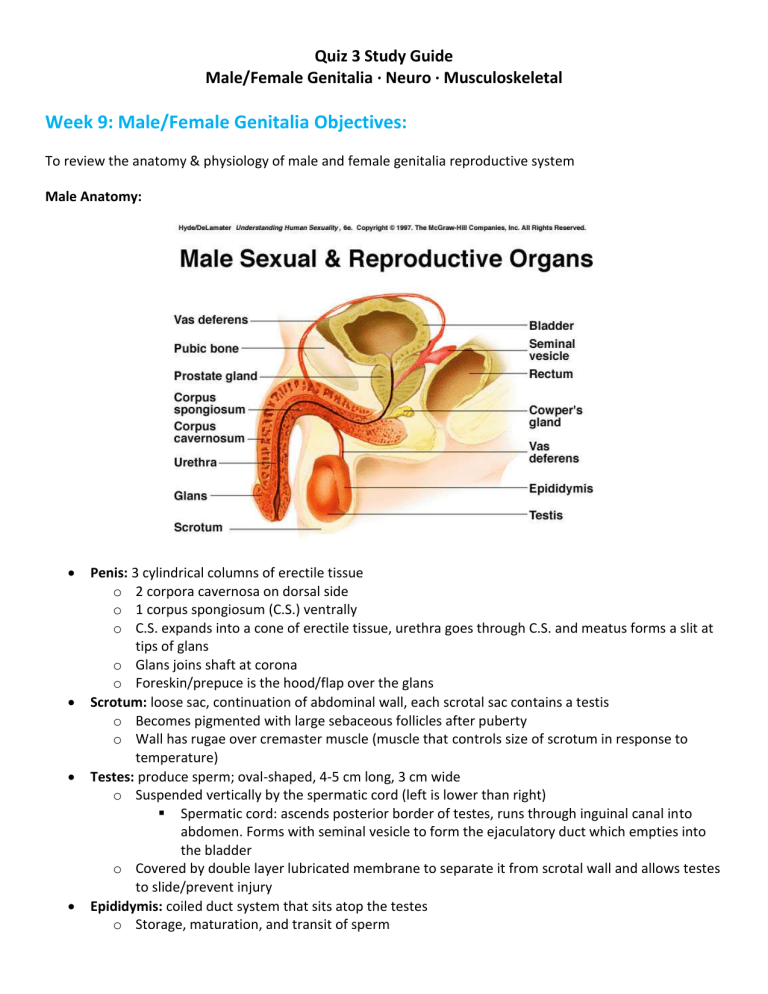
Quiz 3 Study Guide Male/Female Genitalia · Neuro · Musculoskeletal Week 9: Male/Female Genitalia Objectives: To review the anatomy & physiology of male and female genitalia reproductive system Male Anatomy: Penis: 3 cylindrical columns of erectile tissue o 2 corpora cavernosa on dorsal side o 1 corpus spongiosum (C.S.) ventrally o C.S. expands into a cone of erectile tissue, urethra goes through C.S. and meatus forms a slit at tips of glans o Glans joins shaft at corona o Foreskin/prepuce is the hood/flap over the glans Scrotum: loose sac, continuation of abdominal wall, each scrotal sac contains a testis o Becomes pigmented with large sebaceous follicles after puberty o Wall has rugae over cremaster muscle (muscle that controls size of scrotum in response to temperature) Testes: produce sperm; oval-shaped, 4-5 cm long, 3 cm wide o Suspended vertically by the spermatic cord (left is lower than right) Spermatic cord: ascends posterior border of testes, runs through inguinal canal into abdomen. Forms with seminal vesicle to form the ejaculatory duct which empties into the bladder o Covered by double layer lubricated membrane to separate it from scrotal wall and allows testes to slide/prevent injury Epididymis: coiled duct system that sits atop the testes o Storage, maturation, and transit of sperm o Lower part continuous with vas deferens (duct which forms spermatic cord with other vessels) Prostate: 3.5 cm long x 3 cm wide glandular tissue w/ small ducts that open into urethra, lies below bladder & encircles urethra, consists of 5 lobes o Secretions are thin, milky, alkaline and serve as transport medium for spermatozoa (involved in reproduction & protection against UTI) o Site of problem for aging male Health history cues: efficiency of urination, dull low perineal pain, rectal bleeding, change in stool, FH cancer Risk factors: 50+ y/o, AA, FH prostate cancer, diet high in animal fat, high serum testosterone Screening Guidelines Age 50 for average risk of prostate cancer and 10+ year life expectancy should be asked Age 45 for men at high risk of cancer (AA, first-degree relative with cancer at early age <65) Age 40 at even higher risk (more than 1 first-degree relative with prostate cancer at early age) Men who choose to have regular prostate screening should have PSA blood test w/ or w/o rectal exam PSA of less than 2.5 ng/mL only needs retested every 2 years PSA greater than 2.5 ng/ML = yearly screening Men 70+ y/o should not be routinely screened Inguinal area: groin, juncture of lower abdomen & thigh o Lymphatic of penis/scrotum drain to the inguinal lymph nodes o Inguinal canal: 4-6 cm long narrow tunnel passing between layers of abdominal muscle; has internal and external ring o Possible site of inguinal herniation Male Anatomy Function: Excretory organ for urine Introduces sperm into vagina o Erection: 2 corpora cavernosa become engorged with blood; neurovascular reflex stimulated by psychogenic and reflex mechanisms o Orgasm: sensation accompanying ejaculation, emission of fluid, constriction of vessels Procure a history and physical: Health History Cues o C/o frequency, burning, urgency pain, discharge, change in stream, hesitancy, straining o Color, odor o Incontinence; loss of urine when laughing/sneezing o Hx infections o Lesions on penis, lumps, swelling o Safety – sex issues, sexual preference, difficulty having/maintaining erections Age Related: o Chlamydia 14-35 o Testicular torsion 12-25 o Varicocele 15-35 o Testicular cancer 16-35 o GC urethritis <35 o Hydrocele >30 o Testicular lymphoma 50+ o Erectile dysfunction 50+ (affects 30-50% males age 40-70, risks include age, smoking, obesity) o Bacteriuria >65 PMH: STIs, UTI, Tanner’s staging, cancer, trauma, BPH, congenital deformity, impotency FH: Varicocele, cancer, hypospadias, mother’s use of DES (synthetic estrogen) SH: ETOH, TOB, drugs, sexual practice, sleep, diet, exercise, self-exam Medication: antibiotics, hormone replacement, HTN, psychotropic Male Genitalia Assessment & Normal/Abnormal Findings Inspect/Palpate o Hair distribution o Penis Skin is wrinkled, hairless, w/o lesions, glans is smooth, urethral meatus is central, foreskin easily retractable, shaft should be smooth, semi-firm, non-tender Compress glans between thumb & forefinger, meatus edge should be pink and smooth w/o discharge (any discharge should be obtained for culture) Abnormals