal requirement for licensed health care personnel to report suspected elder abuse to protect the public (patient). An LPN should report to the RN supervisor first. The aide is supervised by the nurse and thus the nurse is responsible. It is not the nurses responsibility to determine whether the daughter is abusing the patient but only to report it so that it can be investigated by the proper agency. DIF: Cognitive Level: Analysis REF: dm 170 OBJ: Theory #4 TOP: Family Relationships KEY: Nursing Process Step: Assessment MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A 76-year-old neighbor confides to the nurse that she is having to get up in the middle of the night to void and often wets herself before she can get to the bathroom during the day. The nurses best explanation would be: As you get older, your bladder muscle loses tone and you can hold less urine. • You are probably drinking too much during the day and especially before bedtime. • You probably have a bladder infection that should be treated with antibiotics. pr ep • With age, the urine becomes very concentrated and causes the bladder to empty spontaneously. ANS: A Physiologic changes of aging include decreased bladder and sphincter tone, resulting in stress incontinence and more frequent voiding. DIF: Cognitive Level: Application REF: dm 166, Table 13-1 OBJ: Clinical Practice #1 TOP: Physical Changes KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • A nurse making a home visit to a 75-year-old woman discovers that the patient stays in bed or on the couch most of the time because she is afraid of falling. The nurse should arrange for a: • sitter to stay with the woman during the day. wheelchair to increase mobility. w • w .m yn ur si ng te st • w • • physical therapist to teach resistance training. special cushion for the chair and bed to reduce the risk of decubiti. ANS: C A physical therapist can teach resistance and balance training to help prevent falls. DIF: Cognitive Level: Analysis REF: dm 167 OBJ: Theory #4 TOP: Physical Health Concerns KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • The home health nurse assesses an 80-year-old who has fallen twice in the last 10 days. The nurse discovers that the patient uses a cane for ambulation stability, drinks up to 6 cups of coffee a day, has altered depth perception because of cataracts, and has recently carpeted her home with a smooth tight weave carpet. The nurse suspects the cause of her recent falls to be the: • use of the cane. • new carpet. • large intake of caffeine. • w w w .m yn ur si ng te st pr ep .c om a l t e r e d d e p t h p e r c e p t i o n . A N S : D Altered depth perception, changes in gait, and slow reaction times may cause falls in the elderly. The cane helps with stability, and the smooth tight weave carpet should not cause falls. DIF: Cognitive Level: Analysis REF: dm 167 OBJ: Theory #4 TOP: Fall Prevention KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • A 70-year-old widower continues to work part time in a demanding business, while traveling in his free time with a 68- year-old widow to visit longtime friends and relatives. He remains an active member of several community organizations. His life is an example of a person who: • is acting like a younger person to prove to himself that he is not old. • is adjusting well to the changes of benign senescence. • should slow down and enjoy retirement while he is still healthy. is avoiding the psychosocial tasks of aging such as retirement and slowing down. ANS: B Benign senescence is the normal changes of aging, and many healthy people at 70 years of age do not fit the stereotype of old but are more like older adults of 45 to 70 years. DIF: Cognitive Level: Analysis REF: dm 166, Table 13-1 OBJ: Theory #3 TOP: Cognitive Aspects of Aging KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance • A 78-year-old man is admitted to the hospital after a fall from his bed at home that resulted in a fractured hip and several fractured ribs. He states, I dont know how I broke so many bones. I only fell out of bed. The nurse can explain that: • loss of calcium from bone occurs in older adults and can result in fractures from minor trauma. te st pr ep .c om • it is likely that an underlying disease made him more susceptible to fractures. • the bedside table near the bed added to his injuries. si ng • the height of the bed will need to be lowered when he goes home to prevent further injuries. ANS: A A physiologic change of aging is loss of calcium from bone, resulting in osteoporosis and greater likelihood of fractures. DIF: Cognitive Level: Application REF: dm 166, Table 13-1 OBJ: Theory #4 TOP: Physical Changes of Aging KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • An 84-year-old patient who is hospitalized for pneumonia says to the nurse, I dont know why Ive lived so long. All my friends are gone, my children and grandchildren are all independent and successfulnobody needs me anymore. An appropriate response by the nurse is: • You have a lot to live for. Your children and grandchildren really love you. w w w .m yn ur • • You must have inherited good genes. You should be thankful youre still alive. • Tell me about your children and what it was like when you were raising them. • The pneumonia has made you feel morbid. Things will look up! ANS: C om Encouraging reminiscing helps the older adult put her life in perspective and acquire a sense of ego. DIF: Cognitive Level: Application REF: dm 170 OBJ: Clinical Practice #4 TOP: Psychosocial Aspects of Aging KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • An 80-year-old man has no chronic diseases and is alert, oriented, and physically active. Which of the following nursing diagnoses is likely to be present as a result of the normal aging process? • Poisoning, risk for, related to the many medications an older person must take. Suffocation, risk for, related to declining respiratory function. • Hopelessness, related to recognition of the end of life drawing near. .c • Constipation, related to slowed peristalsis. ANS: D Constipation is a common nursing diagnosis for older adults in otherwise good health. In addition to peristalsis slowing, most older adults experience decreased taste and smell resulting in decreased appetite and food intake, as well as decreased physical mobility. DIF: Cognitive Level: Analysis REF: dm 166, Table 13-1 OBJ: Theory #4 TOP: Physical Changes KEY: Nursing Process Step: Diagnosis MSC: NCLEX: Health Promotion and Maintenance • The nurse warns that infection after exposure to respiratory illness in the older adult: • is more likely to result in serious lower respiratory infection related to weakened respiratory muscle .m yn ur si ng te st pr ep • is likely to be fatal due to the older persons low resistance. • results in rates of infection similar to those in the younger adult. can be easily prevented with the use of antibiotics when the adult is exposed. ANS: A Changes in the older adult respiratory system make older adults more susceptible to infections that can be very serious. Although some infections are life threatening, most are not. DIF: Cognitive Level: Comprehension REF: dm 166, Table 13-1 OBJ: Theory #4 TOP: Physical Changes KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • When the nurse is conducting a class for senior citizens at a local assisted living facility, to enhance physical health, he w w • w • encourages the older residents to engage in some form of exercise for at least: • 1 hour every other day. • 10 minutes at a time several times a day. • 30 minutes a day, five times a week. • w w w .m yn ur si ng te st pr ep .c om 1 h o u r e v e r y m o r n i n g . A N S : C Exercise for as little as 30 minutes a day 5 days a week is beneficial. DIF: Cognitive Level: Application REF: d. 169 OBJ: Clinical Practice #2 TOP: Physical Health Promotion Behaviors KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse points out that there are many myths about the elderly that are not true. The statement that reflects the most accuracy about the elderly is: • most old people live in nursing homes. • genetics is the main factor in longevity. • the optimistic, happy person generally lives longer. • most old people are isolated from their families. ANS: C • integrity. pr autonomy. st • ep .c om Myths about old people include: most old people live in nursing homes, genetics is the main factor in longevity, and most old people are isolated from their families. It is true that a major contributor to longer life is that the optimistic, happy person generally lives longer. DIF: Cognitive Level: Comprehension REF: d. 171 OBJ: Theory #3 TOP: Theories of Aging KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: psychosocial adaptation • When the 75-year-old patient tells the nurse that he has had a good and rewarding life and has enjoyed every minute of it, the nurse is aware that the patient has attained the Eriksonian stage of: • generativity. set a small goal for himself to be met every day. w • arrange his day so that he is able to take a nap in the afternoon. w • .m yn ur si ng te • intimacy. ANS: C Erik Eriksons psychosocial development theory includes the stage of ego integrity vs. despair, which is characterized by reflection on ones life and ones achievements. A sense of pride or despair is developed regarding the accomplishments in life that have been made or were lost. DIF: Cognitive Level: Comprehension REF: d. 170 OBJ: Theory #3 TOP: Theorists KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: growth and development • When a 68-year-old recent retiree confides in the health clinic nurse that he has felt depressed and withdrawn since retirement, the nurse suggests that he: • talk with the physician about anti-depression medication. eat three regular meals as he did when he was employed. ANS: C Setting a small goal to be met allows for direction in the day. Many recent retirees miss the regulation of employment. DIF: Cognitive Level: Application REF: d. 169 OBJ: Theory #3 TOP: Theorists KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity: psychosocial adaptation COMPLETION • An 85-year-old has been increasingly confused and disoriented to place and time over the last several months. He also has difficulty remembering what he ate, who visited, and where the recreation . room is. This behavior is indicative of w • w w w .m yn ur si ng te st pr ep .c MSC: NCLEX: Physiological Integrity: physiological adaptation • A 67-year-old submitted a job application at a local gas station. The station manager said, Arent you retired? I cant hire you. Youre too old to be working! This is an example of . ANS: ageism Ageism is defined as any discrimination related to age, including job discrimination. DIF: Cognitive Level: Analysis REF: d. 169 OBJ: Theory #2 TOP: Employment and Retirement KEY: Nursing Process Step: N/A MSC: NCLEX: N/ A • The home health nurse assesses the older patients in her case load for signs of abuse. The nurse is aware that the primary incidence of abuse is . ANS: neglect In patients over the age of 80 who suffer abuse, the primary type of abuse is neglect. DIF: Cognitive Level: Knowledge REF: d. 170 OBJ: Theory #4 TOP: Elder Abuse KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort MULTIPLE RESPONSE • To promote cognitive health for a 79-year-old, the nursing student should encourage the patient to do which of the following? (Select all that apply.) • Read the newspaper. om ANS: dementia Confusion, memory loss, and disordered thinking are early signs of dementia. Causes of dementia include malnutrition, medications, mini-strokes, and Alzheimers disease. DIF: Cognitive Level: Analysis REF: d. 169, Table 13-2 OBJ: Clinical Practice #4 TOP: Physical Health Concerns KEY: Nursing Process Step: Assessment • Put together puzzles. • Take naps when tired. • Write letters. • T w w w .m yn ur si ng te st pr ep .c om o i l e t i n d e p e n d e n t l y . A N S : A , B , D Mental stimulation such as these activities maintains active and healthy neural connections, which promotes cognitive health. DIF: Cognitive Level: Application REF: d. 169 OBJ: Clinical Practice #3 TOP: Cognitive Health Promotion Behaviors KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • A 76-year-old recently lost her spouse. They lived in a large house with a yard that they managed well until her spouses sudden death. She is in good health and stays active but is becoming concerned about her ability to maintain the large house by herself. The nurses most helpful suggestion would be to: (Select all that apply.) • recommend living with her daughter who lives 2 hours away. • encourage her to investigate apartment rentals. • encourage her to check herself into a skilled nursing facility. • hire a gardener and a housekeeper to maintain the property. • encourage her to involve family in any decisions related to her living arrangements. te st pr ep .c om ANS: B, E Many older adults choose to rent an apartment when they cannot maintain a house and yard. Including family members in important decisions keeps communication lines open. Family members can offer support and recommendations to their parent(s), easing the decisionmaking process. DIF: Cognitive Level: Analysis REF: pp. 170-171 OBJ: Clinical Practice #5 TOP: Psychosocial Health Promotion Behaviors KEY: Nursing Process Step: Planning MSC: NCLEX: Psychosocial Integrity • An 82-year-old patient expresses concern of always being cold. Based on knowledge of the physical changes associated with aging, the nurse could appropriately respond: (Select all that apply.) • Wrap up warmly, because the cold feeling is a result of decreased bone calcium that occurs with ag Chronic constipation can lead to a sense of cold because of the reduced peristalsis. • Subcutaneous fat is reduced as part of aging. This fat that helps to keep you warm decreases. • A low level of thyroid hormone causes you to feel cold. ur si ng • Eat more protein foods to help your body generate heat. ANS: C, D Decreased subcutaneous fat and slowed thyroid production contribute to older people feeling cold. DIF: Cognitive Level: Application REF: d. 166, Table 13-1 OBJ: Theory #4 TOP: Physical Changes KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity • The nurse points out elements in our culture that support longevity in older people, which include: (Select all that apply.) • reducing stress from regular exercise on the body in younger years. w w w .m yn • • being actively involved in their own health care. • taking of antibiotics through their lifetime. • increasing education about health matters. • avoidi ng the eating of red meat. ANS: B, D Active participation in ones own health care, being better educated about illness, and illness prevention are elements in attaining a longer life span. w w w .m yn ur si ng te st pr ep .c om Chapter 6 Culture and Ethnicity T e st B a n k M U L T I P L E C H O I C E • A nurses neighbor confides that she has been treating a health problem through a faith healer in her religion but is worried because the condition seems to be worsening. She asks the nurse what she should do. The nurses best response would be: Faith healing, although frequently effective, makes a disease more difficult or even impossible to tr • medicine. • • Many people use medical treatment along with faith healing. Is there anything in your religion that treatment? Faith healing may take longer than medical treatment to work. Are you doing exactly as your healer You should see a physician or your faith healer, but not both. ANS: B A persons health care choices are influenced by religious beliefs and culture. Many people use religious or folk medicine in addition to modern medicine. DIF: Cognitive Level: Application REF: d. 183, Table 14-3 OBJ: Theory #1 TOP: Religious Influence in Health Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The most culturally sensitive and useful question the admitting nurse should ask the Jewish patient would be: • Do you follow any dietary restrictions or will you eat hospital food as it is prepared here? ep .c om • Are there any medications or treatments your religion does not allow in your medical treatment? • Would you like me to notify your rabbi so that he can make visits to you during your stay? st pr • Tell me about any religious practices you observe that we need to incorporate into your care. ANS: D The response to the general question requesting any special concerns would include information relative to food, prayer, and rabbinical visitation. The other questions do have importance, but the general question will allow the nurse to hear what is most significant to the patient. DIF: Cognitive Level: Application REF: d. 183, Table 14-3 OBJ: Theory #7 TOP: Religion and Health Care KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse referring to an elderly Asian man says, He probably uses acupuncture and believes in yin and yang. This remark is an example of: • stereotyping of the patient. w w w .m yn ur si ng te • • ethnocentrism of the patient. • cultural sensitivity on the part of the nurse. • a w o r l d w I will call your priest to come in, but if he is unable to be there, Ill be sure the baby is baptized. w • .m yn ur si ng te st pr ep .c om v i e w o f t h e n u r s e . A N S : A Stereotyping occurs when common characteristics of a cultural group are applied to an individual with no attention to the individuals characteristics. DIF: Cognitive Level: Comprehension REF: d. 180 OBJ: Clinical Practice #5 TOP: Stereotyping KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A Roman Catholic patient going to surgery for an emergency cesarean delivery is afraid the baby may not survive, and because she is Roman Catholic, she asks you to be sure that the baby is baptized when it is born. Your response to her should be: • There wont be time to baptize the baby in the operating room. w Baptisms are not usually done in the hospital, and certainly not in the operating room, but I will tell your concerns. • • You need to think positively. Both you and the baby are going to be just fine. ANS: B Baptism is very important to practicing Roman Catholic patients, and even stillborns are baptized. Baptism should be performed by the priest, but any believer can baptize in an emergency. DIF: Cognitive Level: Application REF: d. 176, Box 14-1 OBJ: Theory #6 TOP: Religious Characteristics KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A 76-year-old Hispanic woman is in the skilled nursing facility where she is to participate in a rehabilitation program following a hip replacement. She is alert, oriented, and cooperative but speaks only Spanish; her adult children interpret for her when they are present. The nurse plans the most effective way to communicate with this patient is to: • communicate with the patient when the children are present and can translate. arrange to have one of the children present at all times. • create a translation guide with commonly used Spanish and English words and phrases. om • call on the facility translator for every interaction with the resident. ANS: C A simple translation guide can be used with a cooperative patient in this nonacute setting. The other solutions are unworkable and unrealistic. DIF: Cognitive Level: Application REF: d. 181 OBJ: Clinical Practice #3 TOP: Communication KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A person who believes and practices the Christian Science religion is most likely to: • seek the latest technological medical and surgical care available. ng te st pr ep .c • use medicinal herbs and drugs rather than surgery to treat illness and disease. • use prayer and altered thinking to correct the causes of illness and disease. ur si • require the dead to be buried within 24 hours of the death. ANS: C A person of the Christian Science belief does not normally seek traditional health care and uses prayer for healing. DIF: Cognitive Level: Comprehension REF: d. 176, Box 14-1 OBJ: Theory #6 TOP: Religious Characteristics KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A woman who is part of a traditional Muslim family is hospitalized after an accident. It is most important for the nurse to include in the care to: • provide privacy when the priest comes to administer the sacrament of the sick. w w w .m yn • • respect her need for modesty in keeping her body covered. • keep her hair covered at all times. • refrain from touching the soles of her feet. ANS: B Traditional Muslim women are extremely modest and keep their bodies covered. DIF: Cognitive Level: Comprehension REF: d. 178, Box 14-2 OBJ: Theory #6 TOP: Religious Characteristics KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse is aware that when an Orthodox Jewish family has a baby boy, it is expected that the: • baby will be circumcised by the physician as soon as possible after the birth. husband of the woman will provide the physical care she needs. • naming of the baby will be done by the mother before she leaves the hospital. om • baby will be circumcised on the eighth day of life when he is named. ANS: D Male Orthodox Jewish children are named and circumcised by the mohel on the eighth day of life. DIF: Cognitive Level: Comprehension REF: d. 178, Box 14-2 OBJ: Theory #6 TOP: Religious Practices KEY: Nursing Process Step: Planning MSC: NCLEX: Psychosocial Integrity: psychosocial adaptation • A single African-American working mother of three children who is in a state of poverty often misses appointments for the childrens immunizations or well child check-ups. The nurse understands that the likely reason for this could be that she: is more concerned with surviving day-to-day problems than with taking a child to a clinic when the • illness. yn ur si ng te st pr ep .c • would rather enjoy her time off in leisure activities than taking the children to a clinic. • is from a culture that values nontraditional medical care from curanderos and faith healers. w w .m • belongs to a religious group that is opposed to immunizations and medical treatment. ANS: A People who live in poverty are often focused on day-to-day living. Preventative medicine is future oriented. DIF: Cognitive Level: Application REF: d. 179 OBJ: Theory #2 TOP: Low-Income Families KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity: psychosocial adaptation • The nurse is aware that Muslims and Orthodox Jews have similar dietary restrictions in that both groups require that their followers: w • • remain mainly vegetarians. • avoid milk and meat at the same meal. • eat only meat that has been slaughtered according to their religious law. • avoid shellfish. st pr ep .c om ANS: C Muslim and Jewish followers require food to be prepared according to religious law. In the Jewish faith, it is called kosher, which also requires the separation of milk and meat. DIF: Cognitive Level: Comprehension REF: d. 178, Box 14-2 OBJ: Theory #4 TOP: Dietary Restrictions KEY: Nursing Process Step: Planning MSC: NCLEX: Psychosocial Integrity: psychosocial adaptation • A resident in a skilled nursing facility indicates that she is an agnostic and is afraid of what will happen to her when she dies. An appropriate nursing intervention for this patient is to: • request the physician to order an anxiety-reducing medication. ask the patient whether she would like to talk to the facility social worker or chaplain to address her • offer reassurance to the patient that God will understand her confusion. ng te • share your religious belief with the patient. ANS: B Exploring spiritual (meaning of life and death) issues with a social worker or spiritual care person is appropriate to address spiritual distress as demonstrated by the patients anxiety over her impending death. DIF: Cognitive Level: Application REF: d. 179 OBJ: Clinical Practice #4 TOP: Spiritual Distress KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse is sensitive to the fact that Hispanics believe that some foods and fluids have hot and cold properties that affect their health by: • destroying the pathogen causing the disease. w w w .m yn ur si • • • restoring equilibrium to the body. • strengthening the mind to dispel an evil spirit. would be more comfortable with an elder from his tribe present. w • w .m yn ur si ng te st pr ep .c om e n s u r i n g h e a l i n g . A N S : B Hispanics believe that certain foods through their hot or cold properties can restore the bodys equilibrium. DIF: Cognitive Level: Comprehension REF: d. 183, Table 14-3 OBJ: Theory #6 TOP: Nutrition and Religion KEY: Nursing Process Step: Planning MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A patient who is Native American and visiting a health care clinic for the first time keeps his eyes on the floor and seldom makes eye contact with the nurse. The nurse would be correct in thinking that the patient: • is depressed and concerned about his health status. w • • is uncomfortable talking about health issues with a woman. finds direct or sustained eye contact rude or disrespectful. ANS: D Native Americans do not usually sustain eye contact in the same way as European Americans do because they consider it rude. DIF: Cognitive Level: Comprehension REF: d. 181 OBJ: Theory #5 TOP: Cultural Behaviors KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity: coping and adaptation • When a devout Muslim dies, the nurse makes arrangements to: • notify a family member to come bathe the patient. • extinguish all light and leave the room in darkness. • cover the body with the patients prayer rug. place an open Koran over the patients heart. ANS: A A family member must bathe the deceased person before anybody else touches the body. DIF: Cognitive Level: Application REF: d. 178, Box 14-2 OBJ: Theory #6 TOP: Muslim Death KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A nurse who practices in a culturally competent manner is one who is able to: • work in a large facility where there are a variety of diverse cultures. st pr ep .c om • assist a patient from another culture to change and adapt to the medical culture. • look at the world through the eyes of the culturally diverse patient. ng te • recognize which cultural traits are harmful in the health care culture. ANS: C Cultural competence is attained when the nurse makes a conscious attempt to learn about people of diverse cultures and look at the world through their perspective. DIF: Cognitive Level: Comprehension REF: d. 179 OBJ: Clinical Practice #2 TOP: Transcultural Competence KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A young African-American man is admitted to the hospital in sickle cell crisis. He is unmarried and lives with an extended family headed by his grandmother. The nurse takes into consideration that this type of family arrangement is: • egalitarian. w w w .m yn ur si • • t r a n • patriarchal. • matriarchal. s c u l t u r a l . Hispanic • Pacific Islander • European ur w w w .m yn • A f r i c a n A m e r i c a n A N si • ng te st pr ep .c om AN S: C Matriarchal families are headed by women (mother) and are commonly seen in AfricanAmerican families. DIF: Cognitive Level: Knowledge REF: d. 181 OBJ: Clinical Practice #2 TOP: Family Types KEY: Nursing Process Step: Planning MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse must be alert to non-verbal expressions to assess pain in patients from a(n) background. concern about the meaning and importance of her life. • continued anger at God for afflicting her with the illness. ep .c • om S : B Pacific Islanders are reluctant to express emotion to others and are stoic about pain. DIF: Cognitive Level: Comprehension REF: d. 183, Table 14-3 OBJ: Theory #4 TOP: Cultural Sensitivity KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A desired outcome for a patient with a nursing diagnosis of spiritual distress is that the patient expresses: • acceptance that she is not being punished by God with illness. refusal to participate in religious rituals that have no meaning for her now. ANS: A Spiritual distress is often caused by a belief that illness is a punishment for wrongdoing or sin. DIF: Cognitive Level: Application REF: d. 185 OBJ: Clinical Practice #4 TOP: Spiritual Distress KEY: Nursing Process Step: Planning MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse understands that when an Asian patient refers to yin, the patient is referring to a balancing force that is represented by: • light. ur si ng te st pr • a masculine force. • cold and feminine elements. yn • w w w .m • harmony. ANS: C Yin is the balancing force to yang that is represented by elements that are dark, cold, and feminine. DIF: Cognitive Level: Comprehension REF: d. 183, Table 14-3 OBJ: Theory #7 TOP: Nutritional Practices KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse understands that acupuncture and acupressure are alternative therapies based on: • healing through meditation and prayer. • concepts of hot and cold and balancing those against the illness. • the power of suggestion and autohypnosis. • interrupting or changing the flow of energy fields in the body. ANS: D baptize the fetus if a priest is not immediately available. • encourage the mother to consider tubal ligation. discuss hormonal contraception with the mother. ANS: B Within the Catholic religion, infants must be baptized soon after birth because of the belief that babies not baptized will not go to Heaven. Even aborted fetuses must be baptized. If a priest is not immediately available, the nurse may baptize by pouring holy water on the head and saying, I baptize you in the name of the Father, of the Son, and of the Holy Spirit. DIF: Cognitive Level: Application REF: d. 176, Box 14-1 OBJ: Clinical Practice #6 TOP: Spiritual Distress KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A nurse caring for a patient who is a practicing Jehovahs is on hand Witness and who has had surgery confirms that to be infused. • frozen packed cells Dextran w • w .m yn ur si ng te st pr ep • .c • om Acupressure, massage, and acupuncture all are based on theories of energy flow in the body that can be manipulated to affect health. DIF: Cognitive Level: Comprehension REF: d. 183, Table 14-3 OBJ: Theory #5 TOP: Alternative Treatments KEY: Nursing Process Step: Planning MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A nurse is caring for a Catholic patient who has just given birth to a nonviable fetus. When considering the religion of this patient, the nurse should: • discourage baptism since the fetus is nonviable. w • • n o r m a l s a 5% glucose in water st pr ep .c om l i n e A N S : B Jehovahs Witnesses are not permitted to take blood into their bodies, but blood expanders such as Dextran can be infused. DIF: Cognitive Level: Application REF: d. 176, Box 14-1 OBJ: Clinical Practice #1 TOP: Religious Influence in Health Care KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • A practicing member of the Church of Jesus Christ of Latter Day Saints is being prepared for surgery on his left knee. The nurse should remove all the personal possessions with the exception of: • the wedding ring. the religious medallion around the neck. • undergarments. ng ur yn .m w w w l i n e n s o c k s . si • te • A N S: C Members of the Church of Jesus Christ of Latter-Day Saints may wear sacred undergarments that should only be removed in an emergency. If removed, the undergarments should be put back on as soon as possible. DIF: Cognitive Level: Application REF: d. 183, Table 14-1 OBJ: Clinical Practice #1 TOP: Religious Influence in Health Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A nurse is caring for a patient of the Muslim faith. The nurse would send the food tray back if it contains: • pork chops and sweet potatoes. • beef patty with mushroom sauce. • liver and mashed potatoes. crab cakes and rice with almonds. ANS: A Practicing Muslims do not consume pork or alcoholic beverages. They also forbid cremation. DIF: Cognitive Level: Application REF: d. 178, Box 14-2 OBJ: Clinical Practice #1 TOP: Religious Influence in Health Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A nurse is caring for a postpartum patient who adheres to the beliefs of Orthodox Judaism. The question that would be the most culturally sensitive would be: • Would you like crab cakes for your lunch? ur si ng te st pr ep .c om • Would you like your husband to give you a back rub? • Has your husband decided on a name for your new baby? yn • Will your doctor circumcise your baby tomorrow? ANS: C Practicing members of Orthodox Judaism name their male children 8 days after being born, when circumcision is performed. Babies are named by the father. The Orthodox Jewish man cannot touch the woman until after the ritual bath (mikvah). Jewish persons are discouraged from eating shellfish. DIF: Cognitive Level: Application REF: d. 178, Box 14-2 OBJ: Clinical Practice #1 TOP: Religious Influence in Health Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse supervisor becomes concerned when observing the nurse caring for an Orthodox Jewish patient preparing to trim the patients beard with a(n): • pair of scissors. w w w .m • • electric razor. • razor blade. .c ep pr st te ng si ur yn .m b a r b e r s s t r a i g h t r a z o r . A N S : C om • w w w Practicing members of Orthodox Judaism view the beard as a sign of holiness, and no blade must touch the skin. Scissors or an electric razor may be used. DIF: Cognitive Level: Application REF: d. 183, Table 14-3 OBJ: Clinical Practice #1 TOP: Religious Influence in Health Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity • A young Hindu woman who is part of a traditional Hindu family is in a coma and is going to be transferred to the ICU. The family member whom the nurse should consult about this health matter would be the: • eldest woman in the family. • family council. • patients husband. • w w w .m yn ur si ng te st pr ep .c om t h e o l d e r s i b l i n g s . A N S : A Traditional Hindu families consider the eldest woman in the family to be the authority on health and healing matters. She should be consulted and included in any patient teaching. DIF: Cognitive Level: Application REF: d. 178 OBJ: Clinical Practice #1 TOP: Religious Influence in Health Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • An example of an ethnocentric remark would be: • I think Catholics should have as many children as they want. • I dont see why Muslims cant pray in church like we Protestants do. • You have to admire the Asian immigrants for keeping all their eastern traditions. • It seems that Hispanics have taken over this country. ANS: B Ethnocentrism is the tendency of human beings to think that their way of thinking, believing, and doing things is the only way or the only right way. Beliefs that greatly differ from ones own are seen as strange and are therefore considered wrong. DIF: Cognitive Level: Comprehension REF: d. 180 • make sure all females are cared for by females. • refrain from sitting with the sole of my shoe visible. om OBJ: Clinical Practice #5 TOP: Ethnocentrism KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A nursing instructor is teaching a group of nursing students about cultural values practiced by Arab Americans. The nursing instructor would recognize the need for further teaching if a nursing student states, I will: • offer Arab-American patients items using my left hand. refrain from offering Arab-American patients pork. ANS: A Arab Americans do not eat pork or drink alcohol. It is considered rude to pass things with the left hand because it is considered unclean. It is considered rude to sit with the sole of the shoe within view of someone. Arab women are uncomfortable with care performed by males. st pr ep .c • • diabetes mellitus. w .m sickle cell anemia. w s i c k l e c e l l t r • w • yn ur si ng te DIF: Cognitive Level: Comprehension REF: d. 183, Table 14-3 OBJ: Clinical Practice #1 TOP: Religious Influence in Health Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: psychosocial adaptation • A nurse caring for a newborn of Eastern European Jewish ancestry is aware that this patient is predisposed to: • Tay-Sachs disease. • sickle cell anemia st Tay-Sachs disease te • pr ep .c om a i t . A N S : A People of Eastern European Jewish ancestry may carry the trait for a fatal neurologic disorder of infancy called Tay-Sachs disease. DIF: Cognitive Level: Comprehension REF: d. 184 OBJ: Clinical Practice #1 TOP: Religious Influence in Health Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • A home health nurse caring for a patient of American Indian ancestry will be particularly alert to symptoms of because of a genetic predisposition to that illness. • diabetes mellitus ng • w w w .m yn ur si s i c k l e c e l l t r a i t A N S : A Diabetes is more common among the Hispanic and American Indian populations because of a genetic susceptibility. te st pr ep .c om DIF: Cognitive Level: Knowledge REF: d. 184 OBJ: Clinical Practice #1 TOP: Religious Influence in Health Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort COMPLETION • Persons of African extraction are predisposed to the three , and . disorders of , ANS: sickle cell anemia; sarcoidosis; keloids People of African or Mediterranean heritage are prone to sickle cell anemia and trait, sarcoidosis, and keloids. DIF: Cognitive Level: Knowledge REF: d. 184 OBJ: Theory #1 TOP: Racial Predisposition KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The term developed to describe care that recognizes cultural diversity and that is sensitive to the cultural needs of the patient is . ANS: transcultural nursing w w w .m yn ur si ng Recognizing the need for culturally diverse capabilities in nursing is a growing aspect of health care, especially in our global community. DIF: Cognitive Level: Knowledge REF: d. 179 OBJ: Theory #1 TOP: Transcultural Nursing KEY: Nursing Process Step: N/A MSC: NCLEX: N/A described by Dr. Madeline Leininger is the • The concept of force that allows people to grow, remain well, and avoid or face death. ANS: human caring Dr. Leininger described human caring as the force that allows people to grow, remain well, avoid illness, and face or survive death. DIF: Cognitive Level: Knowledge REF: d. 179 OBJ: Theory #2 TOP: Human Caring KEY: Nursing Process Step: N/A MSC: NCLEX: N/A MULTIPLE RESPONSE • Although the words spirituality and religion are often used interchangeably, spirituality actually refers to which of the following? (Select all that apply.) • Concerns of the spirit • Formalized system of beliefs • Understanding ones place in the world • An element of religion Belief in a higher power or creative force ANS: A, C, D, E Spirituality and religion are similar, but both must be addressed for the patients psychosocial integrity to improve. DIF: Cognitive Level: Comprehension REF: d. 175 OBJ: Theory #1 TOP: Spirituality and Religion KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The nurse takes into consideration that culture and religion influence life choices that include: (Select all that apply.) • smoking. • frequency of intercourse. • nutrition. • reading material. pr drug use. te st • ep .c om • si ur yn .m w w w u s e o f c a f f e i n e . A N S : A , B , D ng • basis of a value system. • rational explanation of lifes mysteries. • meaningful employment. te • st • pr ep .c MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse is aware that cultural influences shape the worldview of all people, which define for each person the concepts of the: (Select all that apply.) • meaning of lifes events. om , E , F The use of drugs (including caffeine, tobacco, and alcohol), nutritional choices, and food preparation are influenced by culture. DIF: Cognitive Level: Comprehension REF: d. 174 OBJ: Theory #1 TOP: Cultural Influences on Life Choices KEY: Nursing Process Step: Planning w w w .m yn ur si ng differenc e between good and evil. ANS: A, B, C, E The worldview of an individual shapes his or her value system, defines right and wrong, and helps to explain lifes events and mysteries. Significance of employment is not included in a worldview. DIF: Cognitive Level: Comprehension REF: d. 175 OBJ: Theory #1 TOP: Worldview KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity: coping and adaptation • Protestant denominations that use their own holy books in addition to the Bible include: (Select all that apply.) • Baptists. • • Christian Scientists. • Mormons. • Lutherans. .c om E p i s c o p a l i a n s . te st pr ep ANS : B, C Protestant denominations that use another holy book in addition to the Bible are Christian Scientists, Mormons, Jehovahs Witnesses, and the Unification Church. si ng Chapter 7 The Nurse–Client Relationship MULTIPLE CHOICE • The nurse can best ensure that communication is understood by: • speaking slowly and clearly in the patients native language. asking the family members whether the patient understands. • obtaining feedback from the patient that indicates accurate comprehension. yn ur • checking for signs of hearing loss or aphasia before communicating. ANS: C The best way to determine understanding is to ask the patient. Factors such as anxiety, hearing acuity, language, aphasia, or lack of familiarity with medical jargon or routines can all contribute to misunderstanding. DIF: Cognitive Level: Comprehension REF: pp. 100-101 OBJ: Theory #1 TOP: Feedback KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: basic care and comfort w w w .m • • The nurse recognizes a verbal response when the patient: • nods her head when asked whether she wants juice. • writes the answer to a question asked by the nurse. • begins sobbing uncontrollably when asked about her daughter. • is moaning and restless and appears to be in pain. ANS: B Verbal communication involves words, either written or spoken. Nodding, sobbing, and moaning are nonverbal communication. DIF: Cognitive Level: Comprehension REF: d. 99 OBJ: Theory #1 TOP: Verbal Communication Feedback KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse recognizes the patient who demonstrates communication congruency when the patient: • smiles and laughs while speaking of feeling lonely and depressed. wrings her hands and paces around the room while denying that she is upset. • is tearful and slow in speech when talking about her husbands death. om • states she is comfortable while she frowns and her teeth are clenched. ANS: C Congruent communication is the agreement of verbal and nonverbal messages. DIF: Cognitive Level: Comprehension REF: d. 99 OBJ: Theory #1 TOP: Congruence KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A Hispanic patient approaches the Asian nurse and, standing very close, touches the nurses shoulder during their conversation. The nurse begins to step back to 18 to 24 inches, while smiling and nodding to the patient. This situation is most likely an example of: • the nurses need to maintain a professional role rather than a social role. ur si ng te st pr ep .c • a patients attempt to keep the nurses attention. • a nurses need to establish a more appropriate location for conversation. yn • a difference in culturally learned personal space of the nurse and the patient. ANS: D Personal space between people is a culturally learned behavior; Asians, North American natives, and Northern European people generally prefer more personal space than people of Hispanic, Southern European, or Middle Eastern cultures. DIF: Cognitive Level: Comprehension REF: d. 100 OBJ: Theory #2 TOP: Cultural Differences KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A nurse says to a patient, I am going to take your TPR, and then Ill check to see whether you can have a PRN analgesic. In considering factors that affect communication, the nurse has: • used terminology to clearly inform the patient of what she is doing. w w w .m • • given information that is unnecessary for the patient to know. • used medical jargon, which might not be understood by the patient. taken into consideration the patients need to know what is happening. ANS: C Medical jargon such as abbreviations or medical terminology is often misunderstood, even by well-educated people. DIF: Cognitive Level: Comprehension REF: d. 101 OBJ: Theory #3 TOP: Blocks to Communication KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A nurse using active listening techniques would: use nonverbal cues such as leaning forward, focusing on the speakers face, and slightly nodding to i • message has been heard. • avoid the use of eye contact to allow the patient to express herself without feeling stared at or deme anticipate what the speaker is trying to say and help the patient express herself when she has difficu • sentence. pr ep .c om • ask probing questions to direct the conversation and obtain the information needed as efficiently as ANS: A Eye contact is a culturally learned behavior and in some cases may not be appropriate. Probing questions or finishing the patients sentence is not part of active listening and is detrimental to an interview. DIF: Cognitive Level: Comprehension REF: d. 101 OBJ: Theory #3 TOP: Active Listening KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • When the patient says, I dont want to go home, the nurses best therapeutic verbal response would be: • Im sure everything will be fine once you get home. Doesnt your family want you to come home? w • You dont want to go home? w • .m yn ur si ng te st • I felt like that when I had surgery last year. ANS: B The use of reflecting encourages the patient to expand on his or her feelings or thoughts. DIF: Cognitive Level: Application REF: d. 103, Table 8-1 OBJ: Theory #3 TOP: Communication Techniques KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation w • To begin talking with a newly admitted patient about pain management, the nurse would most appropriately state: • You look pretty comfortable. Are you having any pain? • Tell me about the pain youve been having. • Is this pain the same as the pain you had yesterday? • Dont worry; this pain wont last forever. ANS: B ng te st pr ep .c An open-ended question allows the patient to express his or her feelings or needs. DIF: Cognitive Level: Application REF: d. 103, Table 8-1 OBJ: Theory #3 TOP: Communication Techniques KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • When a patient begins crying during a conversation with the nurse about the patients upcoming surgery for possible malignancy, the nurses most therapeutic response would be: • Your surgeon is excellent, and I know hell do a great job. om • Oh, dear, your gown is way too big, let me get you another one. • Dont cry; think about something else and youll feel better. ur si • Here is a tissue. Id like to sit here for a while if you want to talk. ANS: D Offering self, or presence, and accepting a patients need to cry is supportive. DIF: Cognitive Level: Application REF: d. 103, Table 8-1 OBJ: Theory #3 TOP: Therapeutic Techniques KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • To enhance the establishment of rapport with a patient, the nurse should: • identify himself by name and title each time he introduces himself. w w w .m yn • • share his own personal experiences so that the patient gets to know him as a friend. • act in a trustworthy and reliable manner; respect the individuality of the patient. • share information with the patient about other patients and why they are hospitalized. ANS: C Trust and reliability, as well as conveying respect for the individual, all promote rapport. Identifying oneself is important but in itself does not promote rapport. Sharing personal experiences or divulging the confidential nature of other patients conditions is not appropriate in the nursepatient relationship. DIF: Cognitive Level: Comprehension REF: d. 107 OBJ: Clinical Practice #2 TOP: Rapport KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse explains that the therapeutic nursepatient relationship differs from the social relationship because: • a social relationship does not have goals or needs to be met. the nursepatient relationship ends when the patient is discharged. • the focus is mainly on the nurse in the nursepatient relationship. om • a social relationship does not require trust or sharing of life experiences. ANS: B The nursepatient relationship is limited to the patients stay in the facility and is focused on the patient. A social relationship may have goals or needs and does require trust and sharing of life experiences. DIF: Cognitive Level: Comprehension REF: pp. 106-107 OBJ: Theory #4 TOP: Relationships KEY: Nursing Process Step: Implementation te st pr ep .c • ur si ng MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse has selected an outcome for the patient to eat all of the food on the breakfast tray each day. Assessing that the patient has eaten all of the breakfast, the nurse would give positive feedback by saying: • Wow! That breakfast must have been pretty good. I like pancakes too. Everyone on the hall seemed to enjoy them. • I hope you can keep all that breakfast down. .m yn • Hurray! You finished your whole meal! What would you like for tomorrow? ANS: D Giving positive feedback increases the likelihood of the desired behavior to be repeated. Commenting on the tastiness of the food or the fact that others liked it is not responding directly to the patients having eaten the whole meal. DIF: Cognitive Level: Application REF: d. 100 OBJ: Theory #9 TOP: Positive Feedback KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A 67-year-old woman had major abdominal surgery yesterday. She has IV lines, a urinary catheter, and an abdominal wound dressing, and she is receiving PRN pain medication. The end- ofshift report that best conveys the patient status is: • Doing great, was up in the chair most of the day. No complaints of pain or w w w • discomfort. Voiding ade Abdominal surgery yesterday, dressing is dry and intact, her IVs are on time and shes had pain med • stable. Abdominal dressing dry, IVs800 mL left in #6; NS running at 125 mL/hr; urine output 800 mL this • 15 mg for pain at 8:00 AM and at 1:30 PM. Shes comfortable now. Vital signs are stable, no fever. om Unchanged since this morning. She wanted to know how soon she can have something to eat, so ma d. ep .c ANS: C pr check with her doctor this evening. Her husband has been visiting all day and will let you know if s ur si ng te st This brief clear report addresses the major concerns of the abdominal dressing, the status of the IV fluids, vital signs, and analgesia needs. DIF: Cognitive Level: Application REF: pp. 109-110 OBJ: Clinical Practice #4 TOP: Shift Report KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care • An aspect of computer use in patient care in which the LPN may need to be proficient includes: • input of data such as requests for radiographs or laboratory services. .m scheduling admissions, discharges, and nurse staffing to keep the unit at the best occupancy and uti ANS: A Many facilities use computers for data entry relative to requesting radiograph or lab services and physical assessment and medication administration. Programming such computers is not a w w • teaching patients how to use hospital computers to access information such as discharge instruction relative to specific medications. w • programming the computer to record data from physicians and other health care workers. yn • nursing task, and patients need to have individualized information about discharge and medications. DIF: Cognitive Level: Knowledge REF: pp. 110-111 OBJ: Theory #8 TOP: Computer Use KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A patient with a nursing diagnosis of Sensory perception, disturbed auditory, would most appropriately require the nurse to: • obtain a sign language interpreter when a family member is unavailable. • speak slowly and distinctly, but not shout. • provide bright lighting without glare and orient frequently. reorient frequently to time, place, staff, and events. ANS: B A patient with disturbed auditory perception cannot hear well (or at all); therefore, speaking slowly and distinctly without shouting increases patient comprehension. DIF: Cognitive Level: Application REF: pp. 107-108 OBJ: Clinical Practice #3 TOP: Hearing-Impaired Patient Communication KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • When an office nurse asks the patient to repeat information that he has just given to the patient over the telephone, the nurse is: • testing the patients intelligence and memory. st pr ep .c om • acting in a cautious way to avoid charges of negligence. • verifying that the patient understands the information. te • saving the extra time it would take to mail the information. ANS: C Obtaining feedback from a patient to ascertain that the patient understands instructions is an important part of the communication process, especially over the phone, when the nurse does not have nonverbal cues. DIF: Cognitive Level: Comprehension REF: pp. 100-101 OBJ: Theory #3 TOP: Telephonic Communication KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A 36-year-old woman who is in traction for a fractured femur that she received in an auto accident is found crying quietly. The nurse can best address this situation by saying: • Whats the matter? Why are you crying? Are you in pain? w w w .m yn ur si ng • • Stop crying and tell me what your problem is. • This could have been much worse. Youre lucky no one was killed. • You are upset. Can you tell me whats wrong? ANS: D The nurse offers a general lead as to what is causing the distress. The other options are judgmental or clichs or offer no opportunity for the patient to express feelings. DIF: Cognitive Level: Application REF: d. 103, Table 8-1 OBJ: Theory #3 TOP: Reflecting Observations KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • When the nurse is giving direction to a nursing assistant who is being delegated part of the patient care, the nurses most effective direction would be: • Do the morning care first on the patients in 205 and 206 who cant get out of bed. You take care of all the patients in 205 and 206. Let me know how youre doing and whether you ne • Give the patient in 204A a shower after breakfast, and call me to check her feet before you get her d .c om • Take the vital signs on all the patients in the lounge and tell me whether there are problems. ANS: C The clarity and brevity of the direction makes the delegated task clear and leaves the responsibility of assessment to the nurse. DIF: Cognitive Level: Application REF: d. 110 OBJ: Theory #7 TOP: Delegation KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: coordinated care • When the patient says, I get so anxious just lying here in this hospital bed. I have a million things I should be doing at home, the most empathetic response would be: • Id feel the same way you do. I know just what youre going through. ur si ng te st pr ep • It sounds like youre having a tough time dealing with this situation. • Its always darkest before the dawn. Hang in there; it will get better. yn • You sound pretty sorry for yourself. Why dont you look at the positives? ANS: B Empathy recognizes a patients situation and encourages expression of feelings. DIF: Cognitive Level: Application REF: d. 107 OBJ: Theory #3 TOP: Empathy KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A patient asks the nurse, What would you do if you had cancer and had to choose between surgery and chemotherapy? The reply that can best help the patient is: • If I were you, I would choose surgery and then consider chemo afterward. w w w .m • • What solutions have you considered? • I would talk it over with my friends first. I dont know. Im glad it isnt my decision. ANS: B Nurses can help by reminding patients of alternatives open to them and should refrain from giving advice but can encourage the patient to consider options. The nurse may be glad not to face a decision a patient must, but it is not helpful to the patient to say this. DIF: Cognitive Level: Application REF: d. 103, Table 8-1 OBJ: Theory #3 TOP: Offering Alternatives KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse chooses to use touch in the nursepatient relationship because touch: • can convey caring and support when words are difficult. pr ep .c om • should be avoided because of problems of cultural misinterpretation. • is appropriate only in special circumstances, such as with young children. st • is a nursing intervention of choice in almost all situations. ANS: A Touch is a powerful and supportive nonverbal communication in many situations. It is appropriate for all ages, but not in some situations. Careful assessment of the patients situation and cultural values should determine its use, but it should not be avoided because of stereotypes. DIF: Cognitive Level: Comprehension REF: d. 103 OBJ: Theory #4 TOP: Caring Touch KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • When the nurse makes the statement, We can come back to that laterright now I need to know about when your symptoms started, the nurse is: • letting the patient know that topic of conversation was inappropriate. w w w .m yn ur si ng te • • setting limits on the expression of feelings. • refocusing the patient to the issue at hand when the conversation has wandered. • closing off the conversation by quickly getting to the point of the interview. ANS: C Refocusing is often necessary to accomplish data collection. It does not block communication and is not used to close a conversation or stop an inappropriate topic. DIF: Cognitive Level: Comprehension REF: d. 102 OBJ: Theory #3 TOP: Refocusing Communication KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A patient who has had a stroke is unable to speak clearly and has right-sided hemiplegia. The nurse will design the approach to the assessment interview by: • asking questions and explaining procedures to the patients daughter. • speaking slowly and giving the patient time to respond. • telling the patient he will get all necessary information from the daughter. prompting the answers and finishing the sentences for the patient. ANS: B Speaking slowly recognizes that the patient may process (if able) information more slowly. DIF: Cognitive Level: Application REF: d. 103, Table 8-1 OBJ: Clinical Practice #3 TOP: Impaired Communication KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • When a nurse is conducting an assessment interview, the most efficient technique would be: • explaining the purpose of the interview. te st pr ep .c om • excluding relatives and friends from the interaction. • telling the patient what data are already available. • asking closed questions to obtain essential information. ANS: D yn ur si ng • w w w .m Closed questions have a definite place when the nurse wants to obtain specific essential data. Closed questions force the patient to stick to the topic. DIF: Cognitive Level: Comprehension REF: d. 102 OBJ: Clinical Practice #1 TOP: Interview KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • While interviewing a Native American man for the admission history, the nurse should expect to: • wait patiently through long pauses in the conversation. • maintain eye contact with the patient. • give the patient permission to speak. • have another family member speak for the patient. ANS: A Native Americans use long pauses in their conversation to better consider their answer and consider the question. The culturally sensitive nurse would wait quietly through the pauses. DIF: Cognitive Level: Comprehension REF: d. 102 OBJ: Clinical Practice #1 TOP: Cultural Considerations KEY: Nursing Process Step: Planning MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse is aware that the purpose of therapeutic communication is to: • gather as much information as possible about the patients problem. direct the patient to communicate about his deepest concerns. • focus on the patient and the patient needs to facilitate interaction. om • gain specific medical information and history of illness. ANS: C Therapeutic communication is a conversation that is focused on the patient and promotes understanding between the sender and the receiver. DIF: Cognitive Level: Comprehension REF: d. 102 OBJ: Theory #4 TOP: Therapeutic Communication KEY: Nursing Process Step: Planning MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The practical nursing student who is engaged in a therapeutic communication with a patient will have the most difficulty with the technique of: • closed questions. si ng te st pr ep .c • restating. • using general leads. yn ur • w w w .m • silence. ANS: D The use of silence is the hardest for most students to develop because it makes them uncomfortable, so they tend to end it prematurely. DIF: Cognitive Level: Comprehension REF: d. 102 OBJ: Theory #31 TOP: Silence KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • To convey the intervention of active listening, the nurse would: • maintain eye contact by staring at the patient. • prompt the patient when the patient stops talking for a moment. • make a conscious effort to block out other sounds in the immediate environment. • write down remarks on a clipboard to facilitate later topics of conversation. ANS: C An active listener maintains eye contact without staring, gives the patient full attention, and makes a conscious effort to block out other sounds and distractions. DIF: Cognitive om Level: Comprehension REF: d. 101 OBJ: Theory #3 TOP: Active Listening KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • When the nurse enters the room, the patient is laughing out loud at something on TV. The patient stops and apologizes for the laughter, saying, I guess I ought not be laughing at all since I am stuck here with two broken legs. The nurse can use evidencebased information when she responds: • Laughter is nearly always a cover-up for anxiety when facing a long rehabilitation. Long periods of laughter decrease the amount of oxygen available to your body for healing. • Laughter in a hospital is often distracting and depressing to other patients nearby. ep .c • Laughter truly is the best medicine as it has a positive effect on the immune system. ANS: D Hasen and Hasen (2009) found that laughter and appropriate use of humor decreased stress and anxiety and had a positive effect on the immune system. DIF: Cognitive Level: Application REF: d. 101 OBJ: Clinical Practice #2 TOP: Use of Laughter KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • When interacting with an elderly patient, the nurse would enhance communication by: • speaking slowly in order to allow the patient to process the message. ur si ng te st pr • addressing him by his first name to encourage a therapeutic relationship. • standing in the doorway rather than entering the room to give the elderly patient more privacy. .m yn • speaking in simple sentences, as if to a child. ANS: A When interacting with an elderly person, the nurse should try not to speak too quickly or expect an immediate answer because the elderly take more time to process the message. Do not use baby talk or speak to them as if they were children. DIF: Cognitive Level: Comprehension REF: d. 101 OBJ: Theory #2 TOP: Communication KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • When the nurse observes a resident in a long-term facility pounding his fists on his legs and grinding his teeth, the nurse will validate her perception of the patients non-verbal expression of w w w • anger by: • documenting that the patient was agitated and appeared angry. • asking the male nursing assistant if it is his perception that the patient appears angry. • accessing the nursing care plan to ascertain if there is a nursing diagnosis relative to anger. sitting down near the patient and saying, You seem upsetcan I help? ANS: D All perceptions based on the observation of non-verbal behavior should be validated by consulting the patient. DIF: Cognitive Level: Application REF: d. 100 OBJ: Theory #9 TOP: Validating Perceptions KEY: Nursing Process Step: Assessment | Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • When a patient states, I dont feel like walking today, the nurses most therapeutic verbal response would be: • You have to walk today. te st pr ep .c om • You dont want to walk today? • I dont feel like walking today either. ng • Why dont you want to walk today? ANS: B Reflection is a way to restate the message. The idea is simply reflected back to the speaker in a statement to encourage continued dialogue on the topic. DIF: Cognitive Level: Application REF: d. 103, Table 8-1 OBJ: Theory #3 TOP: Communication Techniques KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • When a patient states, My son hasnt been to see me in months, the nurses best verbal response is: • Dont worry; Im sure your son will visit. w w w .m yn ur si • • Your son hasnt been around much lately? • My son doesnt come to visit me either. • How terrible that he doesnt Did you sleep all night without waking? • How many bowel movements have you had today? • What was your daughters reaction to your desire for hospice? ANS: D st pr ep • .c om visit you. ANS: B Restating in different words what the patient said encourages further communication on that topic. DIF: Cognitive Level: Application REF: d. 103, Table 8-1 OBJ: Theory #3 TOP: Communication Techniques KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • An example of a nurse communicating with a patient using open-ended questions would be: • Is your pain less today than it was yesterday? w w w .m yn ur si ng te An open-ended question is broad, indicating only the topic, and it requires an answer of more than a word or two. Use of an open-ended question or statement allows the patient to elaborate on a subject or to choose aspects of the subject to be discussed. Open-ended questions or statements are helpful to open up the conversation or to proceed to a new topic. They usually cannot be answered with one word or just yes or no. DIF: Cognitive Level: Comprehension REF: d. 103, Table 8-1 OBJ: Theory #3 TOP: Communication Techniques KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse tells a patient, For the last 2 days we have talked about whether to notify your daughter of your upcoming surgery in 2 days. You have indicated you do not want to be a burden to her, but you also would like to have her here. You may have to decide rather quickly because of the time constraint. The nurse is using the technique of: • focusing. • s u • reflection. • restatement. • reflection. w w w .m • o f f e r i n g s e l f . A ur restatement. yn • si ng te st pr ep .c om m m a r i z i n g . A N S : D Summarizing presents the problem and possible solutions with the attendant difficulties. This technique unclutters the problem and presents it back to the patient for his or her choice of a solution. DIF: Cognitive Level: Comprehension REF: d. 104 OBJ: Theory #3 TOP: Communication Techniques KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse is caring for a patient who states, I tossed and turned last night. The nurse responds to the patient, You feel like you were awake all night? This is an example of: • an open-ended question. ep .c om NS :B Restatement is a therapeutic communication technique in which the nurse restates in different words what the patient said. This encourages further communication on that topic. DIF: Cognitive Level: Comprehension REF: pp. 102-103 OBJ: Theory #3 TOP: Restatement KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse is caring for a patient who has just had a mastectomy (breast removal). The patient expresses concern that her husband will no longer find her attractive because of her mastectomy. The nurse appropriately responds: • Youre concerned your husband will find you unattractive because of your mastectomy? Youre a beautiful woman; of course your husband will find you attractive after your mastectomy. • Dont worry; when I had my mastectomy, my husband still found me very attractive. te st pr • You should leave your husband immediately if he thinks youre unattractive after a mastectomy. ANS: A This is an example of restatement, which allows the patient to know her message was understood and encourages the patient to continue about her concerns on the topic. DIF: Cognitive Level: Application REF: pp. 102-103 OBJ: Theory #3 TOP: Restatement/Reflection KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A patient states, Im so worried that I might have cancer. The nurse responds, It is time for you to eat breakfast. The nurses response is an example of: • using clichs. w w .m yn ur si ng • judgmental response. • changing the subject. w • • g i v i n g f summarizes the patients concerns and closes communication. w • shows a judgmental attitude on the part of the nurse. w • .m yn ur si ng te st pr ep .c om a l s e r e a s s u r a n c e . A N S : C Changing the subject is a block to effective communication in which the patient is deprived of the chance to verbalize concerns. DIF: Cognitive Level: Comprehension REF: d. 104 OBJ: Theory #3 TOP: Changing the Subject KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse is aware that the use of false reassurance is harmful to the nursepatient relationship, because this communication block: • discounts the patients stated concerns. confuses the patient by giving information. ANS: A Giving false reassurance is a block to effective communication in which the patients feelings are negated and in which the patient may be given false hope, which, if things turn out differently, can destroy trust in the nurse. DIF: Cognitive Level: Comprehension REF: d. 104 OBJ: Theory #3 TOP: False Reassurance KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping w • and adaptation • A home health patient with a bleeding ulcer informs the nurse that she ate a bowl of chili with jalapenos. An inappropriate communication block with a judgmental tone by the nurse would be: • Well, you have had this problem long enough to know what will happenyou certainly cant blame m I dont think that was a smart thing for you to do considering your ulcer. • Well, you better watch your stool for evidence of blood so you can notify your physician. • Oh, poo! A bowl of chili every now and then wont make a lot of difference to your ulcer. ANS: B .c om • • defensive response. w .m giving advice. w u s i n g c l i c h s . • w • yn ur si ng te st pr ep Judgmental response is a block to effective communication in which the nurse is judging the patients action. It implies that the patient must take on the nurses values and is demeaning to the patient. DIF: Cognitive Level: Analysis REF: d. 105, Table 8-2 OBJ: Theory #3 TOP: Judgmental Response KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A patient tells the nurse that she dislikes the food that is served in the hospital. The nurse responds, Our cooks work very hard; the food that is served is very good. The nurses response is an example of the communication block of: • judgmental response. Defensive response • Inattentive listening st • pr ep .c om A N S: C Defensive response is a block to effective communication in which the nurse responds by defending the hospital food. This prevents the patient from feeling that she is free to express her feelings. DIF: Cognitive Level: Comprehension REF: d. 105 OBJ: Theory #3 TOP: Defensive Response KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A nurse caring for a patient who fell off the roof while he was intoxicated asks the patient, Why in the world were you on the roof when you had been drinking? The nurses statement is an example of which type of communication? • Changing the subject w w ng si ur yn w .m A s k i n g p r o b i n g q u e s t i o n s A N S te • Asking probing questions • Using clichs ep • .c om : D Asking probing questions is a block to effective communication in which the nurse pries into the patients motives and therefore invades privacy. DIF: Cognitive Level: Comprehension REF: d. 105 OBJ: Theory #3 TOP: Probing KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse caring for a patient who is concerned about her 10pound weight loss relative to her chemotherapy tells the patient, Lucky you! Every cloud has a silver lining. The nurses statement is an example of which type of communication block? • Defensive response st te ng si ur yn .m w w w C h a n g i n g t h e s u b j e c t A N S : C pr • Using clichs is a block to effective communication in which the patients individual situation is negated, and the patient is stereotyped. This type of response sounds flippant and prevents the building of trust Giving advice • Using clichs .c • om between the patient and the nurse. DIF: Cognitive Level: Comprehension REF: pp. 105-106 OBJ: Theory #3 TOP: Clichs KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse is caring for a patient with a diagnosis of lung cancer. The nurse states, If I were you, I would have radiation therapy. The nurses statement is an example of which type of communication block? • Inattentive listening ep • w w w .m yn ur si ng te st pr D e f e n s i v e r e s p o n s e A N S : B Giving advice is a block to effective communication and tends to be controlling and diminishes patients responsibility for taking charge of their own health. DIF: Cognitive Level: Comprehension REF: d. 105, Table 8-2 OBJ: Theory #3 TOP: Giving Advice KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse is caring for a patient who is concerned about living alone. The best response by the nurse is: • Where have you considered living? • Why dont you live with your family? • I think you should live with your family. If you were my mom, Id have you live with me. ANS: A Rephrasing will help the patient explore various alternatives. The nurse should not use phrases such as Why dont you, When that happened to me, I did, or I think you should. Rephrasing, for example, Have you thought of your options? or You might want to think about, or Have you considered? will help the patient explore various alternatives. DIF: Cognitive Level: Application REF: d. 104 OBJ: Theory #3 TOP: Offering Alternatives KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The characteristic that is representative of the nursepatient relationship is that this relationship: • focuses on the nurses ability to build rapport. continues after discharge. • does not include humor. • focuses on the assessed patient health problems. ANS: D yn ur si ng • te st pr ep .c om • w w w .m The nursepatient relationship focuses on the patient, has goals, and is defined by specific boundaries. The relationship takes place in the health care setting, and boundaries are defined by the patients problems, the help needed, and the nurses professional role. When the patient is discharged, the relationship ends. DIF: Cognitive Level: Knowledge REF: pp. 106-107 OBJ: Theory #4 TOP: NursePatient Relationship KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • When communicating with an aphasic patient, the nurse appropriately: • speaks quickly and shouts so the patient can hear. • assumes the patient can understand what is heard. • speaks to the patients caregiver about the patient. • assumes the patient cannot understand what is heard. ANS: B • uses long, complex sentences. .c speaks directly into the patients ear. ep • om When communicating with an aphasic patient, the nurse assumes the patient can understand what is heard even though speech is jargon or the person is mute, unless deafness has been diagnosed. The nurse should talk to the patient, and not talk to someone else in the room about the patient. The nurse should speak slowly and distinctly and should not shout. DIF: Cognitive Level: Comprehension REF: d. 108, Box 8-1 OBJ: Clinical Practice #3 TOP: Impaired Communication KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • When communicating with a hearing-impaired patient, the nurse appropriately: • shouts repeatedly at the patient. • w w w .m yn ur si ng te st pr use s sho rt, sim ple sent enc es. AN S: D When communicating with a hearing-impaired patient, the nurse appropriately uses short, simple sentences. The nurse should not shout because this can distort speech and does not make the message any clearer. The nurse should never speak directly into the persons ear. This can distort the message and hide all visual cues. DIF: Cognitive Level: Comprehension REF: d. 108, Box 8-1 OBJ: Clinical Practice #3 TOP: Impaired Communication KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • When communicating with a preschooler, the nurse should: • use abstract explanations. • use unfamiliar language. • use long, complex sentences. • consider the developmental level, using familiar words. ANS: D offering advice. • interrupting frequently. ep • .c om When interacting with a toddler or a preschooler, the nurse should focus on the childs needs and concerns. The nurse should also use simple, short sentences and concrete explanations with familiar words. DIF: Cognitive Level: Comprehension REF: d. 109 OBJ: Clinical Practice #3 TOP: Communication with Children KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • When communicating with an adolescent, the nurse should be very sensitive to avoid: • asking embarrassing questions. pr • w w w .m yn ur si ng te st u s i n g a c t i v e l i s t e n i n g . A N S : C An adolescent needs time to talk. The nurse should use active listening, avoid interrupting, and show acceptance. The nurse should try not to give advice. DIF: Cognitive Level: Comprehension REF: d. 109 OBJ: Clinical Practice #3 TOP: Communication KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The physician informs the student nurse that he would like to give a telephone order. The best response by the student is: • document the telephone order on the physicians orders. • ask another student to listen as a witness to the telephone order. • tape-record the physician giving the order to the student nurse. ask the registered nurse to take the telephone order. ANS: D The student nurse should have an instructor or another registered nurse standing by to take the new orders from the physician because students cannot legally take telephone orders. DIF: Cognitive Level: Application REF: d. 110 OBJ: Theory #6 TOP: Telephone Orders KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A nurse is delegating to a nursing assistant. The most appropriate form of this type of communication would be: • Let me know if Mr. Jones temperature is high. ng te st pr ep .c om • I need to know if Mr. Jones blood pressure is elevated. • Come and get me if Mr. Jones has a high heart rate. si • If Mr. Jones heart rate is greater than 100, let me know. ANS: D It is important to communicate well in order to assign tasks and delegate to others effectively. The nurse should give clear, concise messages that include the desired results. DIF: Cognitive Level: Comprehension REF: d. 110 OBJ: Theory #7 TOP: Delegation KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care • In order to safeguard patient information when using a computer, the nurse should: w w w .m yn ur • • only use the computer located in the nurses station. • wait until the end of the shift and chart all information at one time. • use personal code words and abbreviations to disguise information. • change the computer password frequently. ANS: w w w .m yn ur si ng te st pr ep .c om D Computerized patient information requires extra vigilance by the nurse to safeguard confidentiality. Changing personal passwords frequently helps safeguard information. When using the computer at a health care facility, the nurse must remember not to leave a computer screen open when he or she is finished. The nurse should always log out so that someone else cannot access information using his or her password and must not share his or her password with others. Computers in the nurses station are not as convenient as those at the bedside or in the hall. Personal codes and abbreviations are not useful. DIF: Cognitive Level: Comprehension REF: d. 111 OBJ: Theory #8 TOP: Patient Information Safety KEY: Nursing Process Step: N/A MSC: NCLEX: N/A COMPLETION • Pain is often conveyed through non-verbal communication. Two and other common, non-verbally expressed emotions are _ . ANS: anxiety; fear fear; anxiety Anxiety and fear can be expressed non-verbally by such behaviors as restlessness and picking at the bed covers. DIF: Cognitive Level: Knowledge REF: d. 100 OBJ: Theory #1 TOP: Nonverbal Communication KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: basic care and comfort • To elicit more information from a patient, the nurse should ask questions that require more than a one-word answer. This type of question is called . ANS: open-ended Open-ended questions provide more information than can be gathered from closed questions. DIF: Cognitive Level: Knowledge REF: d. 102 OBJ: Theory #1 TOP: Open-Ended Questions KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation gives the caregiver the • The communication technique of opportunity to ask and respond to questions. ANS: ISBAR-R ISBAR-R format allows the opportunity to ask and respond to questions concerning patient care during the end of shift report. The initials stand for introduction, situation, background, assessment, recommendation, and readback. DIF: Cognitive Level: Comprehension REF: d. 110 OBJ: Theory #9 TOP: ISBAR-R KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care MULTIPLE RESPONSE The nurse is alert to avoid using blocks to effective communication that include: (Select all that apply.) • changing the subject. using non-judgmental remarks. • giving advice. • asking probing questions. • offering hope. .c om • ep • • yn ur si ng te st pr u s i n g c l i c h s . w w w .m A N S: A, C, D, F Such behavior as changing the subject, giving advice, asking probing questions that probe into a patients motive, and using clichs all block communication. Offering hope and giving remarks that are non-judgmental are appropriate forms of communication. DIF: Cognitive Level: Comprehension REF: pp. 104-106 OBJ: Theory #3 TOP: Effective Communication KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • During the initial interview of a patient, the nurse should: (Select all that apply.) • assess the language capabilities of the patient. • use open-ended questions. • limit the interview to approximately 30 minutes. • assess comprehension abilities of the patient. • make the patient as comfortable as possible. obtain the patients medical history from the physician. ANS: A, C, D, E During the initial assessment, the patient should be comfortable and the nurse should ask closed questions to elicit specific information. The interview should last approximately 30 minutes, and the nurse needs to evaluate the language and comprehension skills of the patient to ensure effective communication. DIF: Cognitive Level: Comprehension REF: pp. 107-108 OBJ: Clinical Practice #1 TOP: Interview Skills KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • When using the telephone to communicate with a physician about a patient, the student nurse should have ready: (Select all that apply.) • current information relative to patients condition change. ng te st pr ep .c om • assessment of vital signs. • information on urinary output. • patients social security number or hospital identification number. ur si • w .m w w m e d i c a t i o n s r e c e i v yn • .c om e d . A N S : A , B , C , E ur si ng te st pr ep As a rule the physician does not need to have the social security number or the hospital identification number, but does need information on the patients condition, vital signs, urinary output, and medications received. DIF: Cognitive Level: Comprehension REF: d. 110 OBJ: Theory #6 TOP: Telephone Communication with a Physician KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care • The nurse will appropriately and deliberately use the closed question technique when the patient is: (Select all that apply.) • being asked for specific information. extremely anxious and unfocused. • having difficulty expressing feelings. • confused. .m yn • angry and ranting about his lack of medical care. ANS: A, B, D Closed questions are useful for gaining specific information such as age, address, and listing of allergies. Closed questions help the anxious, confused, and unfocused patient to respond. Patients who are having difficulty expressing feelings are not aided by closed questions. Angry patients need to be helped by silence or general leads. DIF: Cognitive Level: Application REF: d. 102 OBJ: Theory #3 TOP: Closed Questions KEY: Nursing Process Step: Intervention MSC: NCLEX: Psychosocial Integrity: coping and adaptation • Behaviors that indicate to the patient that the nurse is inattentive to the patients concerns are such activities as: (Select all that w w w • apply.) • turning back to straighten the bedside table while the patient is talking. • tapping feet or fingers. • sitting down in a chair near the bed with arms crossed. • leaving a hand on the door to go out. nodding and asking for elaboration . ANS: A, B, C, D Turning from the patient, tapping the feet or fingers, sitting with arms crossed, and leaving the patient all indicate to the patient that his or her concerns are not important and the information is boring to the nurse. Nodding and asking for elaboration indicate that the nurse is attentive and focused on his or her concerns. st pr ep .c om • ur si ng te Chapter 8 Client Teaching MULTIPLE CHOICE • Before beginning to teach a patient to give himself insulin, the nurse asks, Have you ever known anyone who gave himself insulin injections? This question is primarily designed to: • assess the patients learning needs. stimulate the patient to focus on the teaching goal. • reduce the patients anxiety relative to insulin injection. .m yn • reduce the amount of information the nurse has to provide. ANS: A Assessing a patients previous experience (as well as education, learning mode, and motivation) gives the nurse valuable information in developing a teaching plan tailored to the individual. It may reduce the amount of information needed, or it may increase it if some of what the patient knows is erroneous. DIF: Cognitive Level: Analysis REF: d. 119 OBJ: Theory #3 TOP: Assessing Learning Needs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse uses a syringe and vial of insulin to show how to draw up the correct dose while she explains the procedure to the patient. To best promote learning, her next step should be to: • give the patient written materials to study and learn the procedure. w w w • • have the patient explain the procedure to the nurse to assess understanding. • give the patient a day to allow him to process and absorb the information. have the patient practice the procedure with the nurse helping. ANS: D Kinesthetic, or hands-on, learning reinforces the visual