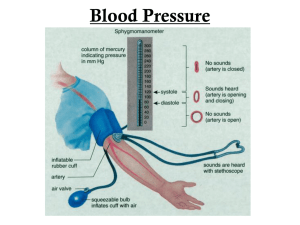
Chapter 23 Med Surge Summer Exam 3 Coronary Artery Disease: CAD Is the most prevalent type of cardiovascular disease in adult Coronary Atherosclerosis: Most common cause of cardiovascular disease Is an abnormal accumulation of lip or fatty substances, and fibrous tissue in the lining of arterial blood vessels walls Block/narrow the coronary vessels and reduces blood flow to the myocardium Involves a repetitious inflammatory response to injury of the artery wall and alteration in the structural/biochemical properties of the arterial walls Pathophysiology: Inflammatory response involved w/the development of atherosclerosis begins w/injury to the vascular endothelium and progresses over may years May be initiated by smoking/tobacco use, HTN, hyperlipidemia Endothelium stops producing the normal antithrombotic and vasodilating agents Heart disease is most often caused by atherosclerosis Clinical Manifestations: CAD produces symptoms/complications according to the location/degree of narrowing of the arterial lumen, thrombus formation, and obstruction of blood flow to the myocardium Impediment to blood flow is usually progressive, causing inadequate blood supply that deprives cardiac muscle cells of oxygen Ischemia Angina Pectoris = chest pain that is brought by myocardial ischemia o Usually is caused by significant coronary atherosclerosis A decrease in blood supply from the CAD may cause the heart to abruptly stop beating = sudden cardiac death Most common manifestation of myocardial ischemia: o Onset of chest pain o Unstable angina, MI, sudden cardiac death events o HX of diabetes or heat failure, SOB, indigestion, nausea, palpitations, numbness o A major cardiac even may be the first indication of coronary atherosclerosis o Angina may present a few hours/days before an acute episode Risk Factors: Elevated LDL Diabetes Peripheral arterial disease Abdominal aortic aneurysm Carotid artery disease Age, gender, systolic blood pressure, smoking history, level of total cholesterol, and level of HDL Metabolic syndrome o Enlarged waist circumference (greater than 35.4 (M) 31.4 (F) o Elevated triglycerides (> or = to 175mg/dL) o Reduced HDL (<40mg/dL (M), <50mg/dL (F)) o Hypertension (systolic > 130 and/or diastolic > or = to 80 on average of 2-3 measurements on 2-3 separate occasions) o Elevated fasting glucose (> or = to 100 on 2 separate occasions) o Type 2 diabetes Nonmodifiable Risk Factors o Family HX of CAD (1st degree relative) o Increasing age o Gender o HX of premature menopause (before 40) history of pregnancy-associated disorders (preeclampsia) o Primary hypercholesterolemia (elevated LDL) Modifiable Risk Factors o Hyperlipidemia o Tobacco use o Hypertension o Diabetes o Metabolic syndrome o Obesity o Physical inactivity o Chronic inflammatory conditions (RA, lupus, HIV/AIDS) o Chronic kidney disease Prevention: 4 modifiable risk factors o Cholesterol, tobacco, hypertension, diabetes Cholesterol lowering dietary changes o Mediterranean diet o Increased consumption of fruits, vegetables, whole-grains, beans, nuts, and seeds o Limit sweets/sugar sweetened beverages o Vegetarian diet Physical Activity o Regular moderate physical activity o Moderate aerobic activity of at least 150min per week or vigorous aerobic activity at least 75min per week or combination of the two Medications o Statins, fibric acids (fibrates), bile acid sequestrants (resins), cholesterol absorption inhibitors, and proprotein convertase subtilisin-kexin type 9 (PCSK9) Tobacco use o Nicotinic acid raise HR/BP, coronary artery constriction o Increase oxidation of LDL (higher probability of thrombus formation) o Inhalation of smoke increased the blood carbon monoxide levels decreasing the supply of oxygen HTN o Systolic greater than 130 and diastolic greater than 80 o Cardiovascular disease increases as BP increases Diabetes o Known to accelerate the development of heart disease o Hyperglycemia fosters dyslipidemia (increased platelet aggregation) and altered red blood cell function which can lead to thrombus formation o Insulin, metformin can lead to improved endothelial function/outcomes Angina Pectoris: Clinical syndrome usually characterized by episodes/paroxysm of pain or pressure in the anterior chest Cause is insufficient coronary blood flow, decreased oxygen supply when there is increased myocardial demand for oxygen in response to physical exertion or emotional stress o Need for oxygen exceeds supply Usually caused by atherosclerotic disease and obstruction of at least one major artery Angina pain factors o Physical exertion o Exposure to cold o Eating a heavy meal o Stress or any emotion-provoking situation Clinical manifestations: Mild indigestion to choking or heavy sensation on the upper chest Severity ranges from discomfort to agonizing pain Pain may be accompanied by severe apprehension and a feeling of impending death Felt deep in the chest behind the sternum (retrosternal area) Pain/discomfort is poorly localized, may radiate to the neck, jaw, shoulders, and inner upper arms, usually the left arm Patient w/diabetes may not have severe pain w/angina due to autonomic