Phimosis: inability to retract foreskin Paraphimosis: unable to return foreskin to original position Hypospadias: ventral location of meatus Epispadias: dorsal location of meatus Inflammation Lesions: chancre, vesicles, condyloma lata (flat warts second stage of syphilis) Pubic lice, excoriated skin Red, everted, edematous meatal edge w/ discharge – infection Stricture – narrowed opening Infant assessment: foreskin not retractable at birth; assess meatus; shaft should be straight (bowing down = chordee, a congenital birth defect which is a contraindication of circumcision until corrected); scrotal edema is not unusual d/t maternal estrogens; palpate testes 10 mm wide, 15 mm long (undescended testicle = cryptorchidism) o Scrotum Scrotal size varies, asymmetry is normal. Contents should slide easily, testes freely movable, oval, firm, rubbery, slightly tender to moderate pressure. Epididymis feels discrete, softer than testes, smooth, non-tender. Spermatic cord should be smooth and non-tender Transillumination - if swelling or mass noted, normal contents do not transilluminate Serous fluid of hydrocele or spermatocele transilluminate as red glow o Prostate Inspect anal opening (lesions, warts, tears, hemorrhoids), note prostate size, contour, consistency, and mobility (normal is firm, smooth, slightly movable, non-tender) BPH = rubbery, boggy, enlarged Cancer = stony, hard, irregular, fixed nodule Prostatic abscess = fluctuant softness Prostatitis = swollen, exquisitely tender o Normal documentation: no tenderness, lesions, inflammation, or discharged from circumcised penis, testes descended bilaterally, no pain, masses, transillumination, no inguinal hernia bilaterally Abnormals o Scrotal swelling (CHF, renal failure, local inflammation) o Lesions (may be STI) o Absent testes (true or r/t migration) o Atrophied testes o Fixed testes o Nodule, tenderness, swelling (may be epididymitis) o Thickened cord, soft, swollen, tortuous (varicocele, pt. must be standing to note) o Testicular torsion: excruciating one-sided testicular pain, sudden swelling, testicle elevation, N/V, ABD pain, fever, hx testicular pain, most frequently seen in 12-18 y/o but can occur at any age o Hydrocele: common in newborns, usually goes away within 1st year; testicle drops into scrotum and fluid flows/surrounds Noncommunicating hydrocele = sac closes and fluid remains, often found in newborns and fluid usually absorbs over time Communicating hydrocele = sac compressed, fluid goes into abdomen or hydrocele changes size; appears after activity; requires intervention o Hernia: bulge observed while pt. standing, triangular slit-like opening may or may not allow finger; causes and risks include stress in abdomen, weak spot in ABD wall, heavy lifting, overweight, family history, ageing Female Anatomy: External: o Vulva - Mons pubis, clitoris, labia majora, labia minora, frenulum o Vestibule – urethral meatus, Skene’s glands posterior to meatus, vaginal orifice, Bartholin’s glands o Perineum, anus Internal: o Vagina, cervix (center = os, has red and rough looking columnar epithetlium), smooth, pink cervical epithelium, uterus, fallopian tubes, ovaries Procure history and assessment Health history cues o Pain w/ urination or intercourse o Discharge, burning, frequency, urgency, color, odor, open sores o Control of urine when laughing, sneezing o Vaginal itching, dryness, discharge (consistency, odor, length of time, douching) o Medication use o ABD pain o Past surgeries Age-related problems o STIs 15-25 o Uterine myomas 30-50 o Cervical cancer 40-60 o Post-menopausal: vulva cancers, cystocele, rectocele, atrophic vaginitis o Over 60: endometrial cancer, ovarian cancer, vaginal cancer PMH: detailed menstrual hx (menarche, frequency, duration, amount of flow, pain, cramping, mood, spotting); obstetric hx; menopausal hx (age of cessation, spotting, symptoms); sexual history (gender, # partners, contraceptives, STIs, abuse) FH: cancer, daughters of DES, multiple pregnancies, congenital anomalies Medications: antibiotics, OC, OTC SH: ETOH, tobacco, sexual practices, home condition, hobbies, exercise, diet, last pap Tanner’s stage Female Assessment Inspect/palpate o Smooth skin, no lesions, hair evenly distributed inverted triangle; labia are symmetric, plump, well-formed Abnormal: open lesion, redness, edema, lice/nits, swelling, excoriation, nodules, rash, adhesions, bruising, foul-smelling discharge, fistulas, fissures, varicosity; bulging of vaginal wall (prolapse, cystocele, rectocele); paper-thin perineum, tenderness o Bartholin’s glands: normally soft and homogenous; Abnormal: swelling, induration, pain, erythema around opening (Bartholin cyst) o Infant assessment: may have milky white discharge, may be prominent d/t maternal estrogen o Child assessment: vaginal discharge may be d/t perineal irrituation or abuse; bleeding is always a concern (trauma, abuse, precocious puberty) Speculum exam o Note vaginal wall, rugae, discharge, abrasions, irritation, swelling, pain, tightness o Cervix Pink, even color Chadwick’s sign – 2nd month of pregnancy cervix is blue Menopausal – pale Smooth, Nabothian cysts are an expected finding (small white or yellow raised cysts) o Discharge from cervix or vagina – normal is creamy or clear, odorless, thick/thin o Abnormals: Redness, inflammation, cyanotic os (not pregnant), lateral positioning (adhesion or tumor), projection (>3 cm = prolapse), hypertrophy (>4 cm = inflammation, tumor); strawberry spot = trichomoniasis; erosion, ulceration; cervical polyp = bright red growth protruding from os; foul smelling yellow, green, white, gray discharge Cervical Cancer HPV causes ~90% cervical cancer Prevention o 1st sexual intercourse until late teens or older o Limit # partners o Quitting smoking o Avoiding intercourse with people who are infected with warts or have high # partners o Vaccine: Gardasil 9 Screening o 21-29 every 3 years with cervical cytology alone o 30-65 every 3 years with cervical cytology alone, every 5 years hrHPV testing alone, or every 5 years combo hrHPV and cytology (co-testing) o 65+ not recommended if they have had adequate prior screening and are not high risk PAP Guidelines o 30+ tested for HPV with pap, if both are normal re-test in 3 years o 65-70 woman can stop screening if they’ve had 3 normal pap tests in a row within 10 years Should continue if sexually active, have multiple partners, or hx abnormal pap o Hysterectomy do not need to have a pap unless they have an intact cervix or surgery was done as a treatment for precancerous condition/cancer o Do not do pap if menstruating, discharge, douche, or intercourse within 24 hours Bimanual Exam Palpate vaginal wall – smooth w/o induration, nodules, or tenderness Cervix – midline, smooth like the tip of nose, softens/feels velvety @ 5-6 weeks (Goodell’s sign); evenly rounded w/o nodules; moveable with finger, no pain o Pain is called +Cervical motion tenderness (CMT) Pelvic inflammatory disease? Infection? Uterus – wall firm, smooth, freely moveable w/o pain Adnexa = fallopian tubes, ovaries – should have no pain Rectovaginal – looking for pain, nodules, or fistula Review Tanner staging male & female Week 10: Neuro Objectives: To review the anatomy & physiology of the neuro system Cerebral Cortex o Frontal – personality, emotion, behavior intellect Broca’s – frontal lobe mediates speech Damage = aphasia (non-fluent: struggle with words, slow, monosyllabic) o Parietal – sensation o Occipital – vision o Temporal – auditory Wernicke’s – associated with auditory reception Damage = aphasia (fluent aphasia: talks and reads easily but words are jumbled and meaningless) o Basal ganglia – primitive motor areas, automatic movement o Thalamus – relay station o Hypothalamus – temperature regulation, sleep Cerebellum – located under occipital lobe o Motor coordination of voluntary movements; equilibrium, muscle tone; operates entirely below conscious level o Brain stem – central core Midbrain Pons Medulla Spinal Column – connects brain to spinal nerves; mediates reflexes o Main highway for ascending/descending fiber tracts o Nerve cell (grey matter) H shape with anterior/posterior horns Major Sensory Pathways o Spinothalamic tract Lateral = pain, temp Anterior = crude or light touch o Posterior columns Position, proprioception, vibration, tactile discrimination Major Motor Pathways o Corticospinal/Pyramidal Voluntary movement (skilled, purposeful), crosses to other side, higher level o Extrapyramidal Muscle control, gross automatic movements, older, lower level o Cerebellar Coordinates movement, equilibrium, posture Peripheral Nervous System o Carry input to CNS via sensory afferent fibers o Deliver from CNS via motor efferent fibers o Spinal Nerves 8 cervical; 12 thoracic; 5 lumbar; 5 sacral; 1 coccygeal Mixed nerves – dorsal (afferent) root & ventral (efferent) root Dermatome – area of skin supplied by a single spinal nerve C6 = thumb T4 = nipple line T10 = umbilicus S2-S4 = perineum L5 = top of foot S1 = bottom of foot o Cranial Nerves I – Olfactory – S II – Optic – S III – Oculomotor – B IV – Troclear – M V – Trigeminal – B VI – Abducens – M VII – Facial – B VIII – Acoustic – S IX – Glossopharyngeal – B X – Vagus – B XI – Spinal accesory – M XII – Hypoglossal – M Autonomic Nervous System – mediates unconscious activity, innervates smooth muscle (cardiac, involuntary, glands) o Sympathetic: fight or flight (accelerate/brake) o Parasympathetic: everyday maintenance Reflex Arc – unconscious defense mechanism of nervous system o DTR o Permits quick reaction to potentially painful/harmful situation To procure a history and physical of the patient with a neurological disorder Most important components: mental status, cranial nerves, motor system, sensory system, cerebellum, gait Infant assessment: abnormalities present as “failure to do”; include assessment of mental status, gross & fine motor, cry, tone (flaccid/spasticity), DTR can be variable (use finger instead of hammer), cranial nerves, primitive reflexes Child assessment: combine neuro & development (DDST), developmental milestones, cranial nerves, gait, strength, coordination, sensation, DTR Developmental quotient o Developmental age x 100 o Developmental quotient > 85 is considered normal o 70-85 may indicate that there is some developmental delay o <70 indicates developmental delay Health history cues o Headaches, dizziness, changes in sensation, concentration, response time, memory, syncope, eyesight, hearing, speech, swallowing, head injury, seizures, tremors, incoordination, gait changes, vertigo PMH: ALS, MS, AVM, CVA, childhood seizures, trauma, neuropathy, migraines, Alzheimer’s, HTN, cardiac disease, DM, surgeries, injuries Meds: Antidepressants, anti-seizure, narcotics, anti-anxiety FH: AVM, headaches, epilepsy, Alzheimer’s, Huntington’s Chorea SH: ETOH, drugs, tobacco, sexual practice, travel history, work/home environment, hobbies, stress, sleep, diet, exercise Cerebral Assessment Fully Awake: able to respond to various stimuli, may be disoriented/forgetful Alert: fully awake, oriented to person, place, time. Able to respond/carry out commands Lethargic: Sleepy but arousable with gentle shaking/calling name/falls back to sleep easily, may be disoriented Obtunded: Sleeps most of the time, few spontaneous movements, vigorous shaking/name calling required, capable of verbal response but likely inappropriate Stuporous: Semi-comatose, unconscious most of the time, strong painful stimuli required for withdrawal response Comatose: Can not be aroused Cranial Nerve Assessment: Olfactory I o Occlude nares one at time, assess patency o Aromatic substance ID o Abnormal: anosmia (can be r/t smoking, cocaine, allergic rhinitis) Optic II o Visual acuity, confrontation, ocular fundus o Abnormal: Defect/absent central vision or peripheral vision (hemianopsia), absent light reflex, papilledema Oculomotor III, Trochlear IV, Abducens VI o Test pupil size, regularity, equality, reaction, accommodation, extra-oculomotor movement o Abnormal: Ptosis, dilated pupil, failure of movement up/down/in/laterally, nystagmus Trigeminal V o Motor function, clench teeth and palpate temporal/masseter muscles Abnormal: asymmetry, pain, decreased strength o Sensory function, eyes closed touch face with light touch ophthalmic, maxillary, mandibular Abnormal: decreased or unequal sensation o Corneal reflex, touch cornea with wisp of cotton Abnormal: no blink Facial VII o Motor: mobility/symmetry with facial expressions Abnormal: muscle weakness, asymmetry, Bell’s palsy Bell’s Palsy – acute peripheral facial nerve palsy of unknown cause; 60-75% facial palsy labeled as Bell’s palsy o Recurrence rate of 4-14% o Infectious causes include Epstein Barr, HSV, adenovirus, rubella, mumps, influenza B, coxsackievirus, cytomegalovirus o Affects men & women equally, less common before 15 or after 60 o DM present in 5-10% o Risk is 3x greater during pregnancy especially 3rd trimester & 1st week postpartum o Symptoms: sudden onset over hours, numbness of face, feels stiff pulled to one side, dry mouth, difficulty speaking, loss of taste in front portion of tongue, dryness or watering of affected eye, turned out lower eyelid, dribbling when drinking, ear pain, intolerance to loud noises on affected side o Pnemonic: COWS = Close your eyes, Open (PCP tries to open pt.’s eyes), Wrinkle your forehead, Smile o Sensory: sweet, salt, sour flavors Abnormal: unable to identify taste/loss of taste Acoustic VIII o Vestibular dysfunction, test with Weber and Rinne tests o Abnormal: decrease/loss of hearing, conduction or sensorial Glossopharyngeal IX, Vagus X o Motor: gag reflex, say “ah”, voice, swallowing o Sensory: nerve mediates taste on posterior 1/3 tongue but difficult to assess o Abnormal: Absence/loss of pharyngeal symmetry, uvula doesn’t rise, no gag, hoarseness Spinal Accessory XI o Strength of sternomastoid, trapezius, rotate head against resistance, shrug shoulders against resistance o Abnormal: atrophy, muscle weakness, paralysis Hypoglossal XII o Inspect tongue and movement, repeat “light, tight, dynamite” o Abnormal: atrophy, fasciculations, deviation of tongue Neuro Assessment - Motor System Muscles: size, strength, symmetry o Decerebrate rigidity: rigid, sustained contracture of extensor – midbrain and pontine damage o Decorticate rigidity: rigid, sustained hyperflexion – lesions interfere with corticospinal tract *think, pulling towards core = decorticate* o Pronator drift: downward drift may indicate hemiparesis or IICP Meningeal Irritation o Signs: violent headache, photophobia, fever, N/V, decreased LOC, convulsions o Nuchal rigidity: pt. in supine position, flex neck – resisting this movement is a positive sign for irritation: meningitis by bacteria, virus, fungi, mycobacteria o Kernig’s sign: pt. in recumbent position, flex hip, flex @ knee, attempt to extend knee. Positive is resistance to extension w/ pain o Brudzinski sign: Passively flex neck forward to chest. Positive is flexion of one or both legs, arms may also flex Gait – observe walking 10-20 ft., turn, return, step length 15” o Abnormal: stiff, immobile, staggering, reeling, lack of arm swing, unequal rhythm, slapping of foot, scraping toes of shoe, ataxia Romberg’s test – stand with feet together and arms at sides, close eyes, hold position for 20 seconds o Abnormal: + Romberg = sways, falls, must widen base of feet to stop fall o + can indicate MS, ETOH, loss of proprioception/vestibular function Rapid alternating movements (RAM) o Pat knees with both sides of hands increasing speed o Abnormal: lack of coordination, slow, clumsy, sloppy response Neuro Assessment – Sensory System Spinothalamic tract: pain (pin prick, sharp vs. dull), temperature, light touch o Abnormal: Hyperesthesia (increased or altered cutaneous sensitivity to touch, pain, or temp) Hypoesthesia (decreased sensitivity to touch, pain, or temp) Analgesic (absence of cutaneous sensitivity) Posterior column: o Vibration – place tuning fork over bony prominence, start distal (fingers/toes) and move inward until senses, compare side to side Abnormal: loss of vibratory sense = peripheral neuropathy (DM, ETOH) o Position – kinesthesia: test ability to perceive passive movements of extremities (big toe up or down and have pt. report place) Abnormal: loss of position sense o Tactile discrimination – fine touch – stereognosis, graphesthesia, two-point discrimination, extinction, point location Abnormal: inability to perform indicates lesion of sensory cortex or posterior column Reflexes – assessing side to side, responses should be equal Reflex response o 4+ very brisk hyperactive with clonus = disease o 3+ brisker than average, may indicate disease o 2+ normal, average o 1+ diminished, low normal o 0 no response = SC damage Biceps Reflex – C5-C6 o Support forearm, place thumb on biceps tendom, strike blow with thumb o Normal = flexion of forearm Triceps Reflex C6-C7 o Suspend by upper arm, strike tendon directly above elbow o Normal = extension of forearm Brachioradialis – C5-C6 o Hold thumb to suspend forearm, strike forearm directly 2-3cm above wrist o Normal = flexion & supination Quadriceps – L3-L4 “knee jerk” o Strike tendon just below patella with knees dangling o Normal = extension of lower leg Achilles – S1-S2 “ankle jerk” o Hold foot in dorsiflexion and strike tendon directly o Normal = plantar flexion against hand Can see slowed relaxation phase in hypothyroidism Superficial o Abdominal upper T8-T10 o Abd lower T10-T12 o Cremasteric L1-L2 (part of spermatic cord, reflex to temperature or stress) o Plantar L5-S1 Pathological o Grasp: abnormal after infancy Frontal lesion on contralateral side o Snout: puckering of lips, abnormal after infancy ALS – amyotrophic lateral sclerosis o Glabellar: hyperactive blinking with tap to forehead Lesion to pons, Parkinson’s o Sucking: abnormal after infancy Bifrontal disease o Clonus: Upper motor neuron disease, preeclampsia o Babinski: normal until 15-18 months, abnormal = fan great toe with toe abduction Lesions of pyramidal tract, stroke, trauma Disorders of CNS AIDS dementia Huntington’s chorea MS Seizures Meningitis Encephalitis Lyme disease Tumors/strokes Disorders of PNS Myasthenia gravis Guillain-Barre Peripheral neuropathy Week 11: Musculoskeletal Objectives: Anatomy Purpose: support, movement, protection, production, storage Joints – union between 2 bones; 3 classifications o Synarthrosis – non-synovial immovable (growth plate, between distal ends of radius & ulna, root of tooth to mandible) o Amphiarthrosis – non-synovial slightly moveable (vertebrae, symphysis pubis) o Diarthrosis – freely moveable (shoulder, elbow) Synovial joints: cavity filled with lubricant, freely moveable o Fibrous capsule surrounded by ligaments – fibrous bands running from bone, bone helps prevent movement in undesirable ways o Uniaxial joints Hinge – angular movement in 1 axis + 1 plane (elbow, fingers, knee) Pivot – rotary movement, ring rotates around a pivot (radioulnar, 1st & 2nd cervical vertebrae) o Biaxial joints Saddle – articulating surface of 1 bone is convex & surface of 2nd bone is concave (thumb) Condyloid – angular motion on 2 planes without axial rotation (wrist between distal radius & carpels) o Multiaxial joints Ball & socket – round end of bone into cuplike cavity (shoulder, hip) Gliding – gliding motion (vertebrae, tarsal bones of ankle) Tendons: strong connective tissue, outer cover of muscle belly, attaches muscle to bone Cartilage: avascular, dense, connective tissue covers end of opposing bone withstanding increased pressure & tension Ligaments: strong fibrous connective tissue, connect bones to each other at joint level & encase capsule, supports purposeful joint movement and prevent wrong movement Bursa: enclosed sac filled with viscous fluid located in areas of potential friction, act as cushion Muscles: 40-50% body weight; produces movement Skeletal – composed only voluntary muscle; exerts pull on bones near a joint, provides body contour, vary in size/strength Smooth Cardiac Health History Cues by structure Joints: stiffness, redness, swelling, pain with motion, pain coinciding with climate change Muscles: weakness, fatigue, aching, wasting, factors r/t exercise or sudden movement Skeletal: gait change, limping, numbness, tingling, crepitus, fractures Important to understand how injury occurred (activity, trauma), if and how pt. has self-treated (meds, splinting, ice/rest) PMH: Any m/s illness, trauma, deformity, immunosuppression, DM, PVD, med use of NSAIDs FH: RA, osteoporosis, gout, Paget’s, Dupytren’s contraction, SLE, Marfan’s, scoliosis SH: ETOH (osteoporosis risk), tobacco (osteoporosis risk), work/home environments, leisure activity, hobbies Risk factors for M/S problems: Obesity Poor nutrition Low calcium intake Medication history Chronic illness Age Gender Musculoskeletal Assessment Inspection – compare size, contour, swelling in hollow spaces (effusion, thickened synovial lining, inflammation of bursa, tendon inflammation, bony enlargements) o Abnormal: dislocation, subluxation (partial dislocation), contracture, ankylosis (fusion of bones across joint) Palpation – ROM (active and passive), isometric (contracts muscles at injured area w/o moving bone) o Abnormal: heat, tenderness, swelling, masses, localize problem to underlying structures (palpable fluid, visible bulge, doughy/boggy, crepitus (grating seen w/ arthritis) Muscle testing – flex and hold against resistance, graded o 5 – full ROM/full resistance o 4 – full ROM/some resistance o 3 – full ROM with gravity o 2 – full ROM gravity removed o 1 – slight contraction (10%) o 0 – no contraction (0%) o Muscle strength grade of 3 or less indicates disability Strain = muscle, heals faster o Grade 1: no specific event; pain/stiffness after activity; vague pain; no pain at rest; no ecchymosis; no know; nearly full ROM; nearly full strength; gait w/o limp or mild o Grade 2: pain w/ several steps; muscle spasm; pain in small area/spot; knot usually palpable; ecchymosis/swelling possible; pain between ½ - ¾ stretch ROM; decreased ROM with pain; definite limp/antalgic gait o Grade 3: “feels like someone hit me w/ a rock”; pain in area of tear of tendon or muscle belly; visible tear defect in muscle belly; no active motion, intense pain in first 1/3 ROM; can’t develop tension in muscle unit; can’t use muscle to ambulate Infant assessment: focus on detection of congenital deformities (dwarfism, extremity/digit abnormalities, annular bands that constrict extremity) Older child: upper extremity abnormalities are rare outside of injury, may have lower extremity/spinal issues Sprain = ligament, heals slowest Pain with passive ROM = joint, ligament, bursa Pain with active ROM = muscle, tendon Shoulder assessments o Resisted tests Abduction-supraspinatus Adduction- subscapularis, pectorals, lats Lateral rotation- infraspinatus Medial rotation- subscapularis Elbow flexion-biceps Triceps extension- triceps Painful arc- bursitis Drop arm - rotator cuff o Passive tests (you are moving their arm)- ligament, bursa, joint structures- you don’t need to do passive ROM if they are able to do active ROM Passive elevation Passive lateral rotation Passive medial rotation Scapula-humeral Horizontal adduction Abnormal: gradual pain, sleepless nights, painful overhead activity, loss of motion, outward prominence of scapula Impingement = + overhead Rotator cuff tear - + drop arm Elbow: o Tendonitis = + resisted bicep/tricep Bursitis = + Arc Serratus muscle damage = + scapular winging Book Test – pt. holds a book with an outstretched arm or tries to pick up a book Medial epicondylitis Golfer's elbow Lateral epicondylitis Tennis elbow Hand o o Tinnel’s - tests for carpal tunnel syndrome-striking median nerve with finger or reflex hammer in the coffin Phalen’s - tests for carpal tunnel syndrome- put wrists in full flexion at the wrist and have them hold that position; test is positive if pain is replicated Abnormals: Ulnar deviation = fingers outward Ankylosis = wrist extreme flexion Duputryen’s contracture (see below) Swan neck deformity = seen with RA Boutoinniere deformity = seen with RA Ganglion of wrist Heberdon’s – DIP seen with OA Bouchard’s – PIP seen with OA o Spine o Scoliosis Testing - have pt. bend over slowly and come back up slowly; watch ROM throughout to see if there is symmetry in the scapula, iliac crest, and gluteal fold Most common pediatric spine disorder 5 categories: degenerative (adult onset), neuromuscular, congenital, secondary, idiopathic (most common) Reported in degrees; >20* require x-ray Abnormals: Low back pain - lumbar strain Sciatica - starts in butt, down mid-posterior thigh, at knee it separates and goes medial/lateral back of leg Herniated disc – walk on toes/heel (increased pain, inability = + herniated disc), painful straight leg raise, DTR (patellar L2, 3, 4 and Achilles L5, S1) positive is contralateral pain = worse sign Lordosis – abnormal increase in forward curvature of lumbar spine Kyphosis – excessive outward curvature of spine, causing hunching Infant abnormalities: major defects often noted before birth (spina bifida); pigmented spots, hairy patches, deep pits Spina bifida Congenital defects in the lumbar spinal column caused by imperfect union of vertebral parts Meningomyelocele: protrusion of the spinal cord and meninges through a defect in the vertebral arch of one or more vertebrae (worst kind of spina bifida) Hip Thomas Test Bend one leg knee to chest and keep opposite leg straight; abnormality would be the opposite leg shifting to compensate-indicates a hip issue Patrick Test With patient supine, position heel of right foot on the left knee, and lower the right leg to the table with modified pressure-inability to lower leg or pain in lower back or inguinal area are indicative of osteoarthritis Straight leg raise Have patient sit or lay supine and raise one leg; positive results will be movement in the contra-lateral hip or the inability to lift leg (increased pain is indicative of a nerve impingement Abnormals Iliopectineal bursa Deep to the iliopsoas Prevents friction from the joint capsule Trochanteric Bursitis Lateral hip pain near the greater trochanter Ischial Bursitis Inflammation of bursa at ischium, common in people who sit a lot o Knee Effusion milk fluid downward toward knee and tap lateral aspect; will see movement of patella Ballottement of the patella compress patellar pouch and push patella against femur; if positive, patella will displace fluid before reaching femur McMurray’s while standing on affected side, place one hand on the lateral side of the knee and hold the heel while flexing the knee and hip, internally rotate the knee while adding resistance to the lateral aspect of the knee and slowly extend the knee; a click is indicative of a meniscus tear Anterior drawer test with the knee flexed at 45*, grasp below the knee and pull towards you and then push away from you; tests for ACL tear or injury Lachman test flex the knee 20-30*, stabilize femur with one hand and place other hand around tibia, then pull the tibia anteriorly; laxity (lack of a solid or firm end point) indicates ACL injury or tear Pivot shift pt lying in the lateral decubitus position, have the affected knee extended with the hip at 20-30* flexion and the tibia internally rotated, apply a valgus stress to the knee as you flex it medially; a positive test-a clunk at about 30* or a jump as you are manipulating the knee Valgus varus stress – tests the MCL stabilize the femur with the knee at full extension or flex the knee at 25*; apply valgus (outward) pressure at the foot/ankle and then apply varus (inward) pressure at the foot/ankle; valgus laxity is indicative of medial collateral ligament, varus laxity is indicative of lateral collateral ligament Grading of laxity 1+ 5mm of medial joint space opening 2+ 10mm medial opening 3+ 15mm medial opening 4+ 20mm medial opening; may be indicative of an associated cruciate ligament injury and must be carefully examined Bulge Test Test to assess for swelling in the supra patellar pouch (fluid in the knee) Tap on one side and you will see a wave of fluid to the other side Knee Abnormals o Osgood-Schlatter disease anterior tuberosity pain r/t age Common cause of knee pain in growing adolescents Inflammation where the patellar tendon attaches to the tibial tubercle Occurs because growth plate is cartilage and the quads pull on the tubercle repetitively causing inflammation Running and jumping increases risk Prominence of a bump can develop over time Swelling at tibial tubercle Tight thigh muscles posteriorly and anteriorly Even if you suspect Osgood-Schlatter’s disease you should still get an x-ray of the knee o Genu valgum Knock knees Condition in which the knees touch but the ankles do not o o o Can be normal in children up to age 3 Locking episodes of knees Meniscus tear (memory tip: lock the men up) Pop, lock and drop it- ligament, meniscus, instability o "popping" sound, ligament o knee "gives out", instability Oxford knee questionnaire: higher score = higher likelihood for knee replacement Ankle/Foot Shelf test support ankle with one hand and grab the calcaneus with the other; apply anterior force to calcaneus; laxity indicated ankle instability Ankle flexion (plantar flexion)-have patient point their foot toward the floor Ankle extension (dorsiflexion)- have patient point their foot toward the ceiling Inversion- have patient turn their heel medially Eversion- have patient turn their heel laterally Objective: Understand the differences between OA, gout, and RA Osteoarthritis: caused by general wear-and-tear of the joints and a loss of the protective tissues that act as padding between the bones of each joint; worse in the evening; can be in any joint (shoulder, elbow, hip, Knee); abnormal assessment findings-very hard and bony; Heberden’s (distal phalangeal joint), Bouchard’s (proximal phalangeal joint); cartilage destruction Gout: caused by crystallization of uric acid in distal areas of the body (metatarsal joints, metacarpal joints, ears, etc.) Rheumatoid arthritis: familial component; is an autoimmune disorder; pain is worse in the morning; abnormal assessment findings-very boggy joints that are painful to touch, swan neck deformity (5th finger), Boutonniere deformity (index finger); inflamed synovial membrane Objective: Review risk factors for osteoporosis o Caucasian or Asian women o small/thin frame o positive family history for adult fractures (1st degree relative) o menopause (especially if early or surgically induced) o chronic illnesses o amenorrhea o low life-time calcium intake o anorexia o impaired GI absorption o smoking, alcohol consumption o low testosterone levels in men o use of certain medications (corticosteroids, chemotherapy, anticonvulsants and others) o lack of impact exercise (leads to maintaining the density of the bone) Screening guidelines o Women 65+ o Younger women with increased fracture risk