demonstration. Immediate handling of the materials reduces anxiety. Giving the patient reading materials or asking the patient to explain verbally will not be as effective as the kinesthetic application. DIF: Cognitive Level: Application REF: d. 116 OBJ: Theory #3 TOP: Modes of Learning KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • In teaching an 82-year-old patient to perform a dressing change to be done at home after discharge, the nurse would adjust the teaching session to: • include another person in the instruction because an 82-year-old person will be unable to master the st pr ep .c om • slow the pace and frequently ask questions to assess comprehension. • speed through the details because age and experience will shorten learning time. te • provide written material and diagrams alone. ANS: B The older patient needs to have the pace slowed and have time to ask questions to confirm comprehension. The inclusion of written materials to reinforce teaching is also good, but should not be the only method of instruction. DIF: Cognitive Level: Application REF: d. 118 OBJ: Theory #5 TOP: Factors Affecting Learning KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • An 80-year-old patient is to be taught the process of colostomy irrigation and reattachment of the colostomy bag. The nurses initial assessment prior to instruction should address the patients: • understanding of the process of irrigation. w w w .m yn ur si ng • • familiarity with the irrigation materials. • manual dexterity. • m o .m yn ur si ng te st pr ep .c om t i v a t i o n t o l e a r n . A N S : D The patients motivation to learn a new skill is essential to the success of the instruction. Some patients need to see the advantage of independence to motivate them to learn. Manual dexterity and basic understanding of materials and process are important, but initially the motivation needs to be assessed. DIF: Cognitive Level: Analysis REF: d. 119 OBJ: Clinical Practice #1 TOP: Motivation KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse can assess her patients ability to read and comprehend written instructions by doing which of the following? • Asking the patient, Did you graduate from high school? w w Giving the patient a printed instruction sheet and saying, Some people have difficulty with written i find them helpful. Would these be helpful to you? • w • Asking the patient, Are you able to read? Giving the patient some printed materials and saying, After you have read this, Ill ask you some qu d. ANS: B in them, to see if youve learned it. Graduation from high school does not guarantee reading comprehension. om Actually reading allows the nurse to know if the patient can read as well as comprehend. DIF: Cognitive Level: Application REF: d. 119 OBJ: Theory #3 TOP: Assessing Literacy KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient being assessed for pre-operative learning needs says his mother had the same surgery by the same surgeon 3 years ago. The nurse should design the teaching plan to: • do a brief review of the preoperative teaching, because the patient is already familiar with the proce teach thoroughly as the procedure may have changed. • simply give the patient a written list of preoperative instructions. ep .c • explore with the patient what he knows about the proposed surgery and add or correct where necess ANS: D Assessing a patients experience and knowledge allows the nurse to tailor the teaching to the individual. The nurse should never assume that a patient knows what he is supposed to know and that teaching again what the patient already knows is a waste of time or insults the patients intelligence and experience. Giving a list of preoperative instructions is simply impossible. DIF: Cognitive Level: Analysis REF: d. 119 OBJ: Theory #4 TOP: Assessing Learning Needs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse is aware that the knowledge deficit of a postpartum patient with her first child that can be safely addressed by the community nurse after discharge is: • weaning the child from breast-feeding. .m yn ur si ng te st pr • care of the patients surgical incision. • feeding the baby by breast or bottle. w w • recognizing signs or symptoms of infection. ANS: A Priority teaching needs prior to discharge are those that have to do with physiologic or safety needs. Thus feeding the baby, care of the incision (prevent infection), and recognition of signs that affect safety must be addressed before discharge. Weaning will not occur until much later and can be addressed safely by the home health nurse. DIF: Cognitive Level: Comprehension REF: d. 116 OBJ: Theory #8 TOP: Prioritizing Learning Needs KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease w • • The nurse evaluates the effectiveness of teaching relative to how to use an eye shield after eye surgery is to: • have the patient tell the nurse what he is going to do. • have the patient demonstrate that he can secure the eye shield. • ask the patient if he has any questions related to the use of the shield. call the patient at home in 3 days and ask if he has been wearing the shield. ANS: B A return demonstration and explanation by the patient will evaluate whether the patients learning needs are met. Having the patient describe the process and ask questions might be helpful but does not show that the patient can place the shield correctly (a psychomotor skill). Evaluation of teaching should be done to allow time to revise the teaching plan if the patient is unable to meet the behavioral objectives. Calling after discharge is too late to correct problems. DIF: Cognitive Level: Application REF: d. 120 OBJ: Theory #2 TOP: Evaluation of Learning KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse will choose the best time to continue postoperative teaching regarding wound care and dressings, which would be: • immediately after the patient has been medicated for pain. ng te st pr ep .c om • just before the patient is discharged, so the information is current. • when the patient is comfortable and receptive to the teaching. ur si • the last thing in the evening, after visitors have left, before bedtime. ANS: C A patient who is in pain, sedated from pain medication, or fatigued at the end of the day after visitors leave will not be receptive to teaching. Teaching should begin before discharge to improve learning. DIF: Cognitive Level: Comprehension REF: d. 119 OBJ: Theory #3 TOP: Readiness to Learn KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse plans to teach a 4-year-old about what to expect after his broken arm has been casted by: bringing a doll and casting materials to the room, showing the casting materials and actually casting • explaining the purpose of the cast. w w w .m yn • • telling the child that while he is asleep, the doctor will take off his arm and wrap it up. • breaking up the teaching sessions into two separate 5-minute sessions. being treated as an adult because this approach helps the child to feel grown up. ANS: C Children benefit from teaching that is geared toward their age and level of understanding. Teaching in short sessions, allowing for the childs brief attention span, will enhance teaching. Children are very literal and improbable stories will be believed. DIF: Cognitive Level: Comprehension REF: d. 118 OBJ: Theory #5 TOP: Teaching a Child KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • The best way for a nurse to reinforce learning during a return demonstration by the patient is for the nurse to: give recognition and praise for the parts the patient does well and to assist or teach when the patient • or forgetful. ep .c om • watch quietly until the return demonstration is finished and then list the errors. • instruct the patient to read the written material again when an error is made. st pr • stop the patient each time he makes a mistake and have him start again after the nurse reviews the p ANS: A Praise and walking through the procedure reinforces learning. DIF: Cognitive Level: Application REF: d. 117 OBJ: Theory #3 TOP: Teaching Methods KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient states, I dont think Ill ever be able to give myself an injection. The best reply by the nurse is: • Everyone feels like that at first. Youll get over it. yn ur si ng te • Dont be afraid. Its an easy skill for anyone to learn. • What bothers you most about the idea of giving yourself an injection? w I know just how you feel. I would have trouble giving myself an injection. ANS: C When a patient lacks self-confidence, the nurse needs to explore the patients feelings. DIF: Cognitive Level: Application REF: d. 117 OBJ: Theory #4 TOP: Confidence and Abilities KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse takes into consideration that when using printed material for teaching a 65-year- old Middle-Eastern patient who speaks perfect English, the nurse should: • use teaching material printed in English. w w • .m • • determine if the patient can read English. • engage a translator to read the English material to the patient. • use English material that is printed in bold type on white paper. ANS: B Determine if the patient is literate in English. If not, a translator may be able to rewrite the instructions in the preferred language. Simply reading the English version is not helpful if the .c om patient is to refer to the material after discharge. Bold print will not help a person who does not read English. DIF: Cognitive Level: Application REF: d. 119 OBJ: Theory #3 TOP: Using Printed Materials KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • Because a person may learn best in a particular manner, to improve patient teaching, the nurse should: • ask the patient whether he learns best visually, aurally, or kinesthetically. use a hands-on approach, because it works best for most people. • test the patients reading comprehension before using visual handouts. pr ep • use a combination of the three modes of learning to enhance learning. ANS: D Many people do not know which mode of learning is their dominant one, and most people learn best with a combination of teaching/learning techniques. DIF: Cognitive Level: Knowledge REF: d. 116 OBJ: Theory #3 TOP: Learning Modalities KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • Once a teaching plan is formulated and placed in the nursing care plan for a hospitalized patient: • one nurse will be designated to teach the plan on a priority basis. yn ur si ng te st • behavioral objectives are used to identify expected outcomes. • it is printed and given to the patient as a guide for learning. w it outlines all that will be taught before the patient is discharged. ANS: B Behavioral objectives identify actions that can be measured; thus they serve as evaluation tools of expected outcomes. Many people are involved in a teaching plan, with responsibility designated in the plan. Not all of the teaching plan may be accomplished during the hospital stay. Priorities identify which learning needs are most important to teach before discharge and which can be taught by the community nurse after discharge. DIF: Cognitive Level: Comprehension REF: d. 119 OBJ: Clinical Practice #2 TOP: Behavioral Objectives KEY: Nursing Process Step: N/A MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • In a skilled nursing home, a newly admitted resident becomes terminally ill following a cerebrovascular accident (CVA). To w w • .m • diminish the familys anxiety, the nurse teaches the family members about activities that are being performed to provide care and comfort to their loved one. This teaching is provided in order to: • reduce the likelihood of a lawsuit over the anticipated death. • decrease the familys needs in the expression of their grief. • increase the familys comfort in their affective domain. enable the family to be better prepared for the approaching death. ANS: C Teaching that addresses a persons feelings, beliefs, or values addresses the affective domain. om • te st pr ep .c DIF: Cognitive Level: Comprehension REF: d. 116 OBJ: Theory #3 TOP: Affective Domain KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse designing a teaching plan for a patient admitted to the hospital for treatment of a heart problem after years of treating the ailment at home with herbal remedies and practices common in his cultural group should: • help the patient to see that using herbal remedies has not worked in the past. explain that cultural remedies may conflict with conventional medicine. • help the patient to identify optimum outcomes that can be achieved through education and comprom si ng • ask family members to intervene for the cessation of the use of cultural remedies. ANS: C A persons cultural values must be considered in formulating a nursing care plan. Working with the patient to identify what is of value to the patient can assist the nurse to plan care that meets the patients needs for education. DIF: Cognitive Level: Application REF: d. 117 OBJ: Theory #4 TOP: Cultural Values and Expectations KEY: Nursing Process Step: Planning MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse recognizes the American Indians need for the intervention of a shaman in dealing with illness because the shaman helps the patient in seeking: • a sense of peace and harmony with nature. w w w .m yn ur • • a spiritual route to healing. • healing through the domination over evil. • support from decease d the patient feels ready to be discharged home. • it is anticipated the patient will be discharged in 8 hours. .c • om ancestor s. ANS: B The American Indian has a strong belief that spiritual healing is essential to physical health. DIF: Cognitive Level: Knowledge REF: d. 117 OBJ: Clinical Practice #2 TOP: Cultural Values and Expectations KEY: Nursing Process Step: Planning MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse appropriately begins discharge planning when: • the physician writes orders to discharge the patient. the patient is admitted to the health care facility. ANS: D Discharge planning requires looking ahead in order to meet the patients ongoing needs at home. It is a process that begins at the time of admission. DIF: Cognitive Level: Comprehension REF: d. 119 OBJ: Theory #1 TOP: Discharge Planning KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • A nurse is showing a diabetic patient how to draw insulin out of a syringe. The mode of learning that the nurse is using is learning. auditory • visual • kinesthetic • oral .m yn • ur si ng te st pr ep • w w w ANS: B Visual learning is based on learning through what the learner sees. DIF: Cognitive Level: Comprehension REF: d. 116 OBJ: Theory #3 TOP: Modes of Learning KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse will plan to offer the teaching session in a quiet area in order to: • ensure that the patient can hear what the nurse says. • reduce distractions. • provide absolute privacy. • make the read the listed steps written on a poster board on the wall. • write down the steps as she performs them. ep .c • om environment more like a classroom. ANS: B Teaching sessions are best done in a quiet environment to reduce distractions. DIF: Cognitive Level: Comprehension REF: d. 119 OBJ: Theory #4 TOP: Enhancing Learning KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • When a nurse is talking through a procedure or assisting the patient to learn, the nurse encourages the patient to: • close her eyes and envision the process. verbalize each step until the steps are memorized. ANS: C Writing down the steps as they are performed provides a guide in the patients own words that can be followed independently. DIF: Cognitive Level: Application REF: d. 120 OBJ: Theory #3 TOP: Modes of Learning KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse who is communicating with a school-age child about receiving anesthesia for surgery later this afternoon would best describe the process by saying: • The doctor who will be wearing a mask will put a needle in your arm and then you go to sleep for a • You will just float off to dreamland and after you come back your tonsils will have been cut out. After the doctor puts medicine in your arm, you will ride on a pony to where fairies will take out yo w w w .m yn ur si ng te st pr • c. d. ANS: D will ride right back here. You will be given a ride on a special bed to a big room where the doctor will give you some medici you very sleepy. Children interpret language literally, so avoid idioms or stories that might be frightening because they can be easily misunderstood. Language should be tailored to the childs understanding. DIF: Cognitive Level: Application REF: d. 118 OBJ: Theory #5 TOP: Communication with School-Age Child KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • When teaching an elderly patient about changing his dressing, the nurse would most appropriately: • be certain the patient is wearing his glasses and/or hearing aid. talk through the process rapidly to keep the patient from becoming tired. • wait for the patient to ask any questions about the procedure. om • point out each mistake during the return demonstration. ANS: A Special considerations when teaching the elderly include being certain the patient is wearing glasses and/or a hearing aid that is turned on and adjusted, if needed. Short sentences should be used, and the nurse should speak slowly. Pointing out mistakes without any praise can diminish the confidence of the patient. DIF: Cognitive Level: Application REF: d. 118 OBJ: Theory #5 TOP: Communication with the Elderly KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse would identify an opportunity for a teachable moment in the situation of a patient who: • has just been told of the malignancy of his tumor. ur si ng te st pr ep .c • says, How will I remember all the things about my new diet? • has just returned from surgery for a deviated septum. yn • is packing belongings in preparation for discharge. ANS: B The teachable moment occurs when the patient is at an optimal level of readiness to learn and shows a willingness to apply that information. DIF: Cognitive Level: Application REF: d. 115 OBJ: Theory #4 TOP: Teachable Moment KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort MULTIPLE RESPONSE • Continuous learning needs for the patient upon discharge should be communicated to the: (Select all that apply.) • visiting nurse. w w w .m • • family. • primary care physician. • pharmacy or medical supply facility. • yn ur si ng te st pr ep .c om h o m e h e a l t h a i d e . A N S : A , B , C w w w .m Health care entities that need to be aware of post-discharge continuous learning needs include the visiting home health nurse, the family, and the primary care physician. Pharmacies and medical supply facilities are not notified. The home health aide will not be instructed by the home health nurse. DIF: Cognitive Level: Comprehension REF: d. 115 OBJ: Theory #8 TOP: Continued Teaching After Discharge KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • The nurse reminds the patient that health instruction supports the goals of Healthy People 2020, which include: (Select all that apply.) • promoting healthy behavior. • increasing the life span. • providing equipment for self-care. • ensuring access to adequate health care. strengthening community relationships. ANS: A, D, E Health instruction supports the goals of Healthy People 2020, which include promoting healthy behaviors, protecting health, ensuring access to quality health care, and strengthening community health promotion programs. DIF: Cognitive Level: Knowledge REF: d. 115 OBJ: Theory #2 TOP: Healthy People 2020 KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • The nurse is aware that the major modes of learning are: (Select all that apply.) • oral. • auditory. • kinesthetic. • gustatory. pr tactile. st • ep .c om • prognosis. w • postoperative care. w • .m yn ur si ng te • visual. ANS: C, D, F Kinesthetic, auditory, and visual are the major modes of learning. DIF: Cognitive Level: Knowledge REF: d. 116 OBJ: Theory #3 TOP: Modes of Learning KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • The LPN/LVN is qualified to give patient teaching on information relative to: (Select all that apply.) • disease process. w • • d i s a s t e rehabilitation. yn ur si ng te st pr ep .c om r p r e p a r e d n e s s . A N S : A , B , D , E LPNs and LVNs are qualified to give teaching on topics relative to disease process, postoperative care, rehabilitation, and disaster preparedness. Information on prognosis is not appropriate. w w w .m Chapter 9 Recording and Reporting T e st B a n k M U L T I P L E C H O I C E om The nurse with a patient who complains of severe pain documents every 15 minutes about the steps taken to try to relieve the pain (without success). The nurse also documents the time and content of two calls made to the patients physician requesting that the physician examine the patient for unexpected complications. This documentation by the nurse is likely to: • cause the physician to come to the attention of the hospital administration. be questioned by the nurses supervisor for time inefficiency. • be used against the nurse if a lawsuit results, because it proves the nurse was not able to relieve the .c • ep • justify insurance reimbursement for an extended duration of hospitalization for the patient. ANS: D Documentation of complications or a patients changing condition is used by insurance companies to justify payments for hospitalization. Documentation also serves as evidence of standards of care in a court of law. DIF: Cognitive Level: Application REF: d. 81 OBJ: Theory #4 TOP: Purposes of Documentation KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient who is very angry and is leaving the hospital against medical advice (AMA) demands to have the medical chart to take, because it is her personal property. An appropriate response would be: • Certainly. This hospital doesnt need to keep it if you are leaving and will not be returning here. .m yn ur si ng te st pr • w w • You are entitled to the information in your chart, but the chart is the property of the hospital. I will copy made for you. w • • The information in your chart is confidential, and you cannot leave this facility with it. Because you are leaving against the medical advice of your physician, you may not have the chart. ANS: B The chart is the property of the facility, but the patient has a legal right to the information in it even if she is leaving AMA. DIF: Cognitive Level: Application REF: d. 83 OBJ: Theory #3 TOP: The Medical Record KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A student nurse is assigned to a clinical unit on which one of the patients is a nationally known celebrity. The student reads the chart to find out why the celebrity is being treated. The student who is not the assigned caregiver is: • motivated to learn about the health problem of this patient and is appropriately seeking knowledge experience. doing appropriate research about nursing care as long as information is not divulged. • violating the confidentiality of the patients record. om • .c neglecting the assigned patient load and should read the unassigned patients chart only after his assi ep d. ANS: C st pr completed. w w .m yn ur si ng te A person reading a patients chart who is not involved in the patients care is in violation of confidentiality. Protecting the patients privacy is of prime importance. DIF: Cognitive Level: Comprehension REF: d. 83 OBJ: Theory #3 TOP: The Medical Record KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A patient with a nursing diagnosis of Skin integrity, impaired, related to surgery as evidenced by disruption of skin surface has the following nursing documentation: Incision clean, dry, intact. No pain or tenderness. Instructed to keep area dry, may wear light dressing to protect from clothing. Verbalizes understanding of wound care and ability to manage at home. Wound healing without complication. This documentation is: • an example of charting by exception. evidence of the use of the nursing process. • using the problem-oriented medical record (POMR) format. w • • usually entered on a flow sheet for treatments and vital signs. ANS: B The nursing process is evident in this documentation. Assessment, interventions, and evaluation are all noted. DIF: Cognitive Level: Analysis REF: d. 83 OBJ: Theory #2 TOP: Methods of Charting KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • Which nursing assessment is an example of brevity and clarity while meeting legal guidelines? • 4 cm reddened area over sacrum. Skin intact, warm, and dry. • Taking fluids poorly, but more than yesterday. • Apparently comfortable all night. Offers no complaints of pain. Patient says she is still slightly nauseated, would like to try some toast and tea. ANS: A Provision of specific objective datasize, location, and characteristics of the patients skinis clear and brief and informative. DIF: Cognitive Level: Comprehension REF: d. 92 OBJ: Clinical Practice #2 TOP: The Charting Process KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse enters a notation in a patients chart but then discovers that the notation was made in the wrong chart. The nurse correctly: pr ep .c om • st te • draws a single line through the notation so that it is still readable and writes mistaken entry, his sign and time. si blacks out the note to protect the confidentiality of the patient about whom it was written and writes wrong patient, his signature, and the date and time. ur • removes the page on which the error is written and rewrites the other correct notes. ng • whites out the wrong entry and writes the note in the chart of the correct patient. ANS: A When an error is made, no attempt to hide or obliterate the error should be made, because this may be questioned in a court of law. DIF: Cognitive Level: Application REF: d. 96, Box 7-4 OBJ: Theory #6 TOP: Charting Error Corrections KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A resident in a skilled nursing facility for a short-term rehabilitation following a hip replacement says to the nurse, I dont want to have you draw any more blood for those useless tests. When the nurse fails to convince the patient to have the blood drawn, the most appropriate documentation would be: • Refuses to have blood drawn. Doctor notified. w w w .m yn • • Refuses to have blood drawn; says tests are useless. Doctor notified. • Doctor notified of failure to draw ordered blood work. Blood not drawn because tests are no longer desired by patient. ANS: B When a patient refuses a treatment, the nurse should document the exact words of the patient regarding why the patient is refusing care. DIF: Cognitive Level: Application REF: d. 96, Box 7-4 OBJ: Clinical Practice #2 TOP: What to Document KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A clinic nurse is documenting in a patient chart about the pain that brought the patient to seek medical attention. The best description is: • Abdominal pain, unrelieved by antacids. Had spaghetti, salad, coffee, and ice cream cake for lunch. ep .c om • Severe pain around umbilicus, unable to sleep because of pain. Started approximately 2 hours after • Pain at level of 7 to 8. Nothing has relieved or lessened pain, it just keeps getting worse. te st pr • Peri-umbilical sharp pain at pain level of 7 to 8 for last 3 hours, started 2 hours after lunch. No relie ANS: D When charting a sign or symptom, the nurse should include the quality (level 7 to 8), chronology (after lunch, last 3 hours), and aggravating or alleviating factors, as well as associated symptoms. DIF: Cognitive Level: Application REF: d. 95, Box 7-2 OBJ: Clinical Practice #2 TOP: The Charting Process KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort w In a chart for a patient who has had an allergic reaction to a drug and an associated nursing diagnosis of Skin integrity, impaired, related to allergic reaction as evidenced by rash and hives, the nurse charts Subjective: denies itching. Happy with improvement in skin. Objective: rash fading on face, chest, and back; no hives visible on skin. Skin warm, dry, and intact. Assessment: skin integrity improving. Plan: check rash daily until discharge. This type of charting is an example of: • charting by exception. w • w .m yn ur si ng • • narrative style. • a problem-oriented medical record (POMR). the case man age ment syste m. ANS :C The POMR focuses on a patient problem or nursing diagnosis and typically uses the SOAP (subjective, objective, assessment, plan) format as shown here. DIF: Cognitive Level: Application REF: d. 83 OBJ: Theory #4 TOP: Methods of Charting KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • In an agency that uses specific protocols (Standard Procedures) and charting by exception, an advantage compared with using traditional (narrative or problem-oriented) charting is that charting by exception: • is well suited to defending nursing actions in court. te st pr ep .c om • contains important data certain to be noted in the narrative sections. • allows staff to learn the system quickly and easily. ng • highlights abnormal data and patient trends. ANS: D Charting by exception enables staff to see notation of changes in a patients condition at a glance. DIF: Cognitive Level: Comprehension REF: d. 83 OBJ: Theory #4 TOP: Methods of Charting KEY: Nursing Process Step: N/ A MSC: NCLEX: N/A • If an agency is using computer-assisted charting, the nurse is responsible for: • learning the passwords of the staff nurses and physicians so that they can communicate with one an • guarding the confidentiality of the patient record by not leaving the patient screen on if he leaves th teaching the patient to input information about herself, such as intake and output or symptoms the p • experience. w w w .m yn ur si • • choosing whether he will use the computer to help in charting or continue to use traditional paper d ANS: B Confidentiality of computer records is as important as that of the paper chart. Nurses must also be protective of their user passwords. DIF: Cognitive Level: Comprehension REF: d. 90, Box 7-1 OBJ: Theory #4 TOP: Methods of Charting KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care om A nurse begins the shift caring for a patient who has just returned from the recovery room after surgery. It is most important to document: • at the end of the shift so that the nurse can give his full attention and time to the patients needs duri a nursing care plan in the chart before assessing the patient so that the nurse can identify priorities. • at least three times during the shift: at the beginning, in the middle, at the end, and as needed. .c • ep • an initial assessment of the patient and a plan based on the needs of the patient as assessed at the be ANS: D An initial assessment should be performed at the beginning of the shift and promptly documented. It will determine the plan and priorities. Charting should be done as close to the time of occurrence as possible. DIF: Cognitive Level: Application REF: d. 96, Box 7-4 OBJ: Theory #1 TOP: The Charting Process KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse uses the flow sheet in patient care documentation primarily: • to track routine assessments, treatments, and frequently given care. yn ur si ng te st pr • to eliminate written narratives and to save time. • in computer-assisted charting to create visual graphs showing change. w to improve continuity of care and exchange of information among disciplines. ANS: A Flow sheets are a time saver but do not eliminate narrative charting. They are used to document information that is routine and that would be lost in a narrative note. DIF: Cognitive Level: Comprehension REF: d. 83 OBJ: Theory #4 TOP: Flow Sheets KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • In a skilled nursing facility, if all of the following are available, the best way for the new nurse to obtain current information about the needs and abilities of his patients would be to use the: w w • .m • • physicians order sheets. • nurses admission history and physical. • nursing Kardex. • w w w .m yn ur si ng te st pr ep .c om m o s t r e c e n t n u r s e s n o t e s . A N S : C A nursing Kardex is a 1-page summary of the patients diagnosis and current orders, treatments, and care needs. DIF: Cognitive Level: Knowledge REF: d. 93 OBJ: Clinical Practice #2 TOP: Nursing Kardex KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: coordinated care • When the nurse charts in narrative or source-oriented format about the patients condition and the nursing care provided, it is appropriate for him to record: • Patient will go to physical therapy after lunch. • Diabetes in excellent control. Continue with current insulin schedule. • I gave the patient a thorough bath and cut her fingernails. To x-ray by wheelchair @ 10:30 AM IV infusing in left arm. ANS: D Documentation that includes specific information regarding time, method of travel, destination, and current status (that an IV medication is infusing) is a clear example of source-oriented charting. DIF: Cognitive Level: Application REF: d. 83 OBJ: Theory #4 TOP: Source Oriented Charting KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care • The nurse understands that a face sheet contains information pertaining to: • serial measurements and observations, such as temperature, pulse, respiration, blood pressure, and om • plan of care for the patient, including nursing diagnoses, goals/expected outcomes, and nursing inte • written report of the nursing process, record of interventions implemented, and the patients respons pr ep .c • patient data, including patients name, address, phone number, insurance company, and admitting di ANS: D The type of information contained on a face sheet includes patient data, including the patients name, address, phone number, next of kin, hospital identification number, religious preference, place of employment, insurance company, occupation, name of admitting physician, and admitting diagnosis. DIF: Cognitive Level: Comprehension REF: d. 82, Table 7-1 OBJ: Theory #4 TOP: Documentation Forms KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: coordinated care • A nurse understands that the physicians directives for patient care are also referred to as the: • history and physical. progress notes. • f a c e s h e e t w w • physicians orders. w • .m yn ur si ng te st • st pr ep .c om . A N S : B The physicians directives for patient care are the same as the physicians orders. DIF: Cognitive Level: Knowledge REF: d. 82, Table 7-1 OBJ: Clinical Practice #4 TOP: The Medical Record KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A nurse tells her neighbor personal information about a hospitalized patient. Telling her neighbor about this indicates that the: nurse is actively promoting nursing as a profession, and it is important to share information that mi • to pursue a nursing career. • nurse has violated the confidentiality of the patient by discussing personal information about the pa neighbor. ur si ng te • actions of the nurse are appropriate since his neighbor is his confidante, and the neighbor has assure information provided will not be shared. .m yn nurse has not violated the confidentiality of the patient because the patient is terminal; sharing this i w ANS: C d. w harm the patient. w As a legal record, the contents of the chart must be kept confidential and can be given out only with the patients written consent because it contains personal information regarding the patient. Only those health professionals caring directly for the patient, or those involved in research or teaching, should have access to the chart. Protecting the privacy of the patient is of prime importance. Patient information is not discussed with others who are not directly involved in the patients care. DIF: Cognitive Level: Application REF: d. 83 OBJ: Theory #3 TOP: Patient Confidentiality KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The Quality and Safety Education for Nurses (QSEN) project has identified the most important pre-licensing skills for nurses as: • effective communication. • informatics. • familiarity with medical terms. • w w w .m yn ur si ng te st pr ep .c om w ri ti n g n ur si n g c ar e pl a ns . A N S: B The Quality and Safety Education for Nurses (QSEN) project has identified informatics as an important pre-licensing skill. DIF: Cognitive Level: Knowledge REF: d. 87 OBJ: Theory #4 TOP: Informatics KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • Advantages of source-oriented or narrative charting include all of the following except that it: • encourages documentation of normal and abnormal findings. • gives information on the patients condition and care in chronological order. • indicates the patients baseline condition for each shift. • includes aspects of all steps of the nursing process. ANS: A A disadvantage of source-oriented, or narrative, charting is that it encourages documentation of both normal and abnormal findings, making it difficult to separate pertinent from irrelevant information. DIF: Cognitive Level: Comprehension REF: pp. 83-84 OBJ: Theory #4 TOP: The Charting Process KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • Which examples of documentation would be most informative to transcribe to the patients medical record? • Patient consumed two slices of bread and a cup of coffee at breakfast. • Patient does not appear to be hungry after consuming breakfast. • Patient ate a small amount of bread and drank a little coffee for breakfast. Patient ate well for breakfast, lunch, and dinner and seems content. ANS: A Use of the words appears to or seems in phrases such as appears to be resting should be avoided. Chart the behavior; the patient either is or is not resting. Words that have ambiguous meanings and slang should not be used in charting. For example, how much is a little, a small amount, or a large amount? What do phrases such as ate well and taking fluids poorly mean? Although such words give a general idea of what is meant, they are not specific. DIF: Cognitive Level: Application REF: d. 92 OBJ: Theory #4 TOP: Source Oriented Charting KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care COMPLETION • Charting that follows the nursing process and uses nursing diagnoses while placing the plan of care within the nurses _ charting. progress notes is ANS: PIE problem identification, intervention, and evaluation The nurse needs to be able to define PIE charting. DIF: Cognitive Level: Knowledge REF: d. 86 OBJ: Theory #2 TOP: Documentation KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care • Health care professionals assigned to a patient require access to the chart to review information and to document care given. All . The contents of the chart contents of the chart must be kept should not be discussed with persons who are not involved in the care of the patient. ANS: confidential The nurse needs to be able to identify what confidentiality entails. DIF: Cognitive Level: Knowledge REF: d. 83 OBJ: Theory #3 TOP: Confidentiality KEY: Nursing w w w .m yn ur si ng te st pr ep .c om • om st pr ep .c Process Step: N/A MSC: NCLEX: N/A • The nurse explains that should a patient return to the hospital for years, the medical chart can be retrieved treatment within from medical records for review. ANS: 10 ten Medical records are kept in the health information department of a hospital for a period of 10 years. DIF: Cognitive Level: Knowledge REF: d. 83 OBJ: Theory #3 TOP: Storage of Medical Records KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care , an • When using a case management system of charting a(n) unexpected event in the patients condition is documented on the back of the pathway sheets. ANS: variance .m yn ur si ng te A variance is an unexpected event in the patients course of care. An example would be a healing wound that was complicated by an infection. DIF: Cognitive Level: Knowledge REF: d. 83, Figure 7-10 OBJ: Theory #4 TOP: Variances KEY: Nursing Process Step: N/A MSC: NCLEX: N/A MULTIPLE RESPONSE • Advantages of the problem-oriented medical record (POMR) are that this method of charting: (Select all that apply.) • promotes the problem-solving approach. formats charting into chronological order. • makes tracking trends in patient care easy. allows for easy auditing of patient records to evaluate staff performance. w • w • reinforces application of the nursing process. ANS: A, D, E POMR promotes problem solving with the reinforcement of the nursing process. This method allows for easy auditing of patient records. DIF: Cognitive Level: Comprehension REF: d. 85 OBJ: Theory #4 TOP: Problem Oriented Charting KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The method of computer-assisted charting: (Select all that apply.) w • • improves communication between departments. • is less costly to educate personnel to the method. • speeds reimbursement for services. • allows electronic records to be retrieved more quickly. allows entries to be made at point of care. ANS: A, C, D, E Computerized charting improves communication between departments, speeds reimbursement for services and retrieval of records, and allows entries to be made quickly at the point of care. It is more expensive to educate personnel in the use of computers than in other forms of documentation. DIF: Cognitive Level: Knowledge REF: pp. 89-90 OBJ: Theory #4 TOP: Documentation K E Y: N u r s i n g P r o c e s s S t e p : Implementation MSC: NCLEX: N/A • Helpful cultural information the nurse should include on the admission note is: (Select all that apply.) • primary language spoken. te st pr ep .c om • number of children in the immediate household. • beliefs about causality of illness. • level of English literacy. • dietary concerns. ur si ng • w w .m yn ANS: A, C, D, E Information relative to primary language, beliefs about cause of illness, level of English literacy, and dietary concerns are helpful items to include on the admission note. DIF: Cognitive Level: Comprehension REF: d. 91 OBJ: Theory #1 w Chapter 10 M U L T I P L E C H O Asepsis I C E • When a patient in the ambulatory clinic is diagnosed as having pneumococcal pneumonia, the nurse is aware that this infection is: • viral and will not respond to antibiotics. • bacterial and should respond to treatment with antibiotics. • fungal and is caused by the alteration of the normal flora of the lung. resultant from a resistant organism and extreme caution must be taken. ANS: B The coccal suffix indicates a bacterial infection with round cocci, which are bacteria that usually respond to antibiotic therapy. DIF: Cognitive Level: Comprehension REF: k 209 OBJ: Theory #1 TOP: Infectious Agents KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse explains to the patient who has pneumococcal pneumonia that the lungs serve as the: • mode of transfer. transmission of the disease. • reservoir. si • ng • te st pr ep .c om • w w w .m yn ur organism s that cause the infection. ANS: C The reservoir is the place where the organism is found, such as a wound or, in this case, the infected lungs. Droplets are modes of transmission from the reservoir. DIF: Cognitive Level: Comprehension REF: k 212 OBJ: Theory #2 TOP: Process of Infection KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: physiological adaptation • The patient inquires about how his body will kill pathogens unassisted by antibiotics. The nurse responds that a process called phagocytosis will: • stimulate the body to make more white blood cells. • create antibodies against the pathogen. • engulf and destroy the pathogen. • stimulate the production of om interferons. ANS: C Phagocytes that are stored in the GI tract, liver, and spleen kill pathogens by engulfing and destroying the invaders and cleaning up the debris. DIF: Cognitive Level: Comprehension REF: k 208 OBJ: Theory #5 TOP: Body Defenses KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse explains that the immunizations against hepatitis B will: • stimulate the body to make antibodies the hepatitis B antigen. offer immediate protection from hepatitis B by the injection of ready-made antibodies. • introduce live antigens into the body that will stimulate the production of antibodies. ep .c • offer protection against hepatitis A, C, and D, in addition to hepatitis B. ANS: A Artificially acquired immunization is achieved by introducing killed or attenuated pathogens that are recognized as antigens by the immune system but that are not able to cause disease. These antigens stimulate the formation of antibodies specific to hepatitis B only. DIF: Cognitive Level: Comprehension REF: k 218 OBJ: Theory #5 TOP: Immune Response KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • A mother and her 2-week-old infant, who is breast-fed, have been exposed to chickenpox. Although the mother had chickenpox as a child, she is concerned about her baby. The nurse explains: • the infant is at risk because the baby has not been immunized against the disease. both infant and mother are at risk because the mothers immunity was acquired too long ago to be ef w w • w .m yn ur si ng te st pr • • the baby should receive immune globulin to protect him from the infection. neither are at risk, because the mother has naturally acquired immunity, and she passes antibodies t d. ANS: D the breast milk. Having had a disease such as chickenpox provides lifelong naturally • 1 minute. .c 15 seconds. ep • om acquired immunity, which allows the mother to pass on antibodies through the placenta and breast milk to protect the infant until his immune system is more mature. DIF: Cognitive Level: Analysis REF: k 218 OBJ: Theory #4 TOP: Immune Response KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • Health personnel should wash their hands with soap and water at the beginning of the shift for: • 10 seconds. • w w w .m yn ur si ng te st pr 2 m i n u t e s . A N S : B Hand hygiene as suggested by the CDC should be done at the beginning of the shift for 15 seconds (30 seconds or longer in specialty areas). DIF: Cognitive Level: Knowledge REF: k 221 OBJ: Clinical Practice #2 TOP: Asepsis KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • An organism that is included in the extended-spectrum betalactamase producing pneumonia (ESBL) group is: • Staphylococcus aureus. ANS: D • Clostridium difficile. • Enterococcus. • Escherichia coli. • is confined to the patients room. • uses sterile attire to protect the patient. om E. coli and Klebsiella pneumoniae are the organisms in the ESBL group. DIF: Cognitive Level: Knowledge REF: k 209 OBJ: Theory #1 TOP: Resistant Organisms KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The nurse explains that medical asepsis differs from surgical asepsis in that medical asepsis: • kills all organisms. uses sterile equipment before contact with the patient. ANS: B Medical asepsis confines the microorganisms to the patients room. Medical asepsis does not kill all organisms; it uses clean attire and equipment. DIF: Cognitive Level: Comprehension REF: k 218 OBJ: Theory #7 TOP: Medical Asepsis KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • When the nurse performs a procedure using sterile technique in the patients unit, it means that: • the equipment and supplies used are disposable and clean. ng te st pr ep .c • all organisms have been killed or removed from materials that come in contact with the patient. • the nurse will do a 10-minute surgical scrub before beginning the procedure. yn ur si • the nurse will be required to don a sterile gown, mask, and eye shields. ANS: B Surgical asepsis or sterile technique uses sterilization to remove all organisms, not just pathogens. The purpose is to protect the patient from the introduction of organisms that could endanger health. Although sterile gloves are used, there is no need for a sterile gown. DIF: Cognitive Level: Comprehension REF: k 218 OBJ: Theory #7 TOP: Asepsis KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A nurse teaching family members about hand hygiene in the home would emphasize: • keeping fingernails short and avoiding wearing rings. w w w .m • • washing hands up to the elbows for 2 minutes the first time in the day, and for 1 minute after a diap • using disposable gloves after hand hygiene when feeding the infant. that home care requires less attention to medical asepsis, so hand hygiene is necessary only after toi d. ANS: A .c Fingernails and jewelry provide hiding places for organisms and can scratch the baby. A 10- to 20-second hand hygiene routine is appropriate before handling the baby and after changing diapers (as well as after toileting, before eating, and anytime they are soiled). DIF: Cognitive Level: Application REF: k 219 OBJ: Clinical Practice #2 TOP: Medical Asepsis KEY: Nursing Process Step: Implementation om soiled diapers. st pr ep MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A nurse is using personal protective equipment (PPE) before entering the room of a patient with diarrhea and vomiting who is being treated for an intestinal infection. The nurse most likely needs to use which combination of PPE? • Gown, gloves, and mask Gown, gloves, and goggles (or glasses) • Shoe covers, gown, and gloves w w ng w .m yn ur si • R e u s a b l e g o w n a n d m a s k A N S te • .c om : B The gown is necessary to protect the nurses uniform from becoming contaminated with organisms from stool or vomitus, gloves protect hands from contact with these body secretions, and goggles prevent splashing of contaminated material into the eyes. Protective gowns are not reused. DIF: Cognitive Level: Application REF: k 228, Skill 16-2 OBJ: Clinical Practice #3 TOP: Standard Precautions KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • When removing a used face mask, the nurse correctly: • lowers it below his chin to use the next time he enters that patients room. removes the mask first before removing any other PPE. • unties the bottom ties first, then the top, and disposes of the mask without touching it. pr ep • discards the mask only if it is wet; otherwise, he folds and stores it to reuse the next time. ANS: C Face masks are not reused, and they should not be worn dangling around the neck. Gloves should be removed first (and eyewear, if worn) before removing the mask so as not to contaminate the nurses hair or face. DIF: Cognitive Level: Comprehension REF: k 228, Skill 16-2 OBJ: Clinical Practice #3 TOP: Standard Precautions KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse uses the Standard Precautions, as outlined by the Centers for Disease Control and Prevention (CDC), when: • there is a suspicion of or risk of infection. .m yn ur si ng te st • caring for patients who have wounds draining body fluids. w • preventing transmission of respiratory and wound infections. w • w • c a r i n g f o r a ng te st pr ep .c om l l p a t i e n t s . A N S : D Standard Precautions include hand hygiene and use of PPE when there is exposure to blood, body fluids, mucous membranes, nonintact skin, secretions, excretions, and contaminated articles. Hand hygiene is part of patient care for all patients all the time, regardless of diagnosis, and the selection of PPE is appropriate for all patients at some time or another. DIF: Cognitive Level: Application REF: k 224, Box 16-3 w w w .m yn ur si OBJ: Clinical Practice #3 TOP: Standard Precautions KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • When the nurse is using a syringe and needle to give a patient an injection, he or she should: • never recap the needle afterwards to avoid risk of needle stick. • carefully break the needle from the syringe, using the needle cover to prevent reuse of a used syring throw the needle and syringe immediately in a covered garbage can with a red plastic liner to indica c. d. ANS: A biohazards. recap the needle and place it carefully on the patients table until leaving the room, then discard it in in the nurses medication room. Used needles and sharps need to be handled very carefully to prevent sticks with contaminated body fluids (blood). Never recapping the diminish possibility of latex allergy. • keep skin of hands from cracking and drying. pr • ep .c om needle is an approved CDC Standard Precaution. The other choices are contraindicated. Sharps should be discarded in a specially marked container that does not endanger the person who empties it. The needle should not be broken or recapped unless it is done with a one hand scoop method. Throwing needles or sharps in a red plastic bag endangers others. DIF: Cognitive Level: Application REF: k 229 OBJ: Clinical Practice #3 TOP: Standard Precautions KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse using protective non-sterile gloves in the provision of patient care will wash his or her hands after removal of the gloves in order to: • avoid transfer of organisms. enhance the ease of donning a fresh pair of gloves. ANS: A Washing the hands immediately after removing barrier gloves decreases the likelihood that organisms will gain access to the skin through small holes or imperfections in the gloves and reduces the transfer of microorganisms to the environment and other persons. DIF: Cognitive Level: Comprehension REF: k 218, Box 16-3 OBJ: Clinical Practice #2 TOP: Standard Precautions KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse encourages the 84-year-old patient who is recovering from a hip replacement to: • cough frequently to make up for the loss of cilia. restrict fluid to prevent pulmonary congestion. w • w .m yn ur si ng te st • w • • e n c o u r a keep the bed flat to aid in lung expansion. pr ep .c om g e b e d r e s t . A N S : A Because of the loss of an adequate cough mechanism and loss of cilia, the mature adult should be encouraged to cough frequently. .m yn ur si ng te st DIF: Cognitive Level: Application REF: k 21, Table 16-6 OBJ: Theory #3 TOP: Prevention of Infection in the Elderly KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient is sent home with an open wound that is still infected and being treated with wet- to-dry dressing changes four times a day. Before discharge, in order to prevent infecting other family members, the nurse would teach the patient to: • be the only person to perform the dressing changes, thus eliminating the risk of infection to other fa wash hands thoroughly before the dressing change. • use gowns, gloves, and masks for any family contact with him. maintain medical asepsis and proper handling of the contaminated dressings. ANS: D Medical asepsis is the most important way of preventing the spread of infection in the home or in the hospital or nursing home. DIF: Cognitive Level: Application REF: k 224, Box 16-3 OBJ: Clinical Practice #4 TOP: Asepsis in the Home Environment KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse instructing a patient in the home use of disinfectant would include the information that the disinfectant can be used to: • decrease organisms on the patients body but take care not to use it around the patients eyes or in the w w • w • • sterilize instruments with a bacteriostatic disinfectant. • thoroughly clean and rinse all soap off the equipment before disinfecting it. first remove all organic matter prior to disinfecting. ANS: C Disinfectants are irritating to the skin. Bacteriostatic disinfectants only weaken or slow the growth of organisms; they do not kill them. Hot water hardens organic matter; therefore equipment should be rinsed with cold water before hot soapy water is used. DIF: Cognitive Level: Comprehension REF: k 230 OBJ: Theory #6 TOP: Disinfection KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse is aware that the use of ethylene oxide gas is reserved for the sterilization of: • dressings. • heat-sensitive items. pr surgical instruments. st • ep .c om • te • w w w .m yn ur si ng f l o o r s a n d w a l l s . A N S : C Ethylene oxide is used to sterilize heat-sensitive items and offers good penetration. DIF: Cognitive Level: Knowledge REF: k 230 OBJ: Theory #8 TOP: Cleaning and Disinfection KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse recommends a good agent for disinfecting contaminated areas in the home is: • to cover the area with boiling water and let air dry. • a 1:10 solution of chlorine bleach. • a 1:2 solution of alcohol. applying a dressing on the leg. • changing a babys diaper. pr • ep .c to soak in a solution of povidone-iodine for 30 minutes and rinse with hot water. ANS: B A 1:10 solution of chlorine bleach is a good home disinfectant. DIF: Cognitive Level: Comprehension REF: k 230 OBJ: Theory #8 TOP: Asepsis in the Home Environment KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The situation in which protective eyewear is required is: • suctioning a tracheotomy. om • gathering the linens off a contaminated bed. ANS: A Suctioning a tracheotomy causes the patient to cough and spray mucus. Protective eyewear is used when there is danger of splashing blood or body fluids, such as in the operating room. It is not necessary in the other situations. DIF: Cognitive Level: Application REF: k 226, Skill 16-2 OBJ: Clinical Practice #3 TOP: Standard Precautions KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • To prevent a urinary infection in an elderly patient who is in traction for a broken femur, the nurse would: • request a Foley catheter to be inserted. w w .m yn ur si ng te st • encourage fluid intake to keep urine dilute. • encourage intake of apple juice to keep urine acidic. w • • off er a uri nal ev ery 2 pr ep .c om ho urs . A NS :B Encouraging fluid intake to keep urine dilute would be the best way to prevent a urinary infection because concentrated urine is a good medium for pathogens. DIF: Cognitive Level: Application REF: k 215, Table 16-6 OBJ: Theory #3 TOP: Urine Infections in the Elderly KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • Fecal matter has contaminated the patients bed sheet. The nurse should: • place a folded clean, dry sheet or plastic-backed protector over the soiled sheet until it dries and the te st don non-sterile gloves and gown, remove the soiled sheet, replace it with a clean one, and then disp • plastic bag to prevent skin or clothing contact. ng si • remove the soiled sheet without exposure of skin or clothing to the sheet and rinse it in the patients dilute or remove as much feces as possible. use PPE to remove the sheet and place it in a pillowcase on the floor; then replace it with a clean sh ANS: B When handling, transporting, or processing linens contaminated with blood or body fluids, prevention of contact with skin, mucous membranes, and clothing or transfer of organisms to the environment is most important. The sheets should not be rinsed in the patients room, nor should they ever be placed on the floor (clean or soiled). DIF: Cognitive Level: Application REF: k 224, Box 16-3 OBJ: Clinical Practice #3 TOP: Standard Precautions KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse explains that the bodys normal flora serve as: • aids to digestion and blood production. w w w .m yn ur • • prevention to the colonizing of pathogens. • managers of fluid balance of the body. • ep .c om c e l l r e b u i l d e r s . yn ur si ng te st pr ANS :B Normal flora of the body prevent harmful microorganisms from colonizing and multiplying. DIF: Cognitive Level: Comprehension REF: k 208 OBJ: Clinical Practice #3 TOP: Prevention of Infection KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • A patient has been diagnosed with Creutzfeldt-Jakob disease (mad cow disease). The nurse recognizes this disease is caused by a: • prion. virus. • protozoa. • fungus. w .m • w w ANS: A Prions are protein particles that lack nucleic acids and are not inactivated by usual procedures for destroying viruses. They do not trigger an immune response but instead cause degenerative neurologic disease such as variant Creutzfeldt-Jakob disease (mad cow disease). DIF: Cognitive Level: Knowledge REF: k 209 OBJ: Theory #1 TOP: Disease KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: physiological adaptation • A patient has been diagnosed with Rocky Mountain spotted fever. The nurse recognizes this disease is caused by a tick bite that infected the patient with: Rickettsia rickettsii. • Rickettsia prowazekii. • Coxiella burnetii. • Aspergillus. • pinworms. pr tape worms. st • ep .c ANS: A Rickettsia rickettsii is the rickettsia responsible for Rocky Mountain spotted fever. DIF: Cognitive Level: Knowledge REF: k 211 OBJ: Theory #1 TOP: Disease KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse is aware that family education is necessary for the control of the most common helminth infection, which is: • hook worms. om • te • w .m yn ur si ng r o u n d w o r m s . w w AN S: C Pinworms are the most common helminth infection, usually seen in children. Families must be educated about the control of these parasites. DIF: Cognitive Level: Knowledge REF: k 210 OBJ: Theory #1 TOP: Helminth Infection KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A patient has been diagnosed with vaginal candidiasis. The nurse recognizes that this condition is usually the result of: • unprotected sex. • poor personal hygiene. • long-term antimicrobial therapy. • w w w .m yn ur si ng te st pr ep .c om u s i n g b a t h o i l s . A N S : C Long-term microbial therapy can alter the vaginal flora and cause fungal infections such as vaginal candidiasis. DIF: Cognitive Level: Knowledge REF: k 210 OBJ: Theory #1 TOP: Candidiasis KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • A young patient became ill with mononucleosis that she contracted from drinking out of the same glass as her boyfriend who also had the disease. The glass, an inanimate object, has caused the indirect transmission. The inanimate transmitter is called: • fomite. • i n • prions. • vector. moistened towelette. • handkerchief. • clean paper tissue. om yn ur si • ng te st pr ep .c t e r f e r o n . A N S : A A fomite is an inanimate object that can transmit pathogens indirectly. DIF: Cognitive Level: Comprehension REF: k 212 OBJ: Theory #2 TOP: Disease KEY: Nursing Process Step: N/A MSC: NCLEX: N/ A • The nurse instructs a patient that in order to reduce diseases that are transmitted via droplet, the nose and mouth should be covered by: w w w b e n t e l b o w . .m • A N S: D Covering the mouth with a bent elbow prevents the respirator droplets from contaminating the hands. DIF: Cognitive Level: Comprehension REF: k 212 OBJ: Theory #2 TOP: Prevention of Disease KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse is aware that the first barrier to pathogen invasion is the: • skin. • immunizations. • good hygiene. om • w w w .m yn ur si ng te st pr ep .c i m m u n e r e s p o n s e . A N S : A Skin is the first barrier to pathogen invasion. DIF: Cognitive Level: Knowledge REF: k 213 OBJ: Theory #4 TOP: Prevention of Disease KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: physiological adaptation • An enzyme found in the mucous membranes that is bactericidal is: • lysozyme. • • ptyalin. • serotonin. • chlorhexidine. .m w w w a n a n t i s e p t i c . A N S yn • si alcohol wipes. ur • ng te st pr ep .c om h i s t a m i n e . A N S : A Lysozyme is an enzyme found in the mucous membranes, tears, and saliva, which is bactericidal and helps with disease prevention. DIF: Cognitive Level: Knowledge REF: pp. 213-214 OBJ: Theory #2 TOP: Prevention of Disease KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A nurse is caring for a patient who was exposed to Bacillus anthracis. The nurse should wash her hands with: • soap and water. : A .c om If exposure to Bacillus anthracis is suspected or proven, hands must be washed with soap and water. The physical action of washing and rinsing hands is recommended because alcohols, chlorhexidine products, iodophors, and other antiseptic agents have poor activity against spores. DIF: Cognitive Level: Application REF: k 226, Box 16-2 OBJ: Theory #6 TOP: Hand Washing KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • After reading a differential blood count on a patient, the nurse assesses that the patients infection is viral because the: • monocyte count is increased. number of basophils is greatly elevated. • monocyte and neutrophil counts are decreased. pr ep • neutrophil count is decreased and the monocyte and the lymphocyte counts are both elevated. ANS: D A viral infection will show a decreased neutrophil count with an elevation of monocytes and lymphocytes. DIF: Cognitive Level: Analysis REF: k 216 OBJ: Theory #4 TOP: Viral Infection KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation COMPLETION • Fleas, ticks, mosquitoes, and other insects that harbor infection . ANS: are called vectors Fleas, ticks, mosquitoes, and other insects that harbor infection and transmit disease through bites are called vectors. DIF: Cognitive Level: Knowledge REF: k 212 OBJ: Theory #2 TOP: Infection Control KEY: Nursing Process Step: N/ A MSC: NCLEX: N/A • The elderly should receive influenza immunization every . ANS: year Influenza immunizations are recommended to be taken every year by the elderly, health care workers, infants over the age of 6 months, and persons with chronic illnesses. DIF: Cognitive Level: Comprehension REF: k 215, Table 16-6 OBJ: Theory #3 | Theory #8 TOP: Influenza Immunization KEY: Nursing Process Step: N/A MSC: NCLEX: N/A w w w .m yn ur si ng te st • The nurse is aware that gram-negative bacteria are capable of . causing hemorrhagic shock by the production of a(n) ANS: endotoxin Gram-negative bacteria are more dangerous than gram-positive bacteria because they produce an endotoxin that can cause hemorrhagic shock. DIF: Cognitive Level: Comprehension REF: k 209 OBJ: Theory #1 TOP: Gram-Negative Bacteria KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: physiological adaptation om • • effective inoculations. • improved hygiene. pr isolation techniques. st • ep .c MULTIPLE RESPONSE • Portal of exit transmission can be controlled by: (Select all that apply.) • treating infected patients. ng si ur yn .m w w w b a r r i e r p r e c a u t i o n s . A N S : A te • ur si ng te st pr ep .c Chapter 11 Admission, Discharge, Transfer, and Referrals M U L T I P L E C H O I C E • The nurse is aware that patients who are admitted to the hospital as a routine admission under a managed care plan must: • have Medicare. om , B , E Portal of exit transmission can be controlled by identifying and treating infected patients, isolation techniques, barrier precautions, and proper handling of secretions, urine, feces, and exudates. be pre-approved. • be able to pay the deductible. yn • be admitted several days prior to the procedure. ANS: B Managed care insurance programs require that all routine admissions be pre-approved. Often the patient is required to come to the hospital several days prior to the admission to complete paperwork or lab procedures. DIF: Cognitive Level: Comprehension REF: d. 392 OBJ: Theory #1 TOP: Managed Care KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: coordinated care • A patient is scheduled to have a diagnostic procedure performed on an outpatient basis at 9:00 AM. The nurse will advise the patient to: • arrive 2 hours before the scheduled procedure. w w w .m • • wear comfortable clothing. • read printed materials about the procedure. be prepared to pay at least 10% of the predicted cost of the hospitalization. ANS: A Patients are usually required to arrive 1 to 2 hours before a scheduled procedure to complete the necessary paperwork. The patient may be requested to pay a co pay or a deductible, but there is no set amount. DIF: Cognitive Level: Comprehension REF: d. 392 OBJ: Theory #1 TOP: Outpatient Admission KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care • If there is a prior authorization for hospitalization required for a routine admission, the nurse explains that the notification to the insurance company is the responsibility of the: • patient. ep .c om • admissions department of the health facility. • patient, physician, and the admissions department. • office of the admittin g physicia n. ANS: D ur si ng te st pr • w w w .m yn The office of the admitting physician is the usual agent to get prior approval for a hospitalization. The admissions department confirms that all pre-admission requirements are met. DIF: Cognitive Level: Knowledge REF: d. 392 OBJ: Theory #1 TOP: Admission Procedures KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care • The nurse orienting a new patient to the unit would include: • expected cost of the room per day. • location of call bell and how to use it. • calling the patient by their first name for less formality. • ti m e s o f .m yn ur si ng te st pr ep .c om t h e s h if t c h a n g e s. A N S : B Newly admitted patients should be treated with respect without familiarity. The physical arrangement of the room and bath, how to work all controls, such as the call bell, and the names of the nurses who will be giving care should be included in the orientation. DIF: Cognitive Level: Comprehension REF: d. 392 OBJ: Clinical Practice #1 TOP: Admission KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A patient admitted to the hospital through the emergency department has jewelry and a large amount of money. The most efficient intervention about these valuables would be: • send them home with a family member. put them away quickly in the patients closet. • lock them in the narcotics cabinet on the nursing unit. place them in a valuables envelope and have them locked in the agency safe. ANS: A Valuables such as credit cards, money, or jewelry should be sent home with a family member. DIF: Cognitive Level: Application REF: d. 393 OBJ: Clinical Practice #1 TOP: Admission KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • While admitting a patient from home to the skilled nursing facility, the nurse notes that the patient has brought medications that are not included on the physicians medication order sheet. The nurses best initial action is to: • send the medications home with a family member. w w • w • • seal the medications in an envelope and lock it in the medicine cart. • administer the medications with the ordered medications. notify the physician about the medications the patient has been taking. ANS: D It is important to notify the physician of any medications the patient has been taking at home that are not included in the present orders. DIF: Cognitive Level: Application REF: d. 393 OBJ: Clinical Practice #1 TOP: Admission KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control New orders have been written by the attending physician for a patient admitted to a skilled nursing facility. After transcription, the orders will be verified by the: • unit secretary. administrative RN. • LPN/LVN in charge. st • pr ep .c • om • ng te • w w w .m yn ur si d i r e c t o r o f n u r s e s . A N S : C In most skilled nursing facilities, verification of orders (checking and signing them) is performed by the LPN/LVN. DIF: Cognitive Level: Application REF: d. 393 OBJ: Clinical Practice #1 TOP: Orders in Skilled Nursing Facility KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care • When the nurse discovers that the patients consent form for an invasive procedure is incorrect, the nurse should: • cross out the incorrect information and write error, and then write in the correct information. destroy the incorrect form and write a new one correctly. • cross out the entire form, but leave it in the chart as a permanent record. om • notify the physician of the error and clarify what the physician prefers to be done. ANS: B The consent form is considered a legal document and should be transcribed accurately to prevent errors; the incorrect one should be destroyed. DIF: Cognitive Level: Application REF: d. 393 OBJ: Clinical Practice #1 TOP: Consent Forms KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care • A patients condition warrants a transfer from Intensive Care to a regular nursing unit in the same hospital. Before assisting with the patients move, the nurse notes that the transfer has been authorized by the: • patient. • physician. si charge nurse. ur • ng te st pr ep .c • w w w .m yn • family. ANS: C In general, transfers from one nursing area to another require a specific order by the attending physician. The charge nurse of the receiving unit should be notified as well as the patient and family. DIF: Cognitive Level: Application REF: d. 395 OBJ: Clinical Practice #3 TOP: Transfer KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care • A newly admitted patient has his own walker that he wishes to use during this hospital stay. The responsibility of the nurse to this piece of durable equipment is to: • write the patients name on a wide piece of tape and affix it to the walker. • list the walker as part of the patients personal belongings and place the list in his chart. • tell the patient that personal walkers cannot be used in the hospital for safety reasons. • write a note in the nursing care plan that the om patient has his own walker. ANS: A All equipment brought to the hospital by the patient should be clearly labeled, usually with a wide piece of tape on which the patients name is written in large letters. DIF: Cognitive Level: Application REF: d. 395 OBJ: Theory #3 TOP: Admission KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse helping to organize the transfer of an elderly patient from the acute care facility to an extended care facility will be sure to: • check drawers and shelves for personal items. give unused medications to the patient. • ask the business office to send stored valuables to the receiving facility. ep .c • send a small snack with the patient. ANS: A Checking drawers and shelves for personal items prior to a transfer is helpful in preventing loss. DIF: Cognitive Level: Knowledge REF: d. 395 OBJ: Clinical Practice #3 TOP: Transfer KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: coordinated care • As a member of the health care team, the LPN/LVN understands that discharge planning for the hospitalized patient begins: • the day before discharge. yn ur si ng te st pr • at the time of admission. • immediately following diagnostic procedures or surgery. w as soon as a family meeting is scheduled. ANS: B Discharge planning begins at admission, especially if the diagnosis indicates that the patient will need rehabilitation or long-term assistance. DIF: Cognitive Level: Comprehension REF: d. 395 OBJ: Theory #5 TOP: Discharge KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: coordinated care • A patient who is scheduled for discharge has items that were stored in the hospital safe. After retrieving them, the nurse should document their return to the patient by: • making an entry in the physician progress notes. w w • .m • writing a note to the charge nurse. • having the patient sign for them as per policy. • asking the unit secretary to place a note in the chart. ANS: C • assisting the patient to get dressed. st writing the discharge instructions. te • pr ep .c Retrieve any valuables stored in the hospital safe before discharge and have the patient sign according to policy and procedure. DIF: Cognitive Level: Application REF: d. 395 OBJ: Theory #5 TOP: Discharge KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care • A patient has a hospital discharge order for later that day. The LPN/LVN understands that part of the discharge process to be performed by the registered nurse is: • packing the patients personal belongings. om • accompanying the patient to the hospital entrance. ANS: B Written discharge instructions are prepared by the RN. The remaining duties can be performed by the LPN/LVN. DIF: Cognitive Level: Application REF: d. 396 OBJ: Theory #5 TOP: Discharge KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care • A patient who has questions about the availability of home health services after hospital discharge should be referred to the: • physician. w w w .m yn ur si ng • • registered nurse. • occupational therapist. • medic al social worke r (MS .c om W). ANS: D An MSW can provide information about long-term planning, financial assistance, and community services available after discharge. DIF: Cognitive Level: Application REF: d. 396 OBJ: Clinical Practice #5 TOP: Discharge KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: coordinated care • A hospitalized patient tells the nurse that he intends to leave the hospital, against medical advice. The nurses initial action(s) should be to: • listen to the patient, answer questions, and offer to have the supervisor or physician speak with the advise the patient that this may mean that insurance would not pay for this hospitalization. • obtain a written explanation of the reasons from the patient and have the patient sign at the bottom pr ep • call both the supervisor and a family member to try to get the patient to reconsider. ANS: A It is the responsibility of the health team to help patients understand the significance of leaving against medical advice. Listen to what the patient has to say and offer to help get the problem resolved without resorting to a discharge. If the ultimate decision is to leave, the physician is notified and the patient is asked to sign a form indicating that he or she is leaving against medical advice. DIF: Cognitive Level: Application REF: d. 396 OBJ: Theory #5 yn ur si ng te st • w w w .m TOP: Discharge Against Medical Advice (AMA) KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A patient is near death and the family is upset and disorganized. The most helpful intervention for the patient and the family would be for the nurse to: • ask the family the name of their mortician. • offer to call the spiritual advisor (e.g., priest, minister, or rabbi). • encourage the family to perform their rituals. • encourage the family to visit the chapel. ANS: B If death is anticipated, many people derive significant comfort from spiritual or religious beliefs • read a number of articles about death and dying. • have a personal experience of a similar nature. om or practices. DIF: Cognitive Level: Application REF: d. 397 OBJ: Clinical Practice #6 TOP: Death of a Patient KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • For the nurse to provide support to families of patients who have died, it is most important to: • have an understanding that all people deal with death in due time. deal with personal feelings about death and dying. ANS: D Before someone can be a support person to someone who has lost a loved one, he or she must have dealt with personal feelings about death. DIF: Cognitive Level: Comprehension REF: d. 397 OBJ: Clinical Practice #6 TOP: Death of a Patient KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: psychosocial adaptation • A nurse who was present at the time of the death of a patient should document: • time of death. ng te st pr ep .c • time at which life signs ceased. • notification of the mortuary. ur si • which family members were notified. ANS: B It is still required in most states for a physician to pronounce death. The nurse should document when all signs of life ceased. The name of the person making the pronouncement and the time should be documented. DIF: Cognitive Level: Knowledge REF: d. 397 OBJ: Theory #6 TOP: Pronouncement of Death KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: coordinated care • A young patient has died in the emergency department after suffering severe trauma. The nurse understands that this patients family may take comfort from the opportunity to: • allow donation of the patients organs. w w w .m yn • • view all of the injuries to the patients body. • plan the funeral before leaving the hospital. donate the patients belongings to charity. ANS: A When handled sensitively, requests for organ donation can be an opportunity for the family to allow something good to come out of a personal tragedy. DIF: Cognitive Level: Application REF: d. 397 OBJ: Clinical Practice #6 TOP: Organ Donation KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A blind, elderly patient is admitted to the hospital for dehydration and weakness. The nurse can make the admission process less stressful by: • sending all personal belongings home with family members. pr ep .c om • performing the initial assessment in a non-hurried manner. • providing a printed orientation handout regarding hospital policy. te st • performing a quick assessment before orienting the patient to the unit. ANS: B Elderly patients need time and support in adjusting to a hospital stay. An unhurried manner will show support and give the patient a little more time to adjust to the change. DIF: Cognitive Level: Application REF: d. 393, Elder Care OBJ: Clinical Practice #3 TOP: Admission KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • It is determined that a patient is brain dead after suffering a massive cerebral bleed. The physician has just talked to the family about removing the patient from life support. The nurse would anticipate: • calling the coroners office. w w w .m yn ur si ng • • calling the insurance company. • contacting the organ donation team. • a s k i n yn ur si ng te st pr ep .c om g a b o u t a n a u t o p s y . A N S : C Requests for organ donation are usually done by a physician or a nurse trained for making such requests. DIF: Cognitive Level: Comprehension REF: d. 397 OBJ: Clinical Practice #6 TOP: Organ Donation KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity • The nurse recognizes that an autopsy must be performed when the patient: • is over 52. died of unknown causes. • has requested it on admission. • has died in an industrial accident. w w .m • w ANS: B Autopsies are required when a patient has died of unknown causes. A family may request an autopsy, but the request must be signed by the next of kin. DIF: Cognitive Level: Knowledge REF: d. 397 OBJ: Theory #2 TOP: Autopsy KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: coordinated care • The nurse is performing an initial assessment on a patient with respiratory difficulty. The nurse would anticipate documenting signs and symptoms such as: • alteration in sensation. • use of accessory muscles. • regular respiratory pattern. • w w w .m yn ur si ng te st pr ep .c om e x c e s s i v e d r y n e s s . A N S : B An example of signs found in a patient with respiratory difficulty is use of accessory muscles of respiration. DIF: Cognitive Level: Comprehension REF: d. 394, Table 23-1 OBJ: Clinical Practice #2 TOP: Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse is assisting with an admission assessment of a patient with hypertension. While the nurse is preparing to weigh the patient, the patient states, It is not necessary to weigh me, because I weighed 130 pounds last week. What would be the nurses best response? • Are you sure that your weight has not changed? • I will write down your stated weight. • It is important to get a more recent weight. • Dont worry; your weight is • breast augmentation. • emergency admission for shortness of breath. postmastecto my breast implants . ANS: B Elective cosmetic surgeries are not covered by managed care companies. DIF: Cognitive Level: Comprehension REF: d. 392 OBJ: Theory #1 ur si ng te st pr • ep .c om confidential. ANS: C The patient should be weighed and measured rather than the stated height and weight being accepted. DIF: Cognitive Level: Application REF: d. 394, Table 23-1 OBJ: Clinical Practice #2 TOP: Assessment KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse reminds a patient that if enrolled in a managed care program, some procedures will not be approved for payment, such as: • cosmetic surgery to repair a scar from an accident. signs his or her name in red immediately below the physicians signature. w • w .m yn TOP: Non-payment for Procedures KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care • When the orders have been verified, the nurse: • draws a line below the orders and signs his or her name and the date. w • • writes: transcribed by A Nurse at 0900. draws a line down the left margin; then signs, dates, and times the transcription. ANS: D After the verification of the order, the nurse draws a line down the left-hand margin; then the nurse signs, dates, and times the transcription. DIF: Cognitive Level: Application REF: d. 294, Skill 19-1 OBJ: Clinical Practice #2 TOP: Documentation KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care COMPLETION • An examination of the remains of a body by a pathologist to determine the cause of death is a(n) . st pr ep .c om ANS: autopsy An autopsy is an examination of the remains by a pathologist to determine the cause of death. An autopsy is usually performed when the patient has died of unknown causes, has died at the hands of another, or has not been seen within a specific period of time by a physician. DIF: Cognitive Level: Knowledge REF: d. 297 OBJ: Theory #6 TOP: Post Mortem KEY: Nursing Process Step: N/ A MSC: NCLEX: N/A MULTIPLE RESPONSE • The nurse is orienting an elderly patient newly admitted to the nursing unit. Which are appropriate interventions to apply to alleviate the patients anxiety? (Select all that apply.) • Call the patient by his first name. Instruct the patient on the use of the call light. • Encourage the patient to ask questions regarding admission. • Allow extra time for the patient to process any new information. ng te • Lock all patient valuables in the facilitys safe storage. ANS: B, C, D Respectful and proper communication, especially during orientation of the patient to the facility, alleviates anxiety. It is best to orient the patient to the room, including the use of the call light, and to allow the patient time to process information and ask questions. DIF: Cognitive Level: Application REF: pp. 392-393 OBJ: Theory #3 TOP: Health Education KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance • A patient dies after suffering a severe cerebrovascular accident (CVA). The family members are informed of his demise and are at the bedside. What documentation should be noted in the patients chart? (Select all that apply.) w w w .m yn ur si • • Results of the autopsy • Who pronounced the patient • Official time of death • Time vital signs ceased • w w w .m yn ur si ng te st pr ep .c om W h y t h e p a t i e n t d i e d A N S : B , C , D Death must be accurately noted in the medical record and should include who pronounced the patients death, the time vital signs ceased, and the official time of death. DIF: Cognitive Level: Application REF: d. 397 OBJ: Clinical Practice #6 TOP: Pronouncement of Death KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity • The nurse appreciates that a routine hospital admission differs from an emergency admission in that a routine admission: (Select all that apply.) • is scheduled in advance. • is not stressful. • is completely covered by insurance. • has a predictable outcome. • allows time to arrange for disruptions in routine. ANS: A, E .c om Routine admissions are scheduled in advance with the full knowledge and permission of the third-party payer. Routine admissions allow for time to arrange for disruptions in a familys routine. All hospital admissions can be stressful and potentially have unpredictable outcomes. Insurance may not completely cover the expense. DIF: Cognitive Level: Comprehension REF: d. 391 OBJ: Theory #1 TOP: Routine Admissions KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: coordinated care • The nurse explains that the Admitting Department of the acute care facility has a number of significant duties, which include: (Select all that apply.) • arranging for pre-admission lab work and radiographs. notifying the patients spiritual counselor of the admission. • confirming that all admission criteria are met. • arranging for special diets. pr ep • making arrangements for co-pays and deductibles. ANS: C, E The Admitting Department handles all the paperwork necessary for hospitalization prior to the actual admission. They confirm that all pre-admission studies have been done and the insurance company is in accordance with the admission. They will also keep track of co-pays and deductibles of the patients insurance. .m w w w M U L T I P L E C H O I C E • Vital Signs yn Chapter 12 ur si ng te st • The nurse would anticipate a patient diagnosed with damage to the hypothalamus after suffering a head injury from a fall to exhibit: • a blood pressure elevation. • a temperature abnormality. • a decrease in pulse rate. • w w w .m yn ur si ng te st pr ep .c om d e p r e s s e d r e s p i r a t i o n s . A N S : B The hypothalamus, which is located between the cerebral hemispheres, controls body temperature. Any damage to the hypothalamus prevents the body from regulating its temperature. DIF: Cognitive Level: Comprehension REF: d. 335 OBJ: Theory #1 TOP: Vital Signs: Temperature KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse documents vital signs on a newly admitted patient as: blood pressure is 148/94 mm Hg, the pulse is 80 beats/min, and the respirations are 16 breaths/min. The nurse would record the pulse pressure as mm Hg. a. 14 b. 54 c. 64 d. 80 ANS: B tympanic arterial thermometer. • axillary. st pr • ep .c om a. 14 b. 54 c. 64 d. 80 ANS: B In calculating pulse pressure, take the difference between the systolic and diastolic pressures (i.e., 148 94 = 54). DIF: Cognitive Level: Analysis REF: d. 356 OBJ: Clinical Practice #4 TOP: Vital Signs: Blood Pressure KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • A patient has been admitted with hypothermia after lying unconscious overnight in an unheated apartment. The most appropriate route to assess the patients core temperature would be: • rectal. te • w w w .m yn ur si ng t y m p a n i c . A N S : D The same blood vessels serve the hypothalamus and the tympanic membrane, so the tympanic temperature is an excellent indicator of core body temperature, although it can be affected by ear wax. DIF: Cognitive Level: Application REF: d. 339 OBJ: Theory #3 | Clinical Practice #1 TOP: Vital Signs: Temperature KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse would document a patient as being febrile if the patients temperature was over F. ep .c om a. 99.5 b. 99.8 c. 100 d. 100.5 ANS: D A patient with a temperature above the normal range (100.2 F) is called febrile. DIF: Cognitive Level: Knowledge REF: d. 339 OBJ: Theory #3 TOP: Vital Signs: Temperature KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • To ensure an accurate reading when using a glass oral thermometer, it is necessary to: • rinse the thermometer with water. wipe the thermometer with alcohol. • shake down the galinstan alloy to below normal. pr • dry the thermometer with a dry cotton ball. ANS: C Oral thermometers remain at the last reading until they are shaken down; therefore, for accuracy, the thermometer must be below normal range before using. DIF: Cognitive Level: Application REF: d. 342 OBJ: Clinical Practice #1 TOP: Vital Signs: Temperature KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse taking an apical pulse would place the stethoscope at: • the left of the sternum at the third intercostal space. .m yn ur si ng te st • slightly above the left nipple. w • directly below the sternum. w • the left midclavicular line at the fifth intercostal space. ANS: D The apical pulse is determined by placing a stethoscope on a point midway between the imaginary line running from the midclavicle through the left nipple in the fifth intercostal space. DIF: Cognitive Level: Application REF: d. 350, Skill 21-4 OBJ: Theory #2 | Clinical Practice #2 TOP: Vital Signs: Pulse KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort The nurse would record a pulse as bradycardic if the rate were beats/min. • w • a. 64 b. 62 c. 60 d. 59 pr ep .c om ANS: D Bradycardia indicates a slow pulse that is less than 60 beats/min. DIF: Cognitive Level: Comprehension REF: d. 349 OBJ: Theory #3 TOP: Vital Signs: Pulse KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse is aware that the use of an oral glass thermometer would be contraindicated in a: • 5-year-old with a facial laceration. 12-year-old patient with a recent seizure. • 15-year-old with an abscessed tooth. st • 20-year-old with severe dehydration . ANS: B The rectal method is best for patients who have seizure activity so as not to put them at risk for biting and breaking the thermometer. DIF: Cognitive Level: Application REF: d. 339 OBJ: Clinical Practice #1 TOP: Vital Signs: Temperature KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse anticipates that if the stroke volume of a patient is reduced, the pulse will be: • stronger. w w .m yn ur si ng te • w • • weaker. bradycardic. • irregular. ANS: B A weak pulse will result if the stroke volume is reduced, because this decreases circulating volume. DIF: Cognitive Level: Comprehension REF: d. 337 OBJ: Theory #2 TOP: Vital Signs: Pulse KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • When caring for a victim with a gunshot wound to the abdomen who has lost a significant amount of blood, the nurse would anticipate the vital signs to reflect: • increase in temperature. • decrease in blood pressure. • decrease in pulse. w w w .m yn ur si ng te st pr ep .c d e c r e a s e i n r e s p i r a t i o n s . A N S : B If blood volume decreases, as with bleeding, blood pressure decreases. DIF: Cognitive Level: Analysis REF: d. 351, Table 21-2 OBJ: Theory #2 TOP: Vital Signs: Blood Pressure KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • When a frail 83-year-old patient whose temperature was 96.8 F at 8:00 AM shows a temperature of 98.6 F at 4:00 PM, the nurse is: om • • pleased that the temperature has come up to normal. • satisfied that the patient is warm enough. • concerned about the evidence of fever. relieved that the patient is improving. ANS: C In older patients who have a frail frame, the normal temperature is often 97.2 F. An elevation of • F is indicative of fever. DIF: Cognitive Level: Application REF: d. 340, Elder Care OBJ: Theory #4 TOP: Vital Signs in the Elderly KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • A patient who is terminally ill is described during shift report as having Cheyne-Stokes breathing. On assessment, the nurse anticipates finding: • a breathing pattern of dyspnea followed by a short period of apnea. te st pr ep .c om • rapid wheezing respirations for two or three breaths with short periods of apnea. • quick shallow respirations with long periods of apnea. ng • respirations gradually decreasing in rate and depth. ANS: A Cheyne-Stokes respirations are faster and deeper rather than slower and are followed by a period of no breathing. DIF: Cognitive Level: Analysis REF: pp. 354-355 OBJ: Theory #5 TOP: Vital Signs: Respirations KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse explains to a patient that the pulse oximeter can measure the arterial oxygen by: • assessing the amount of blood passing through the sensor. w w w .m yn ur si • • assessing the relative warmth of the skin on the monitored part. • measuring the oxygenated hemoglobin through a capillary bed. • measuring the respirations to the blood pressure via infrared rays. ANS: C The pulse oximeter measures oxygen saturation by means of a sensor/probe attached to peripheral digits, an earlobe, the nose, or the forehead as it passes through the capillary bed. Oxygenated blood absorbs more infrared than red light. DIF: Cognitive Level: Comprehension REF: d. 355 OBJ: Theory #5 TOP: Vital Signs: Pulse KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • Because the elderly have non-elastic blood vessels, they are prone to orthostatic hypotension. A priority intervention for a patient with orthostatic hypotension is to: • keep the patient in bed in a high Fowlers position. allow the patient to sit on the side of the bed for a minute before standing. • instruct the patient to use the wheelchair for all mobility activity. om • help the patient to rise quickly and support the patient for a minute. ANS: B The elderly often experience orthostatic hypotension and are at risk for falls and should be encouraged to sit on the side of the bed a minute before standing. These patients also benefit from the use of elastic stockings. DIF: Cognitive Level: Application REF: d. 361, Elder Care OBJ: Theory #2 TOP: Orthostatic Hypotension KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: safety and infection control • An elderly patient has a tympanic temperature of 96.2 F (35.7 C). What nursing intervention would best meet this patients need? • Take the patients vital signs every 4 hours, including temperature. ur si ng te st pr ep .c • Provide fluids to increase circulation. • Increase room temperature to 72 F (22.2 C) and add blankets to the bed. yn • Check the temperature orally to confirm the accuracy of the reading. ANS: C Nursing interventions for treating hypothermia should focus on reducing heat loss and supplying additional warmth, such as increasing the room temperature and adding blankets to the bed. DIF: Cognitive Level: Application REF: d. 341 OBJ: Theory #3 TOP: Vital Signs: Temperature KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse using either a regular or an electronic sphygmomanometer would ensure that the cuff is the correct size by: • using a narrow cuff for an obese patient. w w w .m • • making sure the width of the bladder is at least 3 inches. • confirming that the bladder goes around three fourths of the arm. • w w w .m yn ur si ng te st pr ep .c om a l w a y s u s i n g a w i d e c u f f . A N S : C For accuracy in a BP reading, the cuff of the sphygmomanometer should have a bladder that goes around three fourths of the arm. DIF: Cognitive Level: Comprehension REF: d 358, Skill 21-6 OBJ: Clinical Practice #4 TOP: Vital Signs: Blood Pressure KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • For the nurse to assess the most accurate respiration count, the nurse should: • inform the patient about his respirations and ask him to breathe normally. • count each inhalation and expiration for 1 full minute. • watch the patients chest rise and fall from a distance. • continue to hold the patients radial pulse, and count the respirations for 30 seconds and multiply the ANS: D The respirations should be counted for 30 seconds and multiplied by 2 if they are regular. If the patient knows the nurse is assessing the respiration, he or she may alter breathing. DIF: Cognitive Level: Application REF: d 350, Skill 21-5 OBJ: Clinical Practice #3 TOP: Vital Signs: Respirations KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • Elderly patients with hypertension may have an auscultatory gap in their Korotkoff sounds. It is important when taking their blood pressure measurement to: • continue to listen until the cuff is deflated. pump up the cuff until no sound is heard and then let the air out. • make sure the bell of the stethoscope is placed firmly over the artery. om • stop midway and begin to inflate again. ANS: A Many older adults with hypertension have an auscultatory gap in their Korotkoff sounds, making it important to listen until the cuff is deflated to avoid mistaking the auscultatory gap as the Korotkoff sound. DIF: Cognitive Level: Application REF: d 360 OBJ: Theory #6 TOP: Vital Signs in the Elderly KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • Regarding the blood pressure in children, the diastolic pressure is assessed by the auscultation of a: • clear tapping that gradually grows louder. ur si ng te st pr ep .c • murmur or swishing sound that increases with depression of the cuff. • sudden change or muffling of the sound. .m yn • louder knocking sound that occurs with each heartbeat. ANS: C A sudden change or muffling sound (Phase IV) indicates the diastolic pressure in children and in some adults. DIF: Cognitive Level: Application REF: d 360 OBJ: Clinical Practice #4 TOP: Vital Signs in Children KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse covers a newborn babys head with a cap, because the head: • is wet and needs to be dried. w w w • • has large fontanels. • allows loss of body heat. • can The nurse is caring for a patient who had a cardiac catheterization 2 hours ago and has a pressure dressing to his left groin. In addition to taking routine vital signs, the nurse should also check the: • strength of the femoral pulse. presence of the pedal pulse. • temperature of the right foot. ng • te st pr • ep .c om be resha ped more quick ly. ANS: C Infants lose considerable body heat through the scalp; therefore a cap helps prevent heat loss. DIF: Cognitive Level: Application REF: d 341, Elder Care OBJ: Theory #3 TOP: Vital Signs: Infant Temperature KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort si • w w w .m yn ur abi lity to mo ve the left toe s. A NS :B Pedal pulses are checked to determine whether there is any blockage in the artery following a cardiac catheterization. DIF: Cognitive Level: Application REF: d 351 OBJ: Clinical Practice #7 TOP: Pedal Pulse KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The accuracy in measuring the apical pulse is enhanced when the nurse: • counts the radial pulse at the same time. • counts the beats for one minute. • keeps the patient warm. uses the bell of the stethos cope. ANS: B Using the diaphragm of the stethoscope, the nurse counts the beats for 1 full minute. DIF: Cognitive Level: Application REF: d 350, Skill 21-4 OBJ: Clinical Practice #2 TOP: Counting Apical Pulse KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A 45-year-old patient who is alert and oriented has a blood pressure of 98/66 mm Hg, radial pulse of 76 beats/min (irregular), and respirations of 18 breaths/min (regular). The best nursing intervention is to: • notify the charge nurse of the hypotension. ng te st pr ep .c om • notify the doctor of the bradycardia. • check medications that might be the cause of the irregularity. si • check the patients record to determine his baseline blood pressure. ANS: D Check to see what the patients baseline vital signs indicate regarding the cardiac arrhythmia. DIF: Cognitive Level: Application REF: d 350, Skill 21-4 OBJ: Clinical Practice #6 TOP: Vital Signs KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse is caring for a patient with a cardiac disease history. When measuring vital signs, the nurse finds that the radial pulse is 102 beats/min and irregular. The nurse correctly: • listens to the apical pulse for 1 full minute. w w w .m yn ur • • takes the pulse for 30 seconds on the other wrist. • records the findings on the graphic sheet. • takes the pulse for 1 full minute on the other wrist. ANS: A respirations of 16 breaths/min. • a pulse rate of 120 beats/min. blood pressure of 128/86 mm Hg. ANS: C Pain increases the pulse rate. DIF: Cognitive Level: Application REF: d 351, Table 21-2 OBJ: Theory #2 TOP: Vital Signs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse explains that one method of environmental heat loss is convection, which is exemplified by body heat being reduced by: • being transferred to ice packs. yn ur si ng te st pr ep • .c • om An apical pulse is measured whenever the radial pulse is irregular or when the patient has a cardiac disease history. DIF: Cognitive Level: Application REF: d 358, Skill 21-6 OBJ: Clinical Practice #2 TOP: Vital Signs: Pulse KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse caring for a 30-year-old postsurgical patient would assess that the patient is in pain as indicated by: • a temperature of 102 F. production of sweat. • being removed by fast air currents from a fan. w • .m • w w exposu re to a cool environ ment. ANS: C Heat loss through convection can be accomplished by the use of a fan, which produces fast air currents. DIF: Cognitive Level: Comprehension REF: d 335 OBJ: Theory #1 TOP: Heat Loss by Convection KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • The home health nurse is instructing a caregiver about caring for a patient with hypothermia. The nurse recognizes that further instruction is warranted when the caregiver states, I will: • offer warm fluids to the patient, if permitted. • instruct the patient to remain on strict bed rest. • provide the patient with additional blankets. encourage the patient to increase his muscle activity. ANS: B Nursing activities for treating the patient with a below-normal body temperature should focus on reducing heat loss and supplying additional warmth. These activities may include (1) providing om • w w w .m yn ur si ng te st pr ep .c additional clothing or blankets for warmth (an electric blanket is most effective for raising temperature); (2) giving warm fluids, if permitted; (3) adjusting the temperature of the room to 72 F or higher; (4) eliminating drafts; and (5) increasing the patients muscle activity. DIF: Cognitive Level: Analysis REF: d 341 OBJ: Theory #3 TOP: Vital Signs: Hypothermia KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort COMPLETION • The nurse clarifies the average cardiac output in the adult is about L/minute. ANS: 5 five The average cardiac output of the normal adult is about 5 L/minute. DIF: Cognitive Level: Knowledge REF: d 337 OBJ: Theory #2 TOP: Cardiac Output KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse converts the Fahrenheit temperature of 99.2 to a . ANS: Celsius reading of 37.3 To convert Fahrenheit to Celsius: subtract 32 from the Fahrenheit reading and multiply by 5/9: 99.2 32 = 67.2 5 = 336 / 9 = 37.3. DIF: Cognitive Level: Analysis REF: d 338, Table 21-1 OBJ: Clinical Practice #1 TOP: Conversion of Fahrenheit to Celsius KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort MULTIPLE RESPONSE • Standards of the Joint Commission state that pain is the fifth vital sign and should be documented by assessments of: (Select all that apply.) • location. • duration. • usual methods of relief. • character. patent IV line. • injured hand. • 2-year-old hand amputation. ng te st • w w w .m yn ur si • d i a l y s i s s h u n t . A N S : A , pr ep .c om • intensity. ANS: A, B, D, E Pain should be monitored when vital signs are monitored, to closely assess for any cardiac changes. Pain is documented by assessments relative to location, intensity, character, frequency, and duration. DIF: Cognitive Level: Application REF: d 362 OBJ: Theory #7 TOP: Pain Assessment KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse would refrain from applying a blood pressure cuff on the affected arm of a patient who has a: (Select all that apply.) • previous mastectomy. ep .c om B , E Arms affected by previous mastectomies, patent IVs, or dialysis shunts should not be used to assess the blood pressure using an inflatable cuff. DIF: Cognitive Level: Application REF: d 358, Skill 21-6 OBJ: Clinical Practice #4 TOP: Contraindications for Blood Pressure Cuff Application KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse assesses that the 86-year-old patient is experiencing orthostatic hypotension when assessments indicate: (Select all that apply.) • dizziness upon rising to a standing position. a drop of 15 to 20 mm Hg from baseline when changing position. • nausea. • syncope. te st pr • si ur yn .m w w w b l u r r e d v i s i o n . ng • ANS : A, B, D, E Assessment of dizziness, drop in up to 20 mm Hg from baseline BP, syncope, and blurred vision are all indicative of orthostatic hypotension. Chapter 13 Physical Assessment MULTIPLE CHOICE • When the patient complains of nausea and dizziness, the nurse recognizes these complaints as data. • objective • medical • subjective ep .c om • adjunct ANS: C Subjective data are symptoms that only the patient can identify. DIF: Cognitive Level: Application REF: d 55 OBJ: Theory #3 TOP: Assessment Data KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The major goal of the admission interview (usually performed by the RN) is to: • establish rapport. help the patient understand the objectives of care. • identify the patients major complaints. st pr • initiate nursin g care plan forms. ANS: C The interview is used as part of the assessment process to elicit information about the patients physical, emotional, and spiritual health. DIF: Cognitive Level: Comprehension REF: d 55 OBJ: Theory #1 TOP: Interview KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • An example of a structured format for gathering data that aids in forming a database is: • North American Nursing Diagnosis AssociationInternational (NANDA-I). Maslows hierarchy. w • w .m yn ur si ng te • w • following the information in the history and physical. • Go rdo ns 11 He alth Patt ern s. om AN S: D Mary Gordons assessment guide is a guided path to cover 11 health points. Although Maslow may be used, it is not structured. DIF: Cognitive Level: Knowledge REF: d 55 OBJ: Theory #2 TOP: Gordons 11 Health Patterns KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • During the assessment phase of the nursing process, the nurse • develops a care plan to meet the patients nursing needs. begins to formulate plans for providing nursing intervention. • establishes a nursing diagnosis for the nursing care plan. • .c • • refers only to the admission assessment during the hospitalization. • performs a complete physical examination every day. ur si ng te st pr ep gathers, organizes, and documents data in a logical database. ANS: D Gathering and organizing data is the first step in the assessment phase of the nursing process. DIF: Cognitive Level: Comprehension REF: d 58 OBJ: Theory #1 TOP: Data Collection KEY: Nursing Process Step: N/ A MSC: NCLEX: N/A • After the admission assessment is completed, on subsequent shifts or days, the nurse: • does not assess the patient again unless the condition changes. assesses the patient briefly in the first hour of the shift. ANS: D The patient should be briefly assessed at the beginning of each shift and more thoroughly if his or her condition changes or as per the plan of care. DIF: Cognitive Level: Comprehension REF: d 59 OBJ: Theory #1 TOP: Physical Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse performing an admission interview on an elderly person should: • rush through the interview to avoid tiring the patient. w w w .m yn • • direct questions to the family rather than the patient. • allow more time for a response to questions. • prompt the patient to om speed recall. ANS: C When interviewing an elderly person, allow more time because the person will probably have a more extensive history and may take a little longer to recall the needed information. DIF: Cognitive Level: Application REF: d 58 OBJ: Theory #5 TOP: Admission Interview KEY: Nursing Process Step: Intervention MSC: NCLEX: Physiological Integrity: basic care and comfort • A nursing diagnosis consists of: • the physicians medical diagnosis listed as the nursing diagnosis. diagnostic labels formulated by the North American Nursing Diagnosis AssociationInternational (N • the patients explanation of his or her chief complaint or current complaint. ep .c • the results of the nursing assessment without consideration of doctors orders. ANS: B NANDA-I has formulated an official list of nursing diagnoses to identify patient problems and problems that patients are at risk of developing. A nursing diagnosis is independent of a medical diagnosis. DIF: Cognitive Level: Comprehension REF: d 61 OBJ: Theory #5 TOP: Nursing Diagnosis KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • An elderly patient with a medical diagnosis of chronic lung disease has developed pneumonia. She is coughing frequently and expectorating thick, sticky secretions. She is very short of breath, even with oxygen running, and she is exhausted and says she cant breathe. Based on this information, an appropriately worded nursing diagnosis for this patient is • Airway clearance, ineffective, related to lung secretions as evidenced by cough and shortness of bre w w .m yn ur si ng te st pr • w • • • Pneumonia, cough, and shortness of breath related to chronic lung disease. Difficulty breathing not relieved by oxygen and evidenced by shortness of breath. Cough and shortness of breath caused by pneumonia, chronic lung disease, advanced age, and exha ANS: A The nursing diagnosis from the NANDA list is complete with a cause and signs and symptoms. DIF: Cognitive Level: Analysis REF: d 63, Box 5-4 OBJ: Theory #5 TOP: Nursing Diagnosis KEY: Nursing Process Step: Diagnosis MSC: NCLEX: Physiological Integrity: basic care and comfort • If a patient has several nursing diagnoses, the nurse will first: • consult with the doctor regarding which diagnosis is most important. • devise nursing interventions for the most quickly solved problems. • prioritize the nursing problems according to Maslows hierarchy of needs. • review the patients medical prescriptions and other drugs being taken. st pr ep .c om ANS: C Nursing diagnoses (and thus their interventions) must be prioritized to identify the order of importance based on Maslows hierarchy. DIF: Cognitive Level: Analysis REF: d 63, Box 5-4 OBJ: Clinical Practice #4 TOP: Prioritizing KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A patient has a nursing diagnosis of Imbalanced nutrition: less than body requirements, related to mental impairment and decreased intake, as evidenced by increasing confusion and weight loss of more than 30-pounds over the last 6 months. An appropriate short-term goal for this patient is to: • eat 50% of six small meals each day by the end of 1 week. demonstrate progressive weight gain over 6 months. • eat all of the meals prepared during admission. ng te • verbalize understanding of caloric needs and intention to eat. ANS: A Short-term goals should be realistic and attainable and should have a time line of 7 to 10 days before discharge. DIF: Cognitive Level: Application REF: d 63 OBJ: Clinical Practice #6 TOP: Expected Outcomes KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • The nursing diagnoses that has the highest priority is: • Mobility, impaired physical, related to muscular weakness as evidenced by the inability to walk wi w w .m yn ur si • w Communication, impaired verbal, related to neuromuscular weakness as evidenced by facial weakn • speak. • • Imbalanced nutrition: less than body requirements, related to difficulty swallowing and inadequate evidenced by weight loss of 10 pounds. Airway clearance, ineffective, related to neuromuscular disorder as evidenced by choking and coug ANS: D Choking and aspiration are life-threatening events and take priority over problems such as weakness, inability to speak, or weight loss. DIF: Cognitive Level: Analysis REF: d 62 OBJ: Clinical Practice #4 TOP: Prioritizing KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A patient with visual impairment is identified as at risk for falls related to blindness. An appropriate intervention would be to: • assist the patient with feeding herself at the end of the meal. • arrange furnishings in room to provide clear pathways and orient the patient to these. • take the patients blood pressure before she gets up in the morning. .c pr ep report any falls immediately to the charge nurse and the doctor. ANS: B Providing clear pathways directly reduces the risk of patient falls. DIF: Cognitive Level: Analysis REF: d 59 OBJ: Clinical Practice #6 TOP: Clinical Planning KEY: Nursing Process Step: Planning om • • 3 years. • 5 years. si 2 years. ur • ng te st MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The North American Nursing Diagnosis AssociationI (NANDA-I) list is revised and updated every: • year. w w .m yn ANS: B NANDA-I meets every 2 years to revise and update the list. DIF: Cognitive Level: Knowledge REF: d 61 OBJ: Theory #5 TOP: NANDA-I KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A nursing care plan consists of: • nursing orders for individualized interventions to assist the patient to meet expected outcomes. w • • • orders for diagnostic and therapeutic procedures such as laboratory tests or radiographs. the physicians history and physical examination, as well as medical diagnoses. laboratory and radiograph reports, pathology reports, and the medication record. ANS: A The nursing care plan consists of the nursing orders for interventions to address problems and establish outcomes by which the plan can be evaluated. DIF: Cognitive Level: Comprehension REF: d 65 OBJ: Clinical Practice #5 TOP: Nursing Care Plan KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • In an acute care facility, a nursing care plan is usually reviewed and updated: • every shift. • every 24 hours. • once every 3 days. on ad mis sio n and dis cha rge. AN S: B Ongoing assessment, intervention, and evaluation lead to attainment or modification of the original plan for the patient who is acutely ill. The nursing care plan must be updated daily to reflect these changes. DIF: Cognitive Level: Knowledge REF: d 65 OBJ: Clinical Practice #6 TOP: Nursing Care Plan KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The nurse takes into consideration that the difference between a sign and a symptom is that a sign is: • subjective data. ur si ng te st pr ep .c om • unreliable because it depends on translation. • can be verified by examination. • something a patient reports that is verified by a relative. w .m yn • w w ANS: C Signs are objective data that can be confirmed by examination, assessment, or observation. Signs are reliable research-based data. DIF: Cognitive Level: Comprehension REF: d 62 OBJ: Theory #2 TOP: Assessment (Data Collection) KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse clarifies that nursing orders are also called: • goals. • qualifiers. • interventions. • w w .m yn ur si ng te st pr ep .c om m e a s u r e m e n t c r i t e r i a . A N S : C Nursing orders are also called nursing interventions and follow the same requirements when placed in a nursing care plan. DIF: Cognitive Level: Knowledge REF: d 65 OBJ: Theory #2 TOP: Nursing Orders KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The nurse designs the goals for patients in long-term facilities to be: • conditional. open ended. • based on behavioral norms. w • • l o n g t st pr ep .c om e r m . A N S : D Long-term goals are more appropriate for patients in long-term facilities because they will be there for an extended period and many of their health problems are chronic. DIF: Cognitive Level: Comprehension REF: d 65 OBJ: Theory #7 TOP: Long-Term Goals KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • Standardized Nursing Care Plans can: • be documented without alteration. have items altered or deleted. • become part of the record without documentation. te • help the family understand the concept of Nursing Care Plans. ANS: B Standardized Nursing Care Plans are generic and need to be altered to become individualized. They must be documented. DIF: Cognitive Level: Comprehension REF: d 65 OBJ: Theory #7 TOP: Assessment (Data Collection) KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A nurse is caring for a patient with a medical diagnosis of right lower lobe pneumonia. The patient is expectorating thick green mucus, has an oxygen saturation level of 90%, and has audible crackles in the base of the right lung. An appropriate nursing diagnosis for this patient is: w w w .m yn ur si ng • • • Airway clearance, ineffective, related to retained secretions as evidenced by expectoration of thick saturation level of 90%, and audible crackles in the base of the right lung. Airway clearance, ineffective, related to right lower lobe pneumonia as evidenced by expectoration mucus, oxygen saturation level of 90%, and audible crackles in the base of the right lung. Right lower lobe pneumonia, related to airway clearance, ineffective, as evidenced by expectoration c. d. ANS: A mucus, oxygen saturation level of 90%, and audible crackles in the base of the right lung. om Expectoration of thick green mucus, oxygen saturation level of 90%, and audible crackles in the ba related to right lower lobe pneumonia as evidenced by airway clearance. attainable. w • approved by the physician. w • .m yn ur si ng te st pr ep .c The nursing diagnosis is from the NANDA-I list and is complete with a cause and signs and symptoms. The other answers contain a medical diagnosis of pneumonia, which is inappropriate. DIF: Cognitive Level: Analysis REF: d 61 OBJ: Theory #7 TOP: Nursing Diagnosis KEY: Nursing Process Step: Diagnosis MSC: NCLEX: Physiological Integrity: basic care and comfort COMPLETION • Conclusions that have been made based on . ANS: observed data are inferences Inferences are conclusions made based on observed data. DIF: Cognitive Level: Knowledge REF: d 61 OBJ: Theory #6 TOP: Inferences KEY: Nursing Process Step: N/A MSC: NCLEX: N/A MULTIPLE RESPONSE • The nurse understands that an expected outcome should be: (Select all that apply.) • realistic. w • • within a defined time. included after patient collaborati on. ANS: A, C, D, E An expected outcome should be realistic and attainable and should have a defined time line after collaboration with the patient. DIF: Cognitive Level: Knowledge REF: d 63 OBJ: Theory #6 TOP: Nursing Process KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse is caring for a patient with a nursing diagnosis of impaired physical mobility related to neurologic impairment and muscular weakness. Appropriate interventions for this patient would include which of the following? (Select all that apply.) • Assist with range-of-motion exercises every 4 hours and as needed. Instruct patient to call for assistance when needing to get out of bed. • Apply wrist and ankle restraints to promote safety and prevent falls. • Teach about exercises that will strengthen muscles while lying in bed. om • Ambulate with physical therapy assistance at least three times a day. ANS: A, B, D, E The nurse selects appropriate nursing interventions to alleviate the problems and assist the patient in achieving the expected outcomes. Consider all possible interventions for relief of the problems and then select those most likely to be effective. DIF: Cognitive Level: Application REF: d 65 OBJ: Clinical Practice #5 TOP: Assessment KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • Appropriate nursing roles in the initial assessment would include: (Select all that apply.) • LPN obtains the vital signs of a new patient. si ng te st pr ep .c • RN performs a complete physical assessment. • LPN organizes data into a database. • RN reviews the patients chart for past medical/surgical history. yn ur • LVN contributes ongoing assessments. ANS: A, B, D, E The LPN/LVN, under the NFLPN standard, contributes assessments; the RN performs the physical assessment and medical records review and organizes the database. DIF: Cognitive Level: Comprehension REF: d 61 OBJ: Theory #2 TOP: Planning KEY: Nursing Process Step: Assessment MSC: NCLEX: N/A • Aside from the information obtained from the patient (primary source) in the admission interview, the nurse will also access: (Select all that apply.) • the patients family. w w w .m • • a reliable and up-to-date reference book. • the admission note. • the physicians history and physical. an observation of the patient for non-verbal clues. ANS: A, C, D, E The nurse conducting the interview uses information from the patients family, from the physicians admission note and history and physical, and from personal observation of the patient. DIF: Cognitive Level: Comprehension REF: d 55 OBJ: Theory #2 TOP: Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A nursing diagnosis identifies: (Select all that apply.) • patients response to illness. • underlying medical diagnosis. • causative factors. • potential risk for health problems . ANS: A, B, D, E pr related signs and symptoms. yn ur si ng te st • ep .c om • w w w .m Defining characteristics of nursing diagnosis include the patients response to illness and the causative factors. Signs and symptoms must also be identified for a nurse to select an appropriate nursing diagnosis. Medical diagnoses label an illness; nursing diagnoses are independent of medical diagnoses. DIF: Cognitive Level: Comprehension REF: d 61 OBJ: Theory #5 TOP: Defining Characteristics KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The statements that are correctly stated as expected outcomes are: (Select all that apply.) • Patient will be able to void in the bathroom independently. • Patient will be able to ambulate using a walker independently within 3 days. • The nurse will assist the patient to the bathroom three times a day. • Patient will perform active range of motion (ROM) of her upper extremities independently every 4 • The family will bring food from home to om improve patient appetite. ANS: B, D Expected outcomes need to have a time frame and be measurable. Ambulating with a walker within three days and performing ROM independently for four hours are both measurable outcomes with clear time frames. The outcome of voiding independently does not have a time frame. Assisting the patient to the bathroom is a nursing intervention. DIF: Cognitive Level: Comprehension REF: d 63 OBJ: Theory #6 TOP: Expected Outcomes KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The nurse should make a point when closing the initial interview to: (Select all that apply.) • develop rapport. summarize the problems discussed. • thank the patient for his or her time. • discuss the nursing goals associated with nursing diagnoses. pr ep .c • give a copy of the nursing care plan to the patient. ANS: B, C The nurse should summarize the problems discussed, thank the patient for his or her time, and explain what happens next and when the nurse will return. DIF: Cognitive Level: Comprehension REF: d 58 OBJ: Theory #1 TOP: Nursing Process KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The seven domains of the Nursing Interventions Classification (NIC) taxonomy include: (Select all that apply.) • community. .m yn ur si ng te st • health system. • socioeconomic level. safety. w • w • w • behavioral. ANS: A, B, D, E The seven domains of the NIC taxonomy are: physiological: basic; physiological: complex; behavioral; safety; family; health system; and community. DIF: Cognitive Level: Knowledge REF: d 65 OBJ: Theory #5 TOP: NIC KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The purpose of the Nursing Outcomes Classification (NOC) is to: (Select all that apply.) • validate classification by field test. • identify labels. • provide language labels for desired outcomes. • generate a ready-made nursing care plan for a patient. identify patient outcomes and indicators. ANS: A, B, C, E The purpose of NOC is to provide language labels to help identify and classify patient outcomes and validate classifications by field testing. Chapter 14 Special Examinations and Tests MULTIPLE CHOICE • A patient who is on an anticoagulant (Coumadin) asks, What did the physician mean when he said I was to have my blood tested every 2 weeks? The nurse explains, It is important to monitor the effects of the drug to see how long it takes your blood to clot. The blood test the physician was talking about is the: • complete blood count (CBC). te st pr ep .c om • activated partial thromboplastin time (APTT). • international normalized ratio (INR). ng • erythrocyte sedimentatio n rate (ESR). ANS: C The INR is a method for reporting the prothrombin time, which is prolonged with warfarin (Coumadin) therapy. DIF: Cognitive Level: Knowledge REF: d 403 OBJ: Theory #2 TOP: Blood Tests K E Y: N u r s i n g P r o c e s s S t e p : Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient is scheduled to have a blood chemistry profile drawn at 8 AM tomorrow. The note should be added on the care plan and report provided to the oncoming shift to withhold food and drink after: • 6 AM. w w w .m yn ur si • • • 12 midnight tonight. • 4 AM today. ep .c om n o o n t o d a y . A N S : B yn ur si ng te st pr Food and drink are usually withheld for 8 to 12 hours before blood chemistry tests are performed. DIF: Cognitive Level: Application REF: d 403 OBJ: Theory #3 TOP: Blood Tests KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care • A patient wants to know what was meant when the doctor said that his white blood cell (WBC) count had a shift to the left. The nurse explains that a shift to the left indicates: • an improvement in an infectious process. the relative effectiveness of the antibiotic therapy. • an increase in the number of immature WBCs. .m • that the infection is viral in nature. ANS: C In reporting a differential WBC, the less mature WBCs are reported on the left side of the page. An increase in immature WBCs causes the left side of the report to show large numbers and indicates an infection. DIF: Cognitive Level: Comprehension REF: d 403, Clinical cues OBJ: Clinical Practice #1 TOP: Differential KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse instructing in the collection of a midstream urine catch would tell the patient to first cleanse the external genitalia and w w w • then to: • begin voiding into the specimen cup. • let a few drops of urine dribble into the specimen cup. • void until the bladder is almost empty and then collect the end portion of the voiding in the cup. pass a small amount of urine into the toilet and then collect the specimen. ANS: D To collect a midstream specimen, the external genitalia are cleansed, a small amount of urine is passed, and then a midportion of the voiding is collected in a sterile container and used for a culture. DIF: Cognitive Level: Application REF: d 409 OBJ: Clinical Practice #1 TOP: Urinalysis KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse instructs an outpatient female patient preparing for an abdominal ultrasonography that prior to the procedure, she should: • eat or drink nothing after midnight. drink a liter of water. • empty the bladder fully. use enemas at home to clear the bowel fully. ANS: B For abdominal ultrasonography, the patient is asked to drink a liter of water before the procedure. This helps change the echo-reflection pattern from the bladder, helping to better distinguish the bladder from the female reproductive organs that lie nearby. .m yn ur si ng • te • st pr ep .c om • w w w DIF: Cognitive Level: Application REF: d 413 OBJ: Clinical Practice #1 TOP: Abdominal Ultrasonography KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse preparing a patient for a magnetic resonance imaging (MRI) should determine if the patient has: • respiratory allergies. • d • claustrophobia. • fear of the dark. ur si ng te st pr ep .c om i z z i n e s s . A N S : B The patient with claustrophobia can be reassured that there are methods to contact persons outside the cylinder. DIF: Cognitive Level: Application REF: d 415 OBJ: Theory #1 TOP: Fluoroscopy K E Y: N u r s i n g P r o c e s s S t e p : Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • Prior to the nurse transporting the patient to have a magnetic resonance imaging (MRI), it is essential that the nurse confirm that the patient: • has eaten a meal. has drunk a liter of fluid. • is not wearing anything with metal. yn • has a Fole y cath eter in plac e. AN S: C Nursing care before an MRI involves obtaining consent and ensuring that all metal is removed from the patients body, because the machine emits a strong magnetic field. DIF: Cognitive Level: Application REF: d 415 OBJ: Clinical Practice #4 TOP: MRI KEY: Nursing Process Step: Implementation w w w .m • MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A patient who is scheduled for a cardiac catheterization asks what the catheterization will reveal that an electrocardiogram would not. The nurse explains that the catheterization shows: • the entire heart to find evidence of cancer. • heart rhythm. • electrical activity of the heart action. oxygen concentratio n at various sites. ANS: D Cardiac catheterization is a procedure that determines the function of the heart, valves, and coronary circulation with its attendant oxygen concentration. DIF: Cognitive Level: Comprehension REF: d 416, Box 24-3 OBJ: Clinical Practice #1 TOP: Catheterization KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient who is to have a treadmill stress test at 11:00 AM today should not consume: • coffee and cream. • oatmeal and sugar. si toast and jam. ur • ng te st pr ep .c om • .m w w w p a n c a k e s a n d s y r u p . yn • listen to lung sounds. • take a blood pressure and pulse. pr • ep .c om A N S : B The patient should avoid caffeine and smoking for 6 hours before the test, but may have a light meal 2 or more hours beforehand. DIF: Cognitive Level: Comprehension REF: d 418 OBJ: Clinical Practice #1 TOP: Treadmill KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient who has undergone endoscopy is fully awake and asks the nurse for something to drink. After confirming that liquids are allowed on the physician order sheet, the nurse should: • assist the patient to the bathroom to void. check for the return of gag and swallow reflexes. ANS: D The patient should take nothing by mouth until the effects of local anesthesia have worn off and airway protective reflexes (such as gag and swallow reflexes) have returned. DIF: Cognitive Level: Analysis REF: d 419 OBJ: Clinical Practice #1 TOP: Endoscopic Examinations KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The patient in the skilled nursing facility who is to have a colonoscopy tomorrow complains about his limited diet prior to the examination. The nurse may offer the patient: • lime Jell-O. oatmeal thinned with milk. w w • strawberry soda. w • .m yn ur si ng te st • • v a n i l l a i bright red with clots. • pink tinged. • cherry colored. yn ur si • ng te st pr ep .c om c e c r e a m . A N S : A The patient is placed on a clear-liquid diet for 24 hours before colonoscopy and should avoid liquids that contain red or purple dye. Jell-O is part of a clear liquid diet. DIF: Cognitive Level: Application REF: d 410 OBJ: Clinical Practice #1 TOP: Endoscopic Examinations KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient has undergone cystoscopy and has a Foley catheter in place on return to the nursing unit. Immediately after the procedure, the nurse expects the urine color to be: • clear as water. w w w .m ANS: C It is common for the urine to be pink tinged after cystoscopy, but red bleeding and clots should be reported to the physician. DIF: Cognitive Level: Comprehension REF: d 420 OBJ: Clinical Practice #1 TOP: Cystoscopy KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient will undergo endoscopic retrograde cholangiopancreatography (ERCP) to determine the cause of jaundice. Before the test, the nurse would assess this patient for an allergy to: • eggs. • pork. • aspirin. • shellfish. on his right side-lying for 2 hours. • supine for 3 hours. .c • om ANS: D Allergy to shellfish is assessed, because an iodine-based contrast medium is used during the test. Shellfish hold and store iodine. DIF: Cognitive Level: Application REF: d 421, Safety Alert OBJ: Clinical Practice #1 TOP: Endoscopic Examinations KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: pharmacological and parenteral therapies • For the patient who just had a liver biopsy performed, the nurse should position him: • prone for 1 hour. on his left sidelying for 4 hours. ANS: B The patient should be turned onto the right side for 2 hours after the procedure to minimize bleeding from the site. DIF: Cognitive Level: Comprehension REF: d 422, Table 24-5 OBJ: Clinical Practice #5 TOP: Liver Biopsy KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • Following a colonoscopy with polyp removal, the wife of the patient is distressed that there is slight bleeding from her husbands rectum. The nurses most helpful response would be: • This small amount of bleeding is expected after the removal of polyps. I will notify the physician about this hemorrhage. w • w .m yn ur si ng te st pr ep • I will watch your husband very carefully to assess any further hemorrhage. w • • Dont worry. This small amount of blood happens with these procedures. ANS: A A small amount of bleeding following a colonoscopy with polyp removal is to be expected. The family should be prepared for the slight bleeding. DIF: Cognitive Level: Application REF: d 419 OBJ: Clinical Practice #1 TOP: Colonoscopy KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • To improve the comfort of an elderly patient who is to be in the radiology department for several hours, the nurse should send a(n): • family member with the patient. • extra pillow. • blanket. • w w w .m yn ur si ng te st pr ep .c om n e w s p a p e r t o r e a d . A N S : C Elderly people may become chilled by the cooler temperatures commonly experienced in ancillary departments such as radiology. DIF: Cognitive Level: Application REF: d 423, Elder Care OBJ: Theory #4 TOP: Elder Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • An elderly patient has had a series of enemas in preparation for a gastrointestinal diagnostic procedure. Which electrolytes should be monitored following the enemas? • Calcium and chloride • Sodium and potassium • Magnesium and phosphorus • yn ur si ng te st pr ep .c om S e l e n i u m a n d z i n c A N S : B A series of enemas can upset electrolyte balance, especially potassium and sodium. DIF: Cognitive Level: Application REF: d 419 OBJ: Theory #4 TOP: Loss of Electrolytes KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse explains to the patient that the significance of the hematocrit is that it: • indicates the number of circulating white blood cells. indicates the value of the hemoglobin. • refers to the separation of blood cells from plasma. .m • will decrease when the patient is in shock. ANS: C The hematocrit refers to the relationship of blood cells to plasma in the circulating volume. DIF: Cognitive Level: Knowledge REF: d 402 OBJ: Theory #2 TOP: Hematocrit KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • When obtaining a capillary blood sample for blood glucose, the nurse will select the puncture site to cause the least amount of discomfort, which is: • the end of the index finger. w w w • • the ball of the third finger. • at right angles to the fingerprint lines. • w w w .m yn ur si ng te st pr ep .c om t h e b a l l o f t h e t h u m b . A N S : C Using the right angle to the fingerprint lines places the puncture on the side of the finger rather than on more sensitive areas. DIF: Cognitive Level: Application REF: d 407, Skill 24-9 OBJ: Theory #3 TOP: Capillary Blood Test KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: physiological adaptation • A patient asks why the blood glucose meter directions state to wipe away the first drop of blood. The most informative response by the nurse would be: • This eliminates microorganisms from the sample. • The first drop is usually too small. • The first drop is usually contaminated. • The first drop has serous fluid that can dilute the specimen. ANS: D • after 10 seconds. .c after 5 seconds. ep • om Some machines state to wipe away the first drop of blood, which often contains a large portion of serous fluid that can dilute the specimen, causing a false result. DIF: Cognitive Level: Comprehension REF: d 407, Skill 24-9 OBJ: Theory #3 TOP: Blood Glucose Testing KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • A patient in the outpatient clinic has provided a urine sample. To perform a urine dipstick test accurately, the nurse wets the dipstick and starts timing: • immediately. pr • w w w .m yn ur si ng te st a f t e r 3 0 s e c o n d s . A N S : A The stick is inserted into the urine specimen and removed quickly, and timing is started immediately. It is tapped gently on the side of the container to remove excess urine. DIF: Cognitive Level: Knowledge REF: d 409, Skill 24-3 OBJ: Theory #3 TOP: Urine Dipstick Test KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse obtaining a wound culture would: • use clean gloves. • rotate the swab vigorously in the wound bed. • rinse the exudate on the swab with normal saline. • place the swab in the culture tube without touching the sides. ANS: D pulmonary congestion. • bleeding at insertion site. ng • w w w .m yn ur si • h y p o t e n s i o n . te st pr ep .c om The nurse should use sterile gloves, rotate the swab gently in the wound bed, and place it directly into the culture tube without touching the sides of the tube. DIF: Cognitive Level: Knowledge REF: d 425, Skill 24-5 OBJ: Theory #3 TOP: Wound Culture KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The patient who has just returned to the unit after an angiography test should be assessed immediately for: • swelling of tongue. A NS :C The insertion site is monitored for bleeding or formation of a hematoma. DIF: Cognitive Level: Application REF: d 418 OBJ: Clinical Practice #1 TOP: Angiography KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse instructing a patient who is to have a Papanicolaou smear (Pap smear) in 2 days would tell the patient to avoid: • sexual intercourse. • douching. • eating shellfish. • w w w .m yn ur si ng te st pr ep .c om t a k i n g a b u b b l e b a t h . A N S : B The patient who is to have a Pap smear should avoid douching or using any vaginal medication that might interfere with the collection of the cells of the cervix. DIF: Cognitive Level: Application REF: d 426, Skill 24-6 OBJ: Clinical Practice #7 TOP: Pelvic Examination KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment • The statement made by a patient that would delay a scheduled CT scan would be: • I have terrible claustrophobia. • I have just been started on metformin. • I am allergic to penicillin. I have an implan ted pacem aker. ANS: B Metformin should be discontinued before the test with an iodine-based contrast medium because metformin significantly alters renal function. DIF: Cognitive Level: Analysis REF: d 414, Clinical Cues OBJ: Theory #1 TOP: Metformin KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological and parenteral therapies st pr The nurse evaluates a prothrombin time (PT/INR) for a patient who is taking heparin. The nurses initial action should be to: • document the findings in the chart. notify the lab that they have made an error. • check the physicians order. te • ng • ep .c om • notify the physician of the lab finding. ANS: C Check the physicians orders to determine what test was ordered. If the PT/INR was ordered, confer with the charge nurse or physician as to the intent. The PT/INR measures the effectiveness of the drug warfarin (Coumadin), not heparin. A partial thromboplastin is the test used to evaluate the effectiveness of heparin. DIF: Cognitive Level: Analysis REF: d 403 OBJ: Theory #2 TOP: Partial Thromboplastin KEY: Nursing Process Step: Evaluation MSC: NCLEX: Safe Effective Care Environment: management of care • A major concern for an 86-year-old patient who has been NPO for 8 hours prior to a diagnostic test would be: • fatigue. w w w .m yn ur si • • • circulatory status. • hydration status. w w w .m yn ur si ng te st pr ep .c om n u t r i t i o n a l s t a t u s . A N S : C The elderly who are kept on an NPO status for prolonged periods of time are susceptible to dehydration and electrolyte imbalances. DIF: Cognitive Level: Comprehension REF: d 419, Elder Care OBJ: Theory #4 TOP: Dehydration in the Elderly KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: physiological adaptation COMPLETION • The nurse is aware that a patient who is to have a colonoscopy is requested to stop taking drugs that contain iron for prior to the test. ANS: • days three days Drugs containing iron are held 3 days before a colonoscopy because iron salts can obscure the film. Iron can also cause constipation, which makes the cleansing of the bowel more difficult. DIF: Cognitive Level: Knowledge REF: d 417 OBJ: Theory #1 TOP: Colonoscopy KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: pharmacological and parenteral therapies MULTIPLE RESPONSE • The nurse is aware that the chart of a patient going for a cardiac catheterization should have:(Select all that apply.) • a signed consent form. • a complete history and physical examination. • evidence of the initiation of NPO status at least 2 hours prior. • evidence of patient teaching done before the consent form is signed. • report of kidney function tests. administration of ordered preoperative medications. ANS: A, B, D, F Patient teaching must be done before a signed consent form is initiated. A complete history and physical examination is done and NPO status is initiated at least 6 hours prior to the procedure. The patient is also given ordered preoperative medications. DIF: Cognitive Level: Application REF: d 410, Patient Teachng OBJ: Clinical Practice #1 TOP: Informed Consent KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • The physician has ordered the collection of a 24-hour urine specimen. The nurses instructions to the patient for proper collection of the urine specimen include: (Select all that apply.) • keep the container refrigerated as needed. ng te st pr ep .c om • empty the bladder into the toilet and begin timing the collection. • void a small amount of urine after external genitalia are cleansed. • keep the container on ice if instructed to do so. ur si • save only the first voiding in the morning. ANS: A, B, D When a 24-hour urine specimen is collected, the patient should be instructed to empty the bladder into the toilet and begin timing the collection of the specimen; to add all urine to the collection container for the next 24 hours; to keep the container on ice or refrigerated; and when the 24 hours are up, to empty the bladder and add the urine to the collection container and then seal it and send it to the laboratory. DIF: Cognitive Level: Application REF: d 415 OBJ: Clinical Practice #1 TOP: Health Teaching KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse is aware that patients who are not candidates for magnetic resonance imaging (MRI) include patients with: (Select all that apply.) • a hip prostheses. w w w .m yn • • bleeding tendencies. • allergy to iodine. • cardiac pacemakers. • st pr ep .c om previo us radiolo gical treatme nt. ANS: A, D Patients with prosthetic hips and knees, implanted pacemakers, or metal clips or staples are not candidates for an MRI because of the magnetic field the test creates. DIF: Cognitive Level: Comprehension REF: d 421, Safety Alert .m yn ur si ng te OBJ: Clinical Practice #4 TOP: Topic: MRI KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse informs the patient who is to have an electroencephalogram (EEG) that the technician will try to stimulate seizure activity by asking the patient to: (Select all that apply.) • close his eyes. hyperventilate. • breathe in a rapid shallow fashion. hold a flashing light over his face. w • w • w • submerg e his hands in cold water. ANS: B, C, D During an EEG, abnormal brain activity can be stimulated by the patient being requested to hyperventilate, breathe rapidly with shallow breaths, and respond to a flashing light over his face. .m yn ur si ng te st pr ep .c om DIF: Cognitive Level: Comprehension REF: d 401, Skill 24-1 OBJ: Theory #1 TOP: EEG KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort OTHER • The nurse is to collect a sample of blood for a lab test. Arrange the sequence of a phlebotomy. (Separate letters with a comma and space as follows: A, B, C, D, E, F, G, H.) • Place vacutainer tube inside holder. • Press tube stopper onto needle. • Puncture site. • Apply tourniquet and cleanse site. • Label tube. • Fill tube completely. • Loosen tourniquet and apply pressure to site. • Perform hand hygiene and apply gloves. ANS: E, H, A, D, C, B, F, G The nurse should label the tube with patient identification, perform hand hygiene and apply gloves, place the vacutainer tube inside the holder, apply the tourniquet and cleanse the site, puncture the site, press the tube stopper onto the needle, fill the tube completely, and then loosen the tourniquet and apply pressure to the site. Chapter 15 Nutrition MULTIPLE CHOICE • The nurse reminds the patient that the salivary glands excrete saliva, which initiates the digestion of: • proteins. starches. w • fats. • fiber. w w • ANS: B Saliva initiates the digestion of starches. DIF: Cognitive Level: Knowledge REF: d 453 OBJ: Theory #1 TOP: Functions of the Gastrointestinal System KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse is aware that vitamin B12 is absorbed in the: • stomach. • large intestine. • liver. • ep .c om g a l l b l a d d e r . w w w .m yn ur si ng te st pr A N S: A Vitamin B12, an aid in hemoglobin syntheses, is absorbed in the stomach through the action of the intrinsic factor, which is secreted from the stomach wall. DIF: Cognitive Level: Knowledge REF: d 453 OBJ: Theory #1 TOP: Absorption of Vitamins KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse emphasizes the dietary recommendations made by the American Heart Association is to limit cholesterol mg/day. intake to a. 300 b. 400 c. 425 d. 500 ANS: A The American Heart Association recommends an intake of cholesterol to 300 mg/day or less. DIF: Cognitive Level: Knowledge REF: d 455, Box 26-1 OBJ: Theory #4 TOP: Dietary Recommendations KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • A patient refuses to eat all types of meat, which has led to a protein deficiency. The nurse recognizes that the only plant source that contains all nine essential amino acids is: • bean sprouts. • lima beans. • kidney beans. om • .m yn ur si ng te st pr ep .c s o y b e a n s . A N S : D Soybeans are the only plant source that provides all nine essential amino acids. DIF: Cognitive Level: Knowledge REF: d 455 OBJ: Clinical Practice #1 TOP: Sources of Protein KEY: Nursing Process Step: Planning w w w MSC: NCLEX: Health Promotion and Maintenance: detection and early prevention of disease • A patient weighing 132 pounds has been recommended to increase daily protein intake. The nurse assists the patient to make dietary selections of protein after calculating that the daily protein requirement for this g. patient is a. 24 b. 36 c. 48 d. 60 ANS: C The protein requirement for the day is equal to the number of kilograms of weight (convert lb to kg) multiplied by 0.8 (i.e., 132/2.2 = 48). DIF: Cognitive Level: Analysis REF: d 456 OBJ: Clinical Practice #3 TOP: Dietary Protein Recommendation KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • The nurse consults with a patient who is a vegan and stresses that this diet puts the patient at risk for: • diabetes. • iron deficiency. • osteoporosis • appetite. te gag reflex. ng • st pr ep .c om • scurvy. ANS: B In the vegan diet, all animal food sources are excluded, placing a patient who eats this diet most at risk for deficient intake of protein leading to an iron deficiency. DIF: Cognitive Level: Comprehension REF: d 456 OBJ: Clinical Practice #1 TOP: Vegan Diets KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • The nurse in a long-term care facility understands that the 86-year-old residents frequent complaints about heartburn are most likely due to the age-related decreased: • peristalsis. ur yn .m w w w s p h i n c t e r t o n e . si • ANS :D The age-related loss of muscle tone in the sphincters increases the incidence of heartburn and esophageal reflux. DIF: Cognitive Level: Comprehension REF: d 454 OBJ: Theory #63 TOP: Planning KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • The patient states that he uses a large amount of table sugar (sucrose) in his foods because it gives him quick energy. The nurse explains that sucrose will: • quickly raise the blood sugar, and the level drops slowly. • not raise the blood sugar as quickly as a protein source will. • cause a hunger and energy lag because of the rapid fall of the blood sugar. also act as a good support to the digestion of fiber. ANS: C Table sugar is high in sucrose, which is quickly absorbed into the bloodstream and can cause rapid rises and falls in blood glucose, which leads to hunger and an energy lag. DIF: Cognitive Level: Comprehension REF: d 457 OBJ: Theory #2 TOP: Simple Carbohydrates KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • The nurse evaluates the patients understanding of the fiber content of grains and cereals when the patient selects: • white bread toast with an orange. te st pr ep .c om • wheat bread toast with a peeled apple. • shredded wheat and a banana. si ng • w w yn w .m a b i s c u i t a n d a g r a p e f ur • 1 frankfurter. • 1 3-ounce pork chop. si ng • w yn w .m c h i c k e n b r e a s t w i t h s ur • w te st pr ep .c om r u i t . A N S : C Shredded wheat and a banana contain a total of 6 g of fiber per serving, whereas wheat toast with an apple contain a total of 4 g, white bread with a banana contain a total of 3 g, and a biscuit with a grapefruit contain a total of 4 g. DIF: Cognitive Level: Comprehension REF: d 458, Table 26-1 OBJ: Theory #3 TOP: Fiber KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • A patient has been placed on a reduced-cholesterol diet to help control heart disease. The serving that would be most appropriate for the patient to select for supper is: • 3 ounces of tuna canned in water. st pr ep .c om k i n . A N S : A The tuna canned in water contains only 2 g of fat, whereas the highest fat grams are found in the pork chop (19 g) followed by the chicken breast with skin (18 g). DIF: Cognitive Level: Application REF: d 459, Table 26-2 OBJ: Theory #9 TOP: Cholesterol KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • The nurse points out to the newly diagnosed type 2 diabetic patient that complex carbohydrates: • do not affect the blood sugar level. keep the blood sugar at an unsatisfactory high level. • lack adequate nutritional potential. • maintain a more consistent blood sugar level. ng te • w w w .m yn ur si ANS: D Complex carbohydrates (pasta, cereal, rice) provide a more consistent blood sugar level that simple sugars. DIF: Cognitive Level: Application REF: d 457 OBJ: Clinical Practice #4 TOP: Vitamins KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • When a patient asks how is a good way to increase fiber in the diet, the nurses best response would be: • eating unpeeled apples. • increase intake of dark leafy greens. • eating broiled salmon. • taking daily concentrate d fiber supplement s. ANS: A Eating the skins of fruits is a good source of fiber. Fiber concentrates do not contain needed vitamins and minerals. DIF: Cognitive Level: Application REF: d 457 OBJ: Clinical Practice #4 TOP: Fiber KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • The LPN/LVN filling out the Jewish patients dietary menu for lunch would avoid ordering: • meat and fish. • milk and vegetables. • meat and milk. om • w w w .m yn ur si ng te st pr ep .c v e g e t a b l e s a n d f r u i t . A N S : C Common food practices in Judaism include not eating meat and milk at the same meal. DIF: Cognitive Level: Application REF: d 469, Table 26-7 OBJ: Theory #7 TOP: Nutrition and Culture/Religion KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A nurse takes into consideration that the usual diet of Asian Americans has a potential for altering health because the diet is high in: • protein. • starch. • sodium. • wheat. .m • yn ur si ng te st pr ep .c om v i t a m i n C . A N S : C The Asian diet is high in sodium and fat. DIF: Cognitive Level: Comprehension REF: d 466 OBJ: Theory #7 TOP: Nutrition and Culture/Religion KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • The mother of a 4-month-old infant asks what type of cereal is most appropriate to feed the infant as a first solid food. The best response from the nurse is to suggest: barley. • corn. • rice. w w • w ANS: D A cereal such as rice is the best initial choice, because it is easily tolerated, provides additional calories and iron, and is least likely to be allergenic. DIF: Cognitive Level: Comprehension REF: d 466 OBJ: Theory #8 TOP: Nutritional Needs Across the Life Span KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: growth and development • A mother is concerned that her toddler is not eating enough at mealtimes. The most informative suggestion by the nurse would be to: • provide large servings to stimulate appetite. • provide single-item foods that do not touch each other on the plate. • increase the amount of milk at each meal. use plain white dishes to keep attention focused on food. ANS: B Toddlers prefer single-item foods in small quantities that do not touch each other on a colorful plate. Milk intake should decrease during the toddler years as solid food takes the place of milk. DIF: Cognitive Level: Application REF: d 467 OBJ: Theory #8 TOP: Nutritional Needs Across the Life Span KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: growth and development • On assessment, the nurse finds that the female patient has a BMI of 26, a waist of 37 inches, pale conjunctiva, and a large muscle mass. The indicator of this patient being overweight is: • BMI level. waist measurement. • conjunctiva. ur si • w w w .m yn • l a r g e m u s c l e m a s s . A N ng te st pr ep .c om • om S : B A waist measurement in women of over 35 is an indicator of greater risk for overweight and disease. DIF: Cognitive Level: Analysis REF: d 470 OBJ: Clinical Practice #2 TOP: Physical Signs of Obesity KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • The nursing action that is most beneficial toward creating an atmosphere conducive to eating for a hospitalized patient immobilized in bed is: • lower the head of bed as tolerated. remove the urinal from the over-the-bed table. • invite the patient to wash hands and face before eating. ep .c • use a deodorizer to remove any unpleasant odor in the room. ANS: B Remove distracting articles such as the urinal and emesis basin. DIF: Cognitive Level: Application REF: d 472 OBJ: Theory #6 TOP: Promoting Appetite KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse is delivering a meal tray to a patient in a skilled nursing facility who is a Muslim. The nurse should confirm the meal is free of: • raw fruits. eggplant. .m • yn ur si ng te st pr • pork. • lamb. w • w w ANS: C People of the Muslim faith are prohibited from eating pork. DIF: Cognitive Level: Application REF: d 467, Table 26-7 OBJ: Theory #7 TOP: Culture and Nutrition KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse would be sure the diet of a patient in an extended care facility who has a large pressure ulcer on his sacrum would include foods rich in vitamin: • A. • B1 (thiamine). • C. • E. ep .c om ANS: C Vitamin C helps protect the body against infections and promotes wound healing. DIF: Cognitive Level: Application REF: d 462, Table 26-4 OBJ: Theory #2 TOP: Vitamins KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse is visiting an elderly patient who lives alone. The suggestion made by the nurse that would be most helpful in improving the patients nutrition would be: • keep the environment noise free to concentrate on eating. decrease intake of fluids to improve appetite. • use salt as needed to spice up the flavor of foods. pr • cook favorite foods in bulk and freeze in individual serving containers. ANS: D Cooking and freezing favorite foods for easy preparation later is helpful in improving the overall nutrition of an elderly patient. DIF: Cognitive Level: Application REF: d 469, Patient Teaching OBJ: Clinical Practice #1 TOP: Nutritional Needs Across the Life Span ur si ng te st • w w w .m yn KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • When assisting with the nutritional assessment of a newly admitted, confused, emaciated cancer patient, the nurses most beneficial intervention to support the nutritional status of this patient would be to: • obtain the information from the family. • ask simple questions of the patient. • ask for a dietitian consult. • requ est an orde r for a full liqui • vitamin C. w w w .m yn ur si ng te st pr • r a w f r u i t s a n d v e g e t a b l e s . A N S : om protein. ep • .c d diet. AN S: C A dietitian should be consulted if the patient has high nutritional needs. DIF: Cognitive Level: Application REF: d 462 OBJ: Theory #9 TOP: Nutritional Assessment KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse caring for a patient with human immunodeficiency syndrome HIV would encourage the intake of greater amounts of: • vitamin D. • involving the family. .c giving the patient MyPlate for reference. ep • om B Patients with HIV lose muscle mass and need to increase their nutritional intake in the form of extra calories and protein. DIF: Cognitive Level: Comprehension REF: d 464 OBJ: Clinical Practice #4 TOP: Nutrition for HIV patient KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The home health nurse is visiting an elderly patient with a history of malnutrition and memory loss. The nurse addresses the nutritional needs of the patient by: • writing down all the information for the patient. making out a grocery list for the patient. ANS: C The patient may not be able to remember what needs to be done, and involving the family will help in meeting the patients needs. DIF: Cognitive Level: Application REF: d 469 OBJ: Clinical Practice #1 TOP: Malnutrition KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk • A patient of Mexican-American descent has a blood pressure of 160/90 mm Hg and is moderately obese. The nurse can help the patient modify his diet by suggesting: • decreasing spices when cooking. w w w .m yn ur si ng te st pr • • avoiding fried foods altogether. • limiting corn tortillas to two per day. • substitutin g the use of lard with canola oil. ANS: D Canola oil is an unsaturated fat, whereas lard is saturated, and saturated fats should be limited to w w w .m yn ur si ng te st pr ep .c om 10% of total fat intake. DIF: Cognitive Level: Application REF: d 459 OBJ: Clinical Practice #4 TOP: Patient Education KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease COMPLETION • The nurse takes into consideration that the patient with pernicious anemia who lacks the intrinsic factor cannot absorb . ANS: vitamin B12 The intrinsic factor excreted by the wall of the stomach allows the absorption of vitamin B12 DIF: Cognitive Level: Knowledge REF: d 462, Table 26-4 OBJ: Theory #5 TOP: Pernicious Anemia KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse uses a chart to show an obese patient who is trying to lose weight by counting calories that each calories. gram of carbohydrate supplies _ ANS: 4 four One gram of carbohydrate supplies 4 calories. DIF: Cognitive Level: Knowledge REF: d 457 OBJ: Clinical Practice #4 TOP: Calories KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The portion of carbohydrates that cannot be broken down by intestinal enzymes and juices is . ANS: fiber Fiber is the portion of carbohydrates that cannot be broken down by intestinal flora. Chapter 16 M U L T I P L E Fluid and Chemical Balance C H O I C E metabolic alkalosis. • weight loss. • diaper rash. .c • om A 10-month-old infant has had watery green stool for 2 days and refuses the bottle. The nurse is aware that the primary concern for this baby is: • metabolic acidosis. ep • ur si ng te st pr ANS: A Loss of bowel contents leads to metabolic acidosis. The child will lose weight and will probably have diaper rash, but the primary concern is the electrolyte imbalance. DIF: Cognitive Level: Analysis REF: pp. 436-437 OBJ: Clinical Practice #1 TOP: Dehydration KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • The patient who was admitted after vomiting for 3 days would show an abnormally low blood pressure because of a fluid shift from: • intracellular to the extracellular. interstitial to intravascular. • intravascular to the interstitial. .m yn • • w w w inter stitia l to the intra cellu lar. ANS :C If intravascular fluid, a type of extracellular fluid within the blood vessels, shifts from the plasma in the vascular space out to the interstitial space, a drop in blood volume occurs. DIF: Cognitive Level: Comprehension REF: d 432 OBJ: Theory #3 TOP: Distribution of Body Fluids KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • An isotonic state exists within a patients body fluids when the solute concentration of: • interstitial fluid is less than the transcellular. • intracellular and extracellular fluid is equal. • intracellular fluid is greater than extracellular fluid. extracellular fluid is lesser than intracellular fluid. ANS: B When the intracellular and extracellular fluid has the same concentration of particles, the solution is called isotonic (equal solute concentration). DIF: Cognitive Level: Comprehension REF: d 433 OBJ: Theory #3 TOP: Movement of Fluid KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse is aware that an infant is more at risk for dehydration because the infant: • has kidneys that reabsorb water from the intravascular space. pr ep .c om • has a larger body surface compared with body weight. • urinates more frequently. w w ng si ur yn w .m h a s f a t t h a t a b s o r b s w a t e r. A N S te • st • amino acids. • calcium. ep • .c The nurse points out that non-electrolyte products of metabolism are as important to health as electrolytes. Non-electrolytes include: • magnesium. pr • om : B Infants are more at risk for dehydration because they have a larger body surface compared with body weight. Their immature kidneys cannot reabsorb water as well as an adult, and fat does not absorb water. DIF: Cognitive Level: Comprehension REF: d 431 OBJ: Clinical Practice #1 TOP: Dehydration KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation st • .m yn ur si ng te p h o s p h a t e s . w w w A N S: B The non-electrolytes that are products of metabolism and serve to promote health in the body are amino acids, glucose, and fatty acids. DIF: Cognitive Level: Knowledge REF: d 432 OBJ: Theory #2 TOP: Non-electrolytes KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse assesses that the patient has developed abdominal pain, urinary retention, and confusion. The nurse concludes these signs are the result of an inadequate supply of: • calcium (Ca2+). • sodium (NA+). • phosphates (PO43). • w w w .m yn ur si ng te st pr ep .c om p o t a s s i u m ( K + ) . A N S : D The symptoms of a potassium level below 3.5 mEq/L are abdominal pain, urinary retention, confusion, decreased reflexes, and ECG changes. DIF: Cognitive Level: Analysis REF: d 438, Table 25-4 OBJ: Theory #4 TOP: Hypokalemia KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse gets a positive Chvosteks sign on a young woman with bulimia who has been giving herself frequent enemas containing phosphate. The nurse anticipates a laboratory finding of mEq/L. • sodium 140 • c a l • potassium 4.5 • magnesium 1.6 • magnesium. • sodium. si calcium. yn ur • ng te st pr ep .c om c i u m 6 . 5 A N S : D The low level of calcium is responsible for the sign. The positive Chvosteks sign is an indicator of a reduced calcium level. DIF: Cognitive Level: Analysis REF: d 438, Table 25-4 OBJ: Clinical Practice #2 TOP: Hypocalcemia KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • A patient has been identified as having a dietary deficiency of vitamin D. The nurse understands that this patient is also at risk for having a deficiency of: w w w p o t a s s i u m . A N S : A .m • Nutritional deficiency of vitamin D can result in hypocalcemia because of the patients inability to absorb calcium. DIF: Cognitive Level: Comprehension REF: d 440 OBJ: Clinical Practice #1 TOP: Hypocalcemia KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse explains that the dehydrated patients urine is concentrated because: • renal tubules reabsorb more water and reduce urine output. kidneys cease to function. • blood pressure drops. om • the colon retains more fluid from the fecal waste. ANS: A When dehydration occurs, the renal tubules of the kidney reabsorb more water to be returned to the circulating volume, making the urine concentrated. DIF: Cognitive Level: Comprehension REF: d 433 OBJ: Theory #3 TOP: Dehydration KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse is aware that small ions such as glucose, oxygen, and carbon dioxide redistribute themselves through semi-permeable membranes by a process called: • diffusion. • blood pressure. yn .m w w w A N S: A si osmosis. ur • • r e h y d r a t i o n . ng te st pr ep .c • 12 to 24 hours. • 3 days. • 1 week. ep .c • om Glucose, oxygen, carbon dioxide, and other small ions diffuse through membranes until they are evenly distributed. DIF: Cognitive Level: Knowledge REF: d 433 OBJ: Clinical Practice #5 TOP: Diffusion KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: physiological adaptation • A patient with healthy kidneys experiences metabolic alkalosis resulting from episodes of vomiting. The nurse takes into consideration that the kidneys can clear the alkaline substances and fully stabilize the patients pH in approximately: • 3 to 5 minutes. yn ur si ng te st pr ANS: C The compensatory ability of the kidneys takes more time to work than does the compensatory action of the lungs; 3 days are needed for the kidneys to stabilize pH within normal range. DIF: Cognitive Level: Knowledge REF: d 441, Clinical Cues OBJ: Clinical Practice #5 TOP: AcidBase Balance KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: physiological adaptation • A patient with a history of severe chronic obstructive pulmonary disease (COPD) is most likely to have: • respiratory alkalosis. respiratory acidosis. • metabolic alkalosis. w w w • .m • m e t a b o l i c a • metabolic alkalosis. w w w .m yn ur • m e t a b o l i c a c i d o s i s . ng respiratory acidosis. si • te st pr ep .c om c i d o s i s . A N S : B People with COPD are prone to chronic respiratory acidosis because of the retained CO2. DIF: Cognitive Level: Comprehension REF: d 441 OBJ: Clinical Practice #5 TOP: AcidBase Balance KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • A patient who is experiencing severe diarrhea is losing excessive bicarbonate ions. This patient is at risk for developing: • respiratory alkalosis. • lie down. • breathe through a re-breather mask. te st • pr ep .c om A N S : D Metabolic acidosis can be caused by either an excessive loss of bicarbonate ions or an excessive retention of hydrogen ions. DIF: Cognitive Level: Comprehension REF: d 442, Table 25-5 OBJ: Theory #5 TOP: AcidBase Balance KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • An anxious adult patient is experiencing a respiratory rate of 40 breaths/min. The most appropriate intervention that the nurse could do is to instruct the patient to: • sit up. w w w .m yn ur si ng p a n t w i t h m o u t h o p e n . A N S : C Anxiety can lead to hyperventilation, causing respiratory alkalosis; the treatment is to have the patient breathe through a re-breather mask. In the home setting, the patient can be asked to breathe into a paper bag. DIF: Cognitive Level: Application REF: d 442 OBJ: Theory #5 • osmosis. • active transport. om TOP: AcidBase Balance KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse is aware that a more dynamic process that moves molecules into cells regardless of their electrical charge or concentration in the cell is: • filtration. ep .c • w w w .m yn ur si ng te st pr h y d r o s t a t i c p r e s s u r e s . A N S : C Active transport can move molecules into cells regardless of their electrical charge or concentration already in the cell. DIF: Cognitive Level: Knowledge REF: d 434 OBJ: Theory #3 TOP: Active Transport KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: pharmacological and parenteral therapies • For the accurate measurement to detect fluid retention, the nurse instructs the nursing assistants to measure the weight with the same scale: • each morning before breakfast after the patient has voided. • each day at noon before lunch, dressed in light clothing • in between meals, dressed in light clothing after voiding. just before bedtime, while the patient is in a hospital gown or pajamas. ANS: A Weight is measured at the same time every morning on the same scale, after the patient has voided and before eating. DIF: Cognitive Level: Application REF: d 444, Assignment OBJ: Clinical Practice #1 TOP: Assessment: Fluid and Electrolytes KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient with congestive heart failure has gained 1.1 pounds over the last 24 hours. The nurse is aware that this weight gain represents a fluid retention of L. a. 0.25 b. 0.5 c. 1.0 d. 2.0 ANS: B Each 2.2 pounds of weight equals 1 kg, which in turn equals 1.0 L of fluid. Therefore, 1.1 pounds equals 0.5 kg and is equal to 0.5 L of fluid. DIF: Cognitive Level: Analysis REF: d 444, Clinical Cues OBJ: Theory #4 TOP: Calculation KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse is comparing sitting and standing vital signs for a patient who has been diagnosed with dehydration. The pulse rate has increased by 10 beats/min at 1 minute. The nurse then anticipates the blood pressure to show a(n) mm Hg. w w w .m yn ur si ng te st pr ep .c om • • • increase of 5 • drop of 40 • drop of 20 w w w .m yn ur si ng te st pr ep .c om i n c r e a s e o f 1 0 A N S : C A drop in systolic blood pressure by at least 20 mm Hg accompanied by a pulse rate increase of at least 10 beats/min at 1 minute following position change is suggestive of fluid-volume deficit. DIF: Cognitive Level: Analysis REF: d 444, Clinical cues OBJ: Clinical Practice #1 TOP: Assessment: Fluid and Electrolytes KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • A patient drank a cup of coffee, a half glass of orange juice, and half a carton of milk with breakfast. Using common equivalents of food containers as a guide, the nurse notes on the intake column of mL. the intake and output sheet that the patient consumed a. 360 b. 400 c. 420 d. 600 ANS: C A coffee cup is generally equivalent to 240 mL, a half glass of juice is 60 mL, and half a carton of milk is 120 mL. DIF: Cognitive Level: Analysis REF: d 446, Table 25-8 OBJ: Clinical Practice #1 TOP: Intake and Output KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • At the beginning of the shift, a patients IV bag has 960 mL remaining. The IV fluid is running at 75 mL/hr. In 8 hours, there should be how many milliliters remaining in the IV bag? a. 150 b. 360 c. 450 d. 600 ANS: B • greatest during the night shift. ep greatest during the evening shift. pr • .c om a. 150 b. 360 c. 450 d. 600 ANS: B 75 mL/hr 8 hours = 600; 960 600 = 360. DIF: Cognitive Level: Analysis REF: d 446 OBJ: Clinical Practice #1 TOP: Intake and Output KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: pharmacological and parenteral therapies • The physician orders fluid restriction for a patient with severe fluid-volume excess. When a patient is placed on a fluid restriction, the allowance of fluids should be: • greatest during the day shift. spaced in equal increments for all shifts. ANS: A The greatest amount of fluid is given during the day shift, followed by the evening shift. The least amount of fluid is given at night, when the patient should be sleeping. DIF: Cognitive Level: Comprehension REF: d 447 OBJ: Clinical Practice #1 TOP: Intake and Output KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse is aware that the patient who suffered a brain injury with cerebral edema will most likely receive a fluid that is: • isotonic. hypertonic. w • w .m yn ur si ng te st • w • hypotonic. • e n h a n c e d w i si ng te st pr ep .c om t h v i t a m i n B . A N S : B Hypertonic fluids draw fluid from the intracellular space and reduce edema. DIF: Cognitive Level: Comprehension REF: d 446, Table 25-6 OBJ: Clinical Practice #4 TOP: Hypertonic Solutions KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: basic care and comfort • The patient who is prescribed a diuretic for fluid-volume excess is discharged home. The patient verbalizes understanding of his disease process when he says: • I can put catsup on my scrambled eggs. I can snack on salted popcorn. • I will snack on raisins. yn ur • w w w I w i l l a v o i d a p r i c .m • st pr ep .c om o t s . A N S : C The patient will lose electrolytes, especially potassium, because he is on a diuretic; snacks such as raisins and apricots are rich in potassium. DIF: Cognitive Level: Analysis REF: d 437, Patient Teaching OBJ: Clinical Practice #3 TOP: Teaching Plan for Sodium Restriction KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • The nurse is caring for a patient for whom a dose of IV potassium has been ordered. Prior to hanging the potassium, the nurse should: • check urine output to be above 60 mL/hr. check the dose with another licensed person. • confirm the IV fluid running is compatible with potassium. • start potassium with another venipuncture. ANS: C yn ur si ng te • w w w .m The nurse must confirm that the IV fluid that is running is compatible with potassium. A urine output of at least 30 ml/hr is essential prior to giving IV potassium. DIF: Cognitive Level: Application REF: d 449, Safety Alert OBJ: Clinical Practice #4 TOP: Intake and Output KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse caring for a frail 92-year-old dehydrated patient should add to the plan of care the potential for • over-hydration related to excessive thirst. • diarrhea related to dehydration. • pulmonary congestion related to excessive fluid intake. • f w w w .m yn ur si ng te st pr ep .c om a l l r e l a t e d t o c o n f u s i o n . A N S : D The dehydrated patient may become confused because of fluid and electrolyte losses. DIF: Cognitive Level: Analysis REF: d 435, Elder Care OBJ: Clinical Practice #4 TOP: Elder Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk potential COMPLETION • A patient with a serum potassium value of less than 3.5 mEq/L is . ANS: hypokalemic The normal range for potassium is 3.5 to 5.0 mEq/L. DIF: Cognitive Level: Analysis REF: d 432, Table 25-2 OBJ: Theory #2 TOP: Electrolytes KEY: Nursing Process Step: N/A MSC: NCLEX: N/ A • The nurse clarifies that when electrolytes are in solution, they break up and become . ANS: potassium. • magnesium. • amino acids. • glucose. .c • ep fatty acids. pr • om ions Ions are charged particles of electrolytes in solutions. They become either a cation with a positive charge or an anion with a negative charge. DIF: Cognitive Level: Knowledge REF: d 432 OBJ: Theory #3 TOP: Ions KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation MULTIPLE RESPONSE • The nurse clarifies that the electrolytes include: (Select all that apply.) • sodium. .m yn ur si ng te st ANS: A, C, D The intermediate products of metabolismamino acids (proteins), glucose, and fatty acidsare non- electrolytes. Sodium, potassium, and magnesium are all electrolytes. DIF: Cognitive Level: Comprehension REF: d 432, Table 25-2 OBJ: Theory #2 TOP: Electrolytes KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • Based on the information provided, which of these measurements should be recorded on the output sheet? (Select all that apply.) • 250 mL nasogastric secretions 200 mL diarrhea stool • 900 mL IV therapy 650 mL urine from Foley catheter w • w • w • • 2 4 0 m L m i 50 mL chest tube drainage concentrated urine. • hypertension. • weight gain. .m yn ur • si ng te st pr ep .c om l k A N S : A , B , D , E The nurse should calculate fluid intake, both orally and intravenously, and mark and record the amount of gastric suction contents, chest tube drainage, Foley catheter drainage, and feces. DIF: Cognitive Level: Application REF: d 448, Skill 25-1 OBJ: Clinical Practice #1 TOP: Intake and Output KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse assessing a newly admitted patient with marked edema from severe congestive failure would anticipate that the patient would exhibit: (Select all that apply.) • a thready pulse. • w w w crackl es heard on auscu ltatio n. ANS: C, D, E Persons with excess fluid volume as with a patient in congestive failure would exhibit a bounding hypertension and weight gain. These persons would also have a bounding pulse and copious diluted urine as the kidneys try to excrete the excess fluid. Because of fluid accumulation in the pleural space, crackles can be heard on auscultation when assessing a person with congestive blood pressure regulation. • heat regulation. • removing waste from the cells. .c • om failure. DIF: Cognitive Level: Comprehension REF: d 436 OBJ: Theory #4 TOP: Overhydration KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse explains that water as a constituent of the body has the functions of: (Select all that apply.) • transportation of nutrients. assists with digesti on of protein. ANS: A, C, D Water has four functions: (1) vehicle of transportation to and from the cells, (2) heat regulation, (3) assists with hydrogen balance, and (4) acts as medium for enzymatic action of digestion. Although the amount of water in the circulating volume has an effect on blood pressure, water does not control blood pressure. Water does not digest protein. ur si ng te st pr ep • w w w .m yn Chapter 17 Hygiene M U L T I P L E C H O I C E • The nurse instructs the patient that any injury to the skin initially puts the patient at risk for: • scar formation at the injury site resulting from the healing process. • infection with bacteria or viruses that may affect the person systemically. • loss of sensation caused by damage to the nerves in the area. loss of body fluids and an upset in the fluid and electrolyte balance. ANS: B The skin (and intact mucous membrane) is the first line of defense against invasion by pathogens, and any cut or abrasion can be an entry site. Scar formation, nerve damage, and fluid/electrolyte disturbance are likely only when there is a large or deep wound. DIF: Cognitive Level: Comprehension REF: d 288 OBJ: Theory #1 TOP: Skin Integrity KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • When the patient returns from the physical therapy department, he is diaphoretic and his skin is flushed but cool. Nursing intervention in this situation should be for the nurse to: • call his physician about the amount of exertion in physical therapy. pr ep .c om • suggest the patient walk slowly in the hall to cool down. • offer additional fluids to replace those lost through normal cooling. te st • place a light cover over the patient to prevent his chilling. ANS: C Diaphoresis (sweating) is the bodys normal response to rid itself of heat. Drinking fluids to replace those lost prevents dehydration. DIF: Cognitive Level: Application REF: d 288 OBJ: Theory #1 TOP: Fluid Replacement KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • During an admission assessment to a skilled care facility, the nurse notes that a 76-year-old man is thin and unsteady on his feet and has dry flaky skin on his arms and legs. An appropriate hygiene goal for this patient is that the: • patient will shower daily on an independent basis by the end of 1 month. w w w .m yn ur si ng • • nurse will give a tub bath or full bed bath daily. • patient will shower or tub bathe with assistance twice a week. • patient will tub bathe or shower with assistance daily. ANS: C Elderly people have decreased sweat and sebaceous gland activity and do not need a full bath or shower daily. Their skin is thinner and it becomes drier and itchy with overly frequent bathing. Because of the patients unsteadiness, it is not om safe to have him shower alone. DIF: Cognitive Level: Application REF: d 293, Elder Care OBJ: Theory #6 TOP: Hygiene and Safety KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • In assessing the skin condition of an elderly patient, the nurse notes that, over the sacral area, there is a 2-cm 3-cm area that is reddened, does not blanch around the perimeter, and is open at the center. The most effective documentation would be: • Patient has stage II ulcer on sacrum. No blanching of perimeter. Reddened area over sacrum, skin open in center. • Pressure ulcer on sacrum. Massaged with no improvement in color. ep .c • 2-cm 3-cm reddened area on sacrum with open center. Does not blanch. ANS: D Description of a pressure ulcer should be specific and give a visual picture of the area. Such documentation will be useful in calculating the Medicare reimbursement for the facility. DIF: Cognitive Level: Application REF: d 292, Elder Care OBJ: Clinical Practice #2 TOP: Pressure Ulcers KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • When instructing a nursing assistant about hygiene needs of a frail elderly patient, the nurse correctly educates the nursing assistant to: • Use warm, not hot, water and be sure the room is warm beforehand to avoid chilling. .m yn ur si ng te st pr • Use brisk drying and an alcohol rub to close the patients pores and prevent heat loss after the bath. w w • Put bath oil in the tub and use plenty of soap to really clean the patients skin while she is in the tub. w • • Completely dry the patients skin and apply a mild moisturizer. ANS: A Elderly people have drier, thinner skin and less subcutaneous fat. Therefore warm, not hot, water is needed, and chilling should be avoided. The elderly should use less soap (to decrease dryness), and the use of oils in the water can be hazardous. Elderly people should be patted, not rubbed, dry and moisturizer should be applied to skin that is still damp. DIF: Cognitive Level: Knowledge REF: d 293, Elder Care OBJ: Theory #6 TOP: Skin Care KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • An important factor to consider when assessing the hygiene needs of a patient is that: • the patient knows best what is needed in his hygiene routine. • the routine of the agency will determine when the patient is able to bathe. • hygiene is not as important as other needs of the patient. the patient may not have the same hygiene practices as the nurse. ANS: D Different cultures have different views of hygiene practices, such as use of deodorant, shaving, or daily bathing. These needs are an important part of health and recovery from illness. DIF: Cognitive Level: Application REF: d 289 OBJ: Theory #2 TOP: Culture and Hygiene KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity: psychosocial adaptation • What nursing interventions related to hygiene are appropriate for a patient who has had a recent stroke that caused rightsided (dominant) paralysis and inability to speak? • Perform a full bed bath, brush and floss his teeth, and give him a good back massage. te st pr ep .c om • • Set up a washbasin and supplies, tell the patient to wash what he can, and provide privacy for the p can. yn ur si ng • Encourage the patient to use his nondominant hand to wash his face, brush his teeth, and perform ot activities with assistance as necessary. Teach a family member to give a full bath so that the family member will be able to care for the pat ANS: B Patients should be encouraged to do as much of their hygiene as possible (and allowed) in order to increase their sense of independence. DIF: Cognitive Level: Application REF: d 287 OBJ: Theory #2 TOP: Promoting Independence KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The patient most at risk for a pressure ulcer would be: a 46-year-old man in traction for a fractured femur, who exercised regularly before his accident and • oriented. w w w .m • • a 54-year-old overweight man who is unconscious from a stroke, has a urinary catheter in place, an incontinent of liquid stool since a feeding tube was placed. a 72-year-old man admitted for elective surgery to replace his hip joint, who was • an avid bowler an his hip disease slowed him down. an 84-year-old man with Alzheimers disease who is pacing in the halls and who is incontinent of ur d. ANS: B every 2 hours. ilium. • scapula. si • ur heels. yn • ng te st pr ep .c om With risk factors of obesity, immobility, lowered mental awareness, and incontinence of stool, this patient clearly is at greatest risk of developing a pressure ulcer. DIF: Cognitive Level: Analysis REF: d 289, Box 18-1 OBJ: Theory #3 TOP: Risks for Skin Breakdown KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: reduction of risk • Because the elderly patient lies curled up in a side-lying position most of the time, the nurse, seeking to avoid a pressure ulcer, makes frequent assessments of the: • sacrum. w w w .m ANS: C A patient who lies in a constant side-lying position puts pressure on the bony prominence of the ilium. The sacrum, heels, and scapula are at risk in a patient who lies on his or her back. DIF: Cognitive Level: Application REF: d 291 OBJ: Theory #3 TOP: Pressure Ulcers KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: reduction of risk • A patient has a quarter-sized blackened eschar on both heels surrounded by a 1- to 2-cm indurated reddened area. The nurse is aware that these lesions are: • pressure ulcers that cannot be accurately staged because of the eschar. • stage I pressure ulcers because of the induration and redness. • stage II pressure ulcers because the skin has been broken. • stage III or IV pressure .c om ulcers because of the eschar. ANS: A Eschar must be removed to accurately stage an ulcer, because the nurse cannot know how deep the ulcer is. DIF: Cognitive Level: Analysis REF: d 291 OBJ: Clinical Practice #1 TOP: Pressure Ulcer Staging KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient with a nursing diagnosis of Skin integrity, risk for impaired, is noted to have reddened areas on his right shoulder and hip when he is repositioned on a 2-hour turning schedule. The nurse should: • massage the areas vigorously to restore circulation to the pressured areas. document that the patient has a stage I pressure ulcer of the right shoulder and hip. • not position the patient on the right side for at least 8 hours. ep • reassess the area after 30 to 45 minutes for reactive hyperemia. ANS: D Redness and nonblanching that remain after relief of pressure for 30 to 45 minutes are an indication of a stage I pressure ulcer. Therefore the area needs to be reassessed before it is labeled a stage I pressure ulcer. DIF: Cognitive Level: Application REF: d 291 OBJ: Clinical Practice #1 TOP: Pressure Ulcers KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: basic care and comfort • To perform oral care for an unconscious patient, the nurse takes which action first? • Position the patient in an upright sitting position with the bed at a comfortable working height for th .m yn ur si ng te st pr • Move the patient to the far edge of the bed with the head slightly elevated. w • Raise the bed to a comfortable working height and position the patient in a flat side-lying position. w • w • Lower the bed, lower both side rails, and turn the patients head to one side. ANS: B The bed should be at a comfortable working level for the nurse. The patient should be in a flat side-lying position to promote fluids draining from the mouth rather than running down the back of the throat and possibly resulting in aspiration. DIF: Cognitive Level: Application REF: d 303, Skill 19-2 OBJ: Clinical Practice #3 TOP: Oral Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse assessing for a pressure ulcer in a patient with darkly pigmented skin should: • examine the area under full florescent light. • look for a purple hue under natural light. • reassess areas that appear lighter under a halogen light. identify areas of a green hue under a halogen light. ANS: B Patients with darkly pigmented skin will show a purple coloration under natural light in the beginning stages of a pressure ulcer. DIF: Cognitive Level: Application REF: d 289 OBJ: Theory #3 TOP: Assessing for Pressure Ulcers KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient who has a dry, itchy dermatitis will most likely benefit from: • an oatmeal or starch therapeutic bath with tepid water. pr ep .c om • having his skin patted with alcohol to decrease the itching. • a very warm whirlpool bath for 20 to 30 minutes. st • avoiding any skin contact with water in the affected areas. ANS: A Oatmeal or starch baths are used to soothe dermatitis. Very hot water, soaps, perfumes, and alcohol rubs are contraindicated. The skin must be kept clean, even if there is dermatitis present, so although bathing may be decreased or modified, it is not eliminated. DIF: Cognitive Level: Comprehension REF: d 301 OBJ: Theory #5 TOP: Skin Care KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: pharmacological therapies • A nurse is preparing to give a complete bath to an unconscious patient. After performing the standard steps done before any procedure, the nurse: • washes each eye with a fresh area of the washcloth before washing the rest of the patients face. w w w .m yn ur si ng te • • wears protective gloves throughout the entire procedure. • begins with a back wash and rub to assess for pressure areas over the sacrum. • changes the water after washing the patients face, and again after washing his back. ANS: A The eyes should be washed without soap and before the water is soiled by face washing. Separate areas of the washcloth prevent the transfer of organisms from one eye to the other. DIF: Cognitive Level: Application REF: d 294, Skill 19-1 OBJ: Clinical Practice #2 TOP: Bed Bath KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • When providing perineal care for an uncircumcised male patient, the nurse: • provides perineal care the same as for a circumcised male. • ensures that the foreskin is retracted and the glans is exposed at the end of the procedure. • does not touch the glans during the procedure because it is very sensitive. retracts the foreskin and then cleans the glans, being sure to replace it at the end of the procedure. ANS: D In the uncircumcised male, the foreskin covers the glans and must be retracted to adequately cleanse the secretions that accumulate under the foreskin and can lead to infection. The foreskin must be pulled down to cover the glans after cleaning or it can swell and cause pain and constriction of the glans. DIF: Cognitive Level: Application REF: d 294, Skill 19-1 OBJ: Clinical Practice #4 TOP: Bathing KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • Providing oral care to a patient who has dentures includes: • asking the patient to place his teeth directly in a covered, labeled container for overnight storage. ng te st pr ep .c om • removing, cleaning, and storing the dentures in a labeled container at bedtime. • cleaning the dentures in hot water after each meal to remove debris and bacteria. ur si • using a toothbrush and toothpaste to clean the dentures in the patients mouth. ANS: B Dentures should be removed and cleaned before they are stored. Hot water should never be used. Dentures may be cleaned in the patients mouth, but they need to be removed to clean the patients palate and gums, as well as the undersides of the dentures. DIF: Cognitive Level: Application REF: d 304, Skill 19-3 OBJ: Clinical Practice #4 TOP: Oral Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse caring for a patient who is not taking any food or fluids by mouth because he is unconscious is aware that the patient: • does not need mouth care as frequently as the patient who is eating and drinking. w w w .m yn • • should have complete mouth care once a day when the nurse assesses the condition of his skin and • needs to have his mouth swabbed to moisten and remove secretions every 4 hours. should have his lips lubricated and his teeth brushed with mouthwash once a shift. ANS: C An unconscious patient needs mouth care about every 4 hours to prevent drying of secretions, halitosis, and possible blocking of the respiratory passage with accumulated dried secretions. DIF: Cognitive Level: Application REF: d 302 OBJ: Clinical Practice #3 TOP: Oral Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort .c It is most important for the nurse to write specific personal care plan modifications for the patient who: • is 76 years old, alert, oriented, and able to provide his own care. had a hip replacement 2 years ago and uses a cane to ambulate. • has an artificial eye and poor vision in the other. ep • pr • om • prefers a tub bath to a shower, preferably before bedtime. ANS: C Special care is necessary for the artificial eye, especially because the patient has poor vision in the remaining eye. DIF: Cognitive Level: Analysis REF: k 310 OBJ: Theory #6 TOP: Hygiene KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • A 20-year-old male patient is admitted after an auto accident. He has blood and dirt matted in his hair. The nurse should: • blot the tangled, bloodied hair and then provide a bed shampoo to remove the remaining dirt and de • comb the tangles out with a fine-toothed comb, starting at the scalp and working down to the ends o remove tangles by using alcohol or water on small sections of hair, holding the hair between the sca • nurse is brushing or combing. w w .m yn ur si ng te st • shampoo the hair as well as possible and leave the tangles alone. ANS: C Removing tangles in small sections is more comfortable for the patient. Trying to shampoo before removing some of the tangles makes the situation worse. DIF: Cognitive Level: Application REF: k 306, Skill 19-4 OBJ: Clinical Practice #4 TOP: Hair Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • When the nurse is assisting a male patient to shave his face, it is most important for her w • to: • practice on a male friend or relative before trying it on a patient. • have the patient shave first before any other hygiene measures are performed. • be sure the patient knows to draw the razor in the direction the hair grows. check whether a safety razor can be used or whether it is contraindicated. ANS: D A patient who is on anticoagulants or who has a bleeding tendency should use an electric razor. DIF: Cognitive Level: Application REF: k 308 OBJ: Clinical Practice #4 TOP: Shaving KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity • A usual routine for providing nail care to a patient includes: • soaking the nails in warm soapy water to soften before cleaning under the nail edge with an orange ep .c om • gently cleaning under the nails with a metal file to remove dirt and dead skin and then soaking hand • cutting toenails with rounded edges to prevent scratching or ingrown nails. st pr • cutting toenails and fingernails every 2 or 3 days to keep them short and clean. ANS: A Soaking nails softens them and makes it easier to remove dirt or to cut them. A metal file should not be used under the nails. DIF: Cognitive Level: Knowledge REF: k 308 OBJ: Clinical Practice #4 TOP: Nail Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse is caring for a patient who is wearing contact lenses. If the patient cannot care for the lenses himself, and the nurse has difficulty removing a hard lens by hand, it is correct for the nurse to: • leave the contacts in place for up to a month. use a lens suction cup to remove the lens. w • w .m yn ur si ng te • w • • request an ophthalmologist (eye specialist) to come in to remove the lenses. irrigate the eye with saline until the lens floats out. ANS: B A lens suction cup is usually available in health care facilities to remove contact lenses. DIF: Cognitive Level: Knowledge REF: k 310 OBJ: Clinical Practice #5 TOP: Eye Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • During the provision of oral care to an unconscious patient, the nurse uses suction primarily to: • remove secretions that might block respiratory passages. • remove emesis if the patient should vomit. • prevent fluids from collecting in the patients mouth and being aspirated. stimulate the patients gums and mucous membrane. ANS: C An unconscious patient may not have a gag or swallowing reflex, and thus fluids introduced during mouth care need to be suctioned out (and the patient is positioned to facilitate drainage with the head lowered and turned to the side). DIF: Cognitive Level: Comprehension REF: k 303, Skill 19-2 OBJ: Clinical Practice #3 TOP: Oral Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk • A patient with insulin-dependent diabetes has a below-the-knee amputation on the right leg. What modification of his personal care is noted as most important? • Perineal care should be performed at least twice a day to prevent urinary tract infections. te st pr ep .c om • A safety razor should not be used for shaving; an electric razor should be used. • The patient should be assisted to the shower, where he can use a shower chair. • The patients left foot should be soaked and gently dried, but his toenails should not be cut. ANS: D ur si ng • w w w .m yn A diabetic with a below-the-knee amputation is likely to have circulatory problems in the remaining foot. Therefore, good foot care is essential, but toenail cutting should be performed by a podiatrist. DIF: Cognitive Level: Comprehension REF: k 308 OBJ: Theory #4 TOP: Diabetic Foot Care KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse notes that her patient has an area of red skin that does not blanch with fingertip pressure. The nurse pressure ulcer. documents this finding as a stage • I • III • IV • II ANS: A A stage I pressure ulcer is characterized by an area of red, deep pink, or mottled skin that does not blanch with fingertip pressure. DIF: Cognitive Level: Comprehension REF: k 291 OBJ: Clinical Practice #1 TOP: Skin Integrity KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse stages a pressure ulcer as a stage II based on the knowledge that such lesions have: • mottled skin and induration. full-thickness skin loss and a deep crater. • partial thickness skin loss with the appearance of a blister. om • a deep pink area of unblanchable skin. ANS: D A stage II pressure ulcer is characterized by an area of partial-thickness skin loss involving the epidermis and/or dermis. It may look like an abrasion, blister, or shallow crater. The area surrounding the damaged skin may feel warmer. DIF: Cognitive Level: Comprehension REF: k 291 OBJ: Clinical Practice #1 TOP: Skin Integrity KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The culturally sensitive nurse caring for a Muslim woman who has noticeable body odor as well as abundant underarm hair should: • use soap and water under the arms. ur si ng te st pr ep .c • apply a cream type deodorant. • shave the underarms. .m yn • cut hair close to the armpit with scissors. ANS: A Washing the area with soap and water will reduce odor. Several cultures do not consider the use of deodorant or shaving underarms essential. These personal preferences should be respected. DIF: Cognitive Level: Application REF: k 289 OBJ: Theory #2 TOP: Cultural Considerations KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort w w w • • A nurse admitting a 76-year-old patient to the unit carefully documents the appearance of a stage III pressure ulcer and informs the charge nurse because: • the presence of an ulcer suggests previous lack of care. • the charge nurse will need to report the presence of the ulcer. • Medicare will reimburse the facility if the ulcer advances. documentation of a stage III ulcer on admission is part of good assessment. ANS: C Medicare will reimburse the facility at a higher rate if stages III and IV ulcers are documented within 2 days of admission. ur si ng te st pr ep .c Chapter 18 Comfort, Rest, and Sleep M U L T I P L E C H O I C E • The nurse assesses a patients sleep for NREM (non-rapid-eyemovement) sleep because this sleep has the characteristics of: • daytime activity. om • offering the most rest. • irregular respirations. .m yn • w w i n c r e a s e d h e a r w • chronic • phantom om ng • te st pr ep .c t r a t e . A N S : B NREM sleep is the stage of sleep when the body receives the most rest. DIF: Cognitive Level: Comprehension REF: k 605 OBJ: Theory #5 TOP: NREM Sleep KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient experiencing discomfort because of severe arthritis would be described as having pain. • acute turn the unit on before attaching it to the patient. w w • w .m yn ur si • episodic ANS: B Chronic pain is pain in which symptoms are controlled, but there is no cure, such as in arthritis. DIF: Cognitive Level: Comprehension REF: k 591 OBJ: Clinical Practice #2 TOP: Types of Pain KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient is beginning treatment for pain with a transcutaneous electrical nerve stimulator (TENS) unit. The nurse will initially: • apply conductive jelly to un-coated electrodes. • • place electrodes on all four extremities. adjust the settings below the level at which a tingling sensation is felt. ANS: A Conductive jelly is applied to electrodes that are not precoated to assure conductivity. DIF: Cognitive Level: Application REF: k 597, Skill 30-1 OBJ: Clinical Practice #4 TOP: TENS KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The patient with a recent abdominal incision has an abdominal binder applied. The nurse explains that this appliance helps reduce pain by: • increasing warmth to the incision site. • keeping sutures and staples in place. • supporting surface and internal tissues. adding back support to enhance early ambulation. ANS: C Binders are cloths wrapped around a limb or body part that have an incision and are effective in reducing pain associated with strains, sprains, and surgical incisions by providing support to the surface of the area as well as the internal tissues. DIF: Cognitive Level: Comprehension REF: pp. 595-596 OBJ: Clinical Practice #4 TOP: Pain Control KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse evaluating the effectiveness of an Aquamatic K-pad for the leg is aware that the patient who has the least risk for burn injury from this device would be the patient with: • impaired peripheral circulation. st pr ep .c om • severely sprained ankle. • decreased level of consciousness from a stroke. ng te • • w w w .m yn ur si neuri tis secon dary to diabe tes. ANS: B Patients with poor circulation, impaired movement or feeling, or decreased level of consciousness are more at risk for injury from burns when applications of heat are used. DIF: Cognitive Level: Analysis REF: k 597, Skill 30-1 OBJ: Clinical Practice #4 TOP: Heat Application KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A nurse caring for a patient who suffered a severe sprain and has an order for a cold pack application to the injured area would prevent patient injury by: • using heavy pressure on the cold pack for greater effectiveness. • preparing to apply heat instead if cold is not effective. • leaving the pack in place for over 30 minutes at a time. • placing a towel between the pack and the skin. ANS: D ep .c om A protective towel or pad should be placed between the pack and the skin to avoid cold injury. DIF: Cognitive Level: Application REF: k 598 OBJ: Clinical Practice #4 TOP: Cold Application KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A nurse is instructing a patient about relaxation techniques for pain management. The patient should: • keep bright lights on in the room. use this technique as a way to wake up in the morning. • tense and relax individual muscle groups, starting with the toes and feet. pr • try to tense and relax all of the muscles of the body at the same time. ANS: C Relaxation involves alternately tensing and relaxing the toes and feet, then working upward through the leg, the abdomen, the chest, the arms, and finally, the neck and head. DIF: Cognitive Level: Comprehension REF: k 598 OBJ: Theory #4 TOP: Relaxation KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A patient is receiving an ice massage for relief of muscle spasms in the neck. The patient complains that the ice is making the pain worse. Most helpful response from the nurse would be: • I know it is uncomfortable right now , but is will get better in a few minutes. I will go get an ice pack to pace on your neck. w • w .m yn ur si ng te st • w • • The alteration of hot and cold application is very helpful for your spasms. I will stop these cold applications. Not everyone is helped by them. ANS: D Cold applications make some patients experience an increase in discomfort. DIF: Cognitive Level: Analysis REF: k 598 OBJ: Theory #4 TOP: Ice Application KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient experiencing pain states that guided imagery has made the pain more manageable in the past. To assist this patient, the nurse should: • find a focal point in the room. • bring a newspaper or deck of cards according to patient choice. • obtain skin lotion and a towel to give a back rub. read from a script that helps the patient visualize a restful place. ANS: D Persons who have difficulty with imagery can be assisted by someone reading a script to help a patient mentally travel to a favorite spot that is relaxing, soothing, or peaceful. DIF: Cognitive Level: Application REF: k 599 OBJ: Theory #4 TOP: Imagery KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: basic care and comfort • The nurse takes into consideration that when the patient has an order for a patient controlled analgesia (PCA) the pump will be programmed by the: registered nurse. • physician. • LPN/LVN. ng te • st pr ep .c om • w w ur yn w .m p h a r m a c e u t i c a l c o m p a n y . si • adjuvant analgesic. • narcotic analgesic. pr • ep .c om A N S : A PCA pumps are programmed by the RN or the pharmacist. The physicians order will specify the size of the dose and the minimum time between doses. DIF: Cognitive Level: Knowledge REF: k 601 OBJ: Theory #4 TOP: Chiropractic KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse is aware that the new order for indomethacin (Indocin) involves the administration of a: • Cox-2 inhibitor. nonsteroidal antiinflammator y drug. ANS: D Indomethacin is a nonsteroidal anti-inflammatory drug (NSAID) which requires a prescription. DIF: Cognitive Level: Knowledge REF: k 600, Table 31-2 OBJ: Clinical Practice #4 TOP: Indomethacin KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: pharmacological therapies • The nurse appreciates the principal advantage in using patientcontrolled analgesia (PCA) is that it: • reduces patient anxiety about pain by giving the patient more control in its management. w w .m yn ur si ng te st • reduces the workload of the nurse, because it does not have to be checked often. • eliminates the risk of adverse drug effects from the medication. w • • completely eliminates any pain the patient is experiencing. ANS: A A principal advantage of PCA is that it reduces anxiety about pain, because patients are in control of their pain medication within machine-set limits. DIF: Cognitive Level: Comprehension REF: k 601 OBJ: Clinical Practice #5 TOP: PCA KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse caring for a patient with a Fentanyl patch assesses that the patient is abnormally sleepy, is slurring words and is unsteady when ambulating. The nurse should: • put up the side rails on the bed. elevate the head of the bed 45 degrees and offer coffee or cola drink. • remove the patch and wipe off the skin. • apply ice to skin around the patch. Headache • Nausea yn w w w .m • H y p o v e n t i l a t i o n A ur • si ng te st pr ep .c ANS: C When overdose signs occur with Fentanyl patches, the patch should be removed, the skin cleansed and the problem documented and reported to the charge nurse or physician. DIF: Cognitive Level: Application REF: k 601, Safety Alert OBJ: Clinical Practice #6 TOP: Fentanyl Patch KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies • A nurse is assisting in the care of a patient who is receiving pain medication by the epidural route. It is most important to monitor this patient for which adverse drug effects? • Constipation om • ep .c om N S : D Respiratory depression is a potentially dangerous side effect of epidural analgesia, and a patient receiving this type of pain medication requires frequent monitoring of respiratory rate. DIF: Cognitive Level: Comprehension REF: k 604, Steps 31-1 OBJ: Clinical Practice #6 TOP: Epidural Pain Control KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies • A patient with an epidural catheter needs to have the dressing at the insertion site changed. When cleaning the insertion site with povidone-iodine swabs, the nurse should: • use a circular motion working from the insertion site outward. use a circular motion working from the outside to the insertion site. • start above the insertion site and swab in a downward motion. st pr • start below the insertion site and swab in an upward motion. ANS: A Proper aseptic technique includes starting at the center (the insertion site) and working outward using a circular motion. DIF: Cognitive Level: Application REF: k 604, Steps 31-1 OBJ: Clinical Practice #5 TOP: Epidural Catheter KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A nurse is assessing the status of a patient who is sleeping. Which assessment data indicate that the patient is most likely in stage 3 of nonrapid eye movement (NREM) sleep? • Rapid respirations, rapid heart rate w w .m yn ur si ng te • w • • Rapid respirations, slow heart rate Decreased respirations, slow heart rate • Decreased respirations, rapid heart rate ANS: C Stage 3 of NREM sleep, in which respirations and heart rate slow, is similar to a coma; it is also called delta sleep or slow-wave sleep because of the high-voltage slow brain waves that occur. DIF: Cognitive Level: Comprehension REF: k 604 OBJ: Theory #7 TOP: Sleep KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse recommends that normal sleep patterns can best be acquired by suggesting to the patient that they: • smoke cigarettes. • drink wine. • take a nap during the day. • w w w .m yn ur si ng te st pr ep .c om e x e r c i s e i n t h e m o r n i n g s . A N S : D Maintaining a regular exercise schedule not too close to bedtime helps a person sleep. DIF: Cognitive Level: Comprehension REF: k 604 OBJ: Theory #8 TOP: Sleep KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A sleeping patient has periodic pauses in breathing, then starts to breathe again. The nurse recognizes this sleep pattern is consistent with: • insomnia. • sleep apnea. • narcolepsy. • w w w .m yn ur si ng te st pr ep .c om e x c e s s i v e N R E M s l e e p . A N S : B Sleep apnea is a condition in which the person stops breathing for brief periods during sleep. DIF: Cognitive Level: Analysis REF: k 606 OBJ: Theory #8 TOP: Sleep KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The suggestion by the nurse which is most helpful to a patient who complains of chronically not feeling rested after sleep would be: • avoid going to bed hungry or overly full. • try to exercise just before going to bed. • sleep late the next morning if possible if you are tired on awakening. • take a nap during the day to help relieve overall fatigue. ANS: A Going to bed hungry or with a full stomach can interfere with sleep. DIF: Cognitive Level: Application REF: k 606 OBJ: Clinical Practice #8 TOP: Sleep Disturbances KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The most helpful intervention by the nurse for a hospitalized child who is having difficulty falling asleep would be: • keeping a night light on in the room. • turning off all of the lights in the room. • having the parents bring a favorite blanket or pillow from home. giving of juice and cookies before being put to bed. ANS: C Many patients sleep better when they can have a favorite blanket or pillow from home. DIF: Cognitive Level: Application REF: k 607 OBJ: Clinical Practice #8 TOP: Sleep KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient who has difficulty falling asleep at night because of anxiety over family problems asks if he should start taking sedative pills from the pharmacy to sleep better. The best advice to give this patient is that these pills can be used for: • long periods of time, but it is best to check with the physician first. ng te st pr ep .c om • short periods of time, but it is best to check with the physician first. • long periods of time without physician approval, because they are nonprescription drugs. ur si • short periods of time without physician approval, because they are nonprescription drugs. ANS: B Sedative and hypnotic medications can be used to promote sleep, but they should be used for short-term relief and only after a physician has been consulted. DIF: Cognitive Level: Comprehension REF: k 607 OBJ: Clinical Practice #8 TOP: Sleep KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: pharmacological therapies • A natural supplement that can enhance sleep for many people is: • melatonin. w w w .m yn • • o i l • calcium. • magnesium. ur si ng te st pr ep .c om o f l a v e n d e r . A N S : A Melatonin, a natural supplement can enhance sleep hours for many people. Calcium and magnesium are used to relieve leg cramps. DIF: Cognitive Level: Knowledge REF: k 607, Sleep aids OBJ: Clinical Practice #8 TOP: Natural Sleep Aid KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The nurse takes into consideration The Joint Commission (TJC) standards for pain assessment and treatment include: • pain treatment is based on objective data collected by the nurse. pain treatment ends at discharge. • pain is assessed only for patients who complain of pain. yn • all patients have the right to appropriate assessment of pain. ANS: D The TJC standards related to pain state that all patients have a right to appropriate assessment and management of pain and should be educated in the process prior to discharge. DIF: Cognitive Level: Knowledge REF: k 590 OBJ: Theory #1 w w w .m • TOP: JCOAH KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • A relative complains that an elderly patient takes frequent naps during the day and awakens frequently during the night, and wants to know if this is normal. The nurse explains that an older adult: • will awaken more often during the night, but may nap more often during the day. • needs at least 10 hours of sleep a day to prevent fatigue. • requires less napping during the day to sleep better at night. should be given hypnotics to induce better sleep. ANS: A Sleep habits are very individualized, but normally, as an adult ages, sleep may be less at night with more naps being taken during the day. DIF: Cognitive Level: Comprehension REF: k 605 OBJ: Theory #6 TOP: Sleep Needs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse explains that endorphins are capable of reducing pain: • as a naturally occurring morphine like enzyme. in conditions that are physiological only. • by attaching to opioid receptors. when psychological stressors are the cause of pain. ANS: C Endorphins are naturally occurring opiate like peptides which attach to the opioid receptors of nerve endings and bock pain transmission. Endorphins are effective against both physiologically and psychologically causes pain. DIF: Cognitive Level: Comprehension REF: k 591 OBJ: Theory #4 TOP: Endorphins KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort COMPLETION is considered to • be the fifth vital sign. ANS: Pain Pain assessment is now performed along with each assessment of vital signs, and pain is now considered the fifth vital sign. DIF: Cognitive Level: Knowledge REF: k 590 OBJ: Theory #2 TOP: Pain KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A type of pain that is of short duration, lasting from a few hours to a few days, is known as pain. ANS: acute Acute pain is of short duration, lasting from a few hours to a few days. DIF: Cognitive Level: Knowledge REF: k 591 OBJ: Clinical Practice #2 w w w .m yn ur si ng te st pr • ep • .c om • TOP: Pain KEY: Nursing Process Step: Assessment MSC: NCLEX: N/A • The is the theory that by stimulating large diameter nerve fibers pain is diminished or totally controlled. w w w .m yn ur si ng te st pr ep .c om ANS: Gate Theory The Gate Theory is based on the premise that by stimulating large diameter nerve fibers by massage or vibration the gate to pain perception is closed against the pain impulses from the small diameter nerve fibers. DIF: Cognitive Level: Knowledge REF: k 591 OBJ: Theory #3 TOP: Gate Control Theory KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A pain scale FLACC is used in . ANS: assessing pain in infants FLACC stands for Face, Legs, Activity, Cry and Consolability. Which are assessed to estimate the pain in pre-verbal infants. DIF: Cognitive Level: Knowledge REF: k 594 OBJ: Clinical Practice #1 TOP: Pain in Infants KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • Travelers can combat jet lag by exposure to for several hours. ANS: sun sunlight Exposure to sunlight for several hours will help reset a travelers internal clock and reduce the effects of jet lag. DIF: Cognitive Level: Comprehension REF: k 605 OBJ: Clinical Practice #6 TOP: Jet Lag KEY: Nursing Process Step: Assessment MSC: NCLEX: N/A • A nurse removed a pain medication patch that has a metal clip before the patient goes to have a(n) . ANS: MRI magnetic resonance imaging All metal must be removed from persons who are going to have a MRI. DIF: Cognitive Level: Application REF: k 601 OBJ: Theory #4 TOP: MRI Consideration KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: safety and infection control MULTIPLE RESPONSE • The nurse outlines the four phases of nociceptive pain as: (Select all that apply.) • translation. • transduction. • transmission. • modulation. • .m yn ur si ng te st pr ep .c om p e r c e p t i o n . A N S : B , C , D , E The four phases of nociceptive pain are transduction, transmission, perception and modulation. w w w DIF: Cognitive Level: Comprehension REF: k 593 OBJ: Clinical Practice #1 TOP: Nociceptive Pain KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse attempts to help an 86 year old patient describe his pain because the nurse is aware the elderly do not express pain because they:(Select all that apply.) • are unaware of their discomfort. • believe pain is a natural consequence to aging. • are reluctant to bother the nursing staff. • have been culturally trained not to complain. • fea r ng te st pr ep .c om tak ing pai n me dic ati on. A NS : B, C, D The elderly often do not verbalize their pain out of the mistaken belief that pain is part of aging. They are reluctant to bother the staff and have been culturally trained not to complain. DIF: Cognitive Level: Comprehension REF: k 593 OBJ: Clinical Practice #1 TOP: Pain in the Elderly KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse performing a focused assessment on pain will assess: (Select all that apply.) • history of pain. verbal indicators. • psychological factors. • culture. yn ur si • w w w c o n t r i b u t i n g f a c t .m • st pr ep .c om o r s . A N S : A , B , C , E Factors to be assessed in a focused assessment of pain is the history, verbal and non-verbal indicators, psychological and other contributing factors, medication and treatments used . Although culture may limit a persons ability to express pain, it is not an important issue on a focused assessment. w w w .m yn ur si ng te Chapter 19 Safety M U L T I P L E C H O I C E • An elderly patient who is unable to get out of bed complains that the room is too cold because of the air conditioning and asks the nurse to open the window. The nurses best reply is: • Certainly, that will let in warm air from outside and should make you warmer. • The air conditioner is set to keep the most comfortable temperature in the room. • Ill adjust the thermostat in your room and get a blanket for you. • Agency policy prevents me from opening the window. ANS: C om Older inactive people need a warmer environment because of their poor temperature regulation. Rooms should be kept at a comfortable 68 to 74 F. Most hospitals prohibit the opening of windows for safety reasons. DIF: Cognitive Level: Application REF: k 313 OBJ: Theory #1 TOP: Environment Management KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • An appropriate environmental nursing intervention for a patient with respiratory congestion is to: • maintain the room temperature slightly cooler to decrease congestion. • moisten the respiratory passages with the use of an air humidifier. • order a large floor fan to make it easier to breathe. open the windows to encourage air circulation. ANS: B A very low humidity will dry respiratory passages. Vaporizers or humidifiers may be ordered for a patient with a respiratory condition. Small table fans may help some persons to breathe more easily. DIF: Cognitive Level: Application REF: k 314 OBJ: Clinical Practice #1 TOP: Environment KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The patient complains of an odor in his room that smells like something is rotting. The nurse makes an assessment of the room and: • changes the linens, which are wrinkled and rumpled from 24-hour use. ur si ng te st pr ep .c • rinses out the emesis basin of used dry tissues. • removes an old flower arrangement. .m yn • heavily sprays room deodorant around the patients bed. ANS: C Odors in hospitals are frequently unpleasant. The odor from a deteriorating flower arrangement is offensive. The arrangement should be discarded in a container outside the patients room. DIF: Cognitive Level: Analysis REF: k 314, Box 20-1 OBJ: Theory #1 TOP: Environment KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient complains of not being able to sleep because of the noise in the hall at night. The nurse should: • move the patient to the far end of the hall. w w w • • ask the doctor for a sleeping medication for the patient. • tell the patient to close the door. • request that co-workers limit hallway conversations. ANS: D The main cause of noise is people. Encourage the staff to limit conversations in the hallway and speak in lowered voices. DIF: Cognitive Level: Application REF: k 314 OBJ: Theory #2 make sure that the bed wheels are locked. • place the bed against the wall. ep • .c om TOP: Environment KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The best way to maintain safety measures relative to helping a patient get into bed is to: • set the bed height at the nurses waist level. insist that the patient stay in bed. ANS: B The goal is to provide safety when getting a patient into or out of bed. Locking the wheels to the bed is one way to ensure this safety measure. DIF: Cognitive Level: Application REF: k 315 OBJ: Theory #4 TOP: Safety KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: safety and infection control • When the nurse is making an occupied bed, back safety indicates that the nurse should initially: • raise the bed to the proper working height before starting. keep one side rail up at all times to keep the patient from falling. w • encourage the patient to use the side rail to help turn side to side. w • .m yn ur si ng te st pr • complete the linen change on one side before moving to the other side. ANS: A Bringing the bed to height-appropriate working level can prevent a back injury. Although other options are part of the occupied bed skill, they are not directed at preventing back strain. DIF: Cognitive Level: Application REF: k 321, Box 20-2 OBJ: Clinical Practice #2 TOP: Safety KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control w • • A patient has left-sided paralysis following a right-sided cerebrovascular accident (CVA). After completing a bed bath, the nurse should begin to change the sheets by: • lowering both side rails and rolling the patient to the side of the bed. • asking the patient to roll to his right and hold on to the side rail for support. • positioning the patient in a supine position with both side rails raised. positioning the patient in a side-lying position on his left side with the near side rails raised. ANS: D Moving the patient to the left side-lying position provides safety for the patient and allows the patient to use his good (right) hand to hold the rail. DIF: Cognitive Level: Analysis REF: k 318, Skill 20-2 OBJ: Clinical Practice #2 TOP: Safety KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • An elderly patient is discharged home after hip surgery. The statement that indicates a family member understands discharge safety instructions given by the nurse is, I will: te st pr ep .c om • install grab bars in the bathroom for both the toilet and bathtub. • put all personal items away to prevent my mother from dropping things. • dim the lights at night to prevent wakefulness. si ng • ensure that my mother takes naps during the day to prevent tiredness. ANS: A Grab bars in the tub and at the toilet help the person with joint impairment to bathe and toilet safely. Using well-lit areas during the day and night-lights at night is helpful to avoid falls. Daytime napping may cause restlessness at night. DIF: Cognitive Level: Analysis REF: k 322, Box 20-3 OBJ: Theory #4 TOP: Safety KEY: Nursing Process Step: Assessment MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse in a long-term facility who is making a fall assessment would identify the person most at risk for a fall to be a resident who: • paces all day in the halls and sleeps well at night. w w w .m yn ur • • had knee replacement surgery 2 days ago and wears a knee brace. • had a stroke with right-sided weakness 2 weeks ago and is confused. • uses a walker to ambulate both indoors and outdoors. ANS: C The most common factors predisposing a person to falls are impaired physical mobility, altered mental status, and unavailability of assistance. keep pathways clear of paper, shoes, and equipment. • apply a personal alarm. .c • om DIF: Cognitive Level: Analysis REF: k 321, Box 20-2 OBJ: Theory #4 TOP: Safety KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: safety and infection control • A patient who has right-sided weakness following a stroke is admitted to a long-term care facility and exhibits increasing wandering and inability for self-care. To protect the patient from the most frequent cause of injury among the elderly, the nurses most efficient intervention would be: • provide a night-light in the bathroom. ep • w w w .m yn ur si ng te st pr p r o v i d e h i p p r o t e c t o r s . A N S : C Because falls are the most common accidents among residents, the provision of a personal alarm to sound when the person attempts to get out of bed is the most efficient intervention. Keeping the pathways clear, provision of adequate light, and provision of hip protectors are all safety oriented but do not prevent • a heating pad and place it under the patients feet. • an electric blanket to increase warmth to legs at night. • a hot shower to increase circulation to legs. additional blankets and encourage the use of warm bed socks. ANS: D Extra blankets and bed socks will reduce the sense of cold. A person with diabetes or impaired circulation is more easily burned than a person in good health. DIF: Cognitive Level: Application REF: k 323 OBJ: Theory #1 TOP: Safety KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • An agitated resident who is seated in his wheelchair calls the nurse because the bed linens are smoldering. After moving the patient to the hall, the nurse should: • close the door to the room to confine the fire. ur si ng te st pr ep .c • om falls. DIF: Cognitive Level: Analysis REF: k 322, Box 20-3 OBJ: Theory #3 TOP: Safety KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A diabetic patient has chronic peripheral vascular disease, which results in edema and poor circulation to her feet. She constantly complains of cold legs. The best nursing action is to provide: assess the patient for burns. • extinguish the flames with an appropriate extinguisher. .m yn • activate the fire alarm system immediately. ANS: D RACE is used as an acronym to respond to fire. RACE represents Rescuing the patient from immediate danger, Activating the fire alarm system, Containing the fire by closing doors and windows, and Extinguishing the flames with an appropriate extinguisher. DIF: Cognitive Level: Application REF: k 323 OBJ: Theory #4 TOP: Safety KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • When caring for a patient with acute radiation sickness (ARS) after an accident at an atomic power plant, the nurse should: • wear a paper gown and boots, gloves, and a mask. w w w • • stay in the room and talk to the patient to alleviate anxiety. • decrease the amount of time spent in the room. wear a chemical mask with a filtered respirator. ANS: A For prolonged periods in caring for a patient with ARS, the nurse should use the barrier protection of gown, boots, a mask, and gloves. DIF: Cognitive Level: Application REF: k 325 OBJ: Theory #1 TOP: Safety KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • There is evidence that a resident in a home care environment might have accidentally ingested gasoline left by the gardeners. The nurse should first: • call the family members to notify them of the incident. pr ep .c om • call the poison control center and describe the situation. • induce the patient to vomit. te st • place the gasoline can in a safe place. ANS: B If a nurse suspects gasoline poisoning, it is important to call the poison control center to obtain further instructions. It is also important to prevent vomiting, because this may cause respiratory problems. DIF: Cognitive Level: Application REF: k 326 OBJ: Clinical Practice #1 TOP: Safety KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • A nursing assistant on the day shift reports that he has raised the bed rails to keep an agitated patient from climbing out of bed. The nurses best response to this information is: • Good idea. Be sure to check on the patient every hour to assess the patients comfort. w w w .m yn ur si ng • • A vest protective device will work better; put one on the patient, please. • The rails wont prevent falling; bring the patient out to sit by the nurses station where we can watch • Youll need to check the patient every 15 minutes and reorient the patient as to why the rails are up. ANS: C Seating the patient close to the nurses station will allow the nurse to check on the patient frequently. The nurse needs to get an • instruct the nurses aide to apply a vest restraint. .c obtain an order for a sedative from the physician. ep • om order for a vest restraint. DIF: Cognitive Level: Application REF: k 322, Box 20-3 OBJ: Clinical Practice #6 TOP: Safety KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment • A patient is agitated and confused and keeps getting out of bed and needs to be observed constantly. The best initial nursing intervention is to: • have a family member or friend sit with the patient. make sure the side rails are up and close the door. ANS: A Local and federal laws prohibit the use of physical and chemical restraints except those authorized by a physician. Health care workers are encouraged to find other alternatives such as asking a family member to supervise the patient before resorting to the use of protective devices. DIF: Cognitive Level: Application REF: k 328, Skill 20-3 OBJ: Theory #1 TOP: Safety KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The doctor has written an order to place a resident in the nursing home in a vest protective device. It is the nurses responsibility to: • check with the nursing supervisor about the legality of the order. .m yn ur si ng te st pr • remove the device every 4 hours to toilet the patient. w • remove the device every 2 hours and change the patients position. w • w • apply the device loosely to prevent circulation impairment. ANS: B Changing position helps prevent other complications such as skin decubiti. DIF: Cognitive Level: Comprehension REF: k 327, Box 20-5 OBJ: Theory #6 TOP: Safety KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The physician orders wrist restraints for an agitated patient. To safely use this protective device, the nurse: • checks that circulation is not impaired by evaluating color, warmth, and pulses distal to the device. • secures the ties of the device to the side rails of the bed to allow for easy access by the nurse. • draws the restraint tightly to prevent the patients hands from slipping out. uses a knot that is not easily undone for patient security. ANS: A Checking for signs indicating that circulation has been impaired or skin abraded or for evidence of nerve impairment is part of the nurses responsibility in upholding the principles of the use of protective devices. DIF: Cognitive Level: Application REF: k 327, Protective Devices OBJ: Theory #6 TOP: Safety KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The home health nurse assessing the home for safety hazards notes a hazard that should be remedied is: • an extension cord lying across the floor. st pr ep .c om • non-skid bath mats on the bathroom floor and in the shower. • night-lights high on the wall in the bathroom. te • lack of scatter rugs on the wooden floor. ANS: A Extension cords pose a hazard for falls. The rest of the items assist in the prevention of falls. DIF: Cognitive Level: Application REF: k 322, Box 20-3 OBJ: Theory #1 TOP: Safety KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity • A resident is confused and teary. She is threatening to leave the facility to return home. The nurse should: • call her family immediately and notify them of the problem. w w .m yn ur si ng • have the nurses aide place a vest restraint on the patient. • call the doctor immediately and get an order for a protective device. w • • talk to the patient and attempt to determine the cause of the problem. ANS: D Restraints may not be used without an order or to punish or discipline a patient. Talking to the patient is an excellent strategy to determine the cause of the problem. Medications may also cause mood alterations. DIF: Cognitive Level: Analysis REF: k 328, Skill 20-3 OBJ: Theory #6 TOP: Alternative to Restraints KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse clarifies to the worried family that the guiding principle for using protective devices is: • to use the least amount of immobilization needed for the situation. • to use only immobilization techniques necessary to keep the patient safe. • that protective devices are mandated for behavioral use only. that protective devices must be applied by qualified personnel. ANS: A The principle is derived from local and federal laws and endorsed by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO), which supports restraints only as a last resort. This is because of previous misuse and abuse of these devices by health care personnel. DIF: Cognitive Level: Knowledge REF: k 327, Box 20-5 OBJ: Theory #6 TOP: Safety KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: reduction of risk • Material safety data sheets (MSDS) are required by the Occupational Safety and Health Administration (OSHA). The nurse must: • have a copy of all MSDS on the unit to safely handle biohazards. si ng te st pr ep .c om • know the location of the MSDS and comply with their guidelines. • not handle biohazards identified in the MSDS. ur • keep the MSDS confidential and not discuss them outside the agency. ANS: B MSDS are consulted for recommended methods of storage, labeling, handling spills, and disposal of biohazards. DIF: Cognitive Level: Knowledge REF: k 324 OBJ: Clinical Practice #3 TOP: Environment Management KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A nurse is instructing a nursing student about restraint use. The nurse recognizes the need for further instruction when the nursing student states, I will: • tie the restraints to the side rails to ensure the restraints are secure. w w w .m yn • • use a half-bow knot to secure the restraints to the bed frame. • check the area distal to the restraints every 15 to 30 minutes. • observe for signs of adequate circulation, including distal pulses. The certified nursing assistant (CNA) places a confused, weak patient in a wheelchair and applies a vest protective device. The nurse should instruct the CNA to: (Select all that apply.) • secure the ties in the front to prevent the patient from falling. pr ep • .c om ANS: A Restraint ties should be secured to an immovable part of the bed frame. They should not be tied to the side rails because lowering the rails may cause the device to be pulled too tightly around the patient or cause strain on a joint of an immobilized extremity. A half-bow knot should be used to secure the device to the bed frame or chair. The area distal to the restraint should be checked every 15 to 30 minutes and should be observed for signs of adequate circulation, including pulses distal to the device. DIF: Cognitive Level: Application REF: k 328, Skill 20-3 OBJ: Theory #6 TOP: Restraints KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: basic care and comfort MULTIPLE RESPONSE secure the ties in the back to prevent the patient from falling. • use a double knot to prevent the patient from undoing the tie. • use a half-bow knot to secure the device to a chair. ng te st • provide passive range of motion to the upper extremities as needed. ANS: B, D, E Placing the ties under the armrests and securing at the back will keep the patient from sliding. The half-bow knot makes it difficult for the patient but easy for the health care worker to undo. DIF: Cognitive Level: Application REF: k 328, Skill 20-3 OBJ: Clinical Practice #6 TOP: Safety KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • Legal implications for using a protective device require thorough documentation and require that the nurse include: (Select all that apply.) • alternative methods and actions used. w w w .m yn ur si • • medications that the patient is taking. • teaching done for patient and family. • the patients medical diagnosis. • type of devic e and st pr ep .c om place ment . ANS : A, C, E The nurse should document alternative methods and actions taken before placing the device, the teaching done for both patient and family, and the type of device used and where it was placed. Remember, if it is not documented, it was not done. DIF: Cognitive Level: Knowledge REF: k 328, Skill 20-3 OBJ: Theory #7 TOP: Safety KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk • Each resident admitted must have a fall risk assessment performed so that appropriate actions to prevent falls can be included in the nursing care plan. The items are considered when doing a fall risk assessment on a newly admitted resident include: (Select all that apply.) • gender. age. • weight. • medications. ng te • yn ur si • balance. ANS: B, D, E The common factors that predispose a person to falls may include age, the type of medications the resident is taking, and physical mobility. w w w .m Chapter 20 Pain Management M U L T I P L E C H O I C E • The nurse assesses a patients sleep for NREM (non-rapid-eyemovement) sleep because this sleep has the characteristics of: • daytime activity. • offering the most rest. • irregular respirations. w w w .m yn ur si ng te st pr ep .c i n c r e a s e d h e a r t r a t e . A N S : B NREM sleep is the stage of sleep when the body receives the most rest. DIF: Cognitive Level: Comprehension REF: k 605 OBJ: Theory #5 TOP: NREM Sleep KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient experiencing discomfort because of severe arthritis would be described as having pain. • acute om • • chronic • phantom • episodic ANS: B Chronic pain is pain in which symptoms are controlled, but there is no cure, such as in arthritis. DIF: Cognitive Level: Comprehension REF: k 591 OBJ: Clinical Practice #2 TOP: Types of Pain KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient is beginning treatment for pain with a transcutaneous electrical nerve stimulator (TENS) unit. The nurse will initially: • apply conductive jelly to un-coated electrodes. • turn the unit on before attaching it to the patient. • place electrodes on all four extremities. adjust the settings below the level at which a tingling sensation is felt. ANS: A Conductive jelly is applied to electrodes that are not precoated to assure conductivity. DIF: Cognitive Level: Application REF: k 597, Skill 30-1 OBJ: Clinical Practice #4 TOP: TENS KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The patient with a recent abdominal incision has an abdominal binder applied. The nurse explains that this appliance helps reduce pain by: • increasing warmth to the incision site. te st pr ep .c om • keeping sutures and staples in place. • supporting surface and internal tissues. si ng • adding back support to enhance early ambulation. ANS: C Binders are cloths wrapped around a limb or body part that have an incision and are effective in reducing pain associated with strains, sprains, and surgical incisions by providing support to the surface of the area as well as the internal tissues. DIF: Cognitive Level: Comprehension REF: pp. 595-596 OBJ: Clinical Practice #4 TOP: Pain Control KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse evaluating the effectiveness of an Aquamatic K-pad for the leg is aware that the patient who has the least risk for burn injury from this device would be the patient with: • impaired peripheral circulation. w w w .m yn ur • • severely sprained ankle. • decreased level of consciousness from a stroke. • neuri tis secon st pr ep .c om dary to diabe tes. ANS: B Patients with poor circulation, impaired movement or feeling, or decreased level of consciousness are more at risk for injury from burns when applications of heat are used. DIF: Cognitive Level: Analysis REF: k 597, Skill 30-1 OBJ: Clinical Practice #4 TOP: Heat Application KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A nurse caring for a patient who suffered a severe sprain and has an order for a cold pack application to the injured area would prevent patient injury by: • using heavy pressure on the cold pack for greater effectiveness. preparing to apply heat instead if cold is not effective. • leaving the pack in place for over 30 minutes at a time. te • placing a towel between the pack and the skin. ANS: D A protective towel or pad should be placed between the pack and the skin to avoid cold injury. DIF: Cognitive Level: Application REF: k 598 OBJ: Clinical Practice #4 TOP: Cold Application KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A nurse is instructing a patient about relaxation techniques for pain management. The patient should: • keep bright lights on in the room. use this technique as a way to wake up in the morning. w • w .m yn ur si ng • tense and relax individual muscle groups, starting with the toes and feet. • try to tense and relax all of the muscles of the body at the same time. ANS: C w • Relaxation involves alternately tensing and relaxing the toes and feet, then working upward through the leg, the abdomen, the chest, the arms, and finally, the neck and head. DIF: Cognitive Level: Comprehension REF: k 598 OBJ: Theory #4 TOP: Relaxation KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A patient is receiving an ice massage for relief of muscle spasms in the neck. The patient complains that the ice is making the pain worse. Most helpful response from the nurse would be: • I know it is uncomfortable right now , but is will get better in a few minutes. • I will go get an ice pack to pace on your neck. • The alteration of hot and cold application is very helpful for your spasms. I will stop these cold applications. Not everyone is helped by them. ANS: D Cold applications make some patients experience an increase in discomfort. DIF: Cognitive Level: Analysis REF: k 598 OBJ: Theory #4 TOP: Ice Application KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient experiencing pain states that guided imagery has made the pain more manageable in the past. To assist this patient, the nurse should: • find a focal point in the room. st pr ep .c om • bring a newspaper or deck of cards according to patient choice. • obtain skin lotion and a towel to give a back rub. ng te • read from a script that helps the patient visualize a restful place. ANS: D Persons who have difficulty with imagery can be assisted by someone reading a script to help a patient mentally travel to a favorite spot that is relaxing, soothing, or peaceful. DIF: Cognitive Level: Application REF: k 599 OBJ: Theory #4 TOP: Imagery KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: basic care and comfort • The nurse takes into consideration that when the patient has an order for a patient controlled analgesia (PCA) the pump will be programmed by the: • registered nurse. w w w .m yn ur si • • physician. • LPN/LVN. • p h a r m Cox-2 inhibitor. w • w .m yn ur si ng te st pr ep .c om a c e u t i c a l c o m p a n y . A N S : A PCA pumps are programmed by the RN or the pharmacist. The physicians order will specify the size of the dose and the minimum time between doses. DIF: Cognitive Level: Knowledge REF: k 601 OBJ: Theory #4 TOP: Chiropractic KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse is aware that the new order for indomethacin (Indocin) involves the administration of a: adjuvant analgesic. • narcotic analgesic. w • • nonsteroidal antiinflammator y drug. ANS: D Indomethacin is a nonsteroidal anti-inflammatory drug (NSAID) which requires a prescription. DIF: Cognitive Level: Knowledge REF: k 600, Table 31-2 OBJ: Clinical Practice #4 TOP: Indomethacin KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: pharmacological therapies • The nurse appreciates the principal advantage in using patientcontrolled analgesia (PCA) is that it: • reduces patient anxiety about pain by giving the patient more control in its management. • reduces the workload of the nurse, because it does not have to be checked often. • eliminates the risk of adverse drug effects from the medication. completely eliminates any pain the patient is experiencing. ANS: A A principal advantage of PCA is that it reduces anxiety about pain, because patients are in control of their pain medication within machine-set limits. DIF: Cognitive Level: Comprehension REF: k 601 OBJ: Clinical Practice #5 TOP: PCA KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse caring for a patient with a Fentanyl patch assesses that the patient is abnormally sleepy, is slurring words and is unsteady when ambulating. The nurse should: • put up the side rails on the bed. ng te st pr ep .c om • elevate the head of the bed 45 degrees and offer coffee or cola drink. • remove the patch and wipe off the skin. ur si • apply ice to skin around the patch. ANS: C When overdose signs occur with Fentanyl patches, the patch should be removed, the skin cleansed and the problem documented and reported to the charge nurse or physician. DIF: Cognitive Level: Application REF: k 601, Safety Alert OBJ: Clinical Practice #6 TOP: Fentanyl Patch KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies • A nurse is assisting in the care of a patient who is receiving pain medication by the epidural route. It is most important to monitor this patient for which adverse drug effects? • Constipation w w w .m yn • • Headache • Nausea • w w w .m yn ur si ng te st pr ep .c om H y p o v e n t i l a t i o n A N S : D Respiratory depression is a potentially dangerous side effect of epidural analgesia, and a patient receiving this type of pain medication requires frequent monitoring of respiratory rate. DIF: Cognitive Level: Comprehension REF: k 604, Steps 31-1 OBJ: Clinical Practice #6 TOP: Epidural Pain Control KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies • A patient with an epidural catheter needs to have the dressing at the insertion site changed. When cleaning the insertion site with povidone-iodine swabs, the nurse should: • use a circular motion working from the insertion site outward. • use a circular motion working from the outside to the insertion site. • start above the insertion site and swab in a downward motion. • start below the insertion site and swab in an upward motion. ANS: A Proper aseptic technique includes starting at the center (the insertion site) and working outward using a circular motion. DIF: Cognitive Level: Application • Rapid respirations, slow heart rate • Decreased respirations, slow heart rate om REF: k 604, Steps 31-1 OBJ: Clinical Practice #5 TOP: Epidural Catheter KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A nurse is assessing the status of a patient who is sleeping. Which assessment data indicate that the patient is most likely in stage 3 of nonrapid eye movement (NREM) sleep? • Rapid respirations, rapid heart rate Decreased respirations, rapid heart rate ANS: C Stage 3 of NREM sleep, in which respirations and heart rate slow, is similar to a coma; it is also called delta sleep or slow-wave sleep because of the high-voltage slow brain waves that occur. DIF: Cognitive Level: Comprehension REF: k 604 OBJ: Theory #7 TOP: Sleep KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse recommends that normal sleep patterns can best be acquired by suggesting to the patient that they: • smoke cigarettes. si ng te st pr ep .c • drink wine. • take a nap during the day. w w w .m e x e r c i s e i n t h e m o r n yn • ur • • narcolepsy. te sleep apnea. ng • st pr ep .c DIF: Cognitive Level: Comprehension REF: k 604 OBJ: Theory #8 TOP: Sleep KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A sleeping patient has periodic pauses in breathing, then starts to breathe again. The nurse recognizes this sleep pattern is consistent with: • insomnia. om i n g s . A N S : D Maintaining a regular exercise schedule not too close to bedtime helps a person sleep. w w ur yn w .m e x c e s s i v e N R E M s l e e p . A N si • om S : B Sleep apnea is a condition in which the person stops breathing for brief periods during sleep. DIF: Cognitive Level: Analysis REF: k 606 OBJ: Theory #8 TOP: Sleep KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The suggestion by the nurse which is most helpful to a patient who complains of chronically not feeling rested after sleep would be: • avoid going to bed hungry or overly full. try to exercise just before going to bed. • sleep late the next morning if possible if you are tired on awakening. ep .c • take a nap during the day to help relieve overall fatigue. ANS: A Going to bed hungry or with a full stomach can interfere with sleep. DIF: Cognitive Level: Application REF: k 606 OBJ: Clinical Practice #8 TOP: Sleep Disturbances KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The most helpful intervention by the nurse for a hospitalized child who is having difficulty falling asleep would be: • keeping a night light on in the room. yn ur si ng te st pr • turning off all of the lights in the room. • having the parents bring a favorite blanket or pillow from home. .m • giving of juice and cookies before being put to bed. ANS: C Many patients sleep better when they can have a favorite blanket or pillow from home. DIF: Cognitive Level: Application REF: k 607 OBJ: Clinical Practice #8 TOP: Sleep KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient who has difficulty falling asleep at night because of anxiety over family problems asks if he should start taking sedative pills from the pharmacy to sleep better. The best advice to give this patient is that these pills can be used for: • long periods of time, but it is best to check with the physician first. w w w • • short periods of time, but it is best to check with the physician first. • long periods of time without physician approval, because they are nonprescription drugs. short periods of time without physician approval, because they are nonprescription drugs. ANS: B Sedative and hypnotic medications can be used to promote sleep, but they should be used for short-term relief and only after a physician has been consulted. DIF: Cognitive Level: Comprehension REF: k 607 OBJ: Clinical Practice #8 TOP: Sleep KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: pharmacological therapies • A natural supplement that can enhance sleep for many people is: • melatonin. • magnesium. ep calcium. pr • .c om • st • w w w .m yn ur si ng te o i l o f l a v e n d e r . A N S : A Melatonin, a natural supplement can enhance sleep hours for many people. Calcium and magnesium are used to relieve leg cramps. DIF: Cognitive Level: Knowledge REF: k 607, Sleep aids OBJ: Clinical Practice #8 TOP: Natural Sleep Aid KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The nurse takes into consideration The Joint Commission (TJC) standards for pain assessment and treatment include: • pain treatment is based on objective data collected by the nurse. • pain treatment ends at discharge. • pain is assessed only for patients who complain of pain. all patients have the right to appropriate assessment of pain. ANS: D The TJC standards related to pain state that all patients have a right to appropriate assessment and management of pain and should be educated in the process prior to discharge. DIF: Cognitive Level: Knowledge REF: k 590 OBJ: Theory #1 TOP: JCOAH KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • A relative complains that an elderly patient takes frequent naps during the day and awakens frequently during the night, and wants to know if this is normal. The nurse explains that an older adult: • will awaken more often during the night, but may nap more often during the day. st pr ep .c om • needs at least 10 hours of sleep a day to prevent fatigue. • requires less napping during the day to sleep better at night. ng te • should be given hypnotics to induce better sleep. ANS: A Sleep habits are very individualized, but normally, as an adult ages, sleep may be less at night with more naps being taken during the day. yn ur si • w w w .m DIF: Cognitive Level: Comprehension REF: k 605 OBJ: Theory #6 TOP: Sleep Needs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse explains that endorphins are capable of reducing pain: • as a naturally occurring morphine like enzyme. • in conditions that are physiological only. • by attaching to opioid receptors. • when psychological stressors are the cause of pain. ANS: C Endorphins are naturally occurring opiate like peptides which attach to the opioid receptors of nerve endings and bock pain transmission. Endorphins are effective against both physiologically and psychologically causes pain. DIF: Cognitive Level: Comprehension REF: w w w .m yn ur si ng te st pr ep .c om k 591 OBJ: Theory #4 TOP: Endorphins KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort COMPLETION is considered to • be the fifth vital sign. ANS: Pain Pain assessment is now performed along with each assessment of vital signs, and pain is now considered the fifth vital sign. DIF: Cognitive Level: Knowledge REF: k 590 OBJ: Theory #2 TOP: Pain KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A type of pain that is of short duration, lasting from a few hours to a few days, is known as pain. ANS: acute Acute pain is of short duration, lasting from a few hours to a few days. DIF: Cognitive Level: Knowledge REF: k 591 OBJ: Clinical Practice #2 TOP: Pain KEY: Nursing Process Step: Assessment MSC: NCLEX: N/A • The is the theory that by stimulating large diameter nerve fibers pain is diminished or totally controlled. ANS: Gate Theory The Gate Theory is based on the premise that by stimulating large diameter nerve fibers by massage or vibration the gate to pain perception is closed against the pain impulses from the small diameter nerve fibers. DIF: Cognitive Level: Knowledge REF: k 591 OBJ: Theory #3 TOP: Gate Control Theory KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A pain scale FLACC is used in . ANS: assessing pain in infants FLACC stands for Face, Legs, Activity, Cry and Consolability. Which are assessed to estimate the pain in pre-verbal infants. DIF: Cognitive Level: Knowledge REF: k 594 OBJ: Clinical Practice #1 TOP: Pain in Infants KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort Travelers can combat jet lag by exposure to for several hours. ANS: sun sunlight Exposure to sunlight for several hours will help reset a travelers internal clock and reduce the effects of jet lag. DIF: Cognitive Level: Comprehension REF: k 605 OBJ: Clinical Practice #6 TOP: Jet Lag KEY: Nursing Process Step: Assessment MSC: NCLEX: N/A • A nurse removed a pain medication patch that has a metal clip before the patient goes to have a(n) . ANS: MRI magnetic resonance imaging All metal must be removed from persons who are going to have a MRI. DIF: Cognitive Level: Application REF: k 601 OBJ: Theory #4 TOP: MRI Consideration KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: safety and infection control MULTIPLE RESPONSE • The nurse outlines the four phases of nociceptive pain as: (Select all that apply.) • translation. transmission. • modulation. w w w .m yn • p e r c e p t i o n . A N S : B , C ng • si transduction. ur • te st pr ep .c om • believe pain is a natural consequence to aging. • are reluctant to bother the nursing staff. • have been culturally trained not to complain. pr w w w .m yn ur si ng te st • fea r tak ing pai n me dic ati on. A NS : B, C, D ep • .c om , D , E The four phases of nociceptive pain are transduction, transmission, perception and modulation. DIF: Cognitive Level: Comprehension REF: k 593 OBJ: Clinical Practice #1 TOP: Nociceptive Pain KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse attempts to help an 86 year old patient describe his pain because the nurse is aware the elderly do not express pain because they:(Select all that apply.) • are unaware of their discomfort. The elderly often do not verbalize their pain out of the mistaken belief that pain is part of aging. They are reluctant to bother the staff and have been culturally trained not to complain. DIF: Cognitive Level: Comprehension REF: k 593 OBJ: Clinical Practice #1 TOP: Pain in the Elderly KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse performing a focused assessment on pain will assess: (Select all that apply.) • history of pain. • verbal indicators. • psychological factors. • culture. • w w w .m yn ur si ng te st pr ep .c om c o n t r i b u t i n g f a c t o r s . A N S : A , B , C , E Factors to be assessed in a focused assessment of pain is the history, verbal and non-verbal indicators, psychological and other contributing factors, medication and treatments used . Although culture may limit a person’s ability to express pain, it is not an important issue on a focused assessment. Chapter 21 Oxygenation M U L T I P L E C H O I C E • The nurse uses a diagram to show that when the diaphragm moves: • up, the increased negative pressure in the thoracic space forces air into the lungs. down, the intercostal muscles retract, forcing air out of the lungs. • down, the negative pressure in the thoracic space pulls air into the lungs. om • up, the decreased negative pressure allows air to enter the lungs. ANS: C When the diaphragm moves down, increasing the size of the thoracic space, air is pulled into the lungs. The respiratory action is controlled by the spinal cord. DIF: Cognitive Level: Knowledge REF: k 501 OBJ: Theory #1 TOP: Respiratory Action KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse clarifies that the condition in which there is a decreased amount of oxygen in the blood is: • hypoxia. hypercapnia. • dyspnea. .m yn • w w w • h y p o x e m i a . A N S ur si ng te st pr ep .c • : D pr ep .c om Hypoxemia is a condition in which there is a decreased amount of oxygen in the blood, hypoxia is inadequate oxygen to meet cellular needs, hypercapnia is increased level of carbon dioxide in the blood, and dyspnea is difficulty breathing. DIF: Cognitive Level: Comprehension REF: k 503 OBJ: Theory #1 TOP: Oxygen Levels KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse monitoring patients eating in the dining room of a skilled nursing facility notes that a patient begins choking. As the nurse prepares to deliver the Heimlich maneuver, the fist should be positioned: • halfway between the xiphoid process and the umbilicus. directly over the sternum. • between the umbilicus and the symphysis pubis. st • te • w w w .m yn ur si ng dir ect ly ov er th e u m bil ic us. A N S: A Proper placement of the fist is halfway between the xiphoid process and the umbilicus. DIF: Cognitive Level: Application REF: k 507, Skill 28-2 OBJ: Clinical Practice #1 TOP: Heimlich Maneuver KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient has collapsed and cannot be aroused by asking loudly, Are you okay? The next action should be to: • position the fingers over the carotid artery to feel for a pulse. • tilt the head by placing one hand on the forehead and lift the chin. • call for help or, if there is assistance, have that person get help. deliver two quick short breaths into the patients airway. ANS: C The sequence for resuscitative interventions is to check for responsiveness; if no response, activate emergency medical services, check for pulse at carotid, begin compressions, then open the airway and check for breathing. DIF: Cognitive Level: Application REF: k 509, Skill 28-3 OBJ: Theory #3 TOP: Basic Life Support KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • The nurse instructing the patient to perform forceful exhalation coughing would teach the patient to take in: • one deep breath and quickly exhale. st pr ep .c om • two breaths and force the air out quickly. • two deep breaths, then inhale deeply again and force out the air quickly. • one breath, hold it for 3 seconds, then forcefully exhale three times with mouth open. ANS: C si ng te • w w w .m yn ur Proper coughing procedure is to take in two deep breaths, inhale deeply again and to forcibly exhale (cough) at the end of the third breath. This technique is very effective in moving secretions up the bronchial tree. DIF: Cognitive Level: Knowledge REF: k 511 OBJ: Clinical Practice #1 TOP: Effective Coughing KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse is aware that the best time to schedule a postural drainage treatment is: • shortly after the patient arises in the morning, before breakfast. • in the morning immediately after breakfast. • 30 minutes after lunch. • 1 h o yn ur si ng te st pr ep .c om u r a f t e r s u p p e r . A N S : A Postural drainage is best accomplished in the morning prior to eating, because more secretions accumulate while the patient is asleep. DIF: Cognitive Level: Comprehension REF: k 511 OBJ: Clinical Practice #1 TOP: Postural Drainage KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient who will begin oxygen therapy has a history of sinus disorders. This patient would benefit most from which oxygen setup? • High oxygen flow rate A humidifier • A Venturi mask w .m • w • w A n a s a l c a n n u • 2 to 3 • 1 to 2 st 4 to 5 te • pr ep .c om l a A N S : B If a patient suffers from sinus problems, it is best to add a humidifier to the oxygen setup. DIF: Cognitive Level: Application REF: k 514, Table 28-4 OBJ: Clinical Practice #2 TOP: Oxygen Therapy KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient has a history of chronic obstructive pulmonary disease. The patients oxygen flow rate should be set to no more than L/min. • 5 to 10 .m yn ur si ng ANS: C Patients with obstructive lung disease are given only 2 to 3 L/min of oxygen, because over time they adjust to high carbon dioxide levels, and their stimulus to breathe comes from low arterial oxygen levels. Higher amounts of oxygen could reduce or eliminate the respiratory drive. DIF: Cognitive Level: Comprehension REF: k 514, Safety Alert OBJ: Theory #5 TOP: Oxygen Therapy KEY: Nursing Process Step: Implementation w w w MSC: NCLEX: Physiological Integrity: reduction of risk • The nurse loosens mucus plugs by using percussion on a patient over the area of the: • sternum. • thorax. • spine between the scapulae. • midaxi llary line on the rib cage. ANS: • A partial rebreathing mask .c A non-rebreather mask ep • om B Percussion, a rhythmic clapping with cupped hands over the thoracic area, will loosen mucus plugs. This technique is both useless and painful when applied over bony areas. DIF: Cognitive Level: Knowledge REF: k 511 OBJ: Clinical Practice #1 TOP: Oxygen Therapy: Percussion KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • A patient requires a precise concentration of 40% oxygen. Which of the following devices would best allow for this? • A simple face mask • w w w .m yn ur si ng te st pr A V e n t u r i m a s k A N S : D A Venturi mask is useful when accuracy of delivery is essential. DIF: Cognitive Level: Comprehension REF: k 517, Table 28-3 OBJ: Clinical Practice #2 TOP: Oxygen Therapy: Venturi Mask KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse recognizes that a post-operative patient who can breathe independently but has trouble maintaining an airway because of the tongue falling back into the throat would be best benefited by a(n): • pharyngeal airway. • endotracheal tube. • tracheostomy. partial rebreat her oxyge n mask. ANS: A A pharyngeal airway such as a nasopharyngeal or an oropharyngeal airway is useful for patients who can breathe on their own but tend to occlude the airway with the tongue. DIF: Cognitive Level: Analysis REF: k 516 OBJ: Theory #4 TOP: Airway KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • A nurse performing oral suctioning on an adult patient should set the wall suction machine so that the suction pressure is between mm Hg. • 25 and 50 • 80 and 120 ng 50 and 75 si • te st pr ep .c om • ur d. w w w .m yn 12 0 an d 18 0 A N S: C The range of suction pressure for an adult patient is between 80 and 120 mm Hg. DIF: Cognitive Level: Application REF: k 517, Table 28-3 OBJ: Clinical Practice #1 TOP: Suctioning KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse caring for a patient with a tracheostomy should determine whether the patient needs suctioning by: • monitoring the rate of respirations. • determining the last time the patient was suctioned. • examining the character of the sputum. • si ng te st pr ep .c om auscu ltatin g the breath sound s. ANS: D Auscultating the patients breath sounds helps the nurse assess for retained secretions and verifies the need for suctioning. The respiratory rate may rise when suctioning is needed, but it could also rise for other reasons. DIF: Cognitive Level: Application REF: k 526, Skill 26-6 OBJ: Clinical Practice #1 TOP: Suctioning KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient requires suctioning via the nasotracheal route. In order to perform this procedure safely, the nurse should: • apply suction while advancing the catheter into the airway. suction the nasotracheal passage after suctioning the mouth. • hold the catheter with the dominant hand after donning sterile gloves. yn ur • insert the non-lubricated catheter into the nasal passage. ANS: C The suction catheter should be held with the dominant hand after donning sterile gloves, because sterile technique must be adhered to when suctioning both the nasopharyngeal and tracheal areas. DIF: Cognitive Level: Application REF: k 526, Skill 26-6 OBJ: Clinical Practice #1 TOP: Suctioning KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse recognizes that, immediately before a tracheotomy cuff deflation, the patient should: • be administered extra oxygen. w w w .m • • have the pharynx suctioned. • have the cuff pressure checked. be monitored for respiratory rate. ep .c ANS: B Immediately before deflating a cuff on a tracheotomy tube, the pharynx should be suctioned to prevent accumulated oral secretions from entering the bronchial tree once the cuff is deflated. DIF: Cognitive Level: Application REF: k 527, Skill 28-6 OBJ: Clinical Practice #3 TOP: Tracheostomy KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk • The nurse takes into consideration that while caring for a patient on oxygen therapy, safety precautions should be observed, which include: • using clothing of synthetic cloth for the patient. om • removing any adhesive from the patients skin with acetone. • assessing equipment in room for frayed cords. st pr • reducing humidification on the oxygen delivery device. ANS: C All equipment in a room where oxygen is being administered should be in good working order without frayed or loose connections because of the possibility of fire. DIF: Cognitive Level: Comprehension REF: k 514, Safety Alert OBJ: Clinical Practice #5 TOP: Safety Precautions with Oxygen KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A nurse caring for a patient with a water seal type chest drainage that is on low suction assesses that there is constant bubbling in the suction container. The nurse should: • immediately turn the patient to the side of the insertion site. w w w .m yn ur si ng te • • check for air leaks in drainage system. • include findings in documentation. • clamp the chest tube and place the patient in high Fowlers position. ANS: C Document findings. Constant bubbling in the suction chamber indicates that suction is on. DIF: Cognitive Level: Analysis REF: k 531, Steps 28-1 OBJ: Clinical Practice #4 TOP: Coughing and Deep Breathing KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse is aware that adequate hydration is necessary to mobilize respiratory secretions. To thin respiratory secretions for easier expectoration, the patient should consume at least mL/day. a. 500 to 1000 b. 1000 to 1500 c. 1500 to 2000 d. te st pr ep .c om 25 00 to 300 0 AN S: C A fluid intake of at least 1500 to 2000 mL/day is needed to thin respiratory secretions for easier removal by coughing. yn ur si ng DIF: Cognitive Level: Comprehension REF: k 522 OBJ: Clinical Practice #1 TOP: Mobilizing Secretions KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse would determine that this patient is aware of how to use the incentive spirometer device properly when the patient: • took 10 slow, deep breaths every hour. took five quick huffs and then coughed vigorously. • exhaled deeply and then inhaled quickly and forcefully three times. w took five deep breaths slowly every 4 hours. ANS: A Proper technique for use of an incentive spirometer is to take 10 slow, deep breaths every hour and to hold each breath for 3 seconds to enhance gas exchange. DIF: Cognitive Level: Knowledge REF: k 524 OBJ: Clinical Practice #1 TOP: Incentive Spirometer KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse assists the patient with emphysema into the most beneficial position to facilitate respiration, which is: w w • .m • • semi-Fowlers position with a single pillow behind the head. • high Fowlers position without a pillow behind the head. • right lateral with the head of the bed elevated 45 degrees. sitting upright and forward with arms supported on an over-the-bed table. ANS: D Sitting upright and leaning forward with arms supported on an over-the-bed table is best for this patient, because it allows for expansion of the thoracic cage in all four directions (front, back, and two sides). DIF: Cognitive Level: Application REF: k 524, Figure 28-20 OBJ: Clinical Practice #1 TOP: Positioning KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse performing tracheotomy care will: • raise the head of the bed to high Fowlers position. ep .c om • remove the inner cannula with the ungloved hand. • suction tracheotomy before beginning care. st pr • clean cannula with gauze and replace and lock. ANS: C Proper procedure includes suctioning the tracheotomy before beginning care. DIF: Cognitive Level: Application REF: k 528, Skill 28-7 OBJ: Clinical Practice #3 TOP: Tracheotomy Care KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse caring for a patient with a disposable chest drainage system can promote effective tube function and patient safety by: • taping all connections within the system. keeping the system at the level of the patients chest. w • w .m yn ur si ng te • w • • turning on suction to 35 cm. looping the tubing between the mattress and the bed rail to minimize length. ANS: A All connections in the system should be taped. Suction should be set at 20 cm unless ordered otherwise. Looping the tubing encourages plugs in the tubing. DIF: Cognitive Level: Application REF: k 531, Steps 28-1 OBJ: Clinical Practice #4 TOP: Chest Tube Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk • The nurse takes into consideration that a pulse oximeter may not give an accurate reading if the patient is: • dark skinned. • jaundiced. • obese. ep .c om • febrile. ANS: B An accurate reading is dependent on light passing through the vascular bed. Jaundice may cause an inaccurate reading. DIF: Cognitive Level: Knowledge REF: k 505 OBJ: Theory #1 TOP: Pulse Oximetry KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse clarifies that the cough mechanism is stimulated when: • foreign substances are propelled by the cilia toward the respiratory tract. dehumidified air enters the upper airway passages. • more than 250 mL of air moves in and out of the lungs with each breath. st pr • the blood transports carbon dioxide to the lungs. ANS: A Cilia work to propel foreign substances toward the entrance of the respiratory tract, and the cough reflex works to expel the secretions. DIF: Cognitive Level: Knowledge REF: k 502 OBJ: Theory #1 TOP: Respiratory Structure Function KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • When assessing the lungs of a patient, the nurse assesses a wheezing sound on inspiration. This finding is documented as: • apnea. stridor. w • dyspnea. w • .m yn ur si ng te • w • retractions. ANS: C Stridor is a wheezing sound that can be heard on auscultation or even with the naked ear and indicates respiratory obstruction. DIF: Cognitive Level: Knowledge REF: k 503 OBJ: Theory #1 TOP: Stridor KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation COMPLETION • A sputum specimen is best obtained just after the patient o r w w w .m yn ur si ng te st pr ep .c om after a treatment because this is when there is more mucus available or when it is easier to cough up. ANS: awakens, nebulizer A sputum specimen is best obtained just after the patient awakens or after a nebulizer treatment because this is when there is more mucus available or when it is easier to cough up. DIF: Cognitive Level: Application REF: k 510, Patient Teaching OBJ: Clinical Practice #1 TOP: Specimen Collection KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • When obtaining a sputum specimen, the nurse should provide the patient with a sterile sputum cup and teach the . patient to rinse her mouth with ANS: water When obtaining a sputum specimen, the nurse should provide the patient with a sterile sputum cup and teach the patient to rinse her mouth with water. DIF: Cognitive Level: Application REF: k 510, Patient Teaching OBJ: Clinical Practice #1 TOP: Specimen Collection KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse explains that the rate of respiration is triggered when the medulla senses a change in the level of ions in the blood. ANS: hydrogen When there is an increase in hydrogen ions in the blood (pH), the medulla signals the spinal nerves to increase and deepen respirations. A drop in the pH reverses the process causing a slowing of the respirations. DIF: Cognitive Level: Knowledge REF: k 502 OBJ: Theory #1 TOP: pH Effect on Respiration KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse administering cardiopulmonary resuscitation (CPR) would administer chest compressions at the rate of compressions/minute. ANS: 100 The CPR guidelines require that there be 100 chest compressions/minute DIF: Cognitive Level: Knowledge REF: k 502, Skill 28-3 OBJ: Theory #3 TOP: CPR KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk MULTIPLE RESPONSE • When a patient with a tracheostomy tube is taken care of at home by family, tracheostomy care instructions from the nurse include: (Select all that apply.) • use sterile gloves during suctioning. • avoid going to crowded theaters and malls. • change catheters every 8 hours. • keep the home environment free of dust. use bleach to clean suction equipment. ANS: B, C, D, E The patient should avoid crowded places to decrease the chance of respiratory infections; use household bleach, hydrogen peroxide, or soap and water to clean equipment; change catheter every 8 hours; and maintain the home environment free of air pollutants to decrease irritation to airway passages. DIF: Cognitive Level: Comprehension REF: k 532, Home Care OBJ: Clinical Practice #3 TOP: Home Care of Tracheostomy Patient KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse is aware that changes occur in the respiratory system after the age of 70 that put the elderly more at risk for respiratory problems. These changes include: (Select all that apply.) • decreased oxygen saturation. increased elasticity in thorax and respiratory tissues. • incomplete expirations. • thinning of alveolar membrane. w w .m • w • yn ur si ng te st pr ep .c om • i m p a i r e d c i l i a . pulmonary fibrosis. • hiccoughs. w w w .m yn ur • h i g h a l t i t u d e . A N S : B , te • ng aspirated vomit. si • st pr ep .c om AN S: A, C, E After the age of 70, changes in the respiratory system that put the elderly at risk for respiratory disorders are decreased oxygen saturation and elasticity of the thorax and respiratory tissues, incomplete respirations, thickening of the alveolar membranes, impaired cilia, and a lessened respiratory reserve. DIF: Cognitive Level: Comprehension REF: k 502 OBJ: Theory #1 TOP: Age-Related Changes KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: physiological adaptation • The multiple causes for hypoxia include: (Select all that apply.) • extreme fright. increase fluid intake. • place the patient in isolation. .c • om C , E Among the many causes of hypoxia are aspirated vomit, pulmonary fibrosis, and high altitude. Chapter 22 Infection Control When the patient complains of vague symptoms of malaise and fatigue and has a low grade fever, but has no other specific signs of illness, the nurse suspects that this patient is in the prodromal phase of infection (the time immediately before the illness is diagnosed). The nurse should include in the plan of care to: • increase assessment for specific signs of illness. report findings to the Infection Preventionist Officer. ANS: A The nurse should increase observation and assessments for specific signs of illness during the prodromal phase of infection. DIF: Cognitive Level: Application REF: pp. 234-235 OBJ: Theory #1 TOP: Stages of Infection KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse is aware that the patient most at risk for a health care-associated infection (HAI) would be the: • 45-year-old in traction for a fractured femur. ur si ng te st pr ep • 56-year-old with pneumonia who is receiving oxygen by mask. • 65-year-old with a Foley catheter. .m yn • 70-year-old with congestive heart failure attached to a monitor. ANS: C Patients with incisions, IV lines, urinary catheters, and other invasive procedures are more likely to develop a health care-associated infection (HAI). DIF: Cognitive Level: Analysis REF: k 235 OBJ: Theory #2 TOP: Health Care-Associated Infections KEY: Nursing Process Step: Assessment w w w • MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The most effective part of infection control to reduce the incidence of health care-associated infections (HAIs) is to: • use surgical asepsis for care of patients outside the operating room who are most at risk for a HAI. • put all patients with wounds or invasive procedures on transmission-based precautions before they • place an alcohol-based hand sanitizer solution in every patient room. • use proper hand hygiene before and after caring for any patient, before donning gloves and after the ANS: D Proper hand hygiene is the single most important aspect of medical asepsis and infection control. DIF: Cognitive Level: Application REF: k 237 OBJ: Theory #2 TOP: Infection Control KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse cautions that a person in the incubation period of an infection: • has identifiable signs of a specific illness. can transmit the disease although he or she does not feel ill. • will seek medical attention for the relief of symptoms. will always exhibit symptoms within 48 hours. ANS: B During the incubation period, patients can transmit the disease, although they dont have identifiable symptoms. The incubation period varies depending on the microorganisms. DIF: Cognitive Level: Comprehension REF: k 235 OBJ: Theory #1 TOP: Infection Control KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse clarifies that the difference between the use of earlier types of isolation procedures and the use of current Standard Procedures plus Transmission-Based Precautions as outlined by the CDC is: • that new diseases have continued to appear for which the older isolation techniques were ineffectiv yn ur si ng te st pr ep .c • om • complicated and hard to follow. w • w .m based on the premise in the new procedures that all body substances except sweat may be infectious • person is not known to have a specific disease. based on newer knowledge of how HIV is spread, to better protect health care workers from blood- ANS: B Earlier Universal Precautions and Isolation Precautions focused on preventing the spread of blood-borne pathogens and secretions or excretions of a person specifically known to be infected. They have been replaced with Standard Precautions for all patients, and Transmission- Based Precautions for those specifically infected, because of the understanding that infection may be present in body secretions or excretions even when the person is apparently healthy. DIF: Cognitive Level: Comprehension REF: k 235 OBJ: Theory #3 TOP: History of Infection Control KEY: Nursing Process Step: Planning w • MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A patient who has active primary tuberculosis is placed on Airborne Precautions. In addition to observing Standard Precautions for this patient, the nurse expects that: the patient can be in a room with a roommate, if both persons wear masks. • a special particulate filter mask (respirator) will be worn by anyone entering the room. • the patient may leave the room freely as long as the patient wears a mask at all times. om • no mask is needed unless performing close-contact nursing care. ANS: B An N95 particulate filter respirator is worn by anyone entering the room of a patient with primary tuberculosis. A private room is preferred. The patient should leave the room only for essential activities (with a mask). DIF: Cognitive Level: Application REF: k 239, Box 17-3 OBJ: Theory #5 TOP: Infection Control KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse performing a surgical scrub is aware that the average time for the scrub is minutes. • 3 6 • 7 si • ur 5 yn • ng te st pr ep .c • w w w .m ANS: A The average length of time required for a surgical scrub will differ with the antimicrobial solution used and the agency policy, but the average is 2 to 4 minutes. DIF: Cognitive Level: Knowledge REF: k 244 OBJ: Theory #3 TOP: Infection Control KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A patient has a nursing diagnosis of Infection, related to inadequate primary defenses, as evidenced by surgical incision and intravenous (IV) line access. An appropriate nursing intervention for this patient is to: • assess and document skin condition around the incision and IV site at each shift. • limit visitors to immediate family to decrease exposure to infection. • require the use of a face mask by nursing staff when they are providing care. • maintain clean technique in the change of om wound dressing and IV site. ANS: A Early identification of infection leads to prompt treatment and decreased transmission to others. Effective documentation provides a comparison from shift to shift about appearance of incision and IV site. DIF: Cognitive Level: Application REF: k 235, Health Promotion OBJ: Theory #2 TOP: Infection Control KEY: Nursing Process Step: Assessment MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The correct way to handle soiled linens in the room of a patient who is on Contact Precautions is for the nurse to: • wear a gown to protect the uniform and wear barrier gloves to roll the soiled sheets together and pla designated container. • remove the soiled sheets using barrier gloves and to keep the linens away from the uniform and the laundry bag held by another nurse outside the room. te st pr ep .c • shake out the linens before placing them in a designated laundry bag to ensure that there are no plas caught in the sheets. carry the soiled sheets directly to the unit laundry area before removing the personal protective equi ANS: B The nurse should wear a gown to protect the uniform and should wear barrier gloves to roll the soiled sheets together and place them in the designated container inside the room. DIF: Cognitive Level: Application REF: k 241, Box 17-3 OBJ: Theory #7 TOP: Infection Control KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A patient on Airborne Precautions says to the nurse, I feel like Im going crazy cooped up in here. I feel like just sneaking out and finding someone to talk to. The best response by the nurse is: • You would be jeopardizing everyone you come into contact with. You could give a lot of innocent w w w .m yn ur si ng • • • • It wont be long before you can safely get out of here without being a danger to others. You must be feeling bored being shut up in here. Have you been following the wonderful season ou been having? I know just how you feel. Sometimes I cant get outdoors because of the rain, and its so hard being c ANS: C om Talking about a shared interest will divert the patient. DIF: Cognitive Level: Application REF: k 243 OBJ: Theory #8 TOP: Isolation KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A patient is discharged home with a draining wound that was infected and for which he was on Contact Precautions while in the hospital. He lives at home with his 48-year-old wife and their 17-year-old daughter. It is most important to emphasize to this patient that: • he should maintain a safe distance from his family. he should use paper plates and disposable utensils. • soiled dressings should be disposed of in plastic bags that are tied securely. ep .c • his family members should wear gloves when handling his plate and eating utensils. ANS: C In the home, Contact Precautions require the use of barrier gloves to prevent contact with wound secretions during dressing changes (or if linens were soiled) and during the handling of soiled dressings. Soiled dressings should be disposed of in a securely tied plastic bag. Good hand hygiene and attention to medical asepsis principles are sufficient. DIF: Cognitive Level: Application REF: k 241 OBJ: Theory #6 TOP: Infection Control in the Home KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control A family member has been instructed in the administration of subcutaneous medication at home. The nurse instructs her to: break the needle off from the syringe so that it cant be reused and wrap the broken needle and syrin • throw them in the garbage. recap the needle and dispose of it in the garbage, because it cant accidentally stick anyone with the w w • w .m • yn ur si ng te st pr • • • save the used needles and syringes for the visiting nurse, who can collect them and arrange for prop place the used syringe and needle, without recapping it, in a large plastic bottle with a secure lid. ANS: D The use of a heavy plastic container with a secure lid, such as a bleach or detergent bottle, is a safe way to dispose of the uncapped syringe. DIF: Cognitive Level: Application REF: k 242 OBJ: Theory #6 TOP: Infection Control in the Home KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse recognizes a break in aseptic technique when: • the hand towel is kept above the waist level. • the hands are kept lower than the elbows during the surgical scrub. • faucets are turned off with a paper towel elbow or foot control in a scrub for a surgical operation. the sterile glove is donned by sliding the ungloved hand under the cuff of the sterile glove. ANS: B Allowing the hands to become lower than the elbow is a break in aseptic technique. DIF: Cognitive Level: Application REF: k 246, Skill 17-1 OBJ: Theory #9 TOP: Surgical Asepsis KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nursing intervention most likely to decrease the chance of health care-associated infections (HAIs) for a 76-year-old patient following bowel resection surgery would be to have the patient: • turn, cough, and deep-breathe every 2 hours. pr ep .c om • limit ambulation. • get blood pressure, pulse, and respirations assessed every 4 hours. te st • • w w w .m yn ur si ng ke ep th e ro o m do or cl os ed . A N S: A Having the patient turn, cough, and deep-breathe every 2 hours can help prevent the complication of pneumonia in the postoperative patient. Turning, coughing, and deep-breathing can enhance the prevention of pneumonia in the surgical patient. DIF: Cognitive Level: Application REF: k 235 OBJ: Theory #2 TOP: Health Care-Associated Infections KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • When caring for a patient on Droplet Precautions, it is most important for the nurse to: • wear the appropriate respiratory device for any entry into the room. • cover the patient with a clean sheet when transporting the patient to x-ray. • wear a gown and gloves for any contact with the patient. wear a mask if working within 3 feet of the patient. ANS: D The wearing of a mask when working within 3 feet is all that is necessary for a patient on Droplet Precautions. DIF: Cognitive Level: Application REF: k 241, Box 17-3 OBJ: Theory #4 TOP: Infection Control KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse adding sterile liquids to a sterile field should: • hold the liquid container high over the sterile field. st pr ep .c om • remove the cap and place the container with the inside facing down. • prepare a new sterile field if it becomes wet during the procedure. te • carefully reach over the sterile field to pour the liquid. ANS: C Once a sterile field is wet, it is contaminated and a new field needs to be prepared. DIF: Cognitive Level: Application REF: k 253 OBJ: Clinical Practice #2 TOP: Surgical Asepsis KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A patient with primary tuberculosis is on Airborne Precautions, and he spends much of the day sleeping and is confused and awake at night. An appropriate nursing intervention for this patient is to: • provide diversionary activities or visitors during the day to decrease his sense of isolation and senso w w w .m yn ur si ng • • • arrange for the patient to be transported to the lounge while wearing a surgical mask to provide mor consult with the physician for an order for an antidepressant and sleeping medication to treat the de encourage staff to visit with him from the doorway so that they do not have to wear a mask and the d. ANS: A ep .c A patient on Airborne Precautions (or any isolation) may become confused and have difficulty sleeping related to sensory deprivation, and the daytime sleeping may reflect boredom and further contribute to sleeplessness at night. Providing diversionary activities addresses these problems. DIF: Cognitive Level: Analysis REF: k 243 OBJ: Theory #8 TOP: Isolation KEY: Nursing Process Step: Planning MSC: NCLEX: Psychosocial Integrity: coping and adaptation • An 84-year-old patient is hospitalized for an infected stasis ulcer on his ankle. The nurse is aware that this patient is at risk for a hospital-acquired infection (HAI) because the: • patient already has a blood-borne infection. om wakeful times during the day. patients defenses are already engaged with the initial infection. • ulcer will make this patient bedfast. • stasis ulcers predispose the elderly to pneumonia and urinary infections. st pr • double bag the specimen container and send the specimen to the lab. w • w .m yn ur si ng te ANS: B The elderly have an impaired immune system. This patients immune system is already engaged with the stasis ulcer, which may put him at risk for an HAI. DIF: Cognitive Level: Application REF: k 237, Elder Care OBJ: Theory #2 TOP: Infection Control KEY: Nursing Process Step: Diagnosis MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse collecting a sputum specimen for a patient with staphylococcal pneumonia will: • wipe the specimen container with antimicrobial solution and hand carry it to the lab. w • • send the specimen to the lab in a Biohazard bag. notify the lab to collect the contaminated specimen. ANS: C Contaminated specimens are collected using appropriate PPEs and sent to the lab in a clearly marked Biohazard bag as required by OSHA. DIF: Cognitive Level: Application REF: k 239 OBJ: Clinical Practice #2 TOP: Infection Control KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse is helping the physician perform a sterile procedure at the bedside. Halfway through the procedure, the nurse believes the physician has contaminated the sterile field. The nurse should: • report the physician for violating surgical asepsis and endangering the patient. • ask the physician whether she contaminated her glove and the sterile field. • point out the possible break in surgical asepsis and provide another set of sterile gloves and a fresh not say anything, because it is near the end of the procedure. ANS: C It is the responsibility of the nurse to point out any possible break in surgical asepsis. Saying nothing does not protect the patient and is negligence on the part of the nurse. A fresh sterile field should be provided. DIF: Cognitive Level: Application REF: k 244 OBJ: Theory #9 | Clinical Practice #2 TOP: Surgical Asepsis KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A nurse is instructing one of the facilitys unlicensed assistive personnel (UAP) in ways to prevent health careassociated infections. The nurse recognizes that further instruction is warranted when the UAP states, I will: • wash my hands before and after caring for patients. ng te st pr ep .c om • cleanse patients from the rectum to the urinary meatus. • clean residual urine off the catheter bag when emptying it. • put all the soiled linen in the hamper in the room. ANS: B .m yn ur si • w w w A person should never cleanse from the rectal area to the urinary meatus because of the risk of introducing infection into the urinary tract. DIF: Cognitive Level: Application REF: k 241, Box 17-3 OBJ: Theory #2 TOP: Prevention of Infection KEY: Nursing Process Step: Implementation | Nursing Process Step: Evaluation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A patient is hospitalized with suspected disseminated zoster (varicella). The nurse should anticipate that this patient will be Precautions. placed on • Standard • Droplet • Airborne Airborne Precautions • Droplet Precautions pr • ep .c om • Contact ANS: C Airborne Precautions are used in addition to Standard Precautions for patients with known or suspected serious illnesses transmitted by airborne droplet nuclei. Examples of such diseases are measles, varicella (including disseminated zoster), and pulmonary tuberculosis. DIF: Cognitive Level: Application REF: k 236, Box 17-1 OBJ: Theory #4 TOP: Airborne Precautions KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A patient is hospitalized with pertussis. The nurse should place the patient on what type of precautions? • Contact Precautions te st • w w w .m yn ur si ng S t a n d a r d P r e c a u t i o n s A N S : C Droplet Precautions are used in addition to Standard Precautions for patients with known or suspected serious illnesses transmitted by large-particle droplets. An • Haemophilus influenzae meningitis. • pertussis. om example of such an illness is pertussis. DIF: Cognitive Level: Application REF: k 236, Box 17-1 OBJ: Theory #24 TOP: Prevention of Infection KEY: Nursing Process Step: Implementation MSC: NCLEX: N/A • The patient for whom the nurse should observe Contact Precautions in addition to Standard Precautions would be diagnosed with: • pulmonary tuberculosis. w ep pr st te ng si ur yn w .m re sp ir at or y sy n c yt ia l vi ru s. A N S: D .c • w Contact Precautions are used in addition to Standard Precautions for patients with known or suspected serious illnesses easily transmitted by direct patient contact or by contact with items in the patients environment. An example of such an illness is respiratory syncytial virus. DIF: Cognitive Level: Application REF: k 236, Box 17-1 OBJ: Theory #24 TOP: Contact Precautions KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • When the nurse is explaining Tier 2 as developed by the Hospital Infection Control Practices Advisory Committees (HICPAC), the nurse will emphasize that the purpose of Tier 2 is to: • interrupt the mode of transmission. • monitor the efficiency of the treatment. • be put in place of Standard Precautions. update all information relative to infections. ANS: C Tier 2, or Transmission-Based Precautions, is focused on interrupting the mode of transmission and is always used in combination with Standard Precautions. DIF: Cognitive Level: Comprehension REF: k 236 OBJ: Theory #23 TOP: Prevention of Infection KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • In caring for a patient with active tuberculosis, the nurse should anticipate: • wearing an N95 mask. pr ep .c om • wearing two masks to better filter microorganisms. • donning a mask only in the case of close contact. st • placing a mask on the patient while care is being performed. ANS: A When the patient has known or suspected pulmonary tuberculosis, a special particulate filter mask called an N95 mask must be worn. DIF: Cognitive Level: Application REF: k 239 OBJ: Theory #5 TOP: Prevention of Infection KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse is instructing one of the facilitys unlicensed assistive personnel (UAP) about how to correctly use a sharps container. The nurse recognizes that further instruction is warranted when the UAP states, I will: • drop sharp items, including needles, into a sharps container. w w .m yn ur si ng te • shake the sharps container gently to settle the contents. • put my fingers inside the opening to push the item well inside the container. w • • replace the sharps container when it is two thirds full. ANS: C No one should ever put fingers inside the opening of the sharps container. The container may be shaken gently to settle the contents and make more room if necessary. Sharps containers should be replaced when they are two thirds full. DIF: Cognitive Level: Comprehension REF: k 240 OBJ: Theory #7 TOP: Safety KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A nurse is caring for a patient who is in isolation. The nurse would correctly do which of the following? • Freely take items in and out of the isolation room. • Shake linen when removing it from the bed. • Turn faucets on and off using a paper towel. Consider items dropped on the floor useable. ANS: C General principles regarding isolation include that anything that is brought into the isolation area must not be removed except in proper containers, which are then placed in an outside container labeled Hazardous MaterialBiohazard. They also include never shaking linen when removing it or placing it on the bed, turning faucets on and off using a paper towel to protect the hands, and that floors are considered contaminated; anything dropped on the floor is contaminated and must be discarded or cleaned carefully before reuse. DIF: Cognitive Level: Application REF: k 240, Box 17-2 OBJ: Theory #7 TOP: Isolation KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • When picking up the first sterile glove, the nurse will: • grasp the cuff with the thumb and fingers. si ng te st pr ep .c om • insert fingers into the opening and pull the glove on while holding the cuff. • slip a thumb in the opening and grasp the glove between the thumb and fingers. ur • leave the glove on a flat surface and work the fingers into the opening. ANS: C The first glove is grasped by slipping the thumb in the opening and grasping the cuff with the fingers. DIF: Cognitive Level: Application REF: k 241, Box 17-3 OBJ: Theory #5 TOP: Prevention of Infection KEY: Nursing Process Step: Implementation MSC: NCLEX: N/A • A nurse is instructing a nursing student about principles of aseptic technique. The nurse would recognize the need for further instruction if the nursing student states, I must: • avoid coughing, sneezing, or unnecessary talking near or over a sterile field. w w w .m yn • • avoid reaching across or above a sterile field with my bare hands or arms. • open the wrapper of a sterile pack toward my body, the proximal flap first. • keep my sterile gloved hands in sight, away from all unsterile objects. ANS: C Principles of aseptic technique include avoiding coughing, sneezing, or unnecessary talking near or over a sterile field. They also include avoiding reaching across or above a sterile field with bare hands or arms or with other non-sterile items. The wrapper of a sterile pack must be opened away from the body, the distal flap first, the lateral flaps next, and the proximal flap toward the body last, thus making it unnecessary to reach over the sterile field. When wearing sterile gloves, hands must be kept in sight away from all unsterile objects, and above the waist level. w w w .m yn ur si ng te st pr ep .c om DIF: Cognitive Level: Application REF: k 235 OBJ: Theory #92 TOP: Prevention of Infection KEY: Nursing Process Step: Evaluation MSC: NCLEX: Safe Effective Care Environment: safety and infection control COMPLETION • A patient had abdominal surgery 3 days ago and now has a temperature of 101.2 F and reports feelings of malaise. The nurse assesses the abdominal incision and observes edema around the incision and some purulent drainage. This patient is in the stage of infection. ANS: illness The illness period of infection is defined by the presence of systemic signs and symptoms such as fever, headache, malaise, rash, swelling, leukocytosis, purulent wound exudate, diarrhea, and vomiting. DIF: Cognitive Level: Analysis REF: k 235 OBJ: Theory #1 TOP: Stages of Infection KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity • The most contagious stage of infection is the period. ANS: prodromal Although the prodromal period is short, it is the most contagious. People often do not realize they are ill, and precautions may not be taken, which increases the risk of transmission. DIF: Cognitive Level: Comprehension REF: k 234 OBJ: Theory #1 TOP: Infection Control KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity MULTIPLE RESPONSE • Differences between Airborne and Droplet Precautions include which of the following? (Select all that apply.) • A surgical mask must be worn with Airborne Precautions. • Patients on Droplet Precautions do not need to wear a surgical mask when outside their rooms. • A surgical mask must be worn if working within 3 feet of a patient on Droplet Precautions. • Airborne Precautions include placing the patient in a negative-pressure room. • A specialized respirator mask must be worn with patients on Droplet Precautions. Standard Precautions need to be used only with patients on Airborne Precautions. ANS: C, D, E The Centers for Disease Control and Prevention (CDC) recommends the use of specialized respirator masks when working with patients on Airborne Precautions and a surgical mask when working within 3 feet of a patient on Droplet Precautions. Both Airborne and Droplet Precautions include the use of a private room; however, a negative-pressure room is required for Airborne Precautions. Standard Precautions are to be used with all patients. DIF: Cognitive Level: Comprehension REF: k 241, Box 17-3 OBJ: Theory #4 TOP: Infection Control KEY: Nursing Process Step: N/A MSC: NCLEX: Safe Effective Care Environment • A nurse is caring for a patient in protective isolation for extreme immunosuppression. Before entering the room, which of the following actions should the nurse take? (Select all that apply.) st pr ep .c om • Don a gown. • Don a mask. • Put on gloves. • Apply a head covering. • Apply shoe coverings. ur si ng te • Bring in the blood pressure cuff and stethoscope. ANS: A, B, C A gown, mask, and gloves are all that is required; however, the CDC or hospital policies may require full PPE protection. DIF: Cognitive Level: Application REF: k 237 OBJ: Clinical Practice #2 TOP: Infection Control KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse clarifies that the duties of the facilitys Infection Preventionist include: (Select all that apply.) • viewing every culture that is performed in the facility that is positive for pathogens. w w w .m yn • • investigating possible causes for the occurrence of health careassociated infections (HAIs). • sanitizing isolation rooms after patients have been discharged. • counseling persons who have been found to be careless about infection control protocols. • providing education to health care staff relative to infection control. ANS: A, B, D, E The Infection Preventionist (IP) follows up on all positive cultures, investigates possible causes of HAIs, and provides ongoing education to staff. Counseling and sanitizing are not directly the responsibility of the IP, although he or she might suggest counseling and supervise sanitizing procedures. ep .c om Chapter 23 Body Mechanics, Positioning, and Moving The nurse uses professional knowledge about body mechanics to prevent the most common occupational disorder in nurses, which is: • carpal tunnel syndrome from use of computer keyboards in nursing documentation. shoulder and elbow injuries from moving patients. • knee injuries from standing for long periods. pr • back injuries from lifting and twisting. ANS: D Back injuries are the most common injury in health care workers, and in many cases, they are preventable through use of proper body mechanics. DIF: Cognitive Level: Knowledge REF: k 259 OBJ: Theory #2 TOP: Body Mechanics KEY: Nursing Process Step: Planning yn ur si ng te st • w w .m MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse assisting a weak patient from a bed to the wheelchair to go to physical therapy would: • seat the patient on the side of the bed with feet touching the floor. w • • • place hands under the patients elbows to assist in rising. lock knees as the patient is lowered to the chair. assist the patient to don a robe after being seated in the wheelchair. ANS: A After locking the wheels of the wheelchair, seat the patient on the side of the bed with the feet touching the floor. DIF: Cognitive Level: Application REF: k 276, Skill 18-4 OBJ: Clinical Practice #1 TOP: Patient Transfers KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment • A frail older patient is able to stand but not to ambulate. She has an order to be up in a wheelchair as desired during the day. A safe and appropriate way to assist her up to a chair is to: • use a mechanical lift to transfer her from the bed to a chair. assist her to stand and pivot to a chair at right angles to the bed, using a transfer belt. • have another staff member help lift her out of bed to the chair on the count of three. om • place a chair close to the bed and use a roller board to slide her into it. ANS: B A patient who can stand can safely be assisted to pivot and transfer with the use of a transfer belt. This benefits the patient (active exercise) and is safe for both the nurse and the patient. DIF: Cognitive Level: Application REF: k 276, Skill 18-4 OBJ: Theory #5 TOP: Patient Transfers KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The charge nurse on the night shift of a skilled nursing facility is orienting a new aide to the unit. The LPNs most accurate information relative to moving patients is: Most of your assigned patients are able to move about a little. Dont wake them to change their posit • are sleeping. yn ur si ng te st pr ep .c • .m w • When you get Mrs. S up to the toilet, be sure to keep your feet together and your knees locked, or s over. w Get one other aide to help and use the mechanical lift when you get Mr. A out of bed in the mornin doesnt assist at all. w • • Use your back muscles to liftthat will strengthen them and make it easier for you to lift or move hea ANS: C Getting adequate assistance and using mechanical assistance are important to reduce injury to staff and patients. It also increases the comfort of the move for the patient. DIF: Cognitive Level: Application REF: k 260, Box 18-4 OBJ: Theory #3 TOP: Patient Transfers KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The patient for whom passive range-of-motion exercises would be most beneficial would be the: • 66-year-old patient with loss of mobility related to a recent cerebrovascular accident (CVA). 72-year-old patient with chronic dementia who alternately sits in his wheelchair and wanders aroun • 80-year-old patient with chronic lung disease who can breathe only when he is sitting in a tripod po om • 94-year-old patient with increasing fatigue and weight loss who needs assistance to ambulate. ANS: A A patient with a recent CVA is unable to independently change position or move the affected side. The patient may regain use of motor functions lost, so it is very important to prevent loss of muscle strength, contractures, and pressure ulcers. DIF: Cognitive Level: Analysis REF: k 272, Skill 18-3 OBJ: Theory #2 TOP: Patient Positioning KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • An emaciated semiconscious bed-bound patient does not remain in a side-lying position and repeatedly turns onto her back, where she is developing a pressure area over her sacrum. The nurse should add to the nursing care plan to: • raise the knees to keep the patient from sliding down. yn ur si ng te st pr ep .c • position the patient on her side and use protective wrist and vest devices to keep her from turning o • assist the patient to sit in a wheelchair for short periods before returning her to bed. w place the patient on her stomach (prone position) using a small pillow below her diaphragm. ANS: D The prone position is an excellent (but underused) position to take pressure off the sacral area. Raising the head and the knees of the patient interferes with venous return from the legs and puts a great deal of pressure on the sacrum. Use of a wheelchair for a semiconscious patient is not effective. DIF: Cognitive Level: Application REF: k 264 OBJ: Theory #2 TOP: Patient Positioning KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • To place a patient in the Sims or lateral-lying position, the nurse would initially: • raise the head of the bed to a 45- or 60-degree angle. w w • .m • • raise the bed to a waist-high working level. • bring the patient to the edge of the bed so that she will be centered when turned on her side. place a pillow behind the patients back to support her and prevent her from rolling onto her back. ANS: B A waist-high bed height is a comfortable and safe working height for the nurse and also prevents staff back injuries. The head is not raised in a side-lying position; it is in a Fowlers or semi- Fowlers position. DIF: Cognitive Level: Application REF: k 265, Skill 18-1 OBJ: Clinical Practice #1 TOP: Body Mechanics KEY: Nursing Process Step: Implementation ep .c om • st pr MSC: NCLEX: Safe Effective Care Environment: safety and infection control • To provide correct body alignment for a physically immobile patient in bed in the supine position, the nurse: • uses trochanter rolls between the patients legs to prevent inward rotation. places a large pillow behind the patients head and neck to hyperflex the neck. • raises the head and knees to maintain as much flexion of the hips and knees as possible. ng te • uses a footboard or places high-top sneakers on the patients feet to maintain dorsiflexion. ANS: D The use of high-top sneakers (or a footboard) prevents footdrop and maintains dorsiflexion. DIF: Cognitive Level: Application REF: k 264 OBJ: Theory #2 TOP: Patient Positioning KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse and an assistant are preparing to get a patient out of bed for the first time after a week of bed rest. They begin by having the patient dangle on the edge of the bed. The nurse should: • allow the patient to dangle for 10 to 15 minutes and then transfer her to a nearby chair. • perform passive range-of-motion exercises on the patients arms and legs while she is dangling to im assess the patients response to the changed position, looking for orthostatic hypotension, nausea, or • proceeding. w w w .m yn ur si • • dangle the patient only momentarily and then assist her to ambulate as far as she is able. ANS: C A patient who has been immobilized for any length of time may feel dizzy or experience a drop in blood pressure when sitting or standing for the first time. Therefore the nurse must assess the patient carefully to determine whether transfer to a chair, ambulation, or return to bed is indicated. DIF: Cognitive Level: Analysis REF: k 276 OBJ: Clinical Practice #2 TOP: Sitting up on Side of Bed KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse caring for a patient with a nursing diagnosis of Injury, risk for, related to right- sided weakness as evidenced by unsteady gait, would accommodate the patient by: • keeping the right arm in a sling to prevent injury. keeping bed rails up to prevent the patient from attempting to get up unassisted. • placing the wheelchair on the left side of the patient before transfer. .c • ng te st pr ep allowing unassisted ambulation with the support of a walker. ANS: C Placing the wheelchair on the patients stronger side aids in transfer. DIF: Cognitive Level: Application REF: k 276, Skill 18-4 OBJ: Theory #5 TOP: Patient Transfers KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse explains to the unlicensed assistive personnel (UAP) that a shearing force is applied to the patient when: om • a lifting sheet is used to move the patient to a stretcher. • the patient is pulled up in bed without being lifted. • the patient is seated in a wheelchair without a pressure cushion. yn ur si • the patient is left in the supine position. ANS: B When a patient is pulled up in bed without being lifted up first, shearing force is applied on the bony prominences and tissues of the back, which predisposes the patient to a pressure ulcer. DIF: Cognitive Level: Comprehension REF: k 262 OBJ: Theory #3 TOP: Positioning KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient who has had spinal surgery is not permitted to bend at the waist or to sit in a chair. To position the patient correctly in bed, the nurse: • places her in low- or semi-Fowlers position only. w w w .m • • uses logrolling to accomplish position changes from side to side. • moves the top half of her body first, then the middle, and finally her legs. keeps her in a prone position to keep pressure off her back. ANS: B Logrolling, or moving the patients body as one unit, is used after back surgery or trauma or when twisting or flexion must be avoided. Logrolling is accomplished using a sheet and at least two persons. DIF: Cognitive Level: Application REF: k 268 OBJ: Theory #3 TOP: Positioning K E Y: N u r s i n g P r o c e s s S t e p : Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient in the skilled nursing facility has left-sided paralysis from a stroke several years before, as well as generalized weakness. The nurse should ensure that which of the following devices is in place to prevent flexion contractures? • A trochanter roll to keep her legs from turning outward st pr ep .c om • A rolled washcloth in the palm of her left hand or a hand splint • A protective vest to keep her sitting upright in the chair ng te • A trapeze to permit her to change her position in bed more easily ANS: B A hand splint or rolled cloth in the palm of her hand (along with range-of-motion exercises) will help prevent flexion contractures of her hand. A trochanter roll prevents outward rotation, not flexion. DIF: Cognitive Level: Application REF: k 265, Skill 18-1 OBJ: Theory #3 TOP: Positioning KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • When the post-stroke patient complains to the nurse, I dont see why you are wasting your time doing the passive range-ofmotion exercises on my legs, the nurses most informative response would be based on the knowledge that the exercises: • guarantee the prevention of pressure ulcers. w w w .m yn ur si • • are part of the basic care given to all patients. • prevent contractures of the hips. • maintain the muscle mass of the limb prior to the stroke. ANS: C Passive range-of-motion (ROM) exercises, although not part of care given to all patients, does prevent contractures in persons who are bedfast. ROM does not om guarantee the prevention of pressure ulcers but helps in the improved circulation of the limbs. DIF: Cognitive Level: Application REF: k 272, Skill 18-3 OBJ: Clinical Practice #3 TOP: Effects of ROM KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • While the nurse is assisting a patient to ambulate, the patient suddenly says, Im dizzy. I cant stand up. As the patient begins to fall, the nurse should: • tell the patient, Look up, take some deep breaths, and stand up straight. You can do it. call for another nurse or aide to get a wheelchair to return the patient to her room via wheelchair. • step behind the patient, grasp her around the waist or chest, and slide her down his leg gently to the pr ep .c • look for the nearest chair and assist the patient to it. ANS: C A patient who is threatening to fall needs to be lowered to the floor to avoid injury from a fall by allowing the patient to gently slide down the nurses leg to the floor. DIF: Cognitive Level: Analysis REF: k 282, Skill 18-6 OBJ: Clinical Practice #6 TOP: Patient Transfers KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk • A patient who is weak from inactivity following a car accident benefits most if the nurse provides for: • passive range-of-motion (ROM) exercises to all joints four times a day. active ROM exercises to arms and legs several times a day. w • w .m yn ur si ng te st • w • • active ROM exercises with weights twice a day with 20 repetitions each. passive ROM exercises to the point of resistance or pain and then slightly beyond. ANS: B Active ROM is best to restore strength in a weak patient who can independently perform activities of daily living but is immobilized because of injury. DIF: Cognitive Level: Application REF: k 271 OBJ: Clinical Practice #3 TOP: Active Range of Motion KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • A nurse is ambulating an unsteady patient from the bed to a chair in the patients home. To do so safely, the nurse applies a gait belt and: • slides his hand from the bottom under the gait belt at the middle of the patients back. • grasps the gait belt from the top at the middle of the patients back, pulling it tight against the patien • has one person on each side grasp the belt from the top. secures a regular mans belt snugly around the patients waist to use if the patient starts to fall. ANS: A The nurse puts his hand from the bottom at the rear, so he can pull up if the patient starts to fall and not lose the grip on the gait belt. The gait belt should be tight enough to secure the patient, but loose enough for the passage of the nurses hand. DIF: Cognitive Level: Application REF: k 279 OBJ: Theory #5 | Clinical Practice #6 TOP: Assisted Ambulation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk • An example of the principles of good body mechanics applied to patient care occurs when the nurse: keeps his feet fixed, spread one in front of the other, and turns his upper body to move the patient u • rocking movement. si ng te st pr ep .c om • assists another nurse in pushing a patient from one side of the bed to the other. • bends at the waist to pick up and empty or move the urinary drainage bag attached to the lower end yn ur • works at arms distance from the patient when lifting or transferring the patient. ANS: A Fixing feet and placing one foot in front of the other and facing the direction of the movement will ease the work of moving a patient up in bed. Pulling requires less effort than pushing in this scenario. Twisting should be avoided; nurses should use leg muscles rather than back muscles to pick up objects from the floor. Work should be close to the body to reduce effort and strain. DIF: Cognitive Level: Application REF: k 265, Skill 18-1 OBJ: Theory #2 TOP: Body Mechanics KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A nurse is instructing one of the facilitys unlicensed assistive personnel (UAPs) regarding body mechanics for moving and lifting. The nurse recognizes that further instruction is warranted when the UAP states, I will: • lift using my back muscles. w w w .m • • obtain help whenever possible. • ask the patient to help if able. • 60 to 90 • w • .m yn ur si ng te st pr ep .c om us e a wi de ba se of su pp or t. A N S: A Guidelines for moving and lifting include obtaining help whenever possible; asking the patient to help if able; using thigh, arm, or leg muscles rather than back muscles; and using a wide base of support. DIF: Cognitive Level: Comprehension REF: k 265, Skill 18-1 OBJ: Theory #2 TOP: Body Mechanics KEY: Nursing Process Step: Evaluation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A physician orders the nurse to place a patient in Fowlers position. The nurse should elevate the head of the patients bed degrees. • 15 to 30 w w 30 to 60 • 10 to 15 ANS: A Fowlers position is arranged by elevating the head of the bed 60 to 90 degrees. Semi-Fowlers position is an elevation of 30 to 60 degrees, and low-Fowlers is an elevation of 15 to 30 degrees. Unless contraindicated, the knees can be raised 10 to 15 degrees in these positions. DIF: Cognitive Level: Comprehension REF: k 265, Skill 18-1 OBJ: Clinical Practice #1 TOP: Patient Positioning KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • As the nurse is helping an 85-year-old man to stand and ambulate, he complains that he feels that he has lost all of his strength in the last several years and cannot do the things he could do when he was 80. The nurses most informative response would be: • An increase in testosterone will build your muscle bulk back to where it was when you were young • As we age our muscle cells are lost and replaced by fat, which leads to loss of strength. • Inactivity makes our muscles lazy and they just wont do the work they used to do. Additional vitamins will build your strength back up in a few months. ANS: B Fat replaces muscle cells, which leads to loss of strength and stamina. DIF: Cognitive Level: Application REF: k 259 OBJ: Clinical Practice #1 TOP: Patient Positioning KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation COMPLETION • The primary function of a joint is to provide to the skeleton. ANS: movement Ligaments and tendons attach to bones at the joints, which allows movement. DIF: Cognitive Level: Comprehension REF: k 259 OBJ: Theory #1 TOP: Structure and Function of Musculoskeletal System KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity • There are two main factors in the development of pressure . ulcers. One is pressure and the other is ANS: shearing force Shearing is the applied force that causes a downward and forward pressure on the tissues beneath the skin. Examples include pulling sheets or clothing from underneath the patient and the force applied when a patient pushes down on the bed with her heels while trying to move up in bed. DIF: Cognitive Level: Knowledge REF: k 262 OBJ: Theory #2 TOP: Complications KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity w w w .m yn ur si ng te st pr ep .c om • • The nurse reminds a patient that one of the anatomic parts of a joint that allows the joint to move freely is the fluid-filled . ANS: bursa Bursa are small fluid-filled sacs that provide a cushion at friction Osteoporosis • Contractures • Increased blood pressure • Fluid in the lungs .c • om points and provide freely movable joints. DIF: Cognitive Level: Knowledge REF: k 259 OBJ: Theory #1 TOP: Bursa KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation MULTIPLE RESPONSE • Complications from incorrect alignment and positioning include which of the following? (Select all that apply.) • Pressure ulcers ep • w w w .m yn ur si ng te st pr E l e v a t e d t e m p e r a t u r e A N S : A , C , E Constant pressure on the skin, especially on bony prominences, interferes with circulation, causing pressure ulcers. Contractures occur when joints are not positioned om frequently, and fluid can accumulate in the lungs with infrequent positioning. Osteoporosis, increased blood pressure, and elevated temperature are not results of improper alignment or positioning. DIF: Cognitive Level: Comprehension REF: k 262 OBJ: Theory #2 TOP: Patient Positioning KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: reduction of risk • A 70-year-old immobile patient, who has right-sided weakness caused by a recent stroke, weighs approximately 250 pounds and needs to be moved up in bed. Which of the following actions should the nurse take? (Select all that apply.) • Summon at least one other person to assist. Obtain a mechanical lift. • Perform the move by himself, because it should not be too difficult. • Obtain a lift sheet. • Put the bed in semi-Fowlers position. Place the patient flat on her back. ANS: A, D, F The patients increased weight and inability to assist requires at least two people to move her up in bed. A lift sheet enables the patient to be moved. Placing the patient on her back decreases gravitational pull, making the move easier. A mechanical lift is used to transfer a patient, not to move her up in bed. .m yn ur si ng te st • pr ep .c • w w w Chapter 24 Fitness and Therapeutic Exercise When asked to give an example of complementary therapies, the nurse gives: • eating a macrobiotic diet to treat cancer instead of having surgery. • using imagery along with pain medication to increase comfort. • practicing naturopathic medicine, a natural means of promoting health. • practicing traditional Chinese medicine based on yin and yang. ANS: B Complementary therapies are used jointly with conventional methods to treat a problem. All the other possibilities listed are alternative therapies. DIF: Cognitive Level: Comprehension REF: k 610 OBJ: Theory #1 TOP: Complementary Therapies KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • When the patient asked the nurse about the use of acupuncture for the control of back pain, the nurse warned that acupuncture can put the patient at risk for: • meningitis. • streptococcal infection. • hepatitis. ng te st pr ep .c om • shigella. ANS: C The main concern of acupuncture therapy is the use of needles for this treatment. If sterile needles are not used, there is a high risk of HIV or hepatitis transmission. DIF: Cognitive Level: Comprehension REF: k 611 OBJ: Theory #3 TOP: Acupuncture KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • A nurse is caring for a patient admitted for electrolyte imbalance who has been practicing Ayurveda, a traditional Hindu system of medicine. The nurse should inform the physician that the patient is practicing this traditional form of medicine, because Ayurveda: • uses purgatives as part of the treatment. forbids invasive treatment methods. • requires that the shaman and physician confer. ur si • uses natural electrical currents in meridian areas. ANS: A Ayurveda uses special diets and purgatives as part of the practice, which could cause electrolyte imbalance. It does not forbid invasive procedures such as IVs. DIF: Cognitive Level: Knowledge REF: k 611 OBJ: Clinical Practice #2 TOP: Ayurveda KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk • A Mexican patient is admitted to the hospital with abdominal pain. The nurse learns the patient has been treated for the same condition by a curandero and wants the curandero to visit and perform rituals. The best response via the interpreter by the nurse is: w w w .m yn • • Im sorry, but only immediate family can visit. • It is not safe to have burning of herbs in the hospital. • Trust your doctor; he knows what is best for you. I will inform the doctor so that they can perhaps confer. ANS: D In Mexico, the use of the curandero is very common. It is best for the doctor to talk to the curandero to learn about the herbs used to treat the abdominal pain. DIF: Cognitive Level: Application REF: k 612 OBJ: Theory #2 TOP: Folk Medicine KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies • An elderly Hispanic male was admitted with a severe headache and is anxious. The patient tells the nurse that he was given the mal de ojo. The culturally competent nurse understands that mal de ojo means that the patient believes that he: • has a blockage in the intestine from the influence of Susto. ep .c om • has an opposition in polarities problem because of the effect of empacho. • was given the evil eye, which is thought to cause weeping and headache. st pr • has had a separation of the soul from the body. ANS: C The mal de ojo literally means the evil eye cast from someone, which can bring fear, irritability, headache, and weeping. DIF: Cognitive Level: Comprehension REF: k 612 OBJ: Clinical Practice #1 TOP: Folk Medicine KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A patient asks about the difference between imagery and meditation. The nurse explains that imagery uses a visual stimulus that can decrease stress, whereas meditation: • is a relaxation technique used to help with acute illness. involves focusing on a single repetitive stimulus, altering consciousness. w • w .m yn ur si ng te • w • • is a technique that trains the patient to retrieve memories and induce anesthesia. involves a combination of exercise and controlled breathing. ANS: B Meditation focuses on a single repetitive stimulus, altering consciousness and inducing a restful state. It has been helpful for people with chronic conditions such as asthma and diabetes. DIF: Cognitive Level: Comprehension REF: k 612 OBJ: Theory #4 TOP: Meditation KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A patient who is a heavy smoker has been told by the physician to stop smoking, but does not want to use a smoking cessation patch. The nurse suggests that the most effective alternative is: • meditation. • Qi Gong. • biofeedback. • w w w .m yn ur si ng te st pr ep .c om h y p n o s i s . A N S : D Hypnosis is therapy in which the patient is put into a hypnotic state, during which time suggestions are implanted in the mind that remain after the hypnosis ends. DIF: Cognitive Level: Comprehension REF: k 613 OBJ: Theory #4 TOP: Hypnotherapy KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient who is in labor is having anxiety and sobs with each contraction. The nurse decides to use imagery to calm the patient by: • having the patient close her eyes and picture herself in her favorite place. • having the patient do stretch exercises before each contraction. • telling the patient to relax and to calm down. • telling the patient strenuously focus on some image in the room. ANS: A Imagery involves visual stimuli to produce some physiologic change that can decrease anxiety or decrease pain. It is used often for patients in labor. The patient is asked to mentally recall some visual image that is pleasant to them. DIF: Cognitive Level: Comprehension REF: k 612 OBJ: Clinical Practice #3 TOP: Imagery KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A patients blood pressure measures 170/90 mm Hg. There is no history of hypertension, but the patient is very stressed because of career demands. The best complementary therapy that the patient might benefit from is: • meditation therapy. • meditation and medication. • dance therapy. om • w w w .m yn ur si ng te st pr ep .c p r a y e r a n d h e r b a l t h e r a p y. A N S : B Complementary therapy involves both alternative and conventional forms of medical treatment, such as meditation and antihypertensives. DIF: Cognitive Level: Analysis REF: k 610 OBJ: Theory #2 TOP: Complementary Therapies KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A patient is scheduled to have biofeedback therapy for migraine headaches. On arrival to the clinic, the patient appears anxious and fearful and tells the nurse that she does not want electric shocks. The most reassuring response by the nurse is • Dont worry; this will not hurt a bit. Didnt the doctor explain this procedure to you? • There are no electrical shocks involved; the doctor is looking at your bodys activity. • You seem too anxious for this procedure. Lets reschedule it at another time. ANS: C • Ayurveda. ng dance therapy. si • te st pr ep .c Biofeedback involves applying electrodes to the body to look at the internal activity, so that the patient can gain control of involuntary activity. DIF: Cognitive Level: Application REF: k 612 OBJ: Clinical Practice #2 TOP: Biofeedback KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A patient who has job-related stress and chronic back pain wants to start exercising but dislikes physical activity. The nurse suggests that the most beneficial therapy for this patient is: • yoga therapy. om • ur • w w w .m yn s h a m a n i s m . A N S : A Yoga is a combination of exercise, controlled breathing, posture, and mental focus to bring positive effects on the body and mind. It is effective for stress reduction and chronic back problems. DIF: Cognitive Level: Comprehension REF: k 613 OBJ: Theory #3 TOP: Yoga KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • Before integrating humor in the care of an Asian patient, the nurse should: • develop jokes about the patients condition. • develop jokes about the doctors and nurses. • ask the patient whether jokes are understood. ask the patients feelings about hearing a joke or funny story. ANS: D Humor and laughter are used at the bedside to distract patients from pain, and they have a positive effect on the body. However, it is important to check with the patient first to find out whether it might be considered disrespectful. DIF: Cognitive Level: Application REF: k 613 OBJ: Theory #2 TOP: Humor KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity: psychosocial adaptation • The nurse caring for a patient without any religious affiliation who was admitted 2 days ago with a severe gastrointestinal infection encounters the hospital chaplain who wants to pray with the patient. The most appropriate response by the nurse is: • That is a wonderful idea. I am sure that the patient will find comfort in that. ng te st pr ep .c om • Before you do that, we need to get the patients permission. • I need to get an order from the doctor. ur si • I dont think the patient wants any religious interventions. ANS: B Although prayer has been known to promote healing, the patients privacy must be protected. DIF: Cognitive Level: Application REF: k 613 OBJ: Clinical Practice #1 TOP: Prayer KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: psychosocial adaptation • w w w .m yn • A Hispanic female patient visits the clinic with complaints of sleep loss and wants sleeping pills. In further talking with the patient, the nurse learns that the patient is also drinking valerian tea. The most appropriate nursing action is to: • talk to the patient about her usual sleep habits. • instruct the patient on the appropriate dose for sleeping pills. • inform the doctor that the patient is drinking valerian tea. • give written instructions about the effects and side effects of sleeping pills. ANS: C deep massage. • herbal remedies. ep • .c om Valerian is a minor tranquilizer for sleep disorders. Combining both valerian and hypnotics puts this patient at risk for sedation overdose, so it is best that the doctor is aware. DIF: Cognitive Level: Application REF: k 615, Table 32-1 OBJ: Theory #5 TOP: Herbal Remedies KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • The home health nurse helps a patient schedule an appointment with a chiropractor because of chronic back pain, instructing the patient that the chiropractic treatment will involve: • manipulation of the spine. pr • w w w .m yn ur si ng te st e n e r g y t h e r a p i e s . A N S : A Chiropractic therapy is the manipulation of the spine for relief of pain by correcting the spine alignment, and is being accepted more widely as an alternative form of health care. DIF: Cognitive Level: Knowledge REF: k 616 OBJ: Theory #6 TOP: Chiropractic Therapy KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse is assessing a patient and finds that the patient is taking ephedra for weight control. The finding that is most likely attributable to ephedra is: • BP 138/90 mm Hg, pulse rate 95 beats/minute. • gain of 15 pounds in 4 weeks. • excessive diarrhea for the last 3 days. BP 180/98 mm Hg, pulse rate 130 beats/ minute. ANS: D Ephedra, or ma huang, is a cardiac stimulant found in weight-loss preparations, and the patient should be instructed to stop taking it because of its adverse side effects. DIF: Cognitive Level: Comprehension REF: k 615, Table 32-2 OBJ: Clinical Practice #2 TOP: Herbal Therapy KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • When an asthmatic patient asks the nurse about using aromatherapy oils for decreasing stress, the nurse expresses concern to the patient about: ng te st pr ep .c om • the cost of the aromatherapy. • possible allergic reaction to the oils. • the oils causing staining of furniture. yn ur si • the oils not being very effectiv e. ANS: B The aromatic properties of certain herbs could cause allergic reactions that can trigger asthmatic episodes. DIF: Cognitive Level: Comprehension REF: k 616 OBJ: Clinical Practice #2 TOP: Aromatherapy KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • A patient is seen by an alternative medicine practitioner for menopausal symptoms. The most popular and effective herbal remedy that the alternative medicine practitioner would suggest is: • valerian. w w w .m • • ma huang. • black cohosh. • w .m yn ur si ng te st pr ep .c om e c h i n a c e a . A N S : C Women are using alternative hormone replacement therapy such as black cohosh to treat hot flashes and mood swings. DIF: Cognitive Level: Comprehension REF: k 615 OBJ: Theory #3 TOP: Herbal Remedies KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A patient asks the nurse about the difference between manipulative and body-based methods and mindbody therapies. The nurses correct response is that: manipulative and body-based methods involve touching or manipulation, and mindbody therapies d • ability to affect the body. w mindbody therapies involve touch and manipulation, and body-based methods involve the minds ab body. w • • • mindbody therapies involve the use of herbal remedies, whereas manipulative and body-based meth an example of manipulative body-based methods is biofeedback, and an example of mindbody ther ANS: A Manipulative and body-based methods involve touching, such as in chiropractic therapy, and mindbody therapy is the mind working to heal the body, such as with imagery. DIF: Cognitive Level: Comprehension REF: k 616 OBJ: Theory #4 TOP: Manipulative and Body-Based Methods Versus Mind-Body Therapies KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • An elderly female patient is placed on warfarin sodium (Coumadin) for thrombophlebitis and is seen in the clinic for a follow-up visit. On assessment, the patient complains that her forgetfulness is becoming worse and asks if ginkgo biloba would help. The most appropriate response by the nurse is: Ginkgo biloba improves memory, and you should have good results. • Ginkgo biloba should not be part of your regimen, and the doctor does not believe in it. • You should take St. Johns wort instead, because it works better. .c om • Coumadin and ginkgo biloba should not be taken together because the herb prolongs bleeding time. ANS: D Coumadin and ginkgo biloba should not be used together, because the herb prolongs the bleeding time, placing the patient in danger of hemorrhage. DIF: Cognitive Level: Application REF: k 617 OBJ: Theory #5 TOP: Complementary Therapy Effects KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies • A patient with thrombophlebitis is contemplating being seen by a massage therapist for a deep body massage. The nurse warns that such a therapy may be harmful because: • the practitioner will use magnets on the body to relieve pain. ur si ng te st pr ep • the practitioner will use electrical stimulation. • there is an increased risk of breaking loose a clot with the massage. yn • massage may cause vasoconstric tion. ANS: C With a history of thrombophlebitis, the massage might cause more injury to the patient by breaking loose a clot with the stroking and kneading performed to the legs and by the clot traveling to the lung, heart, or brain. DIF: Cognitive Level: Analysis REF: k 616 OBJ: Clinical Practice #2 TOP: Massage KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • When taking the depressed patients history, the nurse finds that the patient is taking Prozac and the herbal remedy St. Johns wort. The nurse gives this information to the physician immediately because: • the patient is still depressed and needs another antidepressant added. w w w .m • • Prozac and St. Johns wort should not be taken together, because this can cause toxicity. • Prozac and St. Johns wort are complementary therapies and the doctor should know this. the patient should not be taking herbal remedies, because they have proven to be ineffective. ANS: B Prozac and St. Johns wort together have a negative effect on the body, causing toxicity. DIF: Cognitive Level: Analysis REF: m 617 OBJ: Theory #5 TOP: Herbal Remedies KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease COMPLETION • A branch of traditional Chinese medicine in which very fine needles are used to stimulate certain points on the body along lines called meridians to increase or disperse the flow of energy is . known as ANS: acupuncture pr ep .c om • w w w .m yn ur si ng te st Acupuncture is a branch of traditional Chinese medicine. Very fine needles are used to stimulate certain points on the body along lines called meridians to increase or disperse the flow of energy. DIF: Cognitive Level: Comprehension REF: m 611 OBJ: Theory #3 TOP: Alternative Therapy KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • An alternative type of medical practice that stimulates the patients natural defenses to alleviate the problem because illness is considered to be specific to the individual is . ANS: naturopathic medicine Naturopathic medicine uses a combination of lifestyle management, application of botanicals, light, fresh air, and exercise to maintain a high level of wellness. DIF: Cognitive Level: Comprehension REF: m 611 OBJ: Theory #3 TOP: Naturopathic Medicine KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The technique in which the practitioner alters body energy fields by passing his hands over the patient to determine where . tensions exist is the practice of ANS: therapeutic touch The concept of therapeutic touch involves the caregiver causing an alteration of the patients body energy field by passing his or her hands over the patients body. DIF: Cognitive Level: Comprehension REF: yn ur si ng te st pr ep .c om m 617 OBJ: Theory #3 TOP: Therapeutic Touch KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A form of alternative therapy that is used by more than 70% of the worlds population for treatment of disorders with botanicals is . ANS: herbal therapy phytotherapy Herbal therapy (phytotherapy) is a system of herbal applications used to treat a wealth of disorders and is used by 70% of the worlds population. DIF: Cognitive Level: Comprehension REF: m 613 OBJ: Theory #3 TOP: Herbal Therapy KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The alternative practice in which the practitioner journeys to other planes of existence to retrieve information for the . healing process is ANS: Shamanism The Shaman journeys to different planes of existence to retrieve information for healing. The Shaman performs rituals with burning plants and herbs to rebalance the patient with nature. DIF: Cognitive Level: Comprehension REF: m 612 OBJ: Theory #2 TOP: Shamanism KEY: Nursing Process Step: N/A MSC: NCLEX: N/A MULTIPLE RESPONSE • The nurses role(s) when patients practice complementary and alternative therapies include:(Select all that apply.) • asking whether patients are taking over-the-counter herbal remedies. questioning the patient extensively regarding why he or she is practicing complementary or alternat • exploring the cost of treatment and how many treatments are required. w instructing the patient to inform the health care provider when such therapies are being used. ANS: A, D The nurses responsibility is gathering necessary information about the complementary or alternative therapies the patient might be practicing to help the physician make the best decision for the health care of the patient. DIF: Cognitive Level: Application REF: m 617 OBJ: Theory #5 TOP: Nurses Role KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The culturally competent nurse is aware that the American Indian medicine techniques are very significant to the patient. w w • .m • This medical intervention involves: (Select all that apply.) • healing ceremonies. • rituals performed by highly trained medicine people. • burning of sweet grass. • purging with minerals. drums to align the patients heart with Mother Earth. ANS: A, B, C, E The American Indian medicine techniques involve many specific ceremonies and rituals performed by highly trained medicine people. The burning of herbs, shaking rattles, and drumming realigns the patient with Mother Earth. DIF: Cognitive Level: Comprehension REF: m 612 OBJ: Theory #3 TOP: American Indian Medicine KEY: Nursing Process Step: Planning MSC: NCLEX: Psychosocial Integrity: psychosocial adaptation • The practitioner of Reiki acts as a conduit for healing energy by directing healing energy to the patients receptors located in the: (Select all that apply.) • arms. forehead. • groin. • feet. ur si • ng te st pr ep .c om • w .m yn • hands. ANS: B, C Reiki directs energy through the practitioner to the receptors located in the patients crown, forehead, throat, heart, stomach, abdomen, and groin. Chapter 25 Mechanical Immobilization w w 1. The nurse is contributing to the plan of care for a patient who has a right fractured femur. What intervention should the nurse include in the plan of care to prevent fat emboli? • • • • Decrease dietary consumption of fats. Maintain immobilization of the right leg. Encourage coughing and deep breathing hourly. Perform passive range of motion on the right leg. 2. A patient has an open reduction of a radial fracture and is casted. Several hours after the operation, the patient reports a throbbing pain in the arm. What nursing action is essential for the nurse to take? • Reposition arm. Perform neurovascular checks. Administer analgesics as ordered. Notify the physician immediately. 3. The nurse is monitoring a patient with a casted left tibial fracture and a contusion of the thigh. The patient reports increasing pain in the left foot that has not been relieved by morphine injections. What should the nurse do? • Reposition the casted leg. • Repeat the morphine injection now. • Give a higher ordered dose of morphine. • Ensure physician is immediately notified. 4. The nurse finds a 2-day postoperative patient who had a right total hip replacement lying supine with crossed legs. What data should the nurse collect on this patient? • The right leg for shortening • The right knee for crepitation • The left leg for internal rotation • The left leg for loss of function 5. The nurse is caring for a patient who had a closed reduction of the ulna with a cast applied. Later the patient reports left arm pain. What should the nurse do first? • Pad the edges of the cast. • Notify the physician immediately. • Administer an analgesic as ordered. • Perform neurovascular check on fingers. 6. The nurse is reinforcing teaching provided to a patient recovering from right total hip replacement. Which patient statement indicates a correct understanding of the teaching? • Keep legs apart. • Lie prone in bed. • Move right leg closer to the left leg. • Do not bear any weight on the left leg. 7. A patient with a casted, fractured left leg asks why the leg has to be elevated. What should the nurse respond to this patient? • Decreases swelling. • Prevents cast cracking. • Increases your comfort. • Allows the cast to dry evenly. 8. The nurse is caring for a patient who has had a right hip replacement. For which position is the nurse attempting to achieve when a pillow is placed between the legs during turning? • Flexion of the knees • Abduction of the thighs w w w .m yn ur si ng te st pr ep .c om • • • • • Adduction of the hip joint Hyperextension of the knees w w w .m yn ur si ng te st pr om ep .c 9. The nurse sees a neighbor fall and fracture a leg. What should the nurse do first for the neighbor? • Assess pain. • Transport to an emergency department. • Cover site of open fracture with clean dressing. • Immobilize the affected limb using minimal movement. 10. The nurse is reinforcing teaching provided to a patient with rheumatoid arthritis (RA). Which patient statement indicates understanding of the symptoms of RA? • Fatigue • Paralysis • Crepitation • Shortness of breath 11. A patient with a 36-hour-old fractured femur is in traction and is prescribed morphine 10 mg every 3 hours as needed. The patient received a dose 3 hours ago and is now reporting a pain level of 8. The patient is stable. Which action should the nurse take? • Hold medication. • Notify the registered nurse (RN). • Give pain medication as ordered. • Give pain medication in 30 minutes. 12. The nurse is caring for a patient who has a newly casted, fractured wrist. Data collection reveals slightly puffy fingers with good capillary refill. What should the nurse do now to prevent complications? • Notify the RN. • Apply heat to the cast. • Elevate the cast on pillows. • Remove the pillow under the cast. 13. A patient with gout has been instructed on the prescribed medication allopurinol (Zyloprim). Which patient statement indicates understanding of the action of this medication? • Excretes proteins. • Blocks formation of uric acid. • Increases formation of purines. • Increases metabolism of purines. 14. The nurse is evaluating teaching provided to a patient with gout. Which patient menu selection indicates that additional teaching is required? • Pike • Bass • Perch • Sardines 15. The nurse is reinforcing teaching provided to a patient with gout. Which food should the patient state will be avoided that indicates teaching has been effective? • Rice • Beets • • Liver Bananas w w w .m yn ur si ng te st pr ep .c om 16. The nurse is contributing to the plan of care for a patient with Pagets disease. Which outcome should the nurse identify as being appropriate for this patient? • Gain 5 lb weekly. • Intake equals output. • Identify coping skills. • Pain is relieved at a satisfactory level. 17. The nurse is contributing to the plan of care for a patient who has a fractured hip and is placed in Bucks (boot) traction while awaiting surgery. What is the desired outcome for placing the patient in Bucks traction? • Restrain patient. • Realign fracture. • Relieve patient pain. • Maintain fracture reduction. 18. The nurse is reinforcing teaching for a patient who has had a total hip replacement on correct sitting positions. Which position should the nurse teach the patient to avoid? • Crossing legs • Elevating legs • Flexing ankles • Extending knees 19. The nurse is contributing to the plan of care for a patient who has an upper extremity amputation. Why should the nurse keep in mind that this type of amputation can be more debilitating than a lower extremity amputation when planning care? • The upper extremity is more visible. • Prosthetic fitting is easier for the leg. • The upper extremity is more specialized. • There is greater blood supply to the upper extremity. 20. The nurse observes a petechial rash and respiratory distress in a patient recovering from a fractured femur. What should these findings suggest to the nurse? • Infection • Pneumonia • Fat embolism • Pleural effusion 21. A patient who has a displaced mid-shaft fracture of the left femur and is in balanced suspension skeletal traction with 35 pounds of weights is experiencing calf pain with right foot dorsiflexion. Which action should the nurse take? • Notify the RN. • Check the traction setup. • • Reduce 5 pounds of weight. Encourage dorsiflexion more frequently. 22. The nurse is contributing to the plan of care for a patient who is scheduled for a below- the-knee amputation. What nursing diagnosis should be recommended for the preoperative plan of care? • Anxiety • Self-Care Deficit • Fluid Volume Deficit • Ineffective Airway Clearance w w w .m yn ur si ng te st pr ep .c om 23. The nurse is reinforcing teaching on positioning for a patient after a right total knee replacement. Which patient statement indicates a correct understanding of the teaching? • Prone. • Side lying. • Supine with pillow under right knee. • Supine with three pillows between legs. 24. The nurse is reinforcing teaching provided to a patient for carpal tunnel syndrome treatment. Which patient statement indicates a correct understanding of the teaching? • Bedrest. • Arm sling. • Wrist splint. • Hand exercises. 25. A patient with a fractured pelvis and a left acetabular fracture is prescribed bedrest. When the patient asks to toilet, which measure would be appropriate? • Help patient up on a commode very carefully. • Turn patient onto right side, place the bedpan behind, and turn back. • Have patient sit up as high as possible and lift self up with hands pushing on the bed, then slide the bedpan underneath. • Ask patient to lift straight up using a trapeze mounted above the bed and slide a bedpan underneath from the right side. 26. The nurse is caring for a patient with gout. Which laboratory value should the nurse review which indicates that the treatment plan is effective? • Uric acid: 7.9 mg/dL • Creatinine: 0.8 mg/dL • Blood urea nitrogen: 15 mg/dL • Low-density lipoprotein (LDL): 115 mg/dL 27. The nurse is reinforcing teaching provided to a patient who is postmenopausal, has lost 2 inches of height, and has osteoporosis. Which patient statement indicates correct understanding of the purpose of calcium supplements? • To decrease bone loss .c pr ep To increase energy levels To decrease serum calcium To increase excretion of calcium 28. A patient is completing instructions about complications that can occur from osteoporosis. Which complication should the patient state as evidence that teaching has been effective? • Hip fracture. • Overgrowth of bone. • Bone spur formation. • Increased bone density. 29. The nurse is reviewing data collected during the health history for a patient with osteoporosis. What should the nurse identify as a risk factor for osteoporosis development? • Daily use of antacid • Walking 1 mile daily • Increased caffeine intake • Increased dairy food intake om • • • w w w .m yn ur si ng te st 30. The nurse reinforces medication teaching provided to a patient with rheumatoid arthritis. Which medication should the patient identify as helpful to control the symptoms of the health problem? • Digoxin. • Ibuprofen. • Morphine. • Penicillin. 31. The nurse checks a patients casted right leg resting upon a pillow and finds that the cast appears too tight. What should the nurse do? • Notify the RN. • Administer pain medication. • Apply an extra blanket to the leg. • Remove the pillow under the cast. 32. The nurse is contributing to the plan of care for a patient who has a bone fracture that is splintered and has shattered into numerous fragments. Which term should the nurse use to document this type of fracture? • Impacted • Avulsion • Greenstick • Comminuted 33. The nurse reinforces teaching on prevention of osteomyelitis with a patient who has an open fracture of the right leg. Which patient statement indicates that teaching has been effective? • Apply ice to right leg. • Keep leg immobilized. • Increase calcium intake in diet. • Wash hands prior to touching fracture area. w w w .m yn ur si ng te st pr ep .c om 34. An 87-year-old female with a history of osteoarthritis reports an average generalized pain score of 4 on a 0-to-10 scale while using acetaminophen prn. Which response about this pain level should the nurse make to the patient? • Do you take a daily calcium supplement? • Im glad the acetaminophen is working for you. • Are you satisfied with this level of pain control? • Research shows that acetaminophen is not really effective for osteoarthritis pain. 35. A patient is diagnosed with osteomyelitis of the right lower leg. What should the nurse expect to be prescribed for this patients care? • Anticoagulant therapy • Casting of the extremity • Fasciotomy of the wound • L o n g t e r m a n ti b i o ti c t h e r a p y M u lt i p l e R e .c 36. A patient 48 hours after surgery for a fractured femoral shaft is experiencing mental confusion, tachycardia, tachypnea, and dyspnea. The patients blood pressure is elevated and petechiae are present on the chest. After reporting the findings to the RN what should the nurse do while awaiting the physicians specific orders? (Select all that apply.) • Administer oxygen. om s p o n s e Identify one or more choices that best complete the statement or answer the question. Prepare patient for arterial blood gas tests. Prepare patient for chest x-ray or lung scan. Maintain bedrest and keep movement to a minimum. Ask patient to move affected limb to see if pain is worse. Place patient in high Fowlers position or raise the head of the bed. 37. A patient asks the difference between osteoarthritis and rheumatoid arthritis. What manifestations should the nurse explain are characteristic of rheumatoid arthritis? (Select all that apply.) • Low-grade fever • Heberdens nodes • Autoimmune disease • Activity increases pain • Early morning stiffness • Involvement of other major organs 38. The nurse is collecting data from a patient suspected of developing a fat embolus from a fracture of the right femur. Which manifestations should the nurse expect? (Select all that apply.) • Petechiae • A migraine • Tachycardia • Mental confusion • Numbness in the right leg • Muscle spasms in the right thigh 39. The nurse is caring for a patient in traction. Which actions are appropriate when caring for this patient? (Select all that apply.) • Allow weights to hang freely in place. • Use assistance to reposition the patient in bed. • Hold weights up if the patient is shifting position in bed. • Remove weights if the patient is being moved up in bed. • Lighten weights for short periods if the patient reports pain. 40. The nurse is contributing to the plan of care for a patient recovering from total hip replacement. Which exercises should the nurse w w w .m yn ur si ng te st pr ep • • • • • om ep .c recommend to help prevent deep vein thrombosis (DVT) formation? (Select all that apply.) • Foot circles • Toe touches • Heel pumping • Deep knee bends • Quadriceps setting • Straight leg raises (SLRs) 41. A patient in the ambulatory clinic is diagnosed with a muscle strain. What actions should the nurse instruct the patient to do to treat this injury? (Select all that apply.) • Rest the limb. • Elevate the limb. • Apply heat for 1 hour. • Apply ice to the area. • Wrap with an elastic bandage. w w w .m yn ur si ng te st pr 42. The nurse is caring for a patient with a minor rotator cuff shoulder injury. What should the nurse emphasize when reviewing care with this patient? (Select all that apply.) • Apply ice • Rest the shoulder • Take NSAIDs as prescribed • Begin out-patient physical therapy • Use 2 lb hand weights for exercising 43. During a health history the nurse becomes concerned that a patient is at risk for developing osteoporosis. Which modifiable risk factors did the nurse use to come to this conclusion? (Select all that apply.) • Small boned • Postmenopausal • Cigarette smoking • Sedentary lifestyle • Low calcium intake 44. The nurse is assisting in the development of an educational seminar on prevention of osteoporosis for a group of community members. Which actions should the nurse suggest be included in this presentation? (Select all that apply.) • Drink one cup of caffeinated coffee each day • Ensure an adequate intake of calcium each day • Participate in weight-bearing exercise every day • Wear well-supporting nonskid shoes at all times • Consider participating in resistance exercise training MULTIPLE CHOICE • ANS: B Prevention of fat emboli includes keeping the fracture immobilized and hydrating the patient to help dilute and excrete any fat that may escape from the fractured bone. A. Decreasing the consumption of fat will not help prevent fat emboli. C. D. Deep breathing and coughing and performing passive range of motion will not prevent the development of fat emboli. om PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityReduction of Risk Potential | Cognitive Level: Application st pr ep .c • ANS: B The nurse should begin with data collection to determine what the next action to take. For this patient the nurse should perform neurovascular checks. A. The arm might need to be positioned however this should not be done until a neurovascular check is completed. C. Administering pain medication might be indicted however should not be done until a pain assessment is completed. D. The nurse needs to determine the patients neurovascular status before notifying the physician. ng te PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityReduction of Risk Potential | Cognitive Level: Analysis yn ur si • ANS: D The early symptom of acute compartment syndrome is the patients report of severe, increasing pain that is not relieved with narcotics, so the physician should be notified. A. B. C. These actions might be done if prescribed by the physician. w .m PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityReduction of Risk Potential | Cognitive Level: Application w w • ANS: A Crossing the legs puts the hip at risk for dislocation. Symptoms are pain in the affected hip, shortening of the leg, and possibly rotation of the surgical leg. B. The patient did not have surgery on the right knee. C. D. The patient did not have surgery to the left limb. PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityReduction of Risk Potential | Cognitive Level: Analysis • ANS: D The nurse should begin with data collection to determine what the next action is to take. The nurse should perform a neurovascular check. A. The edges of the cast may need to be padded if this is the cause of the patients pain. B. The physician should not be notified until neurovascular checks are performed. C. The nurse needs to assess the patients pain level before providing an analgesic. PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityReduction of Risk Potential | Cognitive Level: Application ep PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityReduction of Risk Potential | Cognitive Level: Analysis .c om • ANS: A Prevention of dislocation is a major nursing responsibility. Correct positioning of the surgical leg is critical. The primary goals are to prevent hip adduction which is done by keeping the legs apart. B. C. D. These actions will not prevent hip adduction. ng te st pr • ANS: A A casted limb is elevated for 24 to 48 hours, and ice can be applied above and below the cast to reduce swelling. B. C. D. The limb is not elevated to prevent cast cracking, promote comfort, or to allow the cast to dry evenly. ur si PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityReduction of Risk Potential | Cognitive Level: Application .m yn • ANS: B A trapezoid-shaped abduction pillow (sometimes called a triangular pillow), splint, wedge, or regular bed pillows may be used between the legs to maintain abduction and prevent adduction. w w w Some research, however, indicates that these precautions may not be necessary and may slow recovery. A. D. The pillow is not used to support knee flexion or hyperextension. C. Adduction of the hip joint is to be prevented. PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityReduction of Risk Potential | Cognitive Level: Analysis • ANS: D For emergency care of a suspected fracture, do not try to reposition the limb. Splint it as it lies and ensure that the limb is secured above and below the break to minimize movement and bone grating. A. B. C. Then cover site, transport, and assess pain level. PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityReduction of Risk Potential | Cognitive Level: Application • ANS: A Because of the systemic nature of RA, in addition to pain and joint involvement, the patient may have a low-grade fever, malaise, depression, lymphadenopathy, weakness, fatigue, anorexia, and weight loss. B. C. D. Paralysis, crepitation, and shortness of breath are not manifestations of RA. om PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityPhysiological Adaptation | Cognitive Level: Analysis ep .c • ANS: C The data collection findings are normal. Since it is time for the pain medication and the patient is in pain, the medication can be given. A. B. D. There is no need to hold the medication, notify the RN, or wait to give the medication in 30 minutes. te st pr PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityPharmacological and Parenteral Therapies | Cognitive Level: Application ur si ng • ANS: C A casted limb is elevated for 24 to 48 hours, and ice can be applied above and below the cast to reduce swelling. A. The RN does not need to be notified. B. Heat should not be applied at this time. D. The pillow should not be removed from under the cast. yn PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityReduction of Risk Potential | Cognitive Level: Application w w .m • ANS: B Allopurinol decreases uric acid production. A. C. D. Allopurinol (Zyloprim) does not excrete proteins or increase the formation or metabolism of purines. w PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityPharmacological and Parenteral Therapies | Cognitive Level: Analysis • ANS: D The patient should avoid high-purine (protein) foods, such as organ meats, shellfish, and oily fish (e.g., sardines). A. B. C. These food items would be appropriate for the patient being treated for gout. PTS: 1 DIF: Moderate KEY: Client Need: Health Promotion and Maintenance | Cognitive Level: Analysis • ANS: C The patient should be instructed to avoid high-purine (protein) foods such as organ meats, shellfish, and oily fish. A. B. D. Rice, beets, and bananas do not need to be avoided. PTS: 1 DIF: Moderate KEY: Client Need: Health Promotion and Maintenance | Cognitive Level: Analysis .c om • ANS: D Pain control is a major issue with many patients with Pagets disease. The outcome stating that pain is relieved at a satisfactory level is the most appropriate for this patient. A. B. C. Outcomes that address weight gain, intake and output, and coping skills are not necessarily appropriate for this patient. ep PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityBasic Care and Comfort | Cognitive Level: Analysis te st pr • ANS: C Bucks traction does not promote bone alignment or healing but is used instead for relief of painful muscle spasms that often accompany fractures. A. Traction is not used to restrain a patient. ng PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityBasic Care and Comfort | Cognitive Level: Analysis ur si • ANS: A Legs should be kept abducted (away from center of body), so legs should not be crossed. B. C. D. These positions do not need to be avoided for the patient with a total hip replacement. .m yn PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityReduction of Risk Potential | Cognitive Level: Application w w w • ANS: C Upper extremity amputations are usually more significant than lower extremity amputations as the arms and hands are necessary for performing activities of daily living. A. B. D. Upper extremity amputations are not more debilitating because the upper extremity is more visible, the prosthetic fitting is easier for the leg, or because of a greater blood supply to the upper extremities. PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityPhysiological Adaptation | Cognitive Level: Analysis • ANS: C The earliest manifestation of fat embolism syndrome is altered mental status from a low arterial oxygen level. The patient then experiences tachycardia, tachypnea, fever, high blood pressure, severe respiratory distress, and petechiae. A. B. D. These findings are not manifestations of infection, pneumonia, or pleural effusion. PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityPhysiological Adaptation | Cognitive Level: Analysis om • ANS: A Calf pain on dorsiflexion can indicate a thrombophlebitis (Homans sign). The RN should be informed. B. The nurse should not take the time now to check the traction setup. C. Traction weight cannot be reduced without a physicians order. D. The patient should not be encouraged to exercise the limb now since a thrombophlebitis might be present. ep .c PTS: 1 DIF: Moderate KEY: Client Need: Safe and Effective Care EnvironmentManagement of Care | Cognitive Level: Application te st pr • ANS: A Patients facing surgery and especially a body image changing surgery such as amputation will experience anxiety. Interventions to aid with this anxiety should be planned. B. C. D. These would be appropriate after surgery has occurred. ng PTS: 1 DIF: Moderate KEY: Client Need: Psychosocial Integrity | Cognitive Level: Application yn ur si • ANS: C The patient lies supine with pillow under right knee if a continuous passive motion (CPM) machine is not used after a total knee replacement. A. B. D. The patient recovering from a total knee replacement does not need to be placed in the prone, side lying, or supine position with pillows between the legs. w .m PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityBasic Care and Comfort | Cognitive Level: Analysis w w • ANS: C The wrist is rested to reduce inflammation, and a wrist splint may be prescribed to do this. A. B. D. Bedrest, an arm sling, and hand exercises are not indicated for treatment of this syndrome. PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityBasic Care and Comfort | Cognitive Level: Analysis • ANS: D The nurse should ask the patient to lift straight up using a trapeze mounted above the bed and slide a bedpan underneath from the right side to avoid the left fracture. A. The patient is on bedrest so a bedside commode is not appropriate. B. The patient should not be turned. C. The patient should be instructed to use the trapeze and not attempt to push self up using the bed. PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityBasic Care and Comfort | Cognitive Level: Application om • ANS: A The diagnosis of gout is based on an elevated serum uric acid level which is a waste product resulting from the breakdown of proteins. Urate crystals, formed because of excessive uric acid buildup, are deposited in joints and other connective tissues, causing severe inflammation. B. C. D. Creatinine, blood urea nitrogen, and lipoprotein levels are not used in the diagnosis or treatment of gout. .c PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityReduction of Risk Potential | Cognitive Level: Analysis te st pr ep • ANS: A If serum calcium falls below normal levels, the parathyroid glands stimulate the bone to release calcium into the bloodstream. The result is demineralized bone. Therefore, calcium supplements are used. B. C. D. Calcium is not taken to increase energy levels, decrease serum calcium, or to increase the excretion of calcium. si ng PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityPharmacological and Parenteral Therapies | Cognitive Level: Analysis .m yn ur • ANS: A Osteoporotic bone may cause a pathological fracture in which the hip breaks before the fall. For other patients, a fall can cause a hip or other fracture. B. C. D. Bone overgrowth, spurs, or increases in bone density are not complications of osteoporosis. w PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityPhysiological Adaptation | Cognitive Level: Analysis w w • ANS: C A risk factor for osteoporosis is excessive caffeine intake or alcohol. A. B. D. Antacids, walking, and dairy intake are not risk factors for the development of osteoporosis. PTS: 1 DIF: Moderate KEY: Client Need: Health Promotion and Maintenance | Cognitive Level: Application • ANS: B Ibuprofen (an NSAID) blocks activity of the enzyme cyclooxygenase, which makes prostaglandins that produce inflammation, fever, and pain found in rheumatoid arthritis. A. Digoxin is a cardiac medication. C. Morphine is an opioid which may not help reduce inflammation. D. Penicillin is an antibiotic, used to treat bacterial infections. PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityPharmacological and Parenteral Therapies | Cognitive Level: Analysis ep pr PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityReduction of Risk Potential | Cognitive Level: Application .c om • ANS: A The nurse should notify the RN. A serious complication of a cast being too tight is compartment syndrome. The physician needs to be contacted for orders to cut the cast with a cast cutter to relieve pressure and prevent pressure necrosis of the underlying skin. B. There is no information to support that the patient is in pain. C. There is no information to support that the limb is cool. D. The limb should be elevated or supported with pillows. si ng te st • ANS: D A bone splintered or shattered into numerous fragments is a comminuted fracture that often occurs in crushing injuries. A. Impacted describes a bone that is forcibly pushed together, resulting in bone being pushed into bone. B. Avulsion describes a piece of bone that is torn away from the main bone while still attached to a ligament or tendon. C. Greenstick describes a bone that is bent and fractures on the outer arc of the bend. yn ur PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityPhysiological Adaptation | Cognitive Level: Application w w .m • ANS: D Washing hands prior to touching a fracture area is the best way to help prevent osteomyelitis. C. Calcium is related to osteoporosis prevention. B. Keeping the leg immobilized relates to fat emboli reduction. A. Ice is applied to reduce swelling. w PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityReduction of Risk Potential | Cognitive Level: Analysis • ANS: C Acetaminophen can be helpful in reducing pain associated with osteoarthritis, so the nurse should assess whether the patient is satisfied with the current level of pain control. A. Calcium supplementation is not related to pain control. B. D. These statements miss the opportunity to assess whether the patient is both comfortable and functional with the current pain management. PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityBasic Care and Comfort | Cognitive Level: Application .c PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityPhysiological Adaptation | Cognitive Level: Application om • ANS: D Long-term antibiotic therapy (4-6 weeks) is the treatment of choice for patients with osteomyelitis. A. Anticoagulant therapy is prescribed for a thromboembolism. B. Casting is indicated for a fracture. C. Fasciotomy may be indicated to treat compartment syndrome. ep MULTIPLE RESPONSE te st pr • ANS: A, B, C, D, F The patient is likely experiencing a fat emboli. The patient should be placed in a high Fowlers position to aid breathing, diagnostic tests will be done, and the patient is kept on bedrest to reduce oxygenation needs and clot movement. Oxygen may be started per agency policy to aid in respiration. E. Limb should not be moved to prevent further release of fat. si ng PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityReduction of Risk Potential | Cognitive Level: Application .m yn ur • ANS: A, C, E, F Rheumatoid arthritis is a systemic autoimmune disease with morning stiffness, low-grade fever, and organ involvement. B. Heberdens nodes are seen in osteoarthritis. D. Pain increases with activity in osteoarthritis. w PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityPhysiological Adaptation | Cognitive Level: Application w w • ANS: A, C, D The earliest manifestation of fat emboli syndrome (FES) is altered mental status from a low arterial oxygen level. The patient then experiences tachycardia, tachypnea, fever, high blood pressure, severe respiratory distress, and petechiae. B. E. F. These are not manifestations of fat emboli. PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityPhysiological Adaptation | Cognitive Level: Analysis • ANS: A, B Weights are to hang unobstructed. Assistance should be used to pull the patient up in bed to protect the health care worker from injury. C. D. E. Weights should never touch the floor or be removed or lifted. PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityReduction of Risk Potential | Cognitive Level: Application ep .c PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityReduction of Risk Potential | Cognitive Level: Application om • ANS: A, C, E, F Because most DVTs occur in the lower extremities, leg exercises are started in the immediate postoperative period and include heel pumping, foot circles, and SLRs. The patient also performs quadriceps-setting exercises (quad sets). B. D. Deep knee bends and toe touches are not standard postoperative exercises and would be restricted in a patient with a total hip replacement due to restricted hip flexion. si ng te st pr • ANS: A, B, D, E RICE is an acronym for rest, ice, compression, and elevation which is the therapy for strain injuries. Immediately after a strain, the injured area should be rested to protect it. Ice should be applied to decrease pain, swelling, and inflammation. Applying an elastic bandage for compression and elevating the affected area provide support and minimize swelling. C. After inflammation subsides, heat application (15 to 30 minutes four times a day) brings increased blood flow to the injured area for healing. Heat should not be immediately applied for 1 hour. yn ur PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityReduction of Risk Potential | Cognitive Level: Application w .m • ANS: A, B, C, D For minor rotator cuff injury, resting the shoulder, ice, NSAIDs, and physical therapy are recommended. E. The use of hand weights will be determined by the physical therapist. w w PTS: 1 DIF: Moderate KEY: Client Need: Physiological IntegrityReduction of Risk Potential | Cognitive Level: Application • ANS: C, D, E Modifiable risk factors for the development of osteoporosis include cigarette smoking, sedentary lifestyle, and low calcium intake. A. B. Bone structure and menopausal status are non-modifiable risk factors for the health problem. PTS: 1 DIF: Moderate KEY: Client Need: Health Promotion and Maintenance | Cognitive Level: Analysis • ANS: B, C, D, E .c om Actions to prevent the development of osteoporosis include ensuring an adequate intake of calcium each day, participating in weightbearing exercise such as walking each day, wearing well-supporting, nonskid shoes at all times, and participating in resistance exercise such as weight training. A. Caffeine is a modifiable risk factor for the development of osteoporosis. Chapter 26 Ambulatory Aids 1. A 15-year-old patient complains of left ankle pain after being tackled while playing football. He asks the nurse what tests he needs to have to determine if he has a strain or a fracture. How should the nurse reply? • You dont need an x-ray; I can tell by the way your ankle looks and feels whether you have a strain Sprains, strains, and fractures have similar symptoms at first; you will need an x-ray of the joint to • We will need to get a venous Doppler study to make sure that there is not a fracture. pr ep • An arterial Doppler will show whether the blood flow is interrupted, which is common for fracture 2. The nurse caring for a frail, malnourished, immobile patient recognizes which of the following as the best treatment to protect the patients integument? • Offering the patient 6 small meals a day si ng te st • Assisting the patient to sit in a chair 3 times a day • Turning the patient at least every 2 hours yn ur • Administering fluid boluses as directed by the healthcare provider 3. A 32-year-old male construction worker presents to the emergency department with complaints of headache, abdominal cramps, nausea, lightheadedness, and extreme fatigue. The patient states he started feeling ill while at the job site. The nurse gathers the following data: T = 99.8F, P = 96, RR = 36, and BP = 136/72. The patients skin is cold and clammy, and the patient is having difficulty answering questions. He tells the nurse that he is never sick, takes no medicines, and has never been in the hospital. What additional information would be most useful in determining whether he is experiencing heat exhaustion (hyperthermia)? • Past medical and surgical history w w w .m • • Immunization history • Dietary intake for the past 24 hours • • Environmental temperature 4. What action is most important in limiting the nurses risk of back injuries? Use good body mechanics at all times. • Work with another nurse or an aide when lifting and turning patients. • Avoid manual lifting by using assistive devices as often as possible. Develop a lift team at the clinical site. 5. The nurse is helping the patient to perform leg exercises after surgery to prevent thrombophlebitis. Which type of muscle is the patient using for these exercises? • Skeletal • Smooth • Cardiac Slow-twitch fibers 6. A nurse is caring for a 25-year-old male quadriplegic patient. Which of the following treatments would the nurse perform to decrease the risk of joint contracture and promote joint mobility? • Active ROM • Passive ROM pr Turning the patient every 2 hours st • ep .c • om • Administering glucosamine supplements 7. A nurse is assessing a 74-year-old male patient for an exercise program to be offered at the local hospital. During the evaluation, the nurse notes the following vital signs: P = 72, RR = 16, BP = 132/70. After 3 minutes of moderate-intensity running on the treadmill, the patient becomes short of breath and states, I have to stop. I cant do this anymore. The nurse measures his vital signs again: P = 152, RR = 40, BP = 172/98. She instructs him to rest. Vital signs return to baseline after 15 minutes. The nurse should recognize his symptoms as associated with which of the following? .m yn ur si ng te • COPD • Orthostatic hypotension • Limited activity tolerance w Impending respiratory failure 8. What is the correct method for turning an adult patient who recently sustained a spinal cord injury? • Ask the patient to assist with the turn by holding the side rails of the bed. w • w • • Place a draw sheet under the patient to assist with turning. • Request help from another nurse to perform the logrolling technique. • Use a mechanical lift for safe turning and protecting the nurses back. 9. An older patient with newly diagnosed osteoporosis asks the nurse to explain her health problem. Which of the following is the correct description of osteoporosis? • Loss of bone density that increases the risk of fracture • Degenerative joint disease that produces pain and decreased function • Chronic inflammatory joint disease that must be treated with steroids Serious infection in the bone that must be treated with antibiotics 10. When caring for a patient with osteoporosis, which of the following is the most important action to take to minimize progression of the disease? • Take a calcium supplement twice a day. Start a weight-bearing exercise program. • Avoid any strenuous activity. .c • om • Schedule regular healthcare checkups. 11. Which course of action taken by her patient with osteoporosis would allow the nurse to know that her teaching was effective? • Taking a calcium supplement every day and increasing her phosphorous intake pr ep • Participating in a low-impact aerobic exercise program at the gym three times a week • Using a wheelchair to reduce the risk of spontaneous fractures to her legs and feet te ng • Seeking healthcare by scheduling a follow-up examination with bone density testing 12. Which of the following is true of synarthroses? Joints are: Freely movable. si • st • Capable of only limited movement. • Immovable. Painful with movement. 13. A man has been admitted to the hospital unit with a medical diagnosis of chronic obstructive pulmonary disease (COPD). He is receiving supplemental oxygen at 2 L/min via nasal cannula. Which positioning technique will best assist him with his breathing? w w .m yn • ur • Fowlers position • Sims position • w • Lateral recumbent position • Lateral position 14. A nurse has been asked to design an exercise program with the goal of increasing a clients muscular strength and endurance. Which exercise program would specifically focus on meeting that goal? • Flexibility training • Resistance training • • • Aerobic conditioning Anaerobic conditioning 15. In order to achieve balance, body mass must be distributed around which point? Center of body alignment • Center of balance • Center of gravity • Isometric toning of lower legs ep Quadriceps and gluteal repetitions pr • .c Base of support 16. A frail 78-year-old man is admitted to the hospital after a fall at home resulted in a left hip fracture. After surgery, he is to begin ambulating with a walker but must avoid weight- bearing on his left lower leg. What is the best intervention to help him use his walker? • Aerobic exercise with deep breathing om • Arm resistance training 17. Identify the most appropriate nursing diagnosis for promoting the safety of a frail, elderly patient after hip replacement surgery, who also has a history of emphysema. • Impaired Mobility related to weakness ng te st • Ineffective Breathing Pattern related to disease process • Activity Intolerance related to injury si • Risk for Injury related to medical condition 18. What would be the most appropriate goal for a frail, elderly patient with a nursing diagnosis of Risk for Injury after hip surgery? • Remain free from injury or falls throughout hospital stay. .m yn ur • Increase activity tolerance by discharge from hospital. • Demonstrate effective breathing when ambulating. w Increase mobility by discharge from hospital. 19. A 16-year-old was hospitalized 3 weeks ago. He has been confined to bed throughout his hospital stay because of a crushed pelvis. His parents tell the nurse, Our son is just staring off w • w • into space; he wont talk to us. We are worried because he has not even listened to his music CDs, watched television, or played his video games for 2 days. That is so unlike him. What is the best response the nurse can make? • I will inform his physician and see if we can get your son started on an antidepressant. He is at a critical time in his life; adolescents are often moody, and being in the • • hospital with an inj that worse. Your son had a major injury, and his immobility can cause feelings of isolation and depression. He is bored because he has been in the hospital for 3 weeks; Ill try to find some new activities for h 20. A healthy, 32-year-old man wants to start a fitness program to increase his muscle tone and muscle strength. What advice should the nurse offer him? The United States Department of Health and Human Services recommends: • That exercising even once a week is beneficial. om • 30 minutes or more of moderate-intensity physical activity three times a week. • 1 hour, three times a week of moderate-intensity physical activity. ep .c • 150 to 300 minutes or more of moderate-intensity physical activity per week. 21. A patient fractured her right ulna 8 weeks ago and has just had her cast removed. The orthopedic surgeon prescribes isometric exercises for the right arm. Which of the following exercises comply with the surgeons orders? • Place a foam ball in the right hand and squeeze; hold the squeeze position for 6 to 8 seconds, and re ng te st pr • si Grasping the right wrist with the left hand, move the right arm up, down, and side to side; hold eac • seconds, and repeat 5 to 10 times. • yn ur Grasping the right wrist with the left hand, pull the right arm across the body; hold this position for repeat 5 to 10 times. Press the right hand against a wall; hold this position for 6 to 8 seconds, and repeat 5 to 10 times. 22. A patient is on strict bed rest for 5 days. During this time he has not had a bowel movement; normally, he passes stools daily. He describes feeling bloated and uncomfortable. What information should the nurse give the patient when explaining constipation? • Immobility often causes constipation. w w w .m • • A stool softener daily will relieve the problem. • Use of a bedpan results in bloating and constipation. • A low-fiber diet will resolve the problem. 23. A patient is on strict bed rest for 5 days. During this time he has not had a bowel movement; normally, he passes stools daily. He describes feeling bloated and uncomfortable. A nursing diagnosis that would best address a patient who is on bed rest is Constipation related to: • Change in previous pattern. • Immobility. • Dietary intake. Change in environment. 24. A 32-year-old paraplegic has been admitted to the hospital for antibiotic therapy to treat pneumonia. He lives independently and has developed strong upper-body strength to maximize his independence. Which transfer device should be used when transferring him from the bed to his wheelchair? • Mechanical lift • Draw sheet .c Transfer belt ep • om • Transfer board 25. An 82-year-old patient is unsteady on her feet when transferring her position in the room. She reports feeling a little sore but has no complaints of weakness. What is the appropriate piece of equipment to use when helping her ambulate? • Crutches • Cane ng Transfer belt si • te st pr • Walker 26. The nurse is helping an 82-year-old patient to ambulate in the hallway. Suddenly she states, I feel so light-headed and weak, as her knees begin to buckle. The nurses best action at this time would be to: • Assist the patient to slide down his leg as he guides her to a seated or lying position. .m yn ur • Grab her under the arms and hold her up as he calls for assistance. • Immediately release the transfer device and place a wheelchair behind the patient to prevent a fall. w Instruct the patient to grab the rail in the hallway while he calls for assistance. 27. According to the U.S. Department of Health and Human Services 2008 Physical Activity Guidelines for Americans, which of the following statements about the benefits of physical activity is correct? • The risks of physical activity outweigh the health benefits. w • w • • Physical activity in excess of recommendations for age is harmful. • Combining aerobic and muscle-strengthening activities promotes better health. • Lesser amounts of activity provide little to no health benefits. 28. When encouraging a fitness program for older adults, what must the nurse consider? • Older adults should engage in 75 to 150 minutes of moderate-intensity physical activity per week. • More than 150 minutes of moderate-intensity physical activity can be harmful to bones. • Structured calisthenics programs achieve greater health benefits for older adults. • Older adults at risk for falling should do activities that maintain or improve balance. Multiple Response Identify one or more choices that best complete the statement or answer the question. • Skeleton .c Muscles ep • om 1. Which of the following body systems must interact to produce mobility and locomotion? Choose all that apply. • Digestive system Nervous system 2. Which of the following patients would you expect to be at risk for decreased activity? Choose all that apply. • Older adult who walks at the mall for physical activity st pr • Someone living in a skilled nursing facility • Healthy adult who works as a computer programmer ng te • Obese child who enjoys video games 3. A patient has started a fitness program. What program features illustrate that he has started a well-rounded program? • Flexibility yn ur si • Isometric exercises • Resistance training .m • Aerobic conditioning 4. The nurse is instructing a patient about the need to replace fluid before, during, and after exercise in order to avoid dehydration. She should teach the patient to determine the amount of fluid to consume on the basis of: • Duration of exercise w w w • • Environmental temperature. • Level of fitness. • Degree of thirst. 5. Which of the following actions represent proper body mechanics for nurses providing care as well as teaching patients about safe body movements? Choose all that apply. • Stand with the body in alignment and erect posture. • Bend at the waist to lift heavy objects from the floor. • Use a wide base of support with your feet at shoulder width. • Keep objects close to your body when carrying them. om MULTIPLE CHOICE • ANS: 2 Signs and symptoms associated with a sprain, strain, or fracture are the same. An x-ray allows the medical provider to visually observe for any breaks in a bone. A venous or arterial Doppler is used to detect blood flow. w w w .m yn ur si ng te st pr ep .c PTS: 1 DIF: Easy REF: V1, m 763 KEY: Nursing process: Interventions | Client need: PHSI | Cognitive level: Application • ANS: 3 External pressure from lying or sitting in one position compresses capillaries and obstructs blood flow to the skin. Immobile patients confined to a bed should be turned at least every 2 hours to protect their skin and relieve pressure. PTS: 1 DIF: Easy REF: V1, m 768 KEY: Nursing process: Interventions | Client need: SECE | Cognitive level: Comprehension • ANS: 4 The patient has an elevated temperature, pulse, and respiratory rate. He developed these symptoms while at work. Lightheadedness, nausea, headache, fatigue, hyperventilation, loss of concentration, abdominal cramps, increased body temperature, and cold and clammy skin are signs of heat exhaustion. The nurse would gather information about any strenuous physical work he may have been doing (which produces heat) and whether the temperature of his environment was too warm to allow his body heat to dissipate. In addition, inadequate fluid intake can cause an elevated temperature; however, the environmental conditions are most telling. PTS: 1 DIF: Difficult REF: V1, m 761 KEY: Nursing process: Diagnosis | Client need: PHSI | Cognitive level: Analysis • ANS: 3 Back injuries are the leading cause of injury among nurses. Good body mechanics and teamwork limit the risk of injury. However, the ANA Handle with Care program advocates the regular use of assistive devices as well as avoiding manual lifting. PTS: 1 DIF: Moderate REF: V1, m 769 KEY: Nursing process: Interventions | Client need: SECE | Cognitive level: Analysis • ANS: 1 Skeletal muscle moves the bones with ligaments. Smooth muscle is found in the digestive tract and other hollow structures, such as the blood vessels and bladder. Cardiac muscle contracts spontaneously and is blood ejected out of the heart. Slow-twitch fibers are a subtype of skeletal muscle cell. Slow-twitch fibers (type I), or red muscle, have a rich blood supply and are te st pr ep .c om rich in mitochondria (the powerhouse of the cell) to give the muscle more oxygen and energy to sustain aerobic activity. The fast-twitch fibers (type II skeletal muscle type) are known as white muscle. These fibers increase the speed of muscle contraction. PTS: 1 DIF: Easy REF: V1, m 752 KEY: Nursing process: Interventions | Client need: PHSI | Cognitive level: Application • ANS: 3 Passive ROM involves moving the joints through their ROM when the patient is unable to do so for himself. Passive ROM promotes joint mobility. Active ROM would not be possible for a quadriplegic patient. Turning the patient every 2 hours prevents skin breakdown but does not promote mobility or prevent contracture. Glucosamine is a building block for the formation and repair of cartilage. However, there is inconclusive, scientific evidence regarding the benefit of this substance to improve joint function. PTS: 1 DIF: Moderate REF: V1, m 754; higher-order item, answer can be derived from text | V1, m 776; higher-order item, answer can be derived from text KEY: Nursing process: Interventions | Client need: PHSI | Cognitive level: Application • ANS: 3 w w w .m yn ur si ng To assess for activity tolerance, assess and record vital signs before and after exercise. A rapid change from baseline vital signs or a slow return to baseline indicates limited activity tolerance. COPD, a form of chronic lung disease, would primarily exhibit signs of shortness of breath, difficulty getting enough air, fatigue, and elevated heart rate during exercise. In this scenario, the blood pressure is elevated, which is not a predominant finding with COPD. Air hunger signals impending respiratory failure. Orthostatic hypotension is a temporary lowering of blood pressure when suddenly standing up. It is not a finding related to exercise. PTS: 1 DIF: Moderate REF: V1, m 767 KEY: Nursing process: Diagnosis | Client need: SECE | Cognitive level: Analysis • ANS: 3 The patients spine should be maintained in straight alignment. Logrolling moves the patients body as a unit and maintains the patients spine in straight alignment. Holding on to the side rail or using a draw sheet or mechanical lift will not keep the spine in alignment. PTS: 1 DIF: Difficult REF: V1, m 773 | V2, m 748 KEY: Nursing process: Interventions | Client need: PHSI | Cognitive level: Application • ANS: 1 Osteoporosis is a decrease in total bone density. The internal structure of the bone diminishes, and the bone collapses in on itself. Women experience a rapid decline in bone mass after menopause. Osteoarthritis is a degenerative joint disease. Osteomyelitis is a serious infection in the bone. .m yn ur si ng te st pr ep .c om PTS: 1 DIF: Easy REF: V1, m 762 KEY: Nursing process: Interventions | Client need: PHSI | Cognitive level: Comprehension • ANS: 2 Osteoporosis causes bones to become porous and weak. Starting a weight-bearing exercise program is the most important aid in promoting bone strength and decreasing the rate of bone loss. Calcium supplementation helps maintain bone density. PTS: 1 DIF: Moderate REF: V1, m 762 KEY: Nursing process: Planning | Client need: PHSI | Cognitive level: Application • ANS: 2 Active participation in an aerobic exercise program demonstrates not only understanding of the treatment of osteoporosis but commitment to an action plan to reduce bone loss that comes with osteoporosis. Calcium supplementation is also part of the treatment for osteoporosis. However, high phosphorous intake lowers calcium levels and would not be appropriate for a client with osteoporosis. Restricting weight-bearing activity to a wheelchair will actually lower bone density. Although followup care is appropriate for a client with osteoporosis, it does not indicate commitment to a daily treatment plan. PTS: 1 DIF: Easy REF: V1, m 762 KEY: Nursing process: Evaluation | Client need: PHSI | Cognitive level: Analysis • ANS: 3 Synarthroses joints are immovable joints. The sutures between the cranial bones are considered synarthroses joints. Although these joints have some flexibility in youth to allow for growth, they gradually become rigid and immovable with age. There is no pain associated with synarthroses. PTS: 1 DIF: Moderate REF: V1, m 752 KEY: Cognitive level: Recall • ANS: 1 Fowlers position is a semisitting position in which the head of the bed is elevated 45 to 60 degrees. This position promotes respiratory function by lowering the diaphragm and allowing the w w w greatest chest expansion. Sims position is a side-lying position where the patient is on his left side with left leg extended and right leg flexed. This position is commonly used for rectal examination. Lateral recumbent position is another term describing Sims position. Lateral position simply means side lying. PTS: 1 DIF: Moderate REF: V1, m 771 KEY: Nursing process: Interventions | Client need: PHSI | Cognitive level: Application • ANS: 2 Resistance training involves movement against resistance, which increases muscular strength and endurance. Most commonly, resistance training refers to weight lifting and isotonic movement. When exercising for strength, the amount of resistance is increased with each exercise. When exercising for endurance, the number of repetitions is increased with each exercise. Flexibility training will not increase w w w .m yn ur si ng te st pr ep .c om muscular strength. Aerobic and anaerobic conditioning may have some benefit on strength and endurance, but their primary focus is cardiovascular conditioning. PTS: 1 DIF: Moderate REF: V1, m 756 KEY: Nursing process: Planning | Client need: HPM | Cognitive level: Analysis • ANS: 3 Balance is achieved when the body is in alignment. To be balanced, a persons line of gravity must pass through his center of gravity, and the center of gravity must be close to his base of support. The center of gravity is the point around which mass is distributed. PTS: 1 DIF: Easy REF: V1, m 754 KEY: Nursing process: Assessment | Client need: HPM | Cognitive level: Comprehension • ANS: 4 Arm strength is necessary for ambulating with a walker and other assistive devices. Upper body resistance training increases muscles strength and tone, which will aid him in using the walker more easily. Toning the lower body through exercise of the quadriceps and gluteal muscles, although important for regaining strength in general after surgery, does not aid in using a walker. Aerobic exercise with deep breathing produced the greatest benefit to the cardiovascular health and does little to improve the upper body strength needed for ambulating with an assistive device. PTS: 1 DIF: Moderate REF: V1, pp. 755-756; not a direct response to the item | V1, m 779; not a direct response to the item KEY: Nursing process: Interventions | Client need: PHSI | Cognitive level: Application • ANS: 4 The patients medical condition places him at an increased Risk for Injury: He is at risk for falls and for further injury to his hip. The patient does have Impaired Mobility; however, his Impaired Mobility puts him at Risk for Injury. A diagnosis of Impaired Mobility would focus the outcomes on improving his mobility rather than protecting him from further injury. We have no data other than a diagnosis of emphysema to indicate that he is experiencing Ineffective Breathing Pattern. He is experiencing Activity Intolerance, but this is not his primary safety risk. A diagnosis of Activity Intolerance would focus the goals on increasing his endurance and conserving his energy. PTS: 1 DIF: Moderate REF: V1, m 767 KEY: Nursing process: Diagnosis | Client need: SECE | Cognitive level: Synthesis • ANS: 1 Remaining free from injury or falls is a measurable goal, and it is directly related to the patients nursing diagnosis, Risk for Injury. Increasing activity tolerance and mobility by the time of discharge is not specific and measurable. Additionally, these outcomes do not relate to Risk for Injury. A goal of effective breathing for a frail, elderly patient after hip surgery does not relate to Risk for Injury. w w w .m yn ur si ng te st pr ep .c om PTS: 1 DIF: Easy REF: V1, m 767 KEY: Nursing process: Planning | Client need: SECE | Cognitive level: Application • ANS: 3 Being immobile, whether in the hospital or home, leads to isolation and mood changes. Patients who are in bed for long periods can suffer from psychological changes such as depression, anxiety, hostility, sleep disturbances, and changes in their ability to perform self-care activities. PTS: 1 DIF: Moderate REF: V1, m 765 KEY: Nursing process: Diagnosis | Client need: PSI | Cognitive level: Analysis • ANS: 4 Exercise involves physical activity and increases muscle tone and strength. The U.S. Department of Health and Human Services recommends 150 to 300 minutes or more of moderate- or vigorousintensity physical activity per week. PTS: 1 DIF: Moderate REF: V1, m 757 KEY: Nursing process: Interventions | Client need: HPM | Cognitive level: Comprehension • ANS: 4 Isometric exercise involves muscle contraction without motion. Isometric exercises are useful for developing strength. This type of exercise is appropriate for the patient who has had an extremity confined to a cast because muscle atrophy occurs when the muscle is not used. PTS: 1 DIF: Difficult REF: V1, m 755 KEY: Nursing process: Interventions | Client need: PHSI | Cognitive level: Application • ANS: 1 Immobility slows peristalsis, which leads to constipation, gas, and difficulty evacuating stools from the rectum. Increasing fiber in the diet often prevents constipation. A stool softener may be ordered if other measures are unsuccessful. Some people do find use of a bedpan difficult. PTS: 1 DIF: Easy REF: V1, m 763 KEY: Nursing process: Interventions | Client need: PHSI | Cognitive level: Comprehension • ANS: 2 Immobility slows peristalsis, which leads to constipation, gas, and difficulty evacuating stools from the rectum. Based on the scenario, this nursing diagnosis would specifically address the patients condition. PTS: 1 DIF: Moderate REF: V1, m 763; higher-order item with implied answer KEY: Nursing process: Diagnosis | Client need: PHSI | Cognitive level: Analysis • ANS: 4 A transfer board is used by patients with longstanding mobility problems; it offers them the greatest amount of independence while ensuring safety. Patients using a transfer board should have sufficient upper-body strength to perform the transfer safely. A mechanical lift could be used, but it does not promote independence. A transfer belt is used for clients who are able to stand. A draw sheet is useful for moving a patient in bed rather than from bed to wheelchair. PTS: 1 DIF: Easy REF: V1, m 775 KEY: Nursing process: Evaluation | Client need: SECE | Cognitive level: Comprehension w w w .m yn ur si ng te st pr ep .c om • ANS: 2 Crutches are commonly used when the patient has an injured lower extremity. A cane or walker is generally used for the patient with a lower extremity injury or weakness. The most appropriate equipment to use would be a transfer belt. A transfer belt allows the patient the greatest amount of independence while ensuring safety. PTS: 1 DIF: Easy REF: V1, pp. 775-776 KEY: Nursing process: Interventions | Client need: SECE | Cognitive level: Application • ANS: 1 If a patient becomes weak or begins to fall when walking, do not attempt to hold the patient up. Instead, protect the patient as you guide her to a seated or lying position. Create a wide base of support, and project forward the hip closest to the patient. Assist the patient to slide down your leg as you call for help. Protect the patients head as her body descends. PTS: 1 DIF: Moderate REF: V1, m 778 KEY: Nursing process: Interventions | Client need: SECE | Cognitive level: Application • ANS: 3 The combination of aerobic and bone- and muscle-strengthening physical activities leads to health benefits for people of all ethnic groups and ages. Physical activity is safe for almost everyone, and the health benefits of physical activity far outweigh the risks. Additional health benefits are provided by increasing to 300 minutes a week of moderate-intensity aerobic physical activity, or 150 minutes a week of vigorous-intensity physical activity, or an equivalent combination of both. For all individuals, some activity is better than none. PTS: 1 DIF: Easy REF: V1, m 757 KEY: Nursing process: Planning | Client need: HPM | Cognitive level: Recall • ANS: 4 Rationale: Older adults should do exercises that maintain or improve balance if they are at risk of falling. Older adults should follow the adult guidelines, which are for 150 minutes per week of moderate-intensity or 75 minutes per week of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate- and vigorous-intensity aerobic physical activity. Aerobic activity should be performed in periods of at least 10 minutes, preferably spread throughout the week. If this is not possible because of limiting chronic conditions, older adults should be as physically active as their abilities allow. They should avoid inactivity. Structured calisthenics programs are no more beneficial for achieving health benefits than other forms of moderate- and vigorous-intensity physical activity. Structured fitness programs can become boring for some individuals. A varied routine often improves compliance and consistency of exercise. PTS: 1 DIF: Easy REF: V1, m 757 | V1, pp. 759-760 om KEY: Nursing process: Planning | Client need: HPM | Cognitive level: Application MULTIPLE RESPONSE 1. ANS: 2, 3, 4 Activity and exercise require bodily movement (mobility) and locomotion (self-powered movement from one place to another). Mobility depends on the successful interaction among the skeleton, the muscles, and the nervous system. PTS: 1 DIF: Easy REF: V1, m 751 KEY: Client need: PHSI | Cognitive level: Recall 2. ANS: 2, 3, 4 w w w .m yn ur si ng te st pr ep .c The person who lives in a skilled nursing facility might be sedentary because of advancing age and other age-associated medical problems that lead to inactivity. With obesity, movement becomes more difficult and strain on joints increases. A sedentary lifestyle, whether adult or child, contributes to obesity; activities, such as computer work and video games, are sedentary and require little physical activity. Physical activity doesnt have to be a structured fitness class but can also be walking, even walking in a mall or neighborhood, just as long as the intensity is vigorous. PTS: 1 DIF: Moderate REF: V1, m 751 | V1, m 767 KEY: Nursing process: Assessment | Client need: HPM | Cognitive level: Comprehension 3. ANS: 1, 3, 4 Flexibility training helps warm up the muscles and prevents injury during exercise. Resistance training increases muscular strength and endurance. Aerobic conditioning affects fitness and body composition. Isometric exerciseis an active form of physical activity using opposing resistance where the joints dont move and muscles dont lengthen, Isometrics are done in static positions, rather than moving through a range of motion. PTS: 1 DIF: Moderate REF: V1, pp. 755-756 KEY: Nursing process: Evaluation | Client need: HPM | Cognitive level: Comprehension 4. ANS: 1, 2 Lost fluids must be replaced to decrease the risk of dehydration, regardless of level of fitness. During intense exercise, the body can lose 2 liters of fluid for every hour of exercise. Elevated environmental temperatures also increases the amount of fluid lost through sweating. When athletes drink according to thirst, the risk that they will over-drink and so develop exercise- associated hyponatremia is minimized (Noakes, 2007). On the other hand, exercise can suppress thirst, making it an unreliable signal to replace fluids lost with exercise. PTS: 1 DIF: Easy REF: V1, pp. 758-759; answer can be derived from the text KEY: Nursing process: Interventions | Client need: PHSI | Cognitive level: Application 5. ANS: 1, 3, 4 Proper body mechanics involves good body alignment, erect posture, and Chapter 27 Perioperative Care MULTIPLE CHOICE • The circulating nurse notes that the anesthetized patient has tensed muscles and irregular respirations. The nurse is aware that the patient has reached stage: • I and the patients hearing is amplified. II and the surgical environment should be kept quiet. • III and the patient has depressed reflexes. IV and the patient will not depend on the anesthesia machine of oxygenations. ANS: B Quiet must be maintained while the patient is in stage II, because noise may cause the patient to become excited, resulting in instability of vital signs. st pr ep • .c • om a wide base of support. To prevent back injury resulting from reaching and straining muscles, carry objects close to the trunk. Bending at the waist to lift objects uses the back muscles and increases the risk of injury. Instead, squat to lower your center of gravity, and use your leg muscles for lifting. yn ur si ng te DIF: Cognitive Level: Comprehension REF: m 736, Box 37-3 OBJ: Theory #5 TOP: General Anesthesia KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • In order for the anesthesiologist to accurately calculate the amount of anesthesia needed for an 82-year-old patient, the nurse should have data available on the chart, such as: • time of last meal. pulse rate and blood pressure. • respiratory rate and oxygen saturation. w w • .m • w h e i g h t a n d w e i pr ep .c om g h t . A N S : D Accurate height and weight are significant for calculation of the anesthetic agents needed for elderly patients. DIF: Cognitive Level: Comprehension REF: m 736, Elder care OBJ: Theory #3 TOP: Anesthesia KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: pharmacological therapies • The illiterate patient signs the surgical consent form with an X. The nurse is aware that this X is: • not an acceptable signature. required to be accompanied by a picture identification. • legal if it is witnessed. te st • acceptable if the surgeon is willing. ANS: C An X is an acceptable signature if it is witnessed. DIF: Cognitive Level: Comprehension REF: m 737 OBJ: Theory #8 TOP: Surgical Consent KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care • A 16-year-old boy injured in a motorcycle accident is unconscious and cannot sign the emergency surgical consent form; no family members can be located. The nurse anticipates that the: • hospital social worker can sign the permit. w w w .m yn ur si ng • • surgeon will write a detailed note about the need for surgery and a registered nurse will then sign th • opinion of a second surgeon is sought regarding the necessity of the surgery. • hospital attorney must authorize the surgery and sign the consent form. ANS: C If no family can be found to sign the permit for an unconscious person, a second surgeon can confirm the need for the immediate surgical intervention and the procedure will take place. DIF: Cognitive Level: Application REF: m 737 OBJ: Theory #8 TOP: Surgical Consent KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: coordinated care • The nurse discovers that the signed operative permit has misspelled the patients name. The nurse must: request a corrected consent form to be signed. • inform the surgeon of the error. • have the new form attached to the old incorrect one and document it. om • allow the patient to be taken to surgery after notifying the circulating nurse. ANS: A A new consent form must be made, signed, and witnessed, provided the patient has not been sedated already. DIF: Cognitive Level: Application REF: m 737 OBJ: Theory #8 TOP: Incorrect Surgical Consent Form KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care • A patient who has recently arrived on the surgical unit after being transferred from the post- anesthesia care unit asks for a drink. The nurse should first check the: • status of the IV fluids. ability to swallow. • nursing progress notes. yn ur si • w w w .m • a n e s t h e s i a r e c o r d ng te st pr ep .c • ep .c om . A N S : B Before a post-surgical patient is offered anything to eat or drink, the ability of the patient to swallow should be assessed. DIF: Cognitive Level: Application REF: m 749 OBJ: Clinical Practice #3 TOP: NPO Status KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient scheduled for surgery has an order for a preoperative surgical skin prep. The nurse may be required to: • shave the entire surgical site. spray the surgical area with an antimicrobial solution. • scrub the surgical area for 1 minute with antibacterial solution. pr • instruct the patient in the use of an antimicrobial soap in the shower. ANS: D The nurse may be required to instruct in the use of an antimicrobial soap in the shower. Although hair may be clipped away from the incision line, this is usually not done by the floor nurse but accomplished in the surgery suite. DIF: Cognitive Level: Application REF: m 741 OBJ: Clinical Practice #2 TOP: Preoperative Surgical Skin Preparation KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • To help prevent errors in the surgical procedure, the National Patient Safety Goal instituted a directive that prior to presurgical medication, each patient must: • verbally state the location of the surgical site and the expected procedure. w when still conscious participate in marking the surgical site. w • .m yn ur si ng te st • w • • have the unit nurse confirm their identity. have a photograph of the surgical site on the chart. ANS: B Prior to presurgical medication, the conscious patient participates in a marking of the body part and site of the expected surgical procedure. DIF: Cognitive Level: Comprehension REF: m 737 OBJ: Theory #6 TOP: Immediate Preoperative Care KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: coordinated care • While completing the preoperative checklist, a patient who is almost ready for transport to the operating room states that he does not want to remove his wedding band. The nurse should: • tape it in place on his finger. • remind him it must be removed, and lock it in the narcotic cabinet. • ask a family member to take care of it. inform him that the hospital cannot be responsible for its loss. ANS: A A wedding band may be worn to surgery, but it must be taped to the finger in a manner that does not restrict circulation. DIF: Cognitive Level: Application REF: m 747 OBJ: Clinical Practice #2 TOP: Immediate Preoperative Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse is aware that in both the very young and the elderly surgical patient, the risk is much higher for: • nausea and vomiting. delayed healing. • anorexia. st • te hydration issues. ng • pr ep .c om • w w .m yn ur si ANS: B Both the very young and the elderly are at greater risk for dehydration or overhydration and alterations in body temperature control. DIF: Cognitive Level: Comprehension REF: m 734 OBJ: Theory #2 TOP: Surgical Risks in Young and Elderly KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: reduction of risk • A patient undergoing preadmission testing before same-day surgery asks how long he will remain in the recovery area before being allowed to go home. The nurses most informative response would be: • 30 to 60 minutes. 1 to 3 hours. • 5 to 6 hours. w • • 6 t o 8 h o u r s . .c pr ep DIF: Cognitive Level: Knowledge REF: m 748 OBJ: Theory #7 TOP: Postanesthesia Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: psychosocial adaptation • The circulating nurse is responsible for: • preparing the sterile field. om A N S: B The usual recovery time in a same-day surgery recovery area is 1 to 3 hours. assisting with sterile draping of the patient. • maintaining an accurate count of sponges. st • pointing out the observation of contamination immediately to the personnel involved. ANS: D Any break in sterile technique in the operating room should be immediately pointed out and remedied. DIF: Cognitive Level: Comprehension REF: m 748 OBJ: Theory #9 TOP: Circulating Nurse KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: safety and infection control • When the patient is ready to return from the post-anesthesia _ is an care unit (PACU), a minimal Aldrette score of indicator that the patient is ready to return to the floor. • 2 to 4 4 to 8 w • w .m yn ur si ng te • w • 9 to 10 • 11 to 12 ANS: C Using an Aldrette scoring system of activity, respiration, circulation, consciousness, and skin color being scored from 1 to 3, a score of 9 to 10 is the minimal indicator that the patient is ready to return to the floor. DIF: Cognitive Level: Comprehension REF: m 747 OBJ: Theory #10 TOP: Postanesthesia Care KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • A patient who has returned to the surgical nursing unit from the post-anesthesia care unit (PACU) is drowsy and requires verbal stimulation to remain aroused. The best position to maintain an airway for this patient is: • supine. • side-lying. • head of bed at 30 degrees with head and neck midline. head of bed at 45 degrees with head and neck midline. ANS: B The patient should be positioned on the side or with the head turned to the side to prevent aspiration. Maintaining an open airway is a priority measure. DIF: Cognitive Level: Application REF: m 749 OBJ: Theory #10 TOP: Safety: Airway KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • The nurse is assessing the surgical dressing of a patient who arrived on the unit an hour ago. The surgical dressing has serosanguineous drainage on the dressing. The nurse should: st pr ep .c om • make a note of the drainage on the worksheet to report it at the end of shift. • change the surgical dressing immediately to prevent infection. • outline the area of drainage with a pen and mark it with the date and time. ng te • reinforce the dressing with clean gauze sponges and tape. ANS: C The area should be outlined, dated, and timed for future reference and comparisons. DIF: Cognitive Level: Application REF: m 750 OBJ: Theory #2 TOP: Safety: Bleeding KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk potential • A nurse is instructing a patient who had surgical removal of a brain tumor on how to prevent respiratory complications from surgery. The nurse would teach the patient to: • turn, cough, and deep breathe. w w w .m yn ur si • • use humidified oxygen. • turn gently from side to side. • use deep breathing and an incentive spirometer. ANS: D Coughing may be contraindicated for patients who have had hernia repair, eye, ear, or brain surgery. This is because the act of coughing could create increased pressure in the surgical area, which is contraindicated. Huffing or the use of an incentive spirometer is effective for post- surgical respiratory health. DIF: Cognitive Level: Application REF: m 750 OBJ: Clinical Practice #4 TOP: Promoting Respiratory Function KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity • A post-operative surgical patient asks how the sequential pneumatic compression boots applied in the operating room will help lower the risk of blood clots forming in the legs. The nurses most appropriate response would be that the boots: • measure pressure in the leg blood vessels and sound an alarm if pressure rises. alternately compress and release to help blood flow through vessels. • provide gentle continuous compression at low pressure. provide firm continuous compression at high pressure. ANS: B Pneumatic boots alternately compress and release to squeeze the blood vessels and thus propel blood through the vessels back to the heart. DIF: Cognitive Level: Comprehension REF: m 751 OBJ: Theory #10 TOP: Promoting Circulation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk potential • A nurse is monitoring the urinary drainage from a patient who returned to the unit a few hours ago from the post-anesthesia care unit (PACU) following a surgical procedure. The urine total is 54 mL for the last 2 hours. The most appropriate nursing action is to: • increase the flow rate of the IV for 10 to 15 minutes. yn ur si ng te st pr ep .c • om • irrigate the indwelling urinary catheter. • apply manual pressure to the patients bladder. w notify the surgeon of the findings. ANS: D If the urinary flow rate is lower than 60 mL for a 2-hour period, the surgeon is notified. DIF: Cognitive Level: Analysis REF: m 751 OBJ: Theory #10 TOP: Inadequate urine output KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • A patient who had surgery earlier in the day using general anesthesia asks whether he can have something to eat. The diet order indicates clear liquids can be taken. Before giving a Jell-O to the patient, the nurse should check for the presence of: w w • .m • • clear lung sounds. • adequate urinary drainage. • bowel sounds in all quadrants. • w w w .m yn ur si ng te st pr ep .c om p al p a bl e p er ip h er al p ul se s. A N S: C Before allowing a patient to eat or drink after surgery, the nurse must ensure that bowel sounds are present in all four quadrants. This is because of the risk of paralytic ileus (lack of return of peristalsis) after surgery. DIF: Cognitive Level: Analysis REF: m 753 OBJ: Theory #10 TOP: Maintaining Fluid Balance KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk potential • A patient who had abdominal surgery is complaining of gas pains and has distention of the abdomen and flatus. To promote patient comfort, the nurse should advise: • early ambulation. • turning to the left side. • drinking fluids that are very hot. • lying supine with knees flexed . ANS: A Ambulation is helpful in expelling gas. Taking large amounts of food or liquid at a time, and drinking fluids that are either very hot or cold, can aggravate the symptoms. DIF: Cognitive Level: Application REF: m 754 OBJ: Clinical Practice #5 TOP: Promoting Comfort KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse preparing to get a patient out of bed for the first time since surgery will initially: • assist the patient to sit and dangle his or her legs on the side of the bed. allow the patient to sit with the head of bed raised to the high-Fowlers position. • assist the patient from a supine position to a standing position. • place a walker at the side of the bed. ANS: B st pr ep .c om • not driving or making important decisions for 24 hours. w • reporting temperatures greater than 99 F. w • .m yn ur si ng te The first step is to raise the head of the bed and let the body adjust to the position change. After a few minutes, the patient can be assisted to sit on the side of the bed with his or her legs dangling (with feet on floor). Finally, the patient is assisted to a standing position. DIF: Cognitive Level: Application REF: m 754 OBJ: Clinical Practice #6 TOP: Rest and Activity KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk potential • A patient is ready for discharge following same-day surgery. The teaching plan for this patient includes: • limiting wine intake for 12 hours. that vomiting might be an expected symptom. ANS: C Patients should not drive or make important decisions for at least 24 hours after surgery, until all residual effects of anesthesia have worn off. DIF: Cognitive Level: Application REF: m 735, Home Care OBJ: Clinical Practice #7 TOP: Same-Day Surgery Discharge KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: physiological adaptation MULTIPLE RESPONSE • The nurse explains that the informed surgical consent form w • should include information relative to: (Select all that apply.) • the procedure to be performed. • the related risks of the procedure. • consent to blood transfusion. • time and date signed. • ng te st pr ep .c om m a r i t a l s t a t u s . w w w .m yn ur si AN S: A, B, D The consent must include the procedure to be performed and the related risks of the procedure; it must also be timed, dated, and witnessed. Consent for transfusion is another permit entirely. DIF: Cognitive Level: Comprehension REF: m 754 OBJ: Theory #38 TOP: Surgical Consent KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk potential • The nurse preparing the surgical patients room for the patients return from the post- anesthesia unit should: (Select all that apply.) • fan fold the sheets on the near side of the bed. • lower the bed for easy transfer of the patient. • place an IV pole at the head of the bed. • gather an emesis basin, tissues, and a small towel. • collect extra dressing supplies and place them on the bedside table. ANS: C, D w w w .m yn ur si ng te st pr ep .c om The post-surgical room should be prepared with the sheets fan folded on the far side of the heightened bed. IV poles, emesis basins, oxygen, and suction equipment should be ready to use; a thermometer, sphygmomanometer, and stethoscope should be available. DIF: Cognitive Level: Application REF: m 738, Table 37-2 OBJ: Theory #3 TOP: Room Preparation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort COMPLETION • A post-operative patient experiences separation of the layers of his abdominal surgical wound during coughing. Separation of the . ANS: layers of a surgical wound is known as dehiscence Dehiscence is separation of the layers of the surgical wound that may occur when the patient is coughing, particularly if the abdominal incision is not properly splinted. DIF: Cognitive Level: Knowledge REF: m 735, Box 37-1 OBJ: Theory #2 TOP: Postoperative Care KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The patient informs the admitting nurse that she has been drinking feverfew tea for the herbal treatment of migraine headaches. The nurse reports this to the surgeon because this herb can cause . ANS: bleeding The herb feverfew can inhibit platelet aggregation and increase the possibility of bleeding. DIF: Cognitive Level: Comprehension REF: m 737 OBJ: Theory #2 TOP: Herbal Substances KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: reduction of risk potential • To help prevent surgical site infections in the diabetic patient, the glycemic should be maintained with a blood glucose of less than mg/dL. ANS: 200 A diabetic patient can be better protected from surgical site infection by maintaining blood glucose below 200 mg/dL. DIF: Cognitive Level: Comprehension REF: m 737 OBJ: Theory #3 TOP: Glucose Control KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 28. The nurse reminds the patient that the member of the surgical team who is responsible for obtaining the surgical consent is the . ANS: surgeon The surgeon is the person responsible for obtaining an informed surgical consent. proliferation. • maturation. • reconstruction. ep • .c om Chapter 28 Wound Care The nurse clarifies that the first stage of wound healing is: pr • .m yn ur si ng te st i n f l a m m a t i o n . w w w AN S: D Inflammation is the first stage of wound healing, followed by the proliferation, maturation, and reconstruction stages. DIF: Cognitive Level: Knowledge REF: m 760 OBJ: Theory #1 TOP: Inflammatory Process KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse is taking care of a post-surgical patient and notes the incision is clean and dry, with sutures intact. The nurse further intention. assesses that the wound is healing by • fourth • third • second • first surgical incision closed with staples. • chest wound left open for a closed system. puncture wound sutured with silk suture. ANS: A A secondary intention healing occurs when there is a jagged wound whose edges do not approximate. DIF: Cognitive Level: Comprehension REF: m 763, Figure 38-3 OBJ: Theory #1 TOP: Wound Types KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • When the patient complains that he feels he is getting worse because of the increased swelling at his wound site on his leg, the nurses most helpful response would be that swelling indicates that: • an infection is in progress at the wound site. w vessels have dilated and allowed plasma to leak into the wound site. w • .m yn ur si ng te st pr • ep • .c om ANS: D A wound with minimal tissue loss, such as a surgical incision, heals by closure, which is first, or primary, intention. Wounds that are not closed heal by either second (secondary) or third (tertiary) intention. DIF: Cognitive Level: Comprehension REF: m 763 OBJ: Theory #1 TOP: Wound Healing Stages KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse gives an example of a wound that heals by second (secondary) intention as a: • laceration with edges that do not approximate. w • • he has lain in one position for such a long time that swelling has occurred. there is probably a deeper injury than what appears on the surface. ANS: B As part of the healing process, histamines and prostaglandins have caused small vessels to dilate and leak plasma and electrolytes into the wound site causing swelling, which causes the wound to become reddened and swollen as the phagocytosis cleans up the microorganisms. DIF: Cognitive Level: Application REF: m 761 OBJ: Theory #3 TOP: Swelling and Inflammation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse warns the patient that one of the patients habits has caused the reduction of functional hemoglobin, which limits the hemoglobins oxygen-carrying ability. To improve this situation, the nurse suggests that the patient quit: • drinking. • using marijuana. • smoking cigarettes. • w w w .m yn ur si ng te st pr ep .c om e a t i n g e x c e s s i v e f a t s . A N S : C Smoking reduces the functional hemoglobin which, in turn, reduces the amount of oxygen carried to the cells of the body. DIF: Cognitive Level: Analysis REF: m 762 OBJ: Theory #2 TOP: Smoking KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • A nurse is assessing a surgical patient for internal hemorrhage, which would be indicated by blood pressure. • restlessness, rising pulse, and falling • restlessness, falling pulse, and rising • headache, rising pulse, and falling blood pressure. • excessive gas. • increased serosanguineous drainage from the wound. ANS: D st • te complaint of constipation. si ng • pr ep .c om lethargy , falling pulse, and rising ANS: A If hemorrhage occurs, it can lead to hypovolemic shock. Indicators of hemorrhage include restlessness, rising pulse, and falling blood pressure. DIF: Cognitive Level: Application REF: m 764 OBJ: Theory #2 TOP: Hemorrhage KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse is alert to the indication of possible dehiscence of an abdominal surgical wound, which would be evidenced by: • increased pallor of the surgical site. w w w .m yn ur Increase in the serosanguineous drainage from the surgical wound is a common sign of impending dehiscence. DIF: Cognitive Level: Application REF: m 765 OBJ: Theory #4 TOP: Dehiscence KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • A nurse is ambulating a patient in the hall a few days after abdominal surgery and the patient says, I think something just let go. The initial intervention by the nurse should be to: • seat the patient in a nearby chair. • assist the patient in a supine position. • ask someone to quickly get an abdominal binder. • instruct the patient to pant to reduce abdominal tension. ANS: B The patient is likely experiencing wound dehiscence and should immediately be assisted into a supine position. This eliminates the force of gravity from putting additional stress on the suture line and possibly causing evisceration. DIF: Cognitive Level: Application REF: m 765 OBJ: Theory #4 • compresses the device in the hand before closing. • refrains from touching the drainage spout with the hand. points the device away from herself while opening it. ANS: A Separate alcohol swabs should be used to clean the spout and the plug. DIF: Cognitive Level: Application REF: m 767, Steps 38-1 OBJ: Clinical Practice #1 TOP: Drainage Devices KEY: Nursing Process Step: Evaluation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse chooses a nonadherent dressing to apply to a wound because the nonadherent dressing: • is smaller and less bulky and will absorb more drainage. ng te st pr ep .c • om TOP: Dehiscence and Evisceration KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk potential • A patient who underwent removal of a breast must be discharged home with a Jackson-Pratt wound drain in place. As the patient demonstrates the procedure for emptying it, the nurse should correct her if she: • uses one alcohol wipe to clean both the spout and the plug. retains sterility longer than plain gauze. • allows drainage to seep through the barrier and be absorbed on the other side. ur si • does not require the use of tape to make it adhere to the skin. ANS: C Telfa dressings have a shiny, nonadherent surface; the shiny side is applied to the wound to prevent the dressing from sticking to the skin. The drainage seeps through the barrier and is absorbed on the other side. It does require some sort of adhesive or binder to keep the pad in place. w w .m yn • w DIF: Cognitive Level: Comprehension REF: m 767, Steps 38-1 OBJ: Clinical Practice #1 TOP: Dressings KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • Because the patient with an abdominal dressing requires frequent dressing changes, the abdomen is beginning to show skin irritation from repeated tape removal. The nurse would change the dressing procedure in order to use: • paper tape. • Montgomery straps. • Karaya paste. • w w w .m yn ur si ng te st pr ep .c om e l a s t i c a d h e s i v e t a p e . A N S : B Montgomery straps allow the dressing to be changed without constantly applying and removing tape. DIF: Cognitive Level: Analysis REF: m 768 OBJ: Clinical Practice #1 TOP: Securing Dressings KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse caring for a patient with a stage I pressure ulcer would most appropriately select a(n) dressing. • nonocclusive • exudate-absorbing • hydrocolloid • thin film ANS: D Thin film dressings are used on stage I ulcers to protect them from shearing forces and to keep them moist. DIF: Cognitive Level: Application REF: m 768 OBJ: Clinical Practice #2 TOP: Treatment of Ulcers KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk potential • A patient has a pooling of blood under unbroken skin of the hip after a fall. The nurse should document that this patient has a(n): • abrasion. • laceration. • hematoma. • avulsion. st pr ep .c om ANS: C A hematoma is a pooling of blood under unbroken skin. An abrasion is a scraping away of skin tissue. A laceration is a torn, ragged, or mangled wound, and a an avulsion refers to something being torn away. DIF: Cognitive Level: Comprehension REF: m 759, Table 38-1 OBJ: Theory #1 TOP: Documentation KEY: Nursing Process Step: Assessment ng te MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse is performing a dry sterile dressing change for an abdominal wound. The nurse should use a swab to clean: • from the outer abdomen toward the wound. in a circular motion around the wound circling to the outside. • from the left to the right across the wound. ur si • w w w .m d i r e c t l y o v e r t h e w o yn • st pr ep .c om u n d . A N S : B A circular motion around the wound toward the outside keeps the wound area cleanest. DIF: Cognitive Level: Application REF: m 774, Skill 38-1 OBJ: Clinical Practice #1 TOP: Wound Cleaning KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A patient is due for a wound dressing change for a horizontal lower abdominal incision. In which direction should the nurse pull to remove the tape from the old dressing? • From left to right across the abdomen From right to left across the abdomen • From the top of the wound to the bottom ng te • From each of the four sides toward the wound ANS: D The tape should be removed by pulling it off toward the wound. This helps prevent disruption of the wound. DIF: Cognitive Level: Application REF: m 774, Skill 38-1 OBJ: Clinical Practice #1 TOP: Wound Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk potential • A nurse explains that the major purpose of the use of a hydrocolloid dressing is to: • keep the wound dry. w w .m yn ur si • help destroy microorganisms in an infected wound. • occlude air and promote breakdown of necrotic tissue. w • • leave the dressing in place for 10 days. ANS: C Hydrocolloid dressings are air-occlusive dressings used on noninfected wounds that provide a moist environment for wound healing. They can be left in place for up to 7 days. DIF: Cognitive Level: Comprehension REF: m 774 OBJ: Clinical Practice #1 • pull it off using slow, steady pressure. • leave it in place and cover it with new, wet dressings. moisten it with povido neiodine. ANS: A If the dressing sticks to the wound, normal saline should be added to loosen it. Pulling loose a stuck dressing damages new tissue. Leaving it in place does not promote a clean wound. Povidone-iodine must be ordered. DIF: Cognitive Level: Analysis REF: m 779, Skill 38-3 OBJ: Clinical Practice #3 TOP: Wetto-Dry Dressings KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk potential • A nurse performing a right eye irrigation will position the patient: • upright with the head hyperextended. yn ur si ng te st pr ep .c • om TOP: Hydrocolloid Dressing KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse changing a wet-to-damp normal saline dressing for a patient with an ulcer on the heel finds that the old dressing is stuck to the wound bed. The nurses most beneficial intervention would be to: • add normal saline to loosen it. upright with the head tilted toward the left eye. • supine with the head hyperextended. w supine with the head tilted toward the right eye. ANS: D The patient should be positioned supine with the head tilted toward the affected eye. This position allows the irrigation solution to drain away from the eye and not contaminate the other eye. DIF: Cognitive Level: Application REF: m 782, Steps 38-4 OBJ: Clinical Practice #3 TOP: Eye Irrigations KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A nurse removing wound staples would engage the staple puller and squeeze the handles completely and: w w • .m • • pull to the right. • pull outward. • pull to the left. • rotate. ep .c om ANS: B The handles should be squeezed together all the way. This depresses the center of the staple and allows it to be lifted outward from the skin. DIF: Cognitive Level: Application REF: m 781, Steps 38-3 OBJ: Clinical Practice #4 TOP: Staple Removal KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse clarifies that a vacuum-assisted closure supports healing of a wound by: • drawing the wound edges together by negative pressure. interrupting the proliferation of bacteria in the wound. • strengthening the wall of the wound. st pr • making an airocclusive cover for the wound. ANS: A A vacuum-assisted dressing that is accomplished by a special dressing and vacuum device applies negative pressure to the wound, which increases blood flow, increases oxygenation, and improves the delivery of nutrients to the wound. DIF: Cognitive Level: Knowledge REF: m 769 OBJ: Theory #6 TOP: Vacuum-Assisted Dressing KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse is aware that the only necrotic wound for which debridement is not recommended is a pressure ulcer located on the: • scapula. w w w .m yn ur si ng te • • f e m o r • sacrum. • heel. a l h e a d . w w w .m yn ur si ng te st pr ep .c om AN S: C Debridement is not recommended for treatment of a pressure ulcer on the heel because of the small amount of tissue available at that site. DIF: Cognitive Level: Knowledge REF: m 767, Clinical Cues OBJ: Clinical Practice #2 TOP: Debridement KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: reduction of risk potential COMPLETION • The nurse places Dakins solution in a wound to accomplish chemical . ANS: debridement Dakins solution is placed in a wound to destroy the necrotic tissue so that granulation tissue can form to heal the wound (debridement). DIF: Cognitive Level: Knowledge REF: m 766 OBJ: Clinical Practice #2 TOP: Chemical Debridement KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies • The nurse assesses the large raised scar on the AfricanAmerican patient. The nurse documents the lesion as a . ANS: keloid Keloids are large raised permanent scars resulting from colloid overgrowth that are seen most frequently on darkly pigmented skin. DIF: Cognitive Level: Comprehension REF: m 762 OBJ: Theory #1 TOP: Keloid KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse explains to the patient that the foot will be submerged in warm water for a maximum of minutes. ANS: 20 twenty adequate fibroblast function. • synthesis of collagen. • intrinsic factor. ep .c • w w w .m yn ur si ng te st pr • a d e q u a t e p h a g o c y t o s i s . A N S : B , C , om Warm soaks that involve submerging the limb should only last for 15 to 20 minutes. DIF: Cognitive Level: Knowledge REF: m 785 OBJ: Clinical Practice #5 TOP: Foot Soak KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk potential MULTIPLE RESPONSE • The nurse is concerned about an HIV immunocompromised patients ability to heal because of the lack of: (Select all that apply.) • hemoglobin. antineoplastic drugs. • pyroxidine. • heparin. ep .c • om E Persons who are immunosuppressed have inadequate fibroblast function, phagocytosis, and synthesis of collagen. DIF: Cognitive Level: Comprehension REF: m 764 OBJ: Theory #2 TOP: Immunocompromise KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse recognizes that of the drugs a patient is currently taking, several contribute to delayed healing, such as: (Select all that apply.) • vitamin C. .m yn ur si ng te st pr • steroids. ANS: B, D, E Drugs such as antineoplastic agents, anticoagulants, steroids, and immunosuppressants all delay healing. DIF: Cognitive Level: Comprehension REF: m 762 OBJ: Theory #2 TOP: Delayed Healing KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: pharmacological therapies • The nurse reminds the 85-year-old patient that his healing will be slower because of age- related changes such as: (Select all that apply.) • excessive production of blood factors. atherosclerosis. • diminished lung function. slow metabolism. w • w • w • i n c r e a s e d i pr ep .c om m m u n i t y . A N S : B , C , D w w w .m yn ur si ng te st Age slows metabolism and production of blood factors. Decreased lung function reduces the bodys supply of oxygen and slows healing, Atherosclerosis impairs blood flow. DIF: Cognitive Level: Comprehension REF: m 762 OBJ: Theory #2 TOP: Factor That Affect Wound Health KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation OTHER • The nurse irrigating an infected wound of the hand would: (Prioritize the steps. Separate the letters by a comma and a space as follows: A, B, C, D, E, F, G.) • Open sterile irrigation basin and solution. • Don sterile gloves to apply dressing. • Pour irrigating solution in basin. • Irrigate keeping the syringe tip 1 inch from the wound surface. • Document procedure. • Pat wound dry and redress. • Place pad under the infecte d hand. ANS: A, C, G, B, D, F, E Prior to donning gloves the basin and solution should be opened, the basin filled with the solution, and the pad placed under the wound. The gloves are donned, the irrigation completed, the wound dried and redressed, and the intervention documented. Chapter 29 Gastrointestinal Intubation MULTIPLE CHOICE • Before any diet tray is delivered to a patient, the nurse has the responsibility of: • determining if the patient needs assistance to eat. • confirming the diet on the tray with the diet sheet. • assessing if the food is of the appropriate temperature. adding extra salt and sugar packets. ANS: B The diet tray should be checked against the diet order to be sure that the patient receives the proper diet. No matter who actually delivers the tray, it is the nurse who confirms the accuracy of the diet. DIF: Cognitive Level: Comprehension REF: m 478, Skill 27-1 OBJ: Theory #1 TOP: Nurse Role KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nutritional documentation that is most informative is: • ate all of lunch. ng te st pr ep .c om • ate 50% of lunch without difficulty. Refused all solid food. • drank most of liquids without difficulty. ur si • assisted feeding liquid diet, choked frequently. ANS: B Nutritional documentation should include percentage of intake and how it is tolerated. .m yn • w w w DIF: Cognitive Level: Application REF: m 478 OBJ: Theory #1 TOP: Nutrition Documentation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • When assisting a patient with a severe visual impairment who wishes to feed himself, the nurse could best facilitate the patients eating by: • placing the plate on his lap. • seating the patient in a chair and placing the over-the-bed table appropriately. • orienting the patient to the position of foods on the plate using a clock-face description. • placing each food in a separate container or Jell-O. • cream soup. ep • .c om bowl. ANS: C It is best to orient a visually impaired patient to the position of the foods on the plate by describing the plate as if it is a clock face (3 oclock, 6 oclock, and so on). DIF: Cognitive Level: Application REF: m 479, Skill 27-1 OBJ: Theory #1 TOP: Assisting Patient with Eating KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: basic care and comfort • A patient who underwent surgery has an order to begin a clear-liquid diet and can be offered: • tea with milk. pr • .m yn ur si ng te st f r u i t s h e r b e t . w w w A NS :B A clear-liquid diet consists of foods that are liquid at room temperature and are clear, have a low residue, and are easily digested. Gelatins are part of a clear liquid diet. DIF: Cognitive Level: Comprehension REF: m 480 OBJ: Theory #2 TOP: Diet for Postoperative Patient KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse caring for a patient with bulimia should add to the care plan to assess for: • hiding food in napkins or under plate. • inducing self to vomit. • refusal to eat. • ng te st pr ep .c om flushi ng food down com mode. ANS: B With bulimia, along with binge eating, there is purging, fasting, and the use of laxatives. These patients may eat everything on their tray then purge by inducing themselves to vomit. DIF: Cognitive Level: Comprehension REF: m 481 OBJ: Theory #3 TOP: Bulimia KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • An obese clinic patient who is in the latter part of the first trimester of a pregnancy asks how much weight she should gain. The nurses best response is to say that the total weight gain should pounds. be no more than w w w .m yn ur si a. 35 b. 30 c. 20 d. 10 ANS: C Total weight gain for an obese patient should be no more than 20 pounds. DIF: Cognitive Level: Comprehension REF: m 482, Table 27-1 OBJ: Theory #4 TOP: Pregnancy KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • The nurse takes into consideration that a patient who abuses alcohol is at risk for a vitamin deficiency in: • thiamine. • cyanocobalamin. • ascorbic acid. • iron. ANS: A Thiamine deficiency is often present in patients who abuse alcohol. DIF: Cognitive Level: Knowledge REF: m 481 OBJ: Theory #4 TOP: Substance Abuse KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • A patient who is on a low-cholesterol diet verbalizes that he enjoys eating meats and doesnt intend to stop. The nurses most helpful response would be, You can enjoy your meat if you will concentrate on such meats as: • broiled sirloin steak. fried catfish. • baked turkey breast. om • • w w w .m yn ur si ng te st pr ep .c s a u s a g e p a t t i e s . A N S : C Red meat, eggs, and high-fat dairy products contain large amounts of saturated fat; poultry (such as turkey breast) and fish are low-fat items and therefore are desirable when trying to reduce serum cholesterol. Fried foods also contain extra cholesterol. DIF: Cognitive Level: Comprehension REF: m 483 OBJ: Theory #4 TOP: Patient Education KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • An older male patient is concerned about his cholesterol lab report that shows an elevated high-density lipoprotein (HDL) level. The nurse explains that such a report indicates that: • he should go on a strenuous low-cholesterol diet. • he is at risk for hypertension. • is developing atherosclerosis. • his vessels are being cleansed of fatty deposits. ep .c om ANS: D High-density lipoprotein (HDL) is the good cholesterol that tends to cleanse the vessels of fatty deposits. DIF: Cognitive Level: Comprehension REF: m 483 OBJ: Theory #4 TOP: HDL KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • An outpatient clinic nurse assesses a blood glucose level of 75 mg/dL in a patient who has been on a low-carbohydrate diet for the last 10 days. The nurse should: • notify the physician about the ineffectiveness of the diet. document the finding. • suggest a moderate increase carbohydrate intake. st pr • arrange a dietician consultation to discuss a more effective diet. ANS: B Document the finding. Normal blood sugar is between 70 and 120 mg/dL. DIF: Cognitive Level: Application REF: m 484 OBJ: Theory #5 TOP: Disease Process Benefiting from Diet Therapy KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • Because of the patients dysphagia, the nurse recommends to the physician that the patient be placed on a Level II texture level diet, which means that the food is: • thickened to prevent aspiration. mechanically altered, moist, minced helpings. w • pureed to a pudding consistency. w • .m yn ur si ng te • w • min ced into bite -siz e pie ces. AN S: C Level II texture is a diet in which the food has been mechanically altered to moist, -inch pieces. DIF: Cognitive Level: Comprehension REF: m 486 OBJ: Theory #3 TOP: Dietary Modifications KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk • A nurse positions a patient for the insertion of a nasogastric (NG) tube by: • turning the patient to a right side-lying position. sitting the patient upright and hyperextending the patients head. • lowering the head of the bed to a flat position. om • raising the head of the bed to 30 degrees. ANS: B The head of the bed should be raised and the patient asked to hyperextend his head to facilitate the passage of the NG tube. DIF: Cognitive Level: Application REF: m 489, Skill 27-2 OBJ: Theory #6 TOP: NG Tube Insertion KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk The nurse who is preparing to give a feeding per a nasogastric (NG) tube tests the placement of the tube most safely by: • checking the lungs for rhonchi. ur si • ng te st pr ep .c • instilling 10 mL of normal saline and checking for cough. • aspirating stomach contents. yn • injecting 20 mL of air and listen at the tip of the xiphoid. ANS: C The safest and most assured method to test for NG tube placement is to aspirate stomach contents and check fluid for pH. Using the air method is not as accurate as the stomach aspiration. DIF: Cognitive Level: Application REF: m 495, Skill 27-4 OBJ: Clinical Practice #3 TOP: NG Tube Insertion KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk • Stopping the infusion and checking for residual, the nurse aspirates 155 mL of gastric contents. The nurse should next: • replace the aspirate and continue with the feeding. w w w .m • • throw the aspirate away and flush the tubing. • replace the aspirate and stop feeding for 1 to 2 hours. throw the aspirate away and stop feeding for 2 hours. ANS: C If the residual volume is greater than 150 mL, the fluid should be replaced, and further feeding should be delayed by 1 to 2 hours, or agency policy should be followed. DIF: Cognitive Level: Application REF: m 493 OBJ: Clinical Practice #4 TOP: Residual KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient is scheduled to receive an intermittent tube feeding. This feeding should be allowed to flow in over how many minutes? a. 1 b. 2 c. 5 d. 10 ANS: D An intermittent feeding should take approximately 10 minutes to flow into the tube. DIF: Cognitive Level: Comprehension REF: m 493 OBJ: Theory #7 TOP: Tube Feeding KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk • When the patient has just finished receiving a tube feeding, the nurse leaves the head of the patients bed elevated for 30 to 60 minutes after feeding in order to: • facilitate stomach emptying and prevent aspiration. .m yn ur si ng te st pr ep .c om • facilitate lung drainage and promote ventilation. w • maintain skin integrity to the buttocks. w • prevent feeding tube from clogging. ANS: A The head of the bed should be left elevated at a 30- to 90- degree angle for 30 to 60 minutes after the feeding to help reduce the risk of aspiration. DIF: Cognitive Level: Comprehension REF: m 49, Box 27-3 OBJ: Clinical Practice #4 TOP: Tube Feeding KEY: Nursing Process Step: Implementation w • • 3 • 4 • 6 pr ep .c ANS: C Both the IV site and the flow rate should be monitored every 4 hours and the site assessed for infection. DIF: Cognitive Level: Knowledge REF: m 497, Table 27-4 OBJ: Theory #8 TOP: TPN KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse explains that adequate vitamin D can be acquired by: • eating 2 oranges a day every week. om MSC: NCLEX: Physiological Integrity: reduction of risk • The nurse caring for the patient receiving total parenteral nutrition (TPN) should monitor the flow rate every hours. • 2 eating fish 3 times a week. • having 10 minutes of sunshine on the limbs. st • te • w w w .m yn ur si ng eatin g gree n leafy vege table s. ANS :C Exposing the limbs to 10 minutes of sunshine daily can provide adequate vitamin D. DIF: Cognitive Level: Comprehension REF: m 483 OBJ: Theory #5 TOP: Vitamin D KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse is caring for a patient who has total parenteral nutrition (TPN) running finds that the infusion is behind by 200 mL. The nurse should: • increase the flow rate 5% until the infusion has caught up. • check the patients stomach residual. • elevate the head of the bed 30 degrees. • document the discrepancy and report to the charge nurse. ANS: • perform a fingerstick blood glucose test. ep slow down the feedings and monitor. pr • .c DIF: Cognitive Level: Application REF: m 497 OBJ: Theory #1 TOP: Monitoring TPN KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient recently started on enteral tube feedings starts complaining of nausea and having diarrhea. The best nursing action is to: • check the enteral tube for placement. om D The rate of a TPN is never increased because of the danger of causing hyperglycemia or circulatory overload. The discrepancy is to be documented and reported to the charge nurse or physician. stop the feedings and inform the physician. ANS: D Nausea, constipation, and diarrhea are concerns following institution of tube feedings. DIF: Cognitive Level: Application REF: m 497, Box 27-3 OBJ: Clinical Practice #4 TOP: Enteral Nutrition KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient has a new order to have an NG tube removed. The nurse should initially: • wash her hands and apply clean gloves. yn ur si ng te st • encourage mouth care as needed. • explain the procedure to the patient. w pinch the tube while removin g it. ANS: C Explaining the procedure to the patient before starting helps in gaining the patients confidence. DIF: Cognitive Level: Application REF: m 492, Steps 27-2 OBJ: Clinical Practice #3 TOP: NG Tube Removal KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe w w • .m • Effective Care Environment • A nurse is instructing a family member who will be caring for a patient receiving enteral feedings after discharge to home. The nurse would emphasize: • taping the gastrostomy tube so that it does not hang lower than the stomach. • discarding unused opened refrigerated formula after 3 to 4 days. • administering tube feedings while they are still cold from the refrigerator. mixing all medications together for administration at the same time. ANS: A The tube should be taped so that it is higher than the entry point into the body. DIF: Cognitive Level: Application REF: m 498, Patient Teaching OBJ: Clinical Practice #2 TOP: Health Teaching KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse inserting an NG tube through the nostril into the back of the throat of a patient would instruct the patient to: • hyperextend the head. te st pr ep .c om • cough forcefully. • drop head forward and begin to swallow. ng • open mouth and extend tongue . ANS: C The patient should be instructed to tip the head forward and begin to swallow to help advance the tube through the esophagus. DIF: Cognitive Level: Application REF: m 490, Skill 27-2 OBJ: Clinical Practice #3 TOP: NG Tube Insertion KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment • The nurse caring for a patient receiving enteral feedings would assess for tolerance of the feeding by monitoring: • for gastric tube patency. w w w .m yn ur si • • for duodenal tube patency. • for abdominal distention. • w w w .m yn ur si ng te st pr ep .c om t h e r a t e o f t h e f e e d i n g . A N S : C Assessing the abdomen for distention helps the nurse identify intolerance of tube feedings. DIF: Cognitive Level: Application REF: m 494, Skill 27-3 OBJ: Clinical Practice #4 TOP: Enteral Nutrition KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • While the nurse is explaining the procedure for inserting a tube for enteral feedings, the patient interrupts and asks why there is a need for this tube. The nurses best response is: • Your physician has ordered this to help your condition. • Tell me what your doctor told you about this procedure. • Are you telling me you dont want this tube inserted? • This tube placement will only be temporary. ANS: B order electrolytes daily. • monitor IV site every shift. • monitor for blood glucose. .c • om In assessing the patients understanding, the nurse should assess the level of the patients understanding and knowledge about the procedure. DIF: Cognitive Level: Application REF: m 497 OBJ: Clinical Practice #3 TOP: NG Tube Insertion KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity: basic care and comfort • When caring for a patient receiving total parenteral nutrition, the nurse knows that it is essential to: • check for flow rate every shift. w w w .m yn ur si ng te st pr ep ANS: D Total parenteral nutrition contains a high concentration of glucose, and monitoring blood glucose every 6 to 8 hours will determine patient tolerance. DIF: Cognitive Level: Comprehension REF: m 497, Box 27-3 OBJ: Theory #10 TOP: TPN KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: reduction of risk COMPLETION • The correct anatomic landmarks to follow when inserting a to the and then nasogastric tube is to measure from the to the . ANS: tip of the nose; tip of the ear; xiphoid process Using landmarks individualizes the tube length. DIF: Cognitive Level: Application REF: m 498, Skill 27-2 OBJ: Clinical Practice #3 TOP: NG Tube Insertion KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse recommends to a patient who desires weight reduction to engage in a minimum of minutes of exercise most days of the week. ANS: 30 minutes Thirty minutes Physical exercise of moderate intensity for 30 to 60 minutes most days of the week is an effective support to weight reduction multigrain bread. • baked potato. • soups. • fruit juices. AN S: A, si ur yn w w w .m • m i l k p r o d u c t s . ng • te st pr ep .c om DIF: Cognitive Level: Comprehension REF: m 482, Table 27-1 OBJ: Theory #4 TOP: Weight Reduction KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • The nurse takes into consideration that excessive intake of saturated and trans-fat leads to the development of fatty deposits being laid down in the walls of the blood vessels and causing . ANS: atherosclerosis Excessive intake of saturated and trans-fat leads to the development of fatty deposits being laid down in the walls of the blood vessels called atherosclerosis. DIF: Cognitive Level: Knowledge REF: m 483 OBJ: Theory #4 TOP: Atherosclerosis KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease MULTIPLE RESPONSE • A nurse instructs a patient who is to receive a soft diet that the diet will include: (Select all that apply.) • eggs. closer proximity to the heart. • more effective monitoring from the IV pump. • for adequate blood flow. st pr • ep .c om D, E, F Soft diets are low in fiber, and foods have a soft consistency. Foods allowed on a soft diet include eggs, breads without seeds, boiled or mashed potatoes, soups, fruit, juices, tender cooked vegetables, ground meats or meats cooked until soft, cooked cereals, and milk products. DIF: Cognitive Level: Comprehension REF: m 480 OBJ: Theory #1 TOP: Nutrition KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • When the patient complains about the insertion of the total parenteral nutrition (TPN) tube interfering with his movement, the nurse explains that the insertion in the subclavian vein allows: (Select all that apply.) • adequate dilution of TPN solution. for more ease in dressing insertion site. ANS: A, D The placement in the subclavian provides a large vein with large blood flow, which dilutes the TPN to keep venous irritation at a minimum and ensures better distribution. DIF: Cognitive Level: Application REF: m 496 OBJ: Theory #10 TOP: Insertion Site KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse giving a bolus feeding through a nasogastric tube with a syringe would: (Select all that apply.) • pull up 50 mL of formula in the syringe. w w .m yn ur si ng te • lower the head of the bed to flat position. • allow feeding to flow in by gravity. • flush the tube with 50 mL of water. w • • chec k the positi on of the tube. .c om ANS : C, E The nurse should roll up the head of the bed, check the placement of the tube, allow 30 mL of formula to flow in by gravity, and flush the tubing with 30 mL of water. DIF: Cognitive Level: Application REF: m 498 OBJ: Theory #2 TOP: Nutrition KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse caring for a patient diagnosed with AIDS would include in the nutritional plan of care: (Select all that apply.) • asking the patient about sexual history. encouraging the patient to eat solid foods high in protein. • offering the patient supplements such as Ensure. • obtaining an order for a dietitian consult. • urging patient to eat three well-balanced meals per day. st pr ep • offer pureed foods when the patients mouth is painful. ANS: C, D, F Solid food may be difficult to eat, so consulting with a dietitian and having the patient eat foods that are high in protein and that are bland or pureed are very appropriate. AIDS patients should eat small meals several times a day. DIF: Cognitive Level: Application REF: m 496 OBJ: Theory #3 TOP: HIV/AIDS and Nutrition KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse counsels the bulimic patient that her eating disorder can lead to serious conditions such as: (Select all that apply.) • esophageal ulcers. w w .m yn ur si ng te • diverticulitis. w • • ulcerative colitis. • peptic ulcers. • c o n g e s brown rice. w • w .m yn ur si ng te st pr ep .c om t i v e h e a r t f a i l u r e . A N S : A , D Long-term bulimic patients may acquire serious conditions such as esophageal and peptic ulcers. DIF: Cognitive Level: Comprehension REF: m 481 OBJ: Theory #4 TOP: Eating Disorders KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • The nurse suggests to a diabetic patient to eat complex carbohydrates, which include: (Select all that apply.) • whole grain foods. w • • • s w e e t p lima beans. legumes. si ng te st pr ep .c om o t a t o e s . A N S : A , B , D Complex carbohydrates include whole grain foods, brown rice, legumes, and whole grain pasta. DIF: Cognitive Level: Comprehension REF: m 484 OBJ: Theory #1 TOP: Complex Carbohydrates KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • Fluid overload is suspected in an 82-year-old patient who is receiving total parenteral nutritional therapy (TPN) when the nurse assesses: (Select all that apply.) • excessive urine output. increased pulse rate. • dyspnea. • hyperactive bowel sounds. • w w w c o m p l a i n t o f h e a .m yn ur • pr ep .c om d a c h e . A N S : A , B , C Indications of fluid overload include output exceeding intake, increased pulse rate, dyspnea, cough, and crackles. w w .m yn ur si ng te st Chapter 30 Urinary Elimination The nurse caring for a severely dehydrated patient who has a Foley catheter in place assesses the patient to confirm adequate urine _ mL. perfusion by the urine output of a. 15 b. 30 c. 45 d. 60 ANS: B There should be an average hourly urine output of 30 mL. DIF: Cognitive Level: Knowledge REF: m 537 OBJ: Clinical Practice #1 TOP: Urinary Output KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • To help reduce a patients risk of recurrent cystitis, the nurse teaches the patient to: • eat citrus fruits to alkalinize the urine. always wipe the perineal area from back to front. • take long, warm bubble baths. w • • wear cotton underwear and avoid nylon or constrictive clothing. ANS: D The patient should wear cotton underwear and avoid nylon and constrictive clothing that worsens perineal moisture. DIF: Cognitive Level: Comprehension REF: m 538, Health Promotion OBJ: Clinical Practice #1 TOP: Prevention of Urinary Infections KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and detection of disease • The nurse is aware that in the elderly, a urinary infection may cause the patient to: • run an exceptionally high temperature. • have foul urine and diarrhea. • become disoriented and confused. • .m yn ur si ng te st pr ep .c om b e c o m e i r r i t a b l e . A N S : C Urinary infections in the elderly patient may not be manifested by fever. There are subtle changes in mental status. w w w DIF: Cognitive Level: Comprehension REF: m 538, Elder Care OBJ: Clinical Practice #1 TOP: Urinary Infection in the Elderly KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • To prevent changes in the chemical characteristics of urine, a nurse sends a sample of fresh urine to the laboratory for urinalysis within at least minutes. • 1 to 2 • 3 to 5 • 5 to 10 • 20 to 30 ANS: C Urine that stands for 15 minutes or longer changes characteristics, and the urinalysis will no longer be accurate. DIF: Cognitive Level: Comprehension REF: m 539 OBJ: Clinical Practice #1 TOP: Urinalysis KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient has been ordered to have a 24-hour urine collection as part of a diagnostic workup. The action taken to perform this procedure correctly is to: • continue the collection if the patient accidentally voids directly into the toilet. obtain a container and put it in a warm water bath in the bathroom. • have the patient void at the beginning of the collection and throw it away. om • have the patient void for the last time a few hours before the collection ends. ANS: C The patients bladder should be empty when the test begins; for this reason, the urine obtained at the start time is discarded and the urine collected should be stored on ice during the 24-hour period. DIF: Cognitive Level: Application REF: m 540 OBJ: Clinical Practice #1 TOP: 24-Hour Urine Collection KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse would modify the urine collection technique when a urine sample is needed from an infant by: • placing the infant on a bedpan after removing the diaper. ur si ng te st pr ep .c • removing the diaper after the infant voids and send the diaper to the laboratory. • attaching a bag with adhesive backing to the skin surrounding the genitals. yn • applying a very small condom catheter. ANS: C A urine collection bag is attached to the skin by an adhesive backing and is placed so that it surrounds the genitals; when sufficient urine is collected, the bag is removed and urine is put into a specimen cup to send to the laboratory. DIF: Cognitive Level: Application REF: m 540 OBJ: Clinical Practice #1 TOP: Urinary Collection Bag KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort w w w .m • • The nurse is admitting a patient with suspected urolithiasis. An appropriate nursing intervention in the care of such a patient would be to: • place a sieve over the commode. • obtain an order for indwelling urinary catheter. • place a graduated cylinder near the commode. • w w w .m yn ur si ng te st pr ep .c om a t t a c h a u r i n a r y l e g b a g . A N S : A When a patient is suspected of having urolithiasis (a urinary stone), the urine is strained through a fine sieve. DIF: Cognitive Level: Application REF: m 540 OBJ: Clinical Practice #1 TOP: Strained Urine Specimen KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • When the patient who has an order to be out of bed complains of feeling too weak to walk to the bathroom, the nurse assists the patient with urination elimination by: • acquiring a walker so that the patient can go to the bathroom. • using a fracture bedpan and keep the patient flat. • obtaining a raised toilet seat. placing a commode at the bedside. ANS: D A bedside commode allows the patient to get out of bed to void and does not tire the patient who feels weak. Allowing a weak patient to ambulate unassisted puts the patient at risk for a fall. DIF: Cognitive Level: Application REF: m 541 OBJ: Clinical Practice #4 TOP: Urinary Elimination KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk • A nurse is observing a nursing assistant offering a bedpan to a patient. The nurse will intervene if the nursing assistant: • closes the bedside curtain. ep .c om • dons clean gloves. • keeps the head of the bed flat after placing the bedpan. st pr • asks the patient to bend his knees and press down with his feet. ANS: C The head of the bed should be raised to 30 degrees after the bedpan is placed unless specifically contraindicated. DIF: Cognitive Level: Application REF: m 544, Skill 29-1 OBJ: Clinical Practice #4 TOP: Assisting with Toileting KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse can assist a patient who needs to void but cannot begin the urinary stream by: • running water in a nearby sink. w pouring cool water over the perineum. w • .m yn ur si ng te • • distracting the patient with conversation. ANS: A The sound of running water helps a patient start voiding. DIF: Cognitive Level: Application REF: m 546 OBJ: Theory #3 TOP: Strategies to Assist with Voiding KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • An adult male patient who cannot void has an order to have a urinary catheter inserted. Which size catheter would be w • inserting an indwelling catheter. most appropriate to use? • 12 French • 16 French • 18 French • .m yn ur si ng te st pr ep .c om 2 2 F r e n c h A N S : C The average-sized urinary catheter used for an adult male is 18 to 20 French. DIF: Cognitive Level: Knowledge REF: m 547 OBJ: Theory #4 TOP: Indwelling Catheter KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • An elderly male patient needs to have a condom catheter applied. An appropriate technique is to: • shave the perineal area before beginning. apply povidone-iodine to the penis before catheter application. • apply an adhesive strip in a circle around the base of the penis. leave 1 to 2 inches between the tip of the penis and the drainage part of the catheter. ANS: D The catheter is placed so that 1 to 2 inches of space are left to allow for urine to drain away from the penis. DIF: Cognitive Level: Comprehension REF: m 548, Skill 29-2 OBJ: Theory #6 TOP: Condom Catheter KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient who underwent prostate surgery is admitted to the surgical unit with a catheter that is used to provide continuous irrigation. The nurse recognizes this catheter is a(n): • Alcock. w w • w • • Malecot. • Coud catheter. • .m yn ur si ng te st pr ep .c om d e P e z z e r c a t h e t e r . A N S : A An Alcock catheter is used for bladder irrigation following prostate surgery. DIF: Cognitive Level: Knowledge REF: m 547 OBJ: Theory #5 TOP: Continuous Bladder Irrigation KEY: Nursing Process Step: Planning w w w MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse is cleansing the perineal area of a female patient who is having a urinary catheter inserted. The nurse should use the last povidone-iodinesoaked cotton ball to cleanse downward over the: • urinary meatus. • p e • left labia. • right labia. om yn ur si ng te st pr ep .c r i r e c t a l a r e a . A N S : A The urinary meatus is cleansed after the labia on each side are cleansed. DIF: Cognitive Level: Comprehension REF: m 550, Skill 29-3 OBJ: Clinical Practice #5 TOP: Catheterizing the Female Patient KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • When attempting to catheterize a male patient, there is resistance to catheter insertion. The nurses initial intervention should be to: • withdraw the catheter and start over. ask the patient to take a deep breath. • ask the patient to bear down and hold his breath. w ask that the patient lie on the right side. ANS: B If resistance is met, the catheter should be twisted, and the patient should be asked to take a deep breath, which relaxes the urinary sphincter. DIF: Cognitive Level: Application REF: m 553, Skill 29-3 OBJ: Clinical Practice #5 TOP: Catheterizing the Male Patient KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient has just had a urinary drainage catheter removed. The nurse plans to measure intake and output for this patient for w w • .m • another hours. • 1 to 2 • 4 to 6 • 6 to 8 ep .c om • 12 to 24 ANS: D Measuring intake and output for 12 to 24 hours after catheter removal allows time to note whether the bladder is draining adequately. DIF: Cognitive Level: Application REF: m 557 OBJ: Clinical Practice #1 TOP: Removal of Indwelling Catheter KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A male patient who suffered a spinal cord injury is learning to perform self-urinary catheterization before being discharged to home. The statement made by the patient that indicates more instruction is needed is: It is a sterile procedure. • The catheter should be pinched before it is withdrawn. • The penis is lifted to a 60- to 90- degree angle for catheter insertion. te st pr • The procedure is done sitting on the toilet. ANS: A Urinary catheterization in the home after spinal cord injury is usually a clean procedure rather than a sterile one. DIF: Cognitive Level: Analysis REF: m 558, Patient Teaching OBJ: Theory #4 TOP: Self-Catheterization KEY: Nursing Process Step: Application MSC: NCLEX: Physiological Integrity: basic care and comfort • An adult patient has an order to have his urinary catheter irrigated with normal saline. The nurse plans to draw up how much solution into the sterile irrigation syringe? • 1 to 20 mL w w w .m yn ur si ng • • 5 0 t o • 20 to 30 mL • 30 to 40 mL te st pr ep .c om 6 0 m L A N S : C The appropriate amount of solution to draw into the syringe for irrigation is 30 to 40 mL in an adult patient, which provides effective irrigation without risking overdistention of the bladder. DIF: Cognitive Level: Application REF: m 559, Skill 29-5 OBJ: Theory #4 TOP: Bladder Irrigation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse irrigating a patients indwelling urinary catheter should instill normal saline as ordered, and then: • unclamp the tubing and lower the collection bag. massage the patients bladder. • ask the patient to take a deep breath and hold it. ng • keep the tubing clamped for 30 to 45 minutes. ANS: A Immediately after irrigating a urinary catheter, the tubing should be unclamped and the collection bag lowered below the level of the bladder for proper drainage. DIF: Cognitive Level: Application REF: m 559, Skill 29-5 OBJ: Theory #4 TOP: Irrigation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse is reinforcing instructions about Kegel exercises with a female patient. An appropriate instruction is to: • do the exercises 12 times each day. w w w .m yn ur si • • hold each muscle contraction for a count of 3 seconds. • tighten the abdominal muscles. • ti g yn ur si ng te st pr ep .c om ht e n th e p el vi c m u sc le s. A N S: D Kegel exercises involve tightening the pelvic muscles to reduce the likelihood of urinary incontinence. DIF: Cognitive Level: Application REF: m 562, Patient Teaching OBJ: Clinical Practice #7 TOP: Kegel Exercises KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse is documenting the removal of a urinary drainage catheter from an assigned patient. If the catheter is removed at 9:00 AM, the nurse recognizes that the patient is due to void by: a. 11:00 AM. .m b. 12 noon. c. 5:00 PM. w w w d. 9:00 PM. ANS: C Documentation of removal of a urinary catheter should include the time the patient is due to void, which is within 8 hours. DIF: Cognitive Level: Comprehension REF: m 564 OBJ: Clinical Practice #1 TOP: Voiding After Urinary Drainage Catheter Removal KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient with a history of cystitis had surgery 24 hours ago and is now unable to void. A bladder scan indicates that he has approximately 400 mL of retained urine. The nurse anticipates that the least invasive intervention the physician will order would be: • inserting an indwelling Foley catheter. • monitoring intake and output. • obtaining a midstream specimen. applying Creds maneuver to the bladder. ANS: D Creds maneuver is less invasive and may be used before invasive measures are taken. The bladder is gently massaged from the top of the bladder and rocking the palm of the hand steadily downward. DIF: Cognitive Level: Application REF: m 546 OBJ: Clinical Practice #4 TOP: Plan of Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse is caring for a patient with prostate enlargement who has an indwelling catheter. As the nurse is attaching a portion of the catheter to the patients abdomen, the patient asks why this is being done. The correct response is: • Taping the catheter to your abdomen will prevent pulling on the meatus. st pr ep .c om • The catheter cant be pulled out if it is taped to your abdomen. • Taping it in this way enhances the draining of your bladder. ng te • This will prevent the Foley catheter from kinking. ANS: A When the catheter is taped to the abdomen, it prevents pulling on the meatus, thus decreasing irritation. DIF: Cognitive Level: Comprehension REF: m 552, Skill 29-3 OBJ: Clinical Practice #5 TOP: Catheter Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse instructing a female patient on obtaining a clean catch urine specimen should stress to: • spread the labia apart and clean the center area first. w w w .m yn ur si • • catch the middle portion of urine after voiding a small amount into the toilet. • carefully collect the urine in the container as soon as the urine stream starts. • fill the urine cup to the brim to ensure an adequate sample. ANS: B The procedure for a midstream or clean-catch urine specimen is to void a small amount of urine into the toilet and to catch the middle portion of urine by moving the container into the stream. DIF: Cognitive Level: Comprehension REF: • glucose. • leukocytes. • ketones. om m 539 OBJ: Clinical Practice #2 TOP: Clean-Catch Urine Specimen KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient is being assessed for a possible urinary tract infection in the outpatient clinic. Before sending a urinalysis specimen to the laboratory, the nurse collects a small amount of urine in order to perform a dipstick test in order to detect: • protein. yn ur si ng te st pr ep .c ANS: C A dipstick test is performed to test for different components and, in this case, for white blood cells or leukocytes, which indicate an infection. The accurate timing of the reading is essential to the accuracy of the result. DIF: Cognitive Level: Analysis REF: m 539 OBJ: Clinical Practice #2 TOP: Dipstick Test KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort COMPLETION • The nurse should provide enough hydration for the patient so that hours. the patient can void at least every ANS: 8 eight Each patient should void at least every 8 hours unless there is a catheter in place. w w w .m DIF: Cognitive Level: Knowledge REF: m 539 OBJ: Clinical Practice #1 TOP: Frequency of Urination KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort MULTIPLE RESPONSE • A nurse instructing a patient about how to prevent recurrent cystitis would include: (Select all that apply.) • increase fluid intake to 2500 to 3000 mL/day. • consume more citrus fruits and juice. • wear cotton underwear. • wipe the rectal area from front to back after a bowel movement. • avoid sitting in a wet bathing suit for extended periods. • empty the bladder st pr ep .c om every 2 to 3 hours. ANS: A, C, D, E, F Cystitis and other urinary tract infections may be avoided by increasing fluid intake to 2500 to 3000 mL/day, avoiding citrus fruits and juice because they cause alkaline urine (bacteria grow more readily in alkaline urine); always wiping the rectal area from front to back after a bowel movement; wearing cotton underwear; not sitting around in a wet bathing suit for extended periods; and emptying the bladder every 2 to 3 hours to prevent stasis and potential for bacteria to multiply if present. DIF: Cognitive Level: Application REF: m 537, Health Promotion OBJ: Theory #3 TOP: Infection Prevention KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patients urinalysis results are available. Which of the following are considered normal characteristics? (Select all that apply.) • Straw-colored Specific gravity (SpG), 1.015 • pH, 6.0 • RBCs, more than 1 per high-power field ng si w w w .m yn ur • C l o u d y a p p e a r a n c e A N S te • • blockage of the pancreatic duct. • recent excessive intake of milk products. pr • ep .c Chapter 31 Bowel Elimination The nurse has assessed that a patients stool has changed from brown to dark black and sticky. The nurse suspects: • blockage of the bile duct. om : A , B , C Urine is normally straw colored; SpG and pH are within normal range; RBCs are abnormal findings; and cloudy urine may indicate a large amount of protein. w w w .m yn ur si ng te st p r e s e n c e o f o c c u l t b l o o d . A N S : D Occult or old blood is suspected when stool changes from a normal brown appearance to a dark • frothy and foul smelling. • very liquid and streaked with blood. om black color with a sticky appearance. DIF: Cognitive Level: Analysis REF: m 569 OBJ: Theory #2 TOP: Stool Characteristics KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse has documented that a patient has had two episodes of steatorrhea, which means that the character of the stool is: • hard and clay colored • w w w .m yn ur si ng te st pr ep .c so ft a n d fil le d w it h m u c us . A N S: B Steatorrhea is defined as stools with abnormally high fat content that are usually frothy, foul smelling, and float on water. DIF: Cognitive Level: Comprehension REF: m 569 OBJ: Theory #2 TOP: Terminology KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse should plan interventions to combat constipation in a patient: • being treated for diabetes mellitus. • who has a routine order for Metamucil. • who just completed barium studies of the bowel. • with orders to ambulate with • the medication with a large amount of fluid. • an ove rthe -co unt er ant aci d. AN S: C ep a fat-soluble vitamin. yn ur si ng te st pr • .c om assistance. ANS: C A patient who is undergoing barium radiograph studies is more prone to constipation than are the other patients. DIF: Cognitive Level: Application REF: m 570 OBJ: Theory #3 TOP: Abnormal Characteristics of Stool KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • An elderly patient who routinely takes the bulk-forming laxative psyllium (Metamucil) is counseled by the home health nurse that in order to prevent constipation and possible fecal impaction, this patient should be sure to take: • extra vitamin C. w w w .m A large amount of fluid should be taken to prevent constipation and fecal impaction when using a product with psyllium. DIF: Cognitive Level: Comprehension REF: m 570 OBJ: Clinical Practice #1 TOP: Abnormal Characteristics of Stool KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient calls the nurse at the health clinic and reports that since his trip to Mexico, he has been experiencing diarrhea. The nurse suggests he try the antidiarrheal drug: • docusate sodium (Colace). • • loperamide (Imodium). • polycarbophil (FiberCon). K o o l A i d A ginger ale • Gatorade w w • w • .m yn ur si ng te st pr ep .c om s e n n a ( S e n o k o t ) . A N S : B Loperamide (Imodium) is an antidiarrheal; the rest are used to prevent or treat constipation. DIF: Cognitive Level: Comprehension REF: m 571, Box 30-2 OBJ: Theory #1 TOP: Medication for Diarrhea KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies • An elderly resident in a long-term care facility has experienced constant diarrhea for 3 days and is now exhibiting signs and symptoms of dehydration. The nurse initiates an intervention to offer small amounts of _ frequently. • a cola beverage ep .c om N S : C The patient may be developing electrolyte imbalance because of the diarrhea, so the best fluid source to offer is Gatorade, which has sodium and potassium. This should be offered 1 to 2 ounces at a time. DIF: Cognitive Level: Application REF: m 571, Elder Care OBJ: Clinical Practice #1 TOP: Abnormal Characteristics of Stool KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient who has started antibiotic therapy is having diarrhea as a side effect of the medication. The nurse should encourage the patient to eat: • yogurt. raisins. • gelatin fruit-flavored dessert (e.g., Jell-O). pr • ng te st • poultry. ANS: A Diarrhea results from the loss of normal intestinal bacteria that are also killed during treatment with antibiotics used to treat a different infection; eating yogurt or drinking buttermilk can help restore normal intestinal flora. steatorrhea. w • w .m yn ur si DIF: Cognitive Level: Comprehension REF: m 574, Patient Teaching OBJ: Clinical Practice #1 TOP: Abnormal Characteristics of Stool KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies • The nurse caring for a patient with lactose intolerance would anticipate the need to offer interventions for: • diarrhea. constipation. w • • h e m o r r h o i yn ur si ng te st pr ep .c om d d i s c o m f o r t . A N S : A Lactose intolerance is the name for the condition in which diarrhea occurs after consuming milk products. DIF: Cognitive Level: Knowledge REF: m 572 OBJ: Theory #2 TOP: Abnormal Characteristics of Stool KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse has performed abdominal assessments on four patients. After reviewing the findings, the nurse is least concerned about problems with bowel elimination for the patient with abdomen bowel sounds in all four quadrants. • nondistended, firm, with hypoactive nondistended, soft, with active • distended, firm, with hypoactive .m • • w w w distend ed, soft, with hyperac tive ANS: B Normal abdominal assessment data are an abdomen that is soft and nondistended and that has active bowel sounds in all four quadrants. DIF: Cognitive Level: Comprehension REF: m 572, Clinical Cues OBJ: Clinical Practice #3 TOP: Assessment: Bowels KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse is monitoring bowel elimination of a patient who has a history of constipation. The nurse implements measures to assist with bowel elimination if the patient has not had a bowel movement within how many days? 5 3 2 .c om a. b. c. d. 1 ANS: B If bowel evacuation has not occurred within 3 days, measures should be taken to assist the patient. DIF: Cognitive Level: Comprehension REF: m 573 OBJ: Theory #2 TOP: Abnormal Characteristics of Stool KEY: Nursing Process Step: Assessment st pr ep MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient has just completed a series of upper gastrointestinal tract radiographs that involved the use of barium as a contrast agent. Which measure will this patient need to help excrete the barium? • Diuretics and fluid restriction to 1.5 L Diuretics and fluid intake increased to 3.5 L • Laxatives and fluid restriction to 1.5 L te • Laxatives and fluid intake increased to 3.5 L ANS: D To get rid of the barium, the patients fluid intake should be increased to 3.5 L, or 3500 mL, and the patient should be given a laxative. DIF: Cognitive Level: Application REF: m 573 OBJ: Clinical Practice #1 TOP: Promoting Regular Bowel Elimination KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity • An ambulatory clinic patient telephones to report diarrhea and to ask for advice on medication to manage it. The best response by the nurse is, Do not use antidiarrheal medication for longer than hours without calling back for an appointment. a. 24 b. 48 c. 72 d. 96 ANS: B Antidiarrheal medication should not be continued for more than 48 hours without calling a physician. w w w .m yn ur si ng • DIF: Cognitive Level: Comprehension REF: m 574 OBJ: Clinical Practice #1 TOP: Promoting Regular Bowel Elimination KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies • There is an order to administer a cleansing enema to an adult patient before bowel surgery. The nurse will fill the enema bag with how many milliliters of fluid for this procedure? a. 500 to 1000 om b. 300 to 500 c. 200 to 300 te st pr ep .c d. 50 to 150 ANS: A The volume of the cleansing enema depends on the age of the patientfor adults, it is between 500 and 1000 mL. DIF: Cognitive Level: Application REF: m 577, Skill 31-1 OBJ: Clinical Practice #5 TOP: Enemas KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort A patient who is badly constipated has just received an oilretention enema. The nurse encourages this patient to try to hold the enema for at least how long before trying to have a bowel movement? • 10 minutes 15 minutes • 20 minutes .m yn • w w w • 4 0 m i n u t e s A N S : C ur si ng • • warm the solution in the microwave. • keep the solution at room temperature. om The oil-retention enema should be retained for 20 minutes. DIF: Cognitive Level: Comprehension REF: m 578 OBJ: Clinical Practice #5 TOP: Retention Enemas KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies • A nurse is preparing a cleansing enema for an adult patient who is constipated and has not responded to laxative use. Before giving the enema, the nurse should: • cool the solution to 70 F. • w w w .m yn ur si ng te st pr ep .c wa rm the sol uti on to 10 5 F. A N S: D Solution that is too cool cannot be retained, and solution that is too hot may cause injury to rectal tissues; it is best to warm it to 105 F. DIF: Cognitive Level: Application REF: m 585, Steps 30-3 OBJ: Clinical Practice #5 TOP: Cleansing Enemas KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient scheduled for bowel surgery has an order to receive enemas until clear. The nurse is aware that no more than three enemas should be given because: • repeated enemas may cause more flatus. • the patient may develop an irritated rectum. • repeated enemas may cause electrolyte imbalance. • the patient may develop severe diarrhea. ANS: C pulse rate decreases from 78 to 52 beats/min. • respiratory rate increases from 16 to 24 breaths/min. .c • om No more than three large-volume enemas are given because of possible electrolyte depletion. DIF: Cognitive Level: Comprehension REF: m 576, Safety Alert OBJ: Clinical Practice #5 TOP: Enemas KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk • A nurse is digitally removing a fecal impaction from a patient. The nurse should stop the procedure immediately and take corrective action if the patients: • blood pressure increases from 110/84 to 118/88 mm Hg. temperature increases from 98.8 F to 99.0 F. ANS: B Stimulation of the sphincter may cause a vagal response as evidenced by bradycardia. DIF: Cognitive Level: Application REF: m 579, Steps 30-1 OBJ: Clinical Practice #1 TOP: Fecal Impaction KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: reduction of risk • A nurse is reinforcing teaching with a patient who will begin a bowel training program. An intervention this program does not include is: • regularly scheduled time for toileting. fluid intake of at least 2500 mL daily. • use of a suppository. w .m • w • yn ur si ng te st pr ep • w u s e o f a n e n e m a ep .c om . A N S : D Enemas and stronger laxatives are not considered a part of the program. DIF: Cognitive Level: Comprehension REF: m 579, Box 30-3 OBJ: Theory #2 TOP: Bowel Training KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse is assisting a patient with a new continent ileostomy to catheterize the internal reservoir to drain the ileostomy. When the catheter meets resistance from the internal valve, the nurse should: • have the patient take a deep breath and apply gentle pressure over the area. withdraw the catheter and start again with a new one. • ask the patient to bear down and hold her breath. st pr • coat the opening with petroleum jelly or a water-soluble lubricant. ANS: A For some patients the taking of a deep breath relaxes muscles and allows passage of the catheter. DIF: Cognitive Level: Application REF: m 581, Steps 30-2 OBJ: Clinical Practice #7 TOP: Ileostomy KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity • A patient with a new colostomy should have the hole in the faceplate cut to allow inch around the stoma. • 1 w w .m yn ur si ng te • 1 w • c. d. ANS: D The faceplate should allow inch around the colostomy stoma. DIF: Cognitive Level: Knowledge REF: m 584, Skill 30-2 OBJ: Clinical Practice #8 TOP: Colostomy Faceplate KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse is caring for a patient who had bowel surgery 3 days ago and is now beginning to have a well-functioning ostomy. The ostomy drainage bag should be emptied whenever it is: • one-fourth full. • one-half full. • three-fourths full. • full. • cucumbers. • beans. ur eggs. yn • si ng te st pr ep .c om ANS: B The ostomy bag should be changed when it is one-third to one-half full so that the weight of the bag will not detach it. DIF: Cognitive Level: Knowledge REF: m 584, Skill 30-2 OBJ: Clinical Practice #8 TOP: Ostomy Bag KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient with a colostomy asks about foods that can be eaten that will reduce odor in the ostomy drainage bag. The most informative response by the nurse is to say that ostomy odor can be decreased with the intake of: • buttermilk. w w w .m ANS: A Buttermilk is among the suggested foods that decrease ostomy bag odor. DIF: Cognitive Level: Comprehension REF: m 582 OBJ: Clinical Practice #8 TOP: Ostomy Bag KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse is caring for an anxious patient who is scheduled for surgery for colostomy placement. While the nurse is talking to the patient, the patient states, I am so scared. The nurses most supportive response would be: • Surgeries like yours are very safe. • What about your colostomy scares you? • Why are you scared? • Sounds like someone has been telling you horror stories. ANS: B The nurse needs to address the patients anxiety and fear first by use of open-ended questioning, because the patient might be focused on a variety of things, including poor body image or the prospect of death. Asking a Why question is not therapeutic and makes the patient defensive. DIF: Cognitive Level: Application REF: m 580 OBJ: Theory #5 TOP: Preoperative Colostomy KEY: Nursing Process Step: Implementation • absorb food substances from the bloodstream. return water from the waste material to the bloodstream. ANS: C The small intestine processes the chyme into a more liquid state and absorbs food substances into the bloodstream. All other listed functions are those of the large intestine. DIF: Cognitive Level: Knowledge REF: m 568 OBJ: Theory #5 TOP: Intestinal Digestion KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse caring for a patient who had a colostomy 2 days ago assesses slight bleeding around the stoma when the area is cleansed, colostomy bag filled with gas, pale stoma, and a reddened area under the adhesive of the appliance. The assessment that should be reported immediately is the assessment pertaining to the: • skin irritation. bleeding around the stoma. w • w .m yn ur si ng te st pr • .c propel waste material toward the anus. ep • om MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse reminds the patient that digestion of food is a complex process with much of the food breaking down in intestines. The small intestine functions to: • reabsorb sodium and chlorides. w • • p a l e s t o amount of gas in the bag. te st pr ep .c om m a . A N S : D The pale stoma indicates a compromised blood supply and should be reported immediately to the physician. DIF: Cognitive Level: Analysis REF: m 582, Clinical Cues OBJ: Clinical Practice #8 TOP: Colostomy Stoma KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and early detection of disease • The patient asks the nurse how an ileostomy differs from a colostomy. The most informative response by the nurse would be that a(n): ileostomy is performed to remove stool from the colon, whereas a colostomy is the removal of lowe • diverting intestinal contents. ileostomy has effluent that is more formed, whereas a colostomy has effluent that is liquid. • colostomy is an opening into the colon, whereas an ileostomy is an opening at the ileum. ur si ng • ileostomy requires irrigating, whereas a colostomy requires catheterizing. ANS: C The colostomy is an opening into the colon, with formed effluent requiring irrigation, whereas the ileostomy is an opening in the ileum, with liquid effluent requiring catheterizing. DIF: Cognitive Level: Comprehension REF: m 582 OBJ: Theory #7 TOP: Intestinal Diversions KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort w w w .m yn • • The patient with the new colostomy is concerned about how to control diarrhea of the effluent. The nurse suggests that diarrhea can be controlled by the intake of: • cheese. • apple juice. • raw vegetables. • beams. .m yn ur si ng te st pr ep .c om ANS: A Cheese can control or decrease the incidence of diarrhea in a colostomy. DIF: Cognitive Level: Comprehension REF: m 582 OBJ: Clinical Practice #1 TOP: Control of Diarrhea KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort COMPLETION • The gastrocolic reflex initiates . ANS: peristalsis. Peristalsis is initiated by the gastrocolic reflex, which creates the urge to defecate. DIF: Cognitive Level: Knowledge REF: m 568 OBJ: Theory #1 TOP: Bowel Elimination KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The nurse assesses a pale, light gray stool and recognizes that the cause of this abnormal color is due to an obstruction in the duct. ANS: bile An obstruction in the bile ducts prevents bile salts from entering the bile. Bile salts give the feces its characteristic brown color. DIF: Cognitive Level: Comprehension REF: m 569 OBJ: Theory #2 TOP: Bowel Elimination KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse reminds a group of older adults that a colonoscopy is recommended every w w w year(s) after the age of 50. ANS: 10 ten Healthy People 2020 recommends a colonoscopy every 10 years in persons over the age of 50. DIF: Cognitive Level: Knowledge REF: m 569 OBJ: Clinical Practice #1 TOP: Colonoscopies KEY: Nursing Process Step: N/A MSC: NCLEX: N/A MULTIPLE RESPONSE • The nurse instructs the patient who has had an ileostomy to modify the diet to include: (Select all that apply.) • increase the protein intake. • choose foods that are high in calories. • select foods that have a milk base. • eat raw vegetables and fruits. include whole grain products in diet daily. ANS: A, B Patients with ileostomies have lost their lower bowel and need food sources that are high in calories and vitamins. Water intake should be up to 10 cups a day to make up for the water reabsorption usually done in the colon. High residue foods such as whole grain products and raw vegetables and fruits can irritate the intestine. DIF: Cognitive Level: Comprehension REF: m 582, Patient Teaching OBJ: Theory #7 TOP: Food Appropriate for Ileostomies KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • The nurse points out that age-related changes in the intestinal tract are relatively insignificant. The changes include: (Select all that apply.) • atrophy of the villi in the small intestine. ng te st pr ep .c om • increased incidence of hemorrhoids. • decreased absorption of fats and vitamin B12. • creation of excessive flatus. ur si • decreased motility in the large intestine. ANS: A, C, D With age there is a decrease in the villi in the small intestine that decreases the absorption of fats and vitamin B12. Motility frequently decreases in the large intestine. DIF: Cognitive Level: Comprehension REF: m 568 OBJ: Theory #1 TOP: Age-Related Changes in the Intestinal Tract KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse instructs a patient with a new colostomy against eating food that may cause an obstruction. These foods include: (Select all that apply.) • spicy foods. w w w .m yn • • whole-kernel corn. • cucumbers. • tomatoes. Chapter 32 Oral Medications MULTIPLE CHOICE • Before the nurse administers a liquid medication to an 83year-old male patient, the nurse should: om • shrimp. ANS: B, D, E Whole-kernel corn, tomatoes, and shrimp are among the food that can cause an obstruction in a colostomy. assess the swallowing reflex by offering a sip of water. • ask the patient if he would prefer to give the medication to himself. • mix thoroughly in applesauce or pudding. pr ep .c • assess the ability to understand information relative to the drug. ANS: A A factor to consider when giving anything orally is the ability of the patient to swallow. DIF: Cognitive Level: Application REF: m 654, Skill 34-1 OBJ: Theory #7 TOP: Routes of Medication Administration KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk • The nurse receives an order to give vitamin D 10 mcg bid. The nurse recognizes that the abbreviation mcg refers to a measurement in: • milligrams. milliliters. w w • milliequivalents. w • .m yn ur si ng te st • • m i c r o g r a m with any licensed person. • with another nurse working on the shift. st • .c pr ep A N S: D The abbreviation mcg refers to a measurement of micrograms. DIF: Cognitive Level: Knowledge REF: m 644, Table 34-3 OBJ: Clinical Practice #4 TOP: Abbreviations KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: pharmacological therapies • The licensed nurse who is responsible for doing the narcotic count for the shift should count the drugs: • alone for accuracy. om s . with a nurse coming on duty for the next shift. ANS: D Controlled substances must be counted by one nurse going off duty and one coming on duty at the change of each shift. DIF: Cognitive Level: Comprehension REF: m 648 OBJ: Theory #1 TOP: Counting Controlled Substances KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • Before the nurse administers a dose of digoxin (Lanoxin) to a patient, the nurse should assess: • blood pressure. apical heart rate. w • respiratory rate. w • .m yn ur si ng te • w • l e v e l o f c o n ep .c om s c i o u s n e s s . A N S : C .m yn ur si ng te st pr The apical heart rate is measured before giving a dose of digoxin (Lanoxin) to determine whether it is safe to give; the apical rate should be greater than 60 beats/min for an adult patient. DIF: Cognitive Level: Application REF: m 654, Skill 34-1 OBJ: Theory #7 TOP: Medication Administration KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: pharmacological therapies • A nurse is administering oral medications to a patient who is having intake and output (I&O) measured. When giving medications, it is most important to: • give the medication with a small piece of cracker or cookie. give the medication with as much fluid as possible. • record the fluid taken on the MAR. record the fluid taken on the intake record. ANS: D When a patient is having I&O measured, the nurse must record all fluid that the patient drinks while taking medications in the oral intake column of the I&O sheet. DIF: Cognitive Level: Application REF: m 654, Skill 34-1 OBJ: Theory #1 TOP: Medication Administration KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort w w • w • • An elderly patient is having difficulty swallowing an entericcoated tablet for which there is no liquid form available. To help the patient swallow the dose more easily, the nurse should: • request the patient to tilt the chin down slightly to swallow. • crush the pill and administer it in applesauce. • use a spoon to place the tablet at the back of the tongue. take only a small sip of water to swallow the tablet. ANS: A If elderly patients have difficulty swallowing, they should swallow a sip of water first, then place the tablet toward the back of the tongue, then take a large sip of water. Finally, they should place the tongue on the roof of the mouth and swallow with the chin tilted downward, followed by another sip of water. Enteric-coated medications should not be crushed. DIF: Cognitive Level: Application REF: m 560, Elder Care OBJ: Theory #7 TOP: Safe Administration of Medications: Elderly KEY: Nursing Process Step: Implementation MSC: NCLEX: Pharmacological Integrity: reduction of risk • A patient complains about the taste of the sublingual nitroglycerin and admits that he swallows it rather than holding it under his tongue. The nurse explains that sublingual medications: • should not be swallowed because it alters the absorption potential. ng te st pr ep .c om • can be inserted rectally without loss of absorption potential. • can be held against the roof of the mouth with the tongue to reduce taste. • can be taken between the cheek and tongue to diminish taste. ANS: A .m yn ur si • w w w Sublingual medications are placed under the tongue and they should not be swallowed because that alters the absorption potential. DIF: Cognitive Level: Comprehension REF: m 651 OBJ: Theory #1 TOP: Medication Administration: Sublingual Route KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies • To reduce the systemic absorption of eye drops, the nurse should: • use finger pressure to close the eyelid tightly. • apply slight finger pressure over the lacrimal duct. • request the patient tilt the head slightly to the side of the unaffected eye. • instruct the patient to widen the eyes in order to increase access to the lacrimal duct. ANS: B Blocking the entrance to the lacrimal duct by placing a finger over it helps reduce systemic absorption of an eye drop. DIF: Cognitive Level: Application REF: m 656, Skill 34-2 OBJ: Clinical Practice #3 TOP: Medication Administration: Optic Route KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies • A patient is attempting to put pills in his mouth from a medicine cup and drops one pill on the bed sheet. The nurse should: • retrieve the pill from the linens and allow the patient to take it. scoop up the pill in a souffl cup and hand the cup to the patient. • discard the pill and get another from the dose pack. om • report the loss of the pill as a medication error. ANS: C A pill that is dropped on the dirty linen or the floor must be discarded and replaced from the dose pack. DIF: Cognitive Level: Application REF: m 649, Elder Care OBJ: Theory #1 TOP: Dropped Pill KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • For an adult patient who has an order to receive an otic medication, the nurse should plan to administer it by pulling the pinna: • down and forward. up and forward. • down and back. yn ur • w w w .m • u p a n d b a c k . si ng te st pr ep .c • A NS :D The pinna of the adult should be pulled up and back, whereas that of a child younger than 3 years of age is pulled slightly down and back. DIF: Cognitive Level: Application REF: m 68, Steps 34-1 OBJ: Clinical Practice #3 TOP: Medication Administration: Otic Route KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies • The nurse administering a nasal medication via an atomizer bottle should: • leave the other nostril open while giving the medication. have the patient squeeze the bottle while inhaling. • have the patient sit up straight. om • have the patient tilt the head forward. ANS: B The proper procedure for using an atomizer bottle is to have the head hyperextended, holding one nostril closed and squeezing the bottle and inhaling at the same time. DIF: Cognitive Level: Application REF: m 657 OBJ: Clinical Practice #2 TOP: Medication Administration: Nasal Route KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies • A nurse is providing instructions to a patient about how to use a metered-dose inhaler. The nurse should instruct the patient to: • lie down while taking the medication. ur si ng te st pr ep .c • gently roll the canister in the hands to mix the medication. • breathe out through the mouth before positioning the canister. yn • try to hold the breath for at least 3 seconds after inhaling the medication. ANS: C The patient should sit up or stand to take the medication, shake the canister to mix the medication with the propellant, breathe out through the mouth before positioning the canister, depress the cylinder, and hold the breath for at least 10 seconds before exhaling. DIF: Cognitive Level: Application REF: m 658 OBJ: Theory #4 TOP: Medication Administration: Inhalant Route KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies • The nurse explains that the patient with a respiratory disorder can open small airways to ease respiration effort with the use of: • albuterol (Proventil). w w w .m • • montelukast (Singulair). • ipratropium (Atrovent). colored red. • a smaller size than the older medication. • offered before a meal. yn ur si • w w w .m • i s i n l i q u i d f o r m . ng te st .c pr ep be clo me tha so ne (V an cer il). A N S: A Albuterol eases respiratory effort by opening the small airways. DIF: Cognitive Level: Comprehension REF: m 659, Table 34-5 OBJ: Theory #4 TOP: Use of Inhalants KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies • A patient of the Cambodian culture reports that a new medication is not adequate for treatment because it is: om • • left Sims st prone te • pr ep .c om A N S : B Persons of Cambodian origin believe the size of the medication indicates its curative value. A small pill does not have as much curative value as a larger one. DIF: Cognitive Level: Comprehension REF: m 650, Cultural OBJ: Theory #1 TOP: Medication Administration: Cultural Concerns KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: pharmacological therapies • For easier insertion of a rectal suppository, the nurse should position the patient in the position. • knee-chest ng • w w w .m yn ur si d o r s a l l i t h o t o m y A N S : C Placing the patient in the left Sims position provides for easier insertion of the suppository into the rectum. DIF: Cognitive Level: Comprehension REF: m 661, Steps 34-2 Chapter 33 Topical and Inhalant Medications A patient has an order for a nitroglycerin transdermal patch. The best way to ensure proper administration of this medication is to: • apply it behind the ear. • rotate sites to avoid skin irritation. • place it over a hairy skin area. put the initials on patch when applied. ANS: B A nitroglycerin transdermal patch should be applied to an area with good circulation, such as the chest, shoulders, or upper arm, and should be placed over hairless areas, with the date and the nurses initials written on the patch. Rotating sites prevents irritation. DIF: Cognitive Level: Application REF: m 662, Skill 34-3 OBJ: Clinical Practice #7 TOP: Medication Administration: Transdermal Route KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies • The nurse administering nitroglycerin ointment to a patient will: • apply with gloves or tongue blade. si ng te st pr ep .c om • apply in same area as the old patch. • place the paste on the chest and massage it in the skin. yn ur • inform the patient that the medicinal effect will take about 45 minutes. ANS: A The nurse should wear gloves to avoid exposure to nitroglycerin. The area of the old patch should be cleaned and the new patch placed in another area and not massaged in. The effect of the patch occurs in about 30 minutes. DIF: Cognitive Level: Application REF: m 662, Skill 34-3 OBJ: Clinical Practice #2 TOP: Medication Administration: Topical Route KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: pharmacological therapies • When the nurse sees the order for Milk of Magnesia 2 tablespoons, qod, hs, the nurse translates to mean he should give: • 1 ounce of Milk of Magnesia every other day at bedtime. w w w .m • • 1 ounces of Milk of Magnesia every day. • 2 tablespoons of Milk of Magnesia whenever necessary. • 2 ounces of Milk 20 to 30 • 15 to 20 ep • .c om of Magnesia every night. ANS: A The order is asking that 3 tablespoons (1 ounce) of Milk of Magnesia be given every other day at bedtime. DIF: Cognitive Level: Analysis REF: m 644, Table 34-3 OBJ: Theory #2 TOP: Abbreviations KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort 4 When administering medications to a patient with a feeding tube, the nurse should dissolve each crushed medication in at least mL of water. • 30 to 60 .m yn ur si ng te st pr • 5 to 15 ANS: B Each medication should be dissolved in 20 to 30 mL of water, which does not include the water used to flush the tube before and after giving medications. DIF: Cognitive Level: Comprehension REF: m 664, Skill 34-4 OBJ: Theory #8 TOP: Medication Administration: Feeding Tube KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: pharmacological therapies • Data pertaining to a patients medication therapy that the nurse should document in the nurses notes, in addition to charting in the medication administration record (MAR), is: • medication name and dose. the time of the medication. w • the route of the medication. w • medication side effects experienced . ANS: D Side effects of drug therapy are charted in the nurses notes. DIF: Cognitive Level: Comprehension REF: m 666 OBJ: Theory #3 TOP: Documentation KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: pharmacological therapies • A patient on the long-term care unit receives the wrong w • medication. The charge nurse should instruct which staff member to complete the incident report? • The nurse who administered the wrong drug • The nursing supervisor for the day • The nurse who discovered the error No one, because the charge nurse should do it ANS: C The nurse who discovers the error reports it and fills out the incident report. DIF: Cognitive Level: Application REF: m 666 OBJ: Theory #8 TOP: Medication Errors KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The physician writes a medication order on the order sheet of the patient. The order that includes all the necessary information is: • 1/5/13 @ 0900: Warfarin (Coumadin) 1 mg mo. qd A. Physician. pr ep .c om • 1/5/13 Give Warfarin 1 tab qd A. Physician. • 1/5/13 Coumadin 1 tab mo. A. Physician. • 0900 Give warfarin (Coumadin) 1 mg mo. A. Physician. ng te st • w w .m yn ur si ANS: A A complete drug order includes the full name of the drug, the dose to be given, the route of administration, how often the drug is to be given, and the date and time written, as well as the prescribers signature. DIF: Cognitive Level: Analysis REF: m 642 OBJ: Theory #1 TOP: Medication Orders KEY: Nursing Process Step: N/A MSC: NCLEX: N/ A • The nurse checking the MAR finds that an order for an antibiotic is now 8 days old. The nurse should: • check the medications, performing three medication checks. give the ordered medication. • contact the physician for a new order. w • • give the medication, then notify the physician. ANS: C The nurse contacts the physician for a new order. Antibiotic orders generally have a 5- to 7-day limit before they need to be renewed. DIF: Cognitive Level: Application REF: m 643 OBJ: Theory #1 TOP: Expired Orders KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse is to administer a dissolved medication via feeding tube. After donning gloves and attaching the irrigation syringe to the tube, the nurse should next: • instill the medication into the syringe slowly. draw the medication into the syringe and gently push into the tube. • flush the tubing with 15 to 30 mL of tap water and add the medication just as the water is about to om • flush the tubing with 15 to 30 mL of sterile water and add the medication just as the water is about t ANS: C The nurse should flush the tubing with tap water and add the medication as the water is about to finish. Administration of medication into the feeding tube should be done by gravity instillation, and pressure should be applied gently only if needed to initiate flow. DIF: Cognitive Level: Application REF: m 664, Skill 34-4 OBJ: Theory #8 TOP: Medication Administration: Feeding Tube KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • When administering several medications via feeding tube, the nurse should: • dilute each medication with at least 40 mL of water. si ng te st pr ep .c • mix each medication individually. • mix all medications together to facilitate administration. ur • use sterile gloves for the procedure. ANS: B Medications should be mixed separately to prevent clumping. DIF: Cognitive Level: Application REF: m 664, Skill 34-4 OBJ: Theory #8 TOP: Medication Administration: Feeding Tube KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies • In the event of a discrepancy in the count of the narcotics between the day shift and the evening shift, the day nurse is required to: • correct the count to the number of pills counted and sign full name. w w w .m yn • • write a report and give it to the charge nurse with signatures of both nurses. • notify the pharmacy of the discrepancy. remain on duty until the miscount is resolved. ANS: D The nurse of the ending shift must resolve the discrepancy before leaving the unit. DIF: Cognitive Level: Application REF: m 648 OBJ: Theory #1 TOP: Narcotic Discrepancy KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • There is an order to give a patient 45 mL of Maalox. The nurse oz. ANS: should administer 1.5 There are 30 mL in 1 oz. Using the D/H formula, the calculation is as follows: 45 / 30 mL/oz = 1.5 oz. .c om • liquid. w • w .m yn ur si ng te st pr ep DIF: Cognitive Level: Analysis REF: m 644, Table 34-3 OBJ: Clinical Practice #2 TOP: Conversions KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The nurse is aware that a medication error event that causes a patient death or causes serious injury to a patient is classified as a(n) event. ANS: sentinel The Joint Commission views an event that causes the patient death or causes serious injury a sentinel event and is followed up with a root cause analysis. DIF: Cognitive Level: Knowledge REF: m 666 OBJ: Theory #8 TOP: Sentinel Event KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The nurse is aware that medications that should not be crushed and administered through a feeding tube include: (Select all that apply.) • enteric-coated. sublingual. • buccal. • sustained-release. w • • a n t i w w w .m yn ur si ng te st pr ep .c om n e o p l a s t i c s . A N S : A , C , D , E , F Many oral medications can be given through a feeding tube. Liquid medications are best, but if a tablet is crushable or a capsule can be opened and the contents mixed with liquid, or if the liquid within the capsule can be aspirated with a needle and syringe, then the medication can be administered through the feeding tube. Medications that should not be crushed and administered through the tube are sublingual or buccal, enteric-coated, or sustainedrelease preparations or products with a carcinogenic potential (e.g., antineoplastics). DIF: Cognitive Level: Application REF: m 663 OBJ: Theory #6 TOP: Medication Administration KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: pharmacological therapies • When applying ophthalmic ointments, the nurse should: (Select all that apply.) • fill only the center of the conjunctival sac. • ask the patient to roll the eye around and from side to side. • remove excess ointment from the lid with a cotton ball. • ask the patient to close the eyelids tightly to distribute ointment. • remove gloves and perform • will hasten the action of the drug. • will take less medicine to make him well. will be painless because the needles are so sharp. ANS: B The parenteral route will hasten the action of the drug. Although the equipment is better, there is still some pain involved in a parenteral application. The parenteral method is not always the best way to administer a drug. DIF: Cognitive Level: Application REF: m 671 OBJ: Theory #2 TOP: Medication Administration: Parenteral KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies • To ensure the proper administration of a tuberculin test, the nurse will: • use a 3-mL syringe. yn ur si ng te st pr ep • .c When the 8-year-old child complains that he does not want to have a shot, the nurse explains that the use of a parenteral route: • is the best way to give medicine. om hand hygiene. ANS: B, C, E When the nurse administers ophthalmic ointment, the entire conjunctival sac should be filled, the patient should be asked to close the lids lightly and move eye about to distribute the medication, the excess ointment should be removed with a cotton ball, and hand hygiene should be performed. Chapter 34 Parenteral Medications choose a 21-gauge, 1-inch needle. • insert the needle at a 30-degree angle. .m • • w w w inj ect slo wl y to for ma ble b. AN S: D An intradermal injection should be done using a 1-mL syringe with a 25-, 27-, or 29- gauge 30 to 45 • 15 to 30 .c • om needle that is 5/8-inch long. The needle is inserted at a 15-degree angle, and medication is injected slowly to form a bump or a bleb underneath the skin. DIF: Cognitive Level: Application REF: m 682, Skill 35-1 OBJ: Theory #1 TOP: Medication Administration: Intradermal KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: pharmacological therapies • The best angle to insert the needle to administration an subcutaneous injection is at an angle of degrees. • 45 to 90 te st pr ep • 5 to 15 ANS: A The needle is inserted at a 45- or 90-degree angle depending on the needle length and the size of the patient. DIF: Cognitive Level: Comprehension REF: m 672, 686, Skill 35-2 OBJ: Theory #1 TOP: Medication Administration: Subcutaneous KEY: Nursing Process Step: Planning ur si ng MSC: NCLEX: Physiological Integrity: pharmacological therapies • The nurse computes the dose of medication as 2.4 million units of penicillin to be delivered in 4 mL. The nurse should: • give the 4 mL using a 5-mL syringe. inform the charge nurse that the dose is too large to be given IM. • divide the dose into two 3-mL syringes and give as a divided dose. yn • ask the physician if another drug can be used. ANS: C The maximum number of milliliters that can be injected into the dorsogluteal muscle is 3 mL. If the person has small muscle mass, or if the dose exceeds 3 mL, the dose should be divided into two doses. DIF: Cognitive Level: Analysis REF: m 688 OBJ: Theory #1 TOP: Intramuscular Medication Administration KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: pharmacological therapies • The nurse understands that the only part of the syringe that can be touched and not contaminated is the: • needle. w w w .m • • outside of the barrel. • sides of the plunger. • w w .m yn ur si ng te st pr ep .c om t i p o f t h e s y r i n g e . A N S : B The needle, inside of the barrel, sides of the plunger, and tip of the syringe must be kept sterile. DIF: Cognitive Level: Knowledge REF: m 673 OBJ: Clinical Practice #2 TOP: Injection Equipment KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A nurse has just administered a medication to a patient using a syringe that is not a safety syringe. To dispose of the needle and syringe safely, the nurse should: • recap the needle and dispose of it in the trash receptacle. recap the needle and dispose of it in the sharps container. • leave the needle uncapped and dispose of it in the trash receptacle. w • • leave the needle uncapped and dispose of it in the sharps container. ANS: D Needles are not to be recapped and should be deposited in the sharps container. DIF: Cognitive Level: Application REF: m 675, Safety Alert OBJ: Clinical Practice #2 TOP: Preventing Needle Sticks KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • When the nurse is preparing to draw medication from an ampule, the proper procedure is to: • allow medication to float freely in the body, neck, and stem. • wrap the neck with a gauze or alcohol sponge to the open ampule. • break the ampule so that it opens toward her. inject air into the ampule to ease the withdrawal of the medication. ANS: B The medication should rest in the body of the ampule before being withdrawn, and the neck should be wrapped to protect the nurse from glass cuts when the ampule is snapped open. DIF: Cognitive Level: Application REF: m 677, Clinical Cues OBJ: Clinical Practice #3 TOP: Using Ampules KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control When withdrawing medication from an ampule, the best needle to use is a needle. • • beveled • 1-inch • filter te 1-inch ng • st pr ep .c om • w w .m yn ur si ANS: D Medication should be withdrawn from an ampule using a filter needle, which prevents small glass fragments from being drawn into the syringe. DIF: Cognitive Level: Application REF: m 677 OBJ: Clinical Practice #3 TOP: Medication via Ampule KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse performs the proper technique when withdrawing medication from the vial by: • wiping the rubber stopper with a povidone-iodine swab. inserting the needle into the vial at a 90-degree angle. • injecting into the vial an amount of air that is equal to the dose. w • • keeping the needle above the level of solution while withdrawing into the syringe. ANS: C The vial should be wiped with an alcohol swab before use, the needle should be inserted at a slight lateral angle to avoid coring the rubber stopper, and an amount of air equal to the dose should be injected into the vial, while the needle is kept below the level of the solution to withdraw the dose. DIF: Cognitive Level: Application REF: m 679, Steps 35-5 OBJ: Clinical Practice #3 TOP: Withdrawing Medication from a Vial KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: pharmacological therapies • A patient has an order to receive two intramuscular injections in the same syringe. The nurse should initially: • determine if the two medications are compatible in the same syringe. obtain a larger syringe that will accommodate both medications. • select two syringes to give the medications separately. • ask the patient whether he would prefer one or two injections. ANS: A om • ng te st pr ep .c The first step is to determine whether the two medications are compatible in the same syringe. DIF: Cognitive Level: Analysis REF: m 679, Clinical Cues OBJ: Clinical Practice #5 TOP: Compatibility of Medications KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: pharmacological therapies • A patient has an order to receive a mixture of short- and longacting insulin. The first step to properly draw them up in the same syringe is to: • shake both vials vigorously before use. inject air into the short acting clear insulin. • withdraw the short acting clear insulin. si • inject air into the long acting cloudy insulin. ANS: D The vials should be rolled gently to mix the insulin suspension evenly, but they should not be shaken. Air is injected first into the long-acting cloudy insulin vial and then into the short-acting clear insulin vial. DIF: Cognitive Level: Analysis REF: m 680, Steps 35-4 OBJ: Clinical Practice #5 TOP: Combining Shortand Long-Acting Insulin KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: pharmacological therapies A nurse has opened and used part of a new multidose vial. The nurse should the • vial. • write the current date on w w w .m yn ur • • wipe the top of • check the expiration date of • replace the plastic top that rotate injection sites systematically. • use a tuberculin syringe to draw up insulin. ep • .c om covered ANS: A Before replacing a newly opened multidose vial in the medication storage area, the nurse should write the date the vial was opened, because out-of-date medication can chemically change. DIF: Cognitive Level: Application REF: m 679, Steps 35-3 OBJ: Clinical Practice #3 TOP: Multidose Vial Tips KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment • When reinforcing instructions to a patient who will selfadminister insulin injections at home, it is important to remind the patient to: • always use a new insulin vial with each dose. aspirate before injecting the insulin. ANS: B The patient should rotate injection sites systematically to promote absorption and to decrease tissue irritation. DIF: Cognitive Level: Application REF: m 684 OBJ: Clinical Practice #11 TOP: Self Administering Insulin KEY: Nursing Process Step: N/A MSC: NCLEX: Health Promotion and Maintenance yn The nurse has an order to administer an injection of purified protein derivative (PPD) by the intradermal route. The maximum amount of medication that can be given using this route is mL. 0.1 0.75 0.50 .m • ur si ng te st pr • w w w a. b. c. d. 0.2 ANS: A The maximum dose that can be given via the intradermal route is 0.1 mL. DIF: Cognitive Level: Knowledge REF: m 682, Skill 35-1 OBJ: Theory #7 TOP: Mantoux Test KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment • A nurse has administered a Mantoux skin test to a patient in the outpatient clinic at 9:00 AM on Monday. The patient should be scheduled to return to the clinic to have the result read: • late Monday afternoon. • late Tuesday afternoon. • any time on Wednesday. • w w w .m yn ur si ng te st pr ep .c om a n y t i m e o n F r i d a y . A N S : C The results of the Mantoux skin test should be read within 48 to 72 hours after injection. DIF: Cognitive Level: Comprehension REF: m 682, Skill 35-1 OBJ: Clinical Practice #8 TOP: Tuberculosis Testing KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: pharmacological therapies • A hospitalized patient has an order for subcutaneous heparin. The best location to administer this medication is the: • upper arm. • a b d o • anterior thigh. • buttock. ng te st pr ep .c om m e n . A N S : D The optimal site for heparin injection is the abdomen, because this area is not involved in muscular activity, as are the arms, buttocks, and legs. DIF: Cognitive Level: Knowledge REF: m 688, Box 35-3 OBJ: Clinical Practice #8 TOP: Heparin Subcutaneous Injection KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: pharmacological therapies • When administering an intramuscular injection to an adult patient using the ventrogluteal site, the nurse should use which landmark to locate the area for injection? • The lower end of the trochanter and the knee The upper end of the trochanter and the knee • The head of the trochanter and the posterior iliac spine si • The head of the trochanter and the anterior iliac spine ANS: D The head of the trochanter and the anterior iliac spine are the landmarks used to give an injection in the ventrogluteal site. The ventrogluteal site is the safest in regard to possible injury to the patients sciatic nerve. DIF: Cognitive Level: Comprehension REF: m 690, Skill 35-3 OBJ: Theory #10 TOP: Landmarks for Injection KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: reduction of risk • When administering an intramuscular injection for a 4-year-old child, the best site to use is the: • gluteus medius. w w w .m yn ur • • d • vastus lateralis. • ventrogluteal. om o r s o g l u t e a l . ng te st pr ep .c A NS :B The vastus lateralis is the best choice for children younger than 5 years old, because the gluteal muscle is not well developed. DIF: Cognitive Level: Comprehension REF: m 692 OBJ: Clinical Practice #7 TOP: Vastus Lateralis Site KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: reduction of risk • The most effective nursing actions to decrease discomfort to the patient during a parenteral injection would be: • inserting the needle while the skin is still wet from the alcohol wipe. asking the patient to look at the injection site for learning purposes. • using the smallest gauge needle that is appropriate for the site. ur si • removing the needle slowly to avoid damaging the tissue. ANS: C Using the smallest gauge needle that is appropriate for the site is one way to decrease patient discomfort. DIF: Cognitive Level: Comprehension REF: m 693, Box 35-4 OBJ: Clinical Practice #9 TOP: Parenteral Injection KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient has a medication order for iron dextran (Imferon) to be given using the Z-track technique. The rationale for using this method is to: • avoid medication irritation. w w w .m yn • • avoid tissue scarring. • cause less painful method. • w w w .m yn ur si ng te st pr ep .c om p r o t e c t t h e s c i a t i c n e r v e . A N S : A Z-track technique should be used with injection of this medication, because it creates a slanted needle track and avoids seepage of the medication back into subcutaneous or skin layers. DIF: Cognitive Level: Comprehension REF: m 694, Skill 35-5 OBJ: Theory #2 TOP: Z Track Technique KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • A patient asks why the clinic nurse asked him to remain in the clinic for 30 minutes after the injection of penicillin. The nurse explains that it is part of the standards of care to monitor for: • any pain reaction. • bleeding at the site. • infection at the site. • a n yn ur si ng te st pr ep .c om y a l l e r g i c r e a c t i o n . A N S : D The nurse should plan to monitor this patient for allergic response for 30 minutes after giving the first dose of a medication. DIF: Cognitive Level: Application REF: m 694, Safety Alert OBJ: Clinical Practice #6 TOP: Allergic Reaction to Parenteral Injection KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity • When preparing to reconstitute a drug from a powder form, the nurse should first: • use sterile water. vigorously shake the powder prior to reconstituting drug. • follow directions on label for diluent to use. w discard the vial and the unused medication. ANS: C Instructions for the diluent should be followed from the directions on the label. DIF: Cognitive Level: Application REF: m 678 OBJ: Clinical Practice #4 TOP: Reconstitution KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies • Which medication order should be documented in the MAR and in the nurses notes after it is given? • Digoxin 0.25 mg PO at 9:00 AM w w • .m • • Demerol 75 mg IM PRN pain • Lasix 40 mg PO twice daily • .m yn ur si ng te st pr ep .c om K C l 2 0 m E q P O d a i l y A N S : B PRN and STAT orders are recorded in both the MAR and nurses notes along with the reason why the medication was given, the result, and the duration of effect of medication. DIF: Cognitive Level: Application REF: m 695 OBJ: Clinical Practice #11 TOP: Documentation KEY: Nursing Process Step: N/A MSC: NCLEX: N/A w w w • A nurse giving a subcutaneous injection will select a: • 3-mL syringe and 22-gauge, 1-inch needle. • 3-mL syringe and 18-gauge, 1-inch needle. • • 3-mL syringe and 25-gauge, 5/8-inch needle. 3-mL syringe and experience a faster response to the medication. • use a 15-degree angle to inject the medication. need extra pressure at the injection site to prevent bleeding. ANS: A For the obese patient, the needle length should be longer than the needle length for a thin person because of excess fatty layers. DIF: Cognitive Level: Application REF: m 674, Clinical Cues OBJ: Clinical Practice #1 TOP: Subcutaneous Injection KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse may refuse to carry out an order for a placebo if the: • medication is labeled as a placebo. ur si ng te st pr ep • .c • om 20-gauge, 1-inch needle. ANS: C For subcutaneous injection, it is best to use a 25-gauge, 5/8-inch needle. DIF: Cognitive Level: Application REF: m 672 OBJ: Clinical Practice #1 TOP: Needle and Syringe Size KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse is teaching a patient who weighs 325 pounds on how to administer a subcutaneous would suggest that the patient would: • require a longer needle because of his weight. nurse has religious grounds for refusing. • placebo is to be delivered by a parenteral route. yn • patient is unaware that the medication is a placebo. ANS: D The nurse is ethically obligated to refuse to give a placebo if the patient has not been informed that the medication is a placebo. DIF: Cognitive Level: Comprehension REF: m 672, Legal/Ethical OBJ: Theory #1 TOP: Placebo KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: pharmacological therapies • When administering heparin, the nurse will avoid: • using the lower abdomen as an injection site. w w w .m • • rotating sites. • massaging area for more than 3 seconds. • a om .c ep pr st te ng si ur yn s p i r a t i n g a f t e r i n j e c t i o n . A N S : D w w w .m After the insertion of heparin, the nurse should not aspirate because this practice tends to increase bruising. DIF: Cognitive Level: Application REF: m 688, Box 35-5 OBJ: Theory #1 TOP: Heparin Injection KEY: Nursing Process Step: Application MSC: NCLEX: Physiological Integrity: pharmacological therapies COMPLETION • The IM injection site recommended for infants under 12 months of . ANS: age is the vastus lateralis The vastus lateralis muscle is the site of choice for infants under 12 months for IM injections. DIF: Cognitive Level: Knowledge REF: m 692 OBJ: Theory #2 TOP: Medication Administration KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • use only a 23-gauge needle to inject a reconstituted drug. • thoroughly mix solute with diluent. • roll the solute between hands to warm powder. pr ep .c • om A drug that has no actual pharmacologic effect is called a(n) . ANS: placebo A drug that has not pharmacologic effect is called a placebo. The use of the fake drugs is unethical if the patient is unaware that placebos are being used. DIF: Cognitive Level: Knowledge REF: m 672 OBJ: Theory #1 TOP: Placebo KEY: Nursing Process Step: N/A MSC: NCLEX: N/ A MULTIPLE RESPONSE • When reconstituting a drug from a powder, the nurse will: (Select all that apply.) • confirm the type of diluent required. label the drug as to the amount of medication per volume after dilution. ANS: A, C, E After confirming the type of diluent required, the solute must be mixed thoroughly with the recommended diluent, then labeled as to the amount of medication per volume after dilution. DIF: Cognitive Level: Application REF: m 678 OBJ: Clinical Practice #4 TOP: Mixing Drug from Powder KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies OTHER • You are preparing to mix short-acting and long-acting insulin. Prioritize these steps accordingly. (Separate letters with a comma and space as follows: A, B, C, D, E, F.) • Withdraw prescribed amount of short-acting insulin. • Inject air into short-acting insulin. • Check medications with MAR using three medication checks. • Choose and prepare site before injection. • Withdraw prescribed amount of long-acting insulin. • Inject air into longacting insuli n. ANS: w w w .m yn ur si ng te st • C, F, B, A, E, D These are the proper steps to take when mixing short- and long-acting insulin in one syringe. • hypotonic. • hypertonic. om Chapter 35 Intravenous Medications MULTIPLE CHOICE • The nurse anticipates that the malnourished post-operative 70-year-old patient will receive an intravenous (IV) infusion of 5% dextrose in 0.45% saline. because it is: • isotonic. ep .c • w w w .m yn ur si ng te st pr t o t a l p a r e n t e r a l n u t r i t i o n . A N S : C 5% Dextrose in 0.45% saline is a hypertonic or high molecular solution and is a frequent choice • controlled-volume om primary infusion ep • .c for post-operative maintenance fluid. DIF: Cognitive Level: Knowledge REF: m 701, Table 36-1 OBJ: Theory #1 TOP: Types of Intravenous Solutions KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: physiological adaptation • The nurse is planning for the initiation of a blood transfusion. The type of tubing the nurse will prepare is a set. • piggyback • w w w .m yn ur si ng te st pr Y a d m i n i s t r a t i o n A N S : D A Y administration set is used to place the blood on one side and normal saline on the other. This is necessary so that the blood can be discontinued but the vein can remain open with the saline in the case of a transfusion reaction or other medically necessary situation. DIF: Cognitive Level: Application REF: m 728, Skill 36-6 OBJ: Clinical Practice #7 TOP: Administration Sets KEY: Nursing Process Step: N/A om .c MSC: NCLEX: Physiological Integrity: reduction of risk potential • The nurse is aware that as a safety precaution against overhydration, the tubing drip factor set appropriate for a 6-month-old infant is gtt/mL. a. 60 b. 20 c. 15 d. 10 ANS: A A microdrip infusion set, which delivers 60 gtt/mL, is used for infants and children. DIF: Cognitive Level: Comprehension REF: m 702 OBJ: Theory #3 st pr ep TOP: Tubing Size KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The nurse evaluating a piggyback IV setup finds an error in the construction of the fluids. Which situation would the nurse correct? • Secondary bag is hung higher than the primary bag. Primary line clamp is closed. • Slide clamp near the insertion site is open. ng te • w w ur yn w .m S e c o n d a r y l i n e c l a m p i s o si • ng te st pr ep .c om p e n . A N S : B When a medication is given via piggyback setup, the secondary bag is hung slightly higher than the primary line and, when the secondary infusion finishes, the primary one takes over again; therefore all clamps (roller and slide) must be open for the setup to work properly. DIF: Cognitive Level: Application REF: m 702 OBJ: Clinical Practice #1B TOP: Secondary or Piggyback Intravenous Set KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: physical care and comfort • The nurse assisting in the initiation of a blood transfusion is aware that the only appropriate solution to infuse through a parallel infusion set before and after the transfusion is: • 5% dextrose in water. 10% dextrose in water. • lactated Ringers solution. ur si • .m w w w n o r m a l s a l i n e . A N S : yn • • intermittent infusion device. .c secondary IV line. ep • om D Normal saline is the only solution used in conjunction with infusion of a blood product. DIF: Cognitive Level: Comprehension REF: m 702 OBJ: Clinical Practice #7 TOP: Blood Infusion KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: reduction of risk potential • To facilitate the administration of an IV antibiotic every 6 hours to a patient who is ambulatory, well hydrated, and on a regular diet, the nurse would insert a(n): • primary IV line. • w w w .m yn ur si ng te st pr c e n t r a l v e n o u s l i n e . A N S : C Patients who do not require large amounts of fluid but receive intermittent IV medications benefit from an intermittent infusion device. DIF: Cognitive Level: Application REF: m 703 OBJ: Theory #1 TOP: Saline or PRN Lock KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: pharmacological therapies • A patient is receiving IV fluids through an infusion pump. How often should the nurse check the functioning of the pump? • Every 15 to 30 minutes • Every 1 to 2 hours • Every 2 to 4 hours om • w w w .m yn ur si ng te st pr ep .c O n c e d u r i n g t h e s h i f t A N S : B An IV infusion pump should be checked every 1 to 2 hours to ensure that it is functioning properly. DIF: Cognitive Level: Comprehension REF: m 703, Box 36-1 OBJ: Clinical Practice #1A TOP: Infusion Pumps KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: safety and infection control • When a patient receiving IV medication exhibits light-headedness, tightness in the chest, flushed face, and irregular pulse, the nurse suspects: • speed shock. • drug allergy. • fluid overload. • ep .c om a i r e m b o l u s . w w w .m yn ur si ng te st pr A N S: A Light-headedness, tightness in the chest, flushed face, and irregular pulse are all signs of speed shock. Speed shock is when a foreign substance is infused into the body rapidly. The infusion should be stopped, the physician notified, and the patient monitored. DIF: Cognitive Level: Analysis REF: m 709, Table 36-2 OBJ: Theory #3 TOP: Intravenous Catheters KEY: Nursing Process Step: Intervention MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A patient is admitted with a peripherally inserted central catheter (PICC). As part of standard care for this patient, the nurse should: • obtain the patients temperature every 2 hours. • prepare to infuse fluids at high volumes. • avoid taking blood pressures on the arm with the PICC line. • have the catheter withdrawn while the patient is hospitalized. ANS: C PICC lines are inserted by physicians or specially trained nurses, and they are used for long-term therapy; blood pressures are not taken in the arm that has the PICC line to avoid interfering with the function or the life of the catheter. Many times this catheter is used in home care. DIF: Cognitive Level: Application REF: m 706, Clinical Cues OBJ: Theory #3 TOP: PICC KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk potential • A patient has just undergone placement of a central venous catheter through the subclavian vein. When the placement is complete, the nurse should: • hang the prescribed fluid at a rate of 1 mL/min. assess the quality of the breath sounds. • note the length of the tubing. om • wait for the results of the chest radiograph before beginning fluids. ANS: D Correct placement of subclavian catheters must be verified by radiographic studies before any fluid is infused through them. DIF: Cognitive Level: Application REF: m 707 OBJ: Theory #3 TOP: Central Venous Catheter Placement KEY: Nursing Process Step: Intervention MSC: NCLEX: Physiological Integrity: reduction of risk potential • The nurse observes that the insertion site of an IV catheter looks pale and puffy and the area feels cool to the touch. The initial action for the nurse should be to: • discontinue the infusion and start a new IV site. apply warm compresses to the site. • monitor the patients temperature every 4 hours. • ur • yn si ng te st pr ep .c • w w w .m call the physician and report these findings. ANS: A Infiltration is the most common complication of IV therapy, and it occurs when fluid or medication leaks out of the vein and into the tissue. The infusion should be discontinued immediately and a new insertion site initiated. Signs are pale, cool skin that is edematous (puffy). DIF: Cognitive Level: Application REF: m 709, Table 36-2 OBJ: Theory #3 TOP: Infiltration of Intravenous Fluids KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient rings the call bell and states that the IV insertion site is painful. The site is reddened, warm, and swollen. The nurse assesses that the patient is most likely experiencing: • bloodstream infection. • catheter embolus. • infiltration of the line. • phlebitis. right side and lower • left side and raise si ng • w w w .m yn ur • l e f t s i d e a n d l o w e r A N S te st pr ep .c om ANS: D Phlebitis is caused by irritation of the vessel by the needle, cannula, medications, or additives to IV solution. Typical signs are erythema, warmth, swelling, and tenderness. DIF: Cognitive Level: Comprehension REF: m 709, Table 36-2 OBJ: Theory #3 TOP: Phlebitis KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient receiving TPN fluid therapy experiences an air embolus in the central line. The nurse should the head immediately turn the patient onto the of the bed. • right side and raise 2 to 4 • 6 to 8 pr • ep .c om : D To anatomically minimize the risk of the air embolus reaching the lungs, the nurse should turn the patient onto the left side and lower the head of the bed. The physician is notified immediately. DIF: Cognitive Level: Application REF: m 709, Table 36-2 OBJ: Theory #3 TOP: Catheter Bolus KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk potential • The nurse takes into consideration that according to The Joint Commission, the first IV antibiotics order for a community-acquired pneumonia must be administered within hours. • 1 to 2 w .m yn ur si ng te st d. 24 ANS: C The Joint Commission suggests that the first IV antibiotic administered for community-acquired pneumonia be administered in the first 6 to 8 hours after admission. DIF: Cognitive Level: Comprehension REF: m 726, Clinical Cues OBJ: Theory #4 TOP: IV Antibiotics KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: pharmacological therapies • A nurse is monitoring the status of an elderly patient who is receiving IV therapy. Indicator of fluid volume overload is suspected when the nurse assesses: • crackles in the lung fields. w • w • • s l i g h t e d pulse rate of 64 beats/min, irregular. respirations of 16 breaths/min, regular. .m yn ur si ng te st pr ep .c om e m a t o t h e f e e t . A N S : A Fluid overload is signaled by crackles in the lung fields, increasing pulse rate, and shortness of breath. DIF: Cognitive Level: Analysis REF: m 709, Table 36-2 OBJ: Theory #5 TOP: Elder Care: IV Therapy KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: prevention and early detection of disease • A patient has an order for an infusion of 5% dextrose in 0.45% sodium chloride at a rate of 100 mL/hr IV. The IV tubing has a drop factor of 15 gtt/mL. At how many drops per minute should the nurse regulate the infusion? a. 15 w c. 25 w b. 17 w d. 33 ANS: C The formula for calculating IV flow rates is as follows: (Amount of solution in mL number of drops/min) / Time in minutes; (100 15) / 60 = 1500 / 60 = 150 / 6 = 25 drops/min. DIF: Cognitive Level: Analysis REF: m 710, Box 36-2 OBJ: Clinical Practice #3 TOP: IV Calculations KEY: Nursing Process Step: N/A MSC: NCLEX: N/A A nurse accessing the injection port of the IV tubing will scrub the hub for • seconds. • Left upper forearm te Right hand ng • st pr ep .c om a. 5 b. 10 c. 15 d. 30 ANS: C The hub of the injection port on a piggyback setup should be scrubbed for 15 seconds. DIF: Cognitive Level: Application REF: m 721, Skill 36-3 OBJ: Clinical Practice #1E TOP: IV Guidelines KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • A patient is to have an IV insertion site changed. The current line is in the lower right forearm. Which location is contraindicated for the new site? • Right upper forearm • w w w .m yn ur si L e f t h a n d A N S : B A new IV site should not be placed distal to an old site; the right hand is distal to the right forearm, so it should not be used. DIF: Cognitive Level: Analysis REF: m 710 OBJ: Clinical Practice #4 TOP: Changing IV Site KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: reduction of risk potential • The nurse would plan to get another nurse to try to obtain a successful venipuncture if the first nurse was attempt(s). not successful in • five • three • two • one .c om ANS: C If the nurse cannot initiate a patent IV in two attempts, it is good judgment to ask another nurse to perform the task. DIF: Cognitive Level: Application REF: m 715, Skill 36-1 OBJ: Clinical Practice #4 TOP: Starting an IV w w w .m yn ur si ng te st pr ep KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • A nurse is aware that for a patient with a continuous IV infusion running, the IV bag should be changed when only mL of solution remains in the bag. a. 10 b. 25 c. 50 d. 100 ANS: C When the container has only 50 mL of solution left, the next ordered solution is added to the setup and the flow begun to prevent air from entering the line. DIF: Cognitive Level: Comprehension REF: m 716 OBJ: Clinical Practice #5 TOP: Maintaining an IV KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: pharmacological therapies • A patient who requires an immediate transfusion of blood has previously signed a consent form to receive it. The nurse confirms that the consent was signed within hours. the last a. 8 b. 12 c. 24 d. 48 to 72 ANS: D A consent to receive blood must be signed by the patient, usually no more than 48 to 72 hours before receiving the blood product. DIF: Cognitive Level: Knowledge REF: m 727 OBJ: Clinical Practice #7 TOP: Blood Transfusion Consent Form KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies • A patient complains of chills, back pain, and shortness of breath a few minutes after the blood infusion is started. The first thing the nurse should do is: • slow down the blood infusion. • stop the blood infusion and start the saline. • monitor vital signs and call the physician. start lowflow oxygen as per facility protocol. ANS: B If a transfusion reaction occurs, such as chills, back pain, and shortness of breath or itching, the nurse should stop the infusion and start the saline to keep the line open. DIF: Cognitive Level: Application REF: m 729, Skill 36-6 OBJ: Theory #6 TOP: Blood Transfusion Reaction KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: safety and infection control • The LVN/LPN is told by the RN to discontinue an IV line to the patient. The best nursing action is to: si ng te st pr ep .c om • check the physicians order. • stop the IV flow by clamping the tubing securely. • wash hands and don gloves. yn quickly withdraw the cannula and apply pressure. ANS: A Checking the physicians order will prevent inadvertently discontinuing the IV and having to restart it. DIF: Cognitive Level: Application REF: m 727, Steps 36-4 OBJ: Clinical Practice #6 TOP: Discontinuing an IV KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse caring for a patient with an intermittent IV device should: • attach continuous fluid infusion to the device. w w w .m • ur • • infuse saline or heparin solution to maintain patency. • discontinue when the IV medication is finished. reduce patient activity to prevent dislodgement. ANS: B The intermittent IV device should be flushed periodically with saline or heparin, depending of facility policy, to maintain patency, which allows more freedom of movement for the patient. DIF: Cognitive Level: Application REF: m 723 OBJ: Clinical Practice #1D TOP: Medication to Intermittent Intravenous Device KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies COMPLETION • A patient has an IV of 1000 mL 5% dextrose in -normal saline (0.45% sodium chloride) infusing via microdrip for 12 hours. The IV is infusing gtt/min. ANS: 83 1000 / 12 = 83. DIF: Cognitive Level: Analysis REF: m 710, Box 36-2 OBJ: Clinical Practice #2 TOP: Intravenous Medication Administration KEY: Nursing Process Step: Intervention MSC: NCLEX: Physiological Integrity: pharmacological therapies • The nurse instills diluted medication in the portion of the . controlled volume IV setup, which is called the ANS: burette The burette is the tube-like chamber that holds only about 150 mL of fluid with diluted medication. DIF: Cognitive Level: Knowledge REF: m 724 OBJ: Theory #1 TOP: Burette KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk potential w w w .m yn ur si ng te st pr ep .c om • • After the blood infusion has started, the nurse should let minutes. the blood flow at 2 mL/min for the first ANS: 15 fifteen The initial rate of blood infusion is 2 mL/min for the first 15 minutes. If the patient tolerates this rate, it can be gradually increased. DIF: Cognitive Level: Comprehension Monitor weight daily. • Flush with heparin solution intermittently. • Monitor lung sounds every 4 hours. • Monitor IV site for infiltration. w w w .m yn ur si ng ep te st pr • M o n i t o r b l o o d s u g a r l e v e l s . A N S : A .c • om REF: m 729, Skill 36-6 OBJ: Clinical Practice #7 TOP: Monitoring Blood KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: reduction of risk potential MULTIPLE RESPONSE • The physician orders an IV of 5% dextrose in normal saline (0.45% sodium chloride) to infuse over a 10-hour period. Which of the following actions should the nurse take? (Select all that apply.) • Monitor intake and output (I&O) every shift. ep .c om , D , E To monitor fluid overload, it is important to assess lung sounds and I&O. Monitoring the IV site for infiltration or phlebitis is also critical. DIF: Cognitive Level: Application REF: m 711, Box 36-3 OBJ: Theory #3 TOP: IV Nursing Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity • The nurse is aware that the disadvantages of infusion pumps include: (Select all that apply.) • a saline lock is required. infusion pump change-out every shift. • the initial expense of machines. • an alarm that can be deactivated by family. te st pr • the need for special admini stration sets. ANS: C, D, E Infusion pumps have some disadvantages such as their initial expense, the need for special administration sets, and the fact that the alarm button sounds when the IV container is empty, when there is air in the line, and when there is an occlusion. DIF: Cognitive Level: Comprehension REF: m 704 OBJ: Theory #3 TOP: Topic: Infusion Pumps KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: reduction of risk w w w .m yn ur si ng • • Signs that would cause the nurse to discontinue a blood transfusion would include: (Select all that apply.) • hives. • facial flushing. • nosebleed. • back pain. • w w w .m yn ur si ng te st pr ep .c om b l o o d y c o l o r e d u r i n e . A N S : A , B , D Symptoms such as hives, facial flushing, back pain, itching, chills, apprehension, and fever are the most common reactions. Many times the physician will order Benadryl for the itching or hives and allow the blood to run. DIF: Cognitive Level: Comprehension REF: m 727 OBJ: Theory #6 TOP: Blood Reaction KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: reduction of risk OTHER • Place the steps in order for the preparation to initiate a blood line: (Separate letters by a comma and space as follows: A, B, C, D, E.) • Compare patient name, ID number on wrist bank with transfusion record. • Obtain Y-connector setup and saline and prime the filter with saline. Clamp off saline and start blood. Confirm the presence of a permission slip. w w w .m yn ur si ng te st pr ep .c O b t a i n b a s e l i n e v i t a l s i g n s . A N S : D, A, B, E, C All permission slips and then identification must be accomplished prior to starting blood. The blood information is checked with two licensed persons. The filter is primed and the saline is started; vital signs are taken and then the blood is started. om • • • Chapter 36 Airway Management A patient in the ICU is producing an increased amount of sputum and has a fever. The nurse suspect Which of the following characteristics of the patients sputum would indicate a bacterial infection, as • infection? Select all that apply. Yellow • Clear • Blood-streaked • Green • Brown • White ep .c om • pr An older patient in the ICU has labored breathing and a history of smoking. The nurse suspects that has chronic obstructive pulmonary disease (COPD). Which of the following signs would tend to con hat the patient has COPD? Select all that apply. te st • Increased anterior-posterior diameter of the chest • The patient lying propped onto one side • Deviation of the trachea from the midline • Inspiration taking just as long as expiration .m yn ur si ng • SaO2 w • Which test would be best for measuring the oxygenation of this patients blood? w • w A patient in the ICU with a history of smoking is having tests performed to assess his respiratory fu • Pulse oximetry • End-tidal carbon dioxide • pH A patient has arterial blood gas testing performed. Her PaO2 is 95 mm Hg, SaO2 is 90%, pH is 7.4, • HCO3 is 23 mEq/L. Which of these values should the nurse be most concerned about? PaO2 • HCO3 • pH • SaO2 .c om • ep A patient in her first trimester is in the ICU and is displaying signs of metabolic alkalosis. On speak with the patient, the nurse learns that she has been experiencing much vomiting, diarrhea, and anxie st pr • • Diarrhea • Vomiting • Anxiety ng Pregnancy .m yn ur si • te in the past week. The nurse should recognize that which of the following is the most likely cause of this acid-base imbalance? w w A patient has arterial blood gas testing performed. His PaO2 is 83 mm Hg, SaO2 is 91%, pH is 7.5, w • PaCO2 is 24 mm Hg, and HCO3 is 22 mEq/L. Which of the following indicates this patients conditi • Respiratory acidosis with normal saturation (uncompensated) • Metabolic alkalosis with low saturation (uncompensated) • Respiratory alkalosis with low saturation (uncompensated) • Metabolic alkalosis with low saturation (fully compensated) Respiratory alkalosis, fully compensated • Respiratory acidosis, partially compensated • Metabolic alkalosis, fully compensated • Metabolic acidosis, partially compensated .c • om • A patient in the ICU has just undergone arterial blood gas testing. Her results are as follows: PaO2 i 90 mm Hg, pH is 7.43, PaCO2 is 24, and HCO3 is 19 mEq/L. Which of the following indicates this patients condition? pr ep A patient in the ICU with pneumonia and on mechanical ventilation is suspected to have pulmonary Chest radiography • Ventilation-perfusion scanning • Pulmonary angiography • Bronchoscopy yn ur si • te st embolus. Which diagnostic study would be best for assessing for this condition? ng • .m A patient in the ICU is suspected of having tuberculosis. The nurse understands that which diagnost • w Sputum culture w • test will most likely be performed on this patient to confirm this suspicion? w • Thoracentesis • Ventilation-perfusion scanning • Pulmonary angiography The nurse is completing a history on a patient with dyspnea. What characteristic of dyspnea is • most indicative of pulmonary disease? Most severe when patient is supine • Awakens patient from sleep at night • Accompanied by anginal chest pain • Most severe with exertion om • Lobular pneumonia • Chronic obstructive pulmonary disease • Acute respiratory distress syndrome • Respiratory syncytial virus ur si ng te • st • pr ep .c During the inspection phase of the physical examination, the nurse notices that the patients chest wall is round, and the anterior-to-posterior diameter and the lateral diameter are equal. Based on this information, what disease process does the nurse suspect? yn The nurse is caring for a patient who has undergone thoracic surgery. What assessment information would best support the nurses suspicion of pulmonary consolidation? .m • Vesicular lung sounds at bases • Bronchial breath sounds over upper airway • w w • w • Egophony at left posterior base of lung Basal crackles that clear with cough A patient is being monitored with continuous pulse oximetry. Under what circumstance would • the nurse question the accuracy of the pulse oximetry reading? • The patient is a victim of a fire in an enclosed space. • Cardiac monitor pattern shows normal sinus rhythm. • Extremities are warm and dry with intact pulses. • Respiratory rate and pulse rate are elevated. • Respiratory acidosis • Respiratory alkalosis ep Metabolic alkalosis pr • st Metabolic acidosis ng • .c What acidbase abnormality should the nurse assess for? te • om The patient is being monitored with an end-tidal CO2 monitor and has values trending upward. • yn ur si The patient has experienced a significant drop in hemoglobin levels and is slightly tachycardic. The pulse oximetry value is 100% and arterial blood gas values are normal. What is the most important adverse physiologic effect that the nurse would expect? Polycythemia • Diminished blood pressure • Hyperalertness and hyperreflexia w w w • .m • Diminished tissue oxygenation • The nurse is evaluating the following arterial blood gas values: pH 7.35, PaO2 95 mm Hg, SaO295 Hg, and HCO3 24 mEq/L. How does the nurse interpret these results? • Normal • Respiratory acidosis • Metabolic acidosis • Technical error The patient is experiencing respiratory acidosis. What nursing action is most likely to alleviate this Suction the endotracheal tube. • Reduce the respiratory rate on the ventilator. • Administer intravenous bicarbonate. • Increase the rate of crystalloid intravenous fluids. .c om • pr ep • st A patient has experienced a cardiopulmonary arrest and is receiving cardiopulmonary resuscitation evaluates the effectiveness of this therapy, what value on arterial blood gases is most indicative of Diminished SaO2 • Elevated HCO3 • Elevated PaCO2 si • ur Diminished PaO2 w .m yn • ng te • w A critically ill patient has arterial blood gas results of pH 7.6, PaCO2 40 mm Hg, and HCO3 30 m medical situation do these results most clearly correlate? w • • Excess nasogastric drainage • Severe diarrhea • Diabetic ketoacidosis • Lobular pneumonia • Metabolic acidosis • Metabolic alkalosis • Respiratory acidosis • Respiratory alkalosis .c • om A patient has arterial blood gas results of pH 7.2, PaCO2 55 mm Hg, and HCO3 24 mEq/L. How d interpret these results? • pr ep A critically ill patient has arterial blood gas results of PaO2 60 mm Hg, SaO2 80%, pH 7.35, PaCO HCO3 24 mEq/L. How does the nurse interpret these results? Hypoxemia and respiratory acidosis • Hypoxemia and normal acidbase balance • Normal oxygenation and metabolic acidosis • Normal oxygenation and acidbase balance ur si ng te st • yn A critically ill patient has arterial blood gas results of pH 7.35, PaCO2 55 mm Hg, and HCO3 28 the nurse interpret these results? .m • Respiratory acidosis • Metabolic alkalosis • w w • w • Partially compensated metabolic alkalosis Fully compensated respiratory acidosis • A patient who is critically ill is attached to a saturation of mixed venous oxygen monitor (SvO2) a SvO2 value that is trending downward and is currently below normal at 55%. What clinical abnor nurse suspect? • Increased cardiac output • Fever and shivering • Fluid volume overload • Oversedation • .c om The nurse is evaluating the chest radiograph of a critically ill patient and notices that the patients tr the left of midline. What additional finding would confirm the presence of a pneumothorax? Absent or diminished breath sounds on the right • Lung fields generally white on chest radiograph • Lung fields dull to percussion on the right • Blunting of costophrenic angles on chest radiograph ng te st pr ep • A, B • A • D • C ur • yn A, D, E w w w .m • si Answer Key • C • A • C • A A • A • D • A • C • B • D • B • A om • .c D ep • pr C st • te A ng • si C ur • yn B .m • w D w w • Chapter 37 Resuscitation • A patient sustained injuries in a motor vehicle accident and is in the Emergency Department. A CT scan of the head and neck have been ordered. What part of the survey is this? • Primary • Secondary • Tertiary Initial Start lactated Ringers at 150 mL/hr. • Start dopamine at 5 mcg/kg/min. • Start an albumin infusion wide open. • Start a unit of uncrossmatched blood. om • .c • A patient who is in the Emergency Department was attacked in a parking lot and suffered several stab wounds to various areas on the chest and abdomen; BP 100/60, heart rate 108, respiratory rate 20, pulse oximetry 98%. In order to counteract the blood loss and restore circulating volume for this patient, what priority intervention will the nurse perform? ep • te • st pr The nurse is assigned to a patient in the Emergency Department who exhibits paradoxical chest movement. What intervention by the nurse can help improve oxygenation in this patient? Elevate the head of the bed 30 degrees. • Splint the chest with 3-inch surgical tape. • Turn the patient with the injured side down. • Place the patient in the prone position. ur si ng • w • .m yn A patient has been involved in a motor vehicle accident. The patient, who was driving, was unrestrained by a seat belt when hitting the car in front of him. The patient is complaining of midsternal pain, restlessness, and difficulty breathing. What is the priority nursing diagnosis for this patient? Anxiety • Impaired gas exchange • w • w • Impaired circulation Pain • A patient has suffered a mild pulmonary contusion from a jet ski accident. What nursing interventions are appropriate for this patient? Select all that apply. • Maintenance of chest tubes • Frequent pulse oximetry monitoring • Assessment of lung sounds every 2 hours • Continuous epidural analgesia Maintainance of ventilatory support • A patient sustained an injury to the right arm after falling off a motorcycle. The patient is complaining of severe pain and is unable to feel the fingers of the right hand. Radial pulse is absent. What is the priority intervention by the nurse? • Elevate the right arm above the level of the heart. • Notify the physician. • Apply ice packs to the affected area. • Place the patient in Trendelenburg position. Pulmonary edema • Cardiac tamponade • Pulmonary embolus • Tension pneumothorax te si The nurse is assigned to care for a patient who was admitted 2 days previous after a four-wheeler accident. The patient sustained a closed fracture to the left ur • st • ng • pr ep .c The nurse is caring for a patient with deep vein thrombosis of the left lower extremity. The patient exhibits a decrease in pulse oximetry readings from 98% to 86%, shortness of breath with a respiratory rate of 34, and is now disoriented to place. The nurse recognizes that these findings are caused by what complication? om • .m yn femur and had an open reduction with internal fixation the same day. What is a priority for the nurse to assess for this patient? White blood count • Urinary output • Cardiac output w w • w • Pulse oximetry A patient has been brought into the Emergency Department via ambulance with resuscitation efforts being performed. It is unlikely that the patient will survive the severe injuries sustained. Two adult children of the patient are present and are requesting to be with the patient at 9. A) B) C) D) om 10. I dont think you should see your loved one like this. Wouldnt you rather remember him the way he was? pr ep Our hospital doesnt allow more than one family member in with a patient. One of you can come in and one of you will have to wait in the waiting area. .c this time. What is the best response by the nurse? st You may come in with your parent and I will have someone stay with you to explain what is happening. ng te I have been through this many times and I promise you, it is a sight that you dont want to remember. si The nurse is caring for the patient with chest tubes. Which observation by the nurse is a priority concern? 250 mL/hr of blood in drainage collection system • Pulse oximetry of 94% • Blood pressure of 104/62 • 30 mL/hr of urine output • A patient is admitted to the emergency department after he was hit by a car. The car was going about 30 mph and was braking at the time of impact. The patient was struck just above the right knee, fell forward over the hood of the car, striking his anterior chest, and then slipped off the hood of the car and hit the pavement head first. Based on the mechanism of injury and transfer of force, what injuries does the nurse most expect? Select all that apply. • Fracture of left femur and damage to left knee • Fractures of thoracic and lumbar spine • Fractured ribs and cardiac and lung contusion w w w .m yn ur • Bilateral radial and humerus fractures • Closed head injury and cervical spine fracture • Bilateral clavicle and scapular fractures • The patient has received a gunshot wound. To help predict the amount of damage, what information does the nurse collect? • Location of the shooting • Information about the shooter • Type of weapon and caliber of bullet • Whether the injury involved a felony • A patient was in a serious motor vehicle crash. At the scene, what is the highest priority of care? • Extrication from the vehicle • Cervical spine protection • Establishing two large-bore intravenous lines • Collecting information about the crash te st pr ep .c om • yn ur si ng On initial admission of a trauma victim to the emergency department, the nurse completes a primary survey. The patient is awake and tachypneic, is using accessory muscles of respiration, has unequal chest expansion, and is very anxious. There are absent breath sounds on the right and cyanosis on 100% oxygen, and the trachea is deviated to the left. What action takes the highest priority during the primary survey? • Jaw thrust maneuver • Suctioning the oral pharynx • Chest tube insertion w w w • .m • Assisting ventilation with bag-mask device A patient has been admitted to the emergency department after being in a severe motor vehicle crash. The patient was a passenger and had a lap and seat belt in place. The patient is lethargic and moaning. Initial exposure and head-to-toe examination reveals scattered minor abrasions and contusions and bruising over the upper abdomen. The patient moans more when the • Administer intravenous opioid for pain. • Increase rate of intravenous crystalloid. • Obtain CT of the abdomen. • Prepare for immediate endotracheal intubation. • As part of a major trauma, a patient has suffered a flail chest injury. What hallmark sign of flail chest does the nurse expect to find? • Flail segment elevation during inhalation • Evidence of rib fractures on chest radiograph • Flail segment depression during inhalation • Hypoxemia evident on arterial blood gases • A patient is admitted to the CCU after experiencing blunt trauma to the chest. Among other injuries, the patient has a flail chest on the left and several extremity fractures. About 12 hours after admission, the patient is tachyp neic and compl aining of shortn ess of breath. Breath sounds are present bilaterally with scattered fine crackles . Chest radiograph shows an ill-defined, patchy, ground-glass area of density on the left. If the patient has a pulmonary contusion, what is the nursing priority? w • w w .m yn ur si ng te st pr ep .c om • abdomen is palpated, and the abdomen is rigid. Heart rate is 110, capillary refill is greater than 4 seconds, and blood pressure is 140/88 mm Hg. What is the nursing priority of care? Monitor pulse oximetry and arterial blood gases closely. • Place an oral endotracheal tube immediately. • Increase the amounts of intravenous crystalloid administration. • Obtain sputum culture and sensitivity and Gram stain. A patient has suffered severe blunt trauma to the abdomen with bruising, diffuse pain, guarding, and rigidity evident. Damage to which structure is most likely? • Stomach • Bladder • Large intestine • Liver • As part of a multiple trauma injury, the patient has suffered a closed fracture of the radius. What nursing assessment finding indicates a significant complication warranting immediate treatment? • Swelling and pain over the fracture • Loss of pulses distal to the fracture • Ecchymosis over the fracture • Deformity of forearm • A patient has experienced multiple fractures, including pelvic and long bone fractures. After 72 hours, the patient complains of tachypnea and dyspnea and is found to have cyanosis, tachycardia, confusion, and fever. Laboratory analysis reveals a ng te st pr ep .c om • ur si normal complete blood count except for thrombocytopenia and progressive respiratory insufficiency. What is the nursing care priority? Administer oxygen and monitor pulse oximetry. • Initiate low-molecular-weight heparin therapy. • Obtain cultures of all body substances. • Initiate fall and seizure precautions. • During a motor vehicle accident, a patient sustained blunt trauma to the head and face, resulting in hairline skull fracture and a LeFort III maxillofacial l fracture. The patient also has bruising across the chest and upper abdomen and multiple small superficial bleeding abrasions and lacerations. On admission to the emergency department, what is the nursing care priority? • Apply direct pressure to bleeding areas. • Assess neurologic status. • Perform endotracheal intubation. • Administer tetanus booster immunization. w w w .m yn • As part of a multiple trauma injury, a patient • Significantly greater chance of death • No change in outcome expectations • Outcome depends on treatment. om • developed hemorrhagic hypovolemic shock, necessitating fluid resuscitation with massive amounts of intravenous crystalloid fluids and blood products as well as extensive surgical repair under general anesthesia. Twenty-four hours later, the patient develops hypoxia unresponsive to oxygen therapy and diffuse white, ground-glass infiltrates of the lung fields on a chest radiograph. Development of this complication has what effect on the patients recovery? B • C • D • C • A • A, C, E • C w B w • w • C • B • C • A • D • B • A • C • A ep • pr B, C, D st • te B ng • si C ur • yn A .m • .c • Lower chance of death Answer Key • B Chapter 38 End-of-Life Care You have heard some very bad news today. Can you describe what you mean by burden? .c • om MULTIPLE CHOICE • A 33-year-old patient has been told that her disease is terminal. The patient is crying and states, I will just be a dependent drain on my family. I hate being a burden to them. The nurse can best respond: Is there any reason to tell your family about this now? You still have some time • in which you can enjoy life. I doubt that your loving family will view your terminal care as a burden. ep • I know. I would feel terrible if I had been told I was dying. ANS: B A persons reaction to a loss is influenced by the importance of what that person perceives the loss entails. To help the patient validate what the loss means is therapeutic. DIF: Cognitive Level: Application REF: m 191 OBJ: Clinical Practice #2 TOP: Value and Loss KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A patient tells the nurse during an admission interview that his wife went on to her reward. The nurse assesses that this statement is an indication that the patient: • has a strong religious belief system. .m yn ur si ng te st pr • has dysfunctional grieving and is unable to address his wifes death. • is uncomfortable with the term death and is using a euphemism. w w • is no longer grieving the death of his wife. ANS: C In many societies there is avoidance of using words such as died or death, and euphemisms are commonly used. DIF: Cognitive Level: Analysis REF: m 190 OBJ: Theory #1 TOP: Societal Views of Death KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A neighbor who was widowed 2 months ago gives the nurse his wife Helens gardening books because the two of you loved w • flowers. He tries to hold back tears, but begins to cry. To decrease his discomfort, the nurse should say: • We certainly did, and Im going to miss her helpshe was a real expert. • Helen wouldnt want to see you cryingshe would rather you smile and remember the good times, an • Things will get easier with time. Time has a way of healing even the most painful losses. Helen is in a better place; you should be glad she isnt suffering anymore. ANS: A Sharing the feeling of loss is appropriate and supportive and recognizes the loss of the grieving husband. DIF: Cognitive Level: Application REF: m 191 OBJ: Clinical Practice #2 TOP: Therapeutic Communication KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A terminally ill patient and his family have requested hospice care. The nurse clarifies hospice care philosophy as: • helping the patient die easily and quickly at home. st pr ep .c om • focusing on symptom management and comfort care. • excluding hospital care. supporting assisted suicide if that is the patients wish. ANS: B The philosophy of hospice care focuses on comfort care and the acceptance of death as part of life. Hospice is opposed to assisted suicide and provides relief of symptoms that are associated with terminal illness. Hospice care can be provided in a hospital, home, or extended care facility. DIF: Cognitive Level: Comprehension REF: m 198 OBJ: Theory #2 TOP: Hospice KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A terminally ill patient is angry and belligerent. He yells at the nurses and his family for not coming quickly enough when he calls, and he states that he isnt receiving the care he needs. The nurses most informative response would be: • Dont let him get away with this abuse. He doesnt need to yell at you. w w w .m yn ur si ng • te • • This may be how he feels best in dealing with this illness. Youll just have to ignore it. • Im afraid he is having a bad day and feels neglected. • Anger is a reaction that dying people experience. You may be feeling some anger yourselves. ANS: D ep .c om Anger is one of the stages terminally ill patients and their caregivers may experience. It may be prolonged, or it may be a passing stage or one that is returned to in the course of the final illness. Reacting with anger or just passively ignoring it does not assist the patient in dealing with his feelings. DIF: Cognitive Level: Analysis REF: m 195, Table 15-1 OBJ: Theory #1 TOP: Anger Phase KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A patient who was admitted to hospice for comfort care of endstage respiratory disease is asked what his hope is for his remaining life. He says, Im hoping for a miraclethat I will wake up one of these mornings and be able to breathe like when I was 20. The nurse would best respond: • Thats not likely to happen. Is there something more realistic you are hoping for? Your lungs are too damaged for you ever to breathe like you did when you were 20. • It must be very tiring to have to struggle for every breath you take. st pr • Your miracle may be in the form of medication that will improve your comfort. ANS: D Instilling hope that the struggle for respiratory relief will be available is a comfort measure. DIF: Cognitive Level: Application REF: m 194 OBJ: Clinical Practice #1 TOP: Hope KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: basic care and comfort • An oncologist has recommended that a hospice patient receive palliative radiation to reduce the pain of bony metastases. The patient reacts with anger, saying, I dont want any more treatments that dont cure my cancer! The hospice nurse tells the patient that the use of radiation: • may disqualify him from receiving hospice care. may halt the metastatic process. w • w .m yn ur si ng te • w • • of this type is not curative and is part of hospice care. will be used as a single treatment measure. Previous medications will be discontinued. ANS: C Palliative radiation is performed to relieve symptoms but does not direct its therapy toward cure, and thus is comfort care or hospice-appropriate treatment. Other medications for comfort will still be used in the hospice care. DIF: Cognitive Level: Analysis REF: m 197 OBJ: Theory #2 TOP: Palliative Radiation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient admitted to the nursing home for terminal care is determined that he should not receive extraordinary measures • including these desires in his will. • filing an advance directive with the health care facility. • informing his physician of his desires. ANS: C ur si ng te st pr ep .c An advance directive sets out the patients desires relative to end-of-life issues. A DNR only prevents the initiation of cardiopulmonary resuscitation (CPR). The naming of a durable power of attorney for health care or a health care proxy appoints a person to carry out the advance directive. DIF: Cognitive Level: Application REF: m 200 OBJ: Clinical Practice #4 TOP: Advance Directive KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • The nurse is aware that in order to provide effective support to grieving patients and families, the nurse must: • keep a professional distance from the situation. om such as resuscitation or the use of a ventilator if he stops breathing, or intravenous (IV) fluids or a feeding tube if he is unable to eat or drink. The nurse explains that these desires can best be honored by: • signing a do-not-resuscitate (DNR) request. understand all the theories of grief. • solidify his or her own view of death. yn • stay positive and optimistic at all times. ANS: C Nurses must understand and solidify their own view of death before they can offer effective support to dying patients and their significant others. Constant optimism and positive attitudes are not always appropriate. DIF: Cognitive Level: Comprehension REF: m 190 OBJ: Clinical Practice #1 TOP: Attitude Toward Death KEY: Nursing Process Step: Planning MSC: NCLEX: Psychosocial Integrity: psychosocial adaptation • The patient in hospice care says to the hospice nurse, I want you to read my obituary that I just wrote. The nurse assesses that this patient is in the Satir-Blevins (2008) stage of: • practice. w w w .m • • chaos. • integration. • wheezing and labored. w • w .m yn ur si ng te st pr ep .c om a c c e p t a n c e . A N S : A According to the Satir-Blevins theory of loss (2008), this patient is in the phase of practice. The patient is practicing with the writing of the obituary the fact that life is coming to an end. DIF: Cognitive Level: Analysis REF: m 190 OBJ: Theory #1 TOP: Satir/Blevins theory of Change & Loss KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse can assess Cheyne-Stokes respiration by its characteristics of respirations that are: • harsh and rattling. w • shallow followed by periods of apnea. • long periods of apnea followed by a hiccoughing breath. ANS: C Cheyne-Stokes respirations become more and more shallow followed by periods of apnea, and then respirations resume. DIF: Cognitive Level: Comprehension REF: m 191 OBJ: Theory #5 TOP: The Dying Process KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • When a patient admitted for terminal care is asked by the admitting nurse, What has your doctor told you about your illness? the patient states, She says that I have a terminal illness, but I know shes wrong. The nurse recognizes that: • the patient has a doctor who does not tell patients when they have a terminal illness. the patient is in denial and is unable to consciously admit what he has been told by the doctor. • the patient needs to be told that he doesnt have long to live so that he can make his final arrangeme om • she will have to avoid all conversation that refers to his disease or symptoms so as not to increase h ANS: B The patients statement indicates Kbler-Rosss stage of denial in which patients will not accept information and buffer themselves from information that may be painful. DIF: Cognitive Level: Analysis REF: m 195, Table 15-1 OBJ: Theory #1 TOP: Denial Phase KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity: coping and adaptation • A terminal patient asks the nurse if he could be given a deliberate overdose of medication that would end this. According to the Code for Nurses, the nurses most ethical response would be: • Bringing on your death in this manner would be a subject you should discuss with your family and .m yn ur si ng te st pr ep .c • I cannot ethically give you a deliberate overdose. w • I can contact the physician and request an order for a drug that could be used as you request. w • Let me have a while to consider your request. ANS: C The position of the American Nurses Association (ANA) expressly states that active euthanasia and assisted suicide are considered a violation of the ANAs Code for Nurses. DIF: Cognitive Level: Application REF: m 200 OBJ: Theory #7 TOP: Assisted Suicide KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A patient who is terminally ill has been unable to maintain good w • nutrition because of nausea and anorexia and has lost a great deal of weight. He is now unable to change his position in bed and needs frequent perineal care because of urinary incontinence. The nurse planning his care would include in the plan of care to: • coax him to eat high-calorie, high-fat food. • provide laxatives and stool softeners to prevent constipation. • contact the physician for an order for tube feeding. provide him with an air pressure mattress. ANS: D Provision of an air pressure mattress will help preserve the patients skin integrity that the weight loss, inactivity, poor nutritional intake, and incontinence have caused. DIF: Cognitive Level: Application REF: m 198 OBJ: Clinical Practice #3 TOP: Skin Integrity KEY: Nursing Process Step: Implementation st pr ep .c om • yn ur si ng te MSC: NCLEX: Physiological Integrity: reduction of risk • A terminal patient in a skilled nursing home has stated that he does not want to get out of bed, because he is too tired and weak to sit in a chair. He sleeps on and off all day and night, his position is changed every 2 hours, and he is comfortable on his pain regimen. The next day the nurse will: assess his strength and desire to get out of bed, but permit him to remain in bed if he chooses, becau • position of comfort. .m w w w • • encourage him to sit in the chair for an hour, because it is important to change his activity or he wil inactivity. leave him in bed if he wishes, but have him do active exercises of his legs and arms to prevent furth get him out of bed for an hour in the morning and afternoon and for a short time (15 minutes) befor d. ANS: A does not sleep all day and stay awake at night. Comfort care recognizes that the patient is the best judge of his energy; if he does not wish to get out of bed, then frequent turning and positioning and use of appropriate pressure- and pain-relief measures are a better choice. DIF: Cognitive Level: Application REF: m 198 OBJ: Clinical Practice #3 TOP: Comfort KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort • A hospice patient is unable to tolerate food or fluids and has advance directives that indicate that he does not want IV fluids or tube feedings if he is unable to take oral feedings. His family is concerned that he will be very uncomfortable without food or fluids. The nurse should tell them that: • once the patient is unconscious, his health care proxy can order IV fluids or tube feedings to preven dehydration is painful, and medication can be given to overcome any pain. om • .c IV fluids or a tube feeding would make the patient much more comfortable, and they should try to t ep c. pr d. st ANS: D te accepting them. ng IV fluids or tube feeding would likely make the patient more uncomfortable, and dehydration has b decrease pain and discomfort. w w w .m yn ur si Dehydration in the terminally ill patient has been shown in research to decrease pain and to be a more comfortable condition than when tube feeding is introduced into the intestine or when IV fluids are used to reverse dehydration. DIF: Cognitive Level: Application REF: m 198 OBJ: Clinical Practice #5 TOP: Comfort KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: basic care and comfort • To help the family deal with the delirium of their dying relative, the nurse can suggest that they should: • stimulate the patient with music and visits from friends. • talk to the patient in quiet tones. • sit quietly in the room with the patient. • speak firmly to the patient to bring him back to reality. ANS: B Talking with the patient is comforting to the patient. Even when unresponsive, patients can hear. Stimulation is not helpful and may confuse the patient further. DIF: Cognitive Level: Application REF: m 198 OBJ: Theory #5 TOP: Delirium KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • After a patient death, the nurse is preparing to perform postmortem care. The body is placed supine with the head raised so that: • the deceased will appear to be sleeping. blood will not pool in the face and cause discoloration. • movement of the deceased will be more convenient. om • feces and urine will drain onto the bed pads. ANS: B After death, the head of the deceased is raised to prevent discoloration by the pooling of blood in the face. DIF: Cognitive Level: Comprehension REF: m 202 OBJ: Clinical Practice #6 TOP: Postmortem Care KEY: Nursing Process Step: Implementation MSC: NCLEX: N/A • The family members of a young man, who is in the intensive care unit on life support after suffering irreversible brain damage resulting from a motorcycle accident, have been approached by the organ transplant team to consider organ donation. When they ask the nurse about this process, the nurses best response would be: • There is a small cost to the family for the donation, but it is for a good cause. yn ur si ng te st pr ep .c • Often families are comforted by the knowledge that some good came from this tragedy. • Because your son has been on life support, the only organs they can use would be his kidneys. w Organ donation will probably delay the funeral. ANS: B There are many more persons needing organs than there are donors. Nurses are in a position to educate the public about organ donation. DIF: Cognitive Level: Application REF: m 201 OBJ: Clinical Practice #2 TOP: Organ Donation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A terminally ill patient is experiencing a great deal of dyspnea and noisy, rattling, rapid respirations. The nurse administers morphine in a very small liquid or intramuscular dose. The w w • .m • purpose of this is to: • decrease pain caused by dyspnea. • hasten death by stopping respirations. • decrease respiratory rate and relieve dyspnea. dry up secretions that are causing rattling. ANS: C Morphine is used to ease terminal dyspnea by reducing the rate and increasing the depth of respirations. bargaining. • anger. ng • w w w .m yn ur si • d e p r e s s i o n . te st pr ep .c DIF: Cognitive Level: Comprehension REF: m 198 OBJ: Clinical Practice #3 TOP: Use of Morphine KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • When the patient says, I can die happily if I can live long enough to see my first grandchild that will be born next month. The nurse assesses that this patient is experiencing Kbler-Rosss stage of: • denial. om • A N S : B Kbler-Rosss stages of coping with death include the bargaining stage in which the person seeks the reward of extended life. DIF: Cognitive Level: Comprehension • bargaining. • depression. om REF: m 195, Table 15-1 OBJ: Theory #1 TOP: Stages of Coping with Death KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity: coping and adaptation • When the nurse notes an increase in the level of daily function in the terminal patient, the nurse assesses that this patient has reached Kbler-Rosss level of: • yearning. .c • w w w .m yn ur si ng te st pr ep a c c e p t a n c e . A N S : D Kbler-Rosss stages of coping with death include the acceptance stage in which the struggle is over, the pain is gone, and the patient has found peace. The patient frequently demonstrates a heightened level of activity in his or her daily function during this stage. DIF: Cognitive Level: Comprehension REF: m 191 OBJ: Theory #1 TOP: Acceptance Stage KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity: coping and adaptation • When the parents of a child who is on life support ask what indicates brain death, the nurse responds that brain death occurs when: • there have not been signals on the EKG. • no deep tendon reflexes can be stimulated. • there is an absence of EEG waves. there have been no voluntary respirations for 5 minutes. ANS: C Brain death is the absence of brain waves on an EEG; this has been the definition of death since the 1970s. DIF: Cognitive Level: Knowledge REF: m 191 OBJ: Theory #1 TOP: Brain Death KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation The culturally sensitive nurse would delay a discussion relative to a patients terminal illness if that patient were a: • 28-year-old Caucasian auto mechanic. 35-year-old Mexican American farm laborer. • 40-year-old Chinese businessman. 50-year-old American Indian policeman. ANS: B Persons with Hispanic and Korean backgrounds are less likely to want to know about their terminal disease, feeling that the family should make the decisions about life-sustaining treatments. DIF: Cognitive Level: Comprehension REF: m 192 OBJ: Theory #3 TOP: Cultural Considerations KEY: Nursing Process Step: Planning MSC: NCLEX: Psychosocial Integrity: coping and adaptation • The nurse caring for a terminally ill patient with renal failure would question an order for pain control that prescribed: • methadone. w w .m yn ur si ng te st • pr • ep .c • om • oxycodone. • meperidine. w • • m o r p h w .m yn ur si ng te st pr ep .c om i n e . A N S : C Patients in renal failure cannot adequately clear meperidine (Demerol) from their system and will become oversedated. DIF: Cognitive Level: Application REF: m 197, Table 1-2 OBJ: Theory #4 TOP: Meperidine KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: pharmacological therapies COMPLETION • When a patient chooses to die by refusing treatment that would prolong life, it is called . ANS: passive euthanasia Passive euthanasia is when the patient is choosing to refuse treatment for himself or herself, which will result in death. DIF: Cognitive Level: Comprehension REF: m 200 OBJ: Theory #6 TOP: End-of-Life Issues KEY: Nursing Process Step: N/A MSC: NCLEX: N/A , • The five stages identified by Dr. Elisabeth Kbler-Ross are , , and . ANS: , denial; anger; bargaining; depression; acceptance Each dying patient and family member may experience any of these stages during the dying process. Understanding the stages assists in early identification and appropriate interventions to help the patient and family cope. DIF: Cognitive Level: Knowledge REF: m 195, Table 15-1 w w OBJ: Theory #1 TOP: The Dying Process KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • Individuals move through the stages of grief at their own pace. When a person is stuck in a stage and cannot move forward, this . is called ANS: dysfunctional grieving Dysfunctional grieving is visible grief over a prolonged period of time. Some theorists say grief after 6 months is dysfunctional; others say up to 2 years. DIF: Cognitive Level: Analysis REF: m 191 OBJ: Theory #1 TOP: Grieving KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The nurse who adopts the Maciejewski theory of grief assesses for the reduction of grief after a period of months. ep .c om ANS: 6 six According to the theory of Maciejewski the indicators of grief should peak and begin to diminish after a period of 6 months. DIF: Cognitive Level: Application REF: m 191 OBJ: Theory #1 TOP: Maciejewski Theory KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity: coping and adaptation MULTIPLE RESPONSE • During the dying process, patients may experience a bad taste in their mouth. Which of the following are appropriate nursing actions? (Select all that apply.) • Offer the patient hard candy. Assist the patient with frequent oral care. • Offer the patient large amounts of water or juice. • Explain to the patient that this is a normal part of dying and nothing can be done. • Offer the patient mouthwash. te Offer the patient frequen t meals. ANS: A, B, E Hard candy, mouthwash, and oral care help stimulate saliva production and relieve the dryness and any bad taste in the patients mouth related to the dryness. DIF: Cognitive Level: Application REF: m 198 OBJ: Clinical Practice #3 TOP: Nursing Process and the Dying Patient KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort • A coroner is required to investigate death in which of the following situations? (Select all that apply.) • Deaths from injury w w w .m yn ur si ng • st pr • • All deaths that occur at home • Suspected suicides • Any death in the hospital • Deaths of persons not under the care of a physician ANS: A, C, E The coroner investigates death when there may be a question of cause. DIF: Cognitive Level: Analysis REF: m 201 OBJ: Clinical Practice #6 TOP: Postmortem Issues KEY: Nursing Process Step: N/A MSC: NCLEX: N/A • The nurse discusses the grief theory of Maciejewski, which outlines the stages of grief as including: (Select all that apply.) • yearning. bargaining. • anger. • denial. .c om • ep • ur si ng te st pr d e p r e s s i o n . w w w .m yn A N S : A , C , D , E The grief theory of Maciejewski states that the loss is accepted, but followed by denial, yearning, anger, depression, and acceptance. DIF: Cognitive Level: Comprehension REF: m 191 OBJ: Theory #1 TOP: Maciejewski Theory KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation OTHER Place the steps of postmortem care in their proper sequence. (Separate letters with a comma and space as follows: A, B, C, D, E.) Remove all tubing and equipment from the room. Cleanse the body of all body fluids. Position the body with the head of the bed raised 15 degrees. Dress the deceased in a hospital gown and cover the deceased up to the chest. Replace dentures. w w w .m yn ur si ng te st pr ep .c • • • • • ANS: C, E, B, A, D Postmortem care should be performed with dignity and reference for the deceased. The body should be positioned with the head raised, dentures should be replaced, the body should be cleansed of all body fluids and soiled dressings, all tubing and equipment should be removed from the room, and the deceased should be dressed in a gown and covered up to the chest. om •