neuropathy Feeling of weakness/numbness in the arms/wrists/hands w/SOB , pallor, diaphoresis, dizziness or lightheadedness, nausea/vomiting (may occur) Pain subsides w/rest or admin of nitroglycerin Unstable angina increase in frequency/severity and are not relieved by rest and nitroglycerin admin. (require medical intervention) Gerontologic: Older adults may not exhibit typical pain profile due to diminished pain transmission Presenting symptom in older adults is dyspnea Sometimes no symptoms present (“silent” CAD) Should recognize chest pain-like symptom (weakness) as a sign to rest or take prescribed meds Pharmacologic stress testing and cardiac catheterization may be used to diagnose CAD in older patients Assessment/Diagnostic Findings: Begins w/patient’s history related to the clinical manifestations of ischemia 12-lead ECG shows changes indicative of ischemia (T wave inversion, ST segment elevation or abnormal Q wave) Labs: cardiac biomarker testing to rule out ACS Exercise or pharmacologic stress test Nuclear scan or invasive cardiac catheterization, coronary angiography Medical management: objective is to decrease the oxygen demand of the myocardium and to increase the oxygen supply Pharmacologic Therapy: Nitroglycerin o Nitrates are standard treatment for angina pectoris o Is a potent vasodilator (improves blood flow to heart muscles/relieves pain) o Dilates the veins and lesser extent the arteries o Dilation of the veins causes pooling of blood throughout the body Less blood returns to the heart preload is reduced o Relax systemic arteriolar bed, lowering BP and decreasing afterload Decrease myocardial oxygen requirements Equalizes supply/demand o Routes: oral, topical, sublingual, IV Beta-Adrenergic Blocking Agents o Metoprolol reduce myocardial oxygen consumption by blocking beta-adrenergic sympathetic stimulation to the heart o Reduction of HR, slowed conduction of impulses, decreased BP, reduced myocardial contractility (force of contraction) and amount of oxygen available (supply) o Helps control chest pain/delays onset of ischemia during work or exercise o Reduce the incidence of recurrent angina, infarction, and cardiac mortality o Side effects/contraindications Hypotension, bradycardia, advanced atrioventricular block, acute heart failure Depressed mood, fatigue, decreased libido, dizziness If Given IV MX ECD/BP/HR Calcium Channel Blocking Agents: Decrease sinoatrial node automaticity/atrioventricular node conduction o Slower HR/decrease in strength of myocardial contraction (negative inotropic effect) Increase myocardial oxygen supply by dilating smooth muscle wall of the coronary arterioles Decrease myocardial oxygen demand by reducing systemic arterial pressure and workload of the left ventricle Most common o Amlodipine and diltiazem o Used for angina and hypertension ACS (acute coronary syndrome): is an emergent situation characterized by an acute onset of myocardial ischemia that results in myocardial death (MI) if interventions do not occur promptly Pathophysiology o Unstable angina Reduced blood flow in a coronary artery – rupture of an atherosclerotic plaque Clot begins to form on top of the coronary lesion (artery not completely occluded) Can result in chest pain/other symptoms (preinfarction angina) Patient will have an MI if prompt interventions do not occur o MI Plaque rupture/subsequent thrombus formation result in complete occlusion of the artery Leading to ischemia and necrosis of the myocardium supplied by the artery Vasospasm (sudden constriction/narrowing) of a coronary artery, decreased oxygen supply (acute blood loss, anemia or low BP), increased demand for oxygen (rapid HR, thyrotoxicosis, ingestion of cocaine), are other causes of MI A profound imbalance exist between myocardial oxygen supply and demand o Area of infarction develops over minutes to hours o “Time is muscle” reflects the urgency of appropriate treatment to improve patient outcomes o Descriptions used for MI ID NSTEMI, STEMI, location (anterior, inferior, posterior, or lateral wall), point in time w/in the process of infarction (acute, evolving, or old) Differentiation between NSTEMI AND STEMI is determined by diagnostic tests 12-lead ECG IDs the type/location of the MI Q wave, patient history, identify timing o Goals are to relieve symptoms, prevent or minimize myocardial tissue death, and prevent complications Manifestations o Chest pain that occurs suddenly/continues despite rest/meds o SOB, indigestion, nausea, anxiety, cool, pale and moist skin o HR/RR may be increased Assessment/Diagnostic Findings o Is generally based on the presenting symptoms 12-lead ECD/labs (serial cardiac biomarkers) used to clarify if patient has unstable angina, NSTEMI, or STEMI Prognosis depends on the severity of coronary artery obstruction and the presence/extent of myocardial damage Physical exam is always conducted o Cardiac enzymes/biomarkers Troponin, creatine kinase (CK), myoglobin Used to diagnose an acute MI Troponin regulates the myocardial contractile process (C, I, T) Increased troponin levels can be detected w/in a few hours during acute MI, remains elevated for as long as 2 weeks o Levels may rise w/inflammation/other mechanical stress on the myocardium (sepsis, HF, resp. failure) o Patient history Description of the presenting symptoms, history of previous cardiac/other illnesses, family history of heart disease, and risk factors for heart disease Treatment Guidelines for Acute MI: Use rapid transit to the hospital obtain 12 lead electrocardiogram to be read within 10 minutes obtain laboratory blood specimens of cardiac biomarkers including troponin obtain other diagnostics to clarify the diagnosis began routine medical interventions o supplemental oxygen o nitroglycerin o morphine o aspirin o beta blocker o angiotensin converting enzyme inhibitor within 24 hours o Statin evaluate for indications for reperfusion therapy: o percutaneous coronary intervention o thrombolytic therapy continue therapy as indicated o Ivy heparin, low-molecular-wait heparin, bivalirudin, or fondapariunux o Clopidogrel o Bed Rest for a minimum of 12 to 24 hours o statin prescribed at discharge S/S: MI Angina Pectoris or MI: Areas of Damage: MI Percutaneous Coronary Interventions: PTCA – percutaneous transluminal coronary angioplasty A balloon tip catheter is used to open blocked coronary vessels and resolve ischemia it is used in patients with angina and as an intervention for ACS catheter based interventions can also be used to open blocked CABGs let's see purpose is to improve blood flow within the coronary artery by compressing the atheroma PTCA Is carried out in the cardiac catheterization laboratory hollow catheters called sheaths are inserted usually in the femoral or radial artery Providing the conduit for other catheters angiography is performed using injected radiopaque contrast agents commonly called dye to identify the location extent of the blockage a balloon tip dilation catheter is passed through the sheath and positioned over the lesion the balloon is then inflated with high pressure for several seconds and then deflated o this pressure compresses and often cracks the atheroma o Several inflations of balloons of different sizes may be needed to achieve the goal of improved blood flow Intracoronary stents are usually positioned in the intima of the vessel to maintain patency of the artery after the balloon is withdrawn Coronary Artery Stents: After PTCA the area that has been treated may close off partially or completely - a process called restenosis The intima of the coronary artery has been injured and responds by initiating an acute inflammatory process process may include release of mediators that leads to vasoconstriction, clotting, and scar tissue formation o a coronary artery stent may be placed to overcome these risks a stent is a metal mesh that provides structural support to a vessel at risk of acute closure o the stent is initially positioned over the angioplasty balloon o when the balloon is inflated the mesh expands and presses against the vessel wall holding the artery open o the balloon is withdrawn but the stent is left permanently in place within the artery o endothelium covers the stent and is incorporated into the vessel wall Complications: Complications during a PCI procedure include coronary artery dissection, perforation, abrupt closure, or vasospasm o acute MI, serious arrhythmias (ventricular tachycardia), and cardiac arrest o some complications may require emergency surgical treatment complications after the procedure may include abrupt closure of the coronary artery and a variety of vascular complications such as bleeding at the insertion site, retroperitoneal bleeding, hematoma and arterial occlusion o Additionally there is a risk of acute kidney injury from the contrast agent used during the procedure Post Procedure Care: Patients who are not already hospitalized are admitted the day of the PCI o if no complications arise patient can go home the same day when the PCI is performed emergently to treat ACS patients typically go to a critical care unit and stay in the hospital for a few days during the PCO patients receive Ivy heparin or a thrombin inhibitor and are monitored closely for signs of bleeding help me your stasis is achieved and femoral sheaths may be removed at the end of the procedure by using a vascular closure device or a device that sutures the vessels o homeostasis after sheath removal may also be achieved by direct manual pressure, and mechanical compression device, or a pneumatic compression device patients may return to the nursing unit with a large peripheral vascular access sheath in place the sheets are then removed after blood studies (activated clotting time) indicate that the heparin is no longer active and the clotting time is within an acceptable range o this usually takes a few hours depending on the amount of heparin given during the procedure o the patient must remain flat in bed and keep the affected leg straight until the sheets are removed and then for a few hours afterward to maintain homeostasis o she's removal and the application of pressure on the vessel insertion site may cause the heart rate to slow and the blood pressure to decrease (vasovagal response) a dose of IV atropine is usually given to treat this response o after homeostasis is achieved, a pressure dressing is applied to the site patients resumed self-care and ambulate unassisted within a few hours of the procedure coronary artery revascularization: coronary artery bypass graft (CABG) is a surgical procedure in which a blood vessel is grafted to an occluded coronary artery so that blood can flow beyond the occlusion; it is also called a bypass graft o major indications for CABG alleviation of angina that cannot be controlled with medication or PCI treatment for left main coronary artery stenosis or multivessel CAD prevention of and treatment for MI, arrhythmias, or heart failure treatment for complications from an unsuccessful PCI o the recommendation for CABG it's determined by the number of disease coronary vessels, the degree of left ventricular dysfunction, the presence of other health problems, the patient symptoms and any previous treatment o CABG is performed less frequently in women compared to men for a patient to be considered for CABG the coronary arteries to be bypassed must have at least a 70% occlusion or at least 50% occlusion in the left main coronary artery o if the blockage is not significant flow through the artery will compete with flow through the bypass and circulation to the ischemic area of myocardium may not improve CABG procedures are performed with the patient under general anesthesia o the surgeon performs a median sternotomy and connects the patient to the cardiopulmonary bypass machine o a blood vessel from another part of the patients body is grafted distal to the coronary artery lesion, bypassing the obstruction o CPB is then disconnected, chest tubes and epicardial pacing wires are placed, and the incision is closed o patient is then admitted to the critical care unit Cardiopulmonary Bypass: CPB maintains perfusion to body organs and tissues and allows the surgeon to complete the anastomoses in a motionless, bloodless surgical field CPB is accomplished by placing the cannula in the right atrium, vena cava, or femoral vein to withdraw blood from the body o the cannula is connected to tubing filled with an isotonic crystalloid solution o venous blood removed from the body by the cannula is filtered, oxygenated, cooled or warmed by the machine, and then return to the body o the cannula used to return the oxygenated blood is usually inserted in the ascending aorta, or it may be inserted in the femoral artery o the hardest stop by the injection of a potassium rich cardioplegia solution into the coronary arteries o the patient receives heparin to clotting and thrombus formation in the bypass circuit when blood comes in contact with the surfaces of the tubing o at the end of the procedure when the patient is disconnected from the bypass machine, protamine sulfates is given to reverse the effects of heparin o during the procedure, hypothermia is maintained at a temperature about 82.4◦F patients are frequently admitted to the hospital the day of the procedure nursing and medical personnel perform a history and physical examination o preoperative testing consists of a chest X ray; ECG; laboratory tests, including coagulation studies; And blood typing and crossmatching health assessment focuses on obtaining baseline physiologic, psychological, and social information o cognitive status is carefully assessed, as patients with impaired cognitive status will need more assistance after surgery and may require sub acute care prior to returning home o the patient usual functional level, coping mechanisms, and available support systems, affect the patient post operative course, discharge plans, and rehabilitation o status of the cardiovascular system is determined by reviewing the patient symptoms, including past and present experiences with chest pain, palpitations, dyspnea, intermittent claudication and peripheral edema initial postoperative care focuses on achieving or maintaining hemodynamic stability and recovery from general anesthesia o care may be provided in the post anesthesia care unit (PACU) or ICU when the patient is admitted to the critical care unit or PACU, a complete assessment of all systems are done at least every four hours o Nora logical status: level of responsiveness, pupil size and reaction to light, facial symmetry comment movement of the extremities, and hand grip strength o cardiac status: heart rate and rhythm, heart sounds, pacemaker status, arterial blood pressure, central venous pressure; in some patients hemodynamic parameters: pulmonary artery pressure, pulmonary artery wedge pressure, cardiac output and index, systemic and pulmonary vascular resistance, mixed venous oxygen saturation a pulmonary catheter is often used to monitor these parameters o respiratory status: chest movement, breast sounds, ventilator settings, respiratory rate, peak inspiratory , percutaneous oxygen saturation, intitle carbon dioxide, pleural chest tube drainage, arterial blood gases o peripheral vascular status, peripheral pulses (color of skin, nailbeds, mucus, lips, and earlobes) skin temperature, edema, condition of dressings and invasive lines o renal function: urinary output, serum creatinine and electrolytes o fluid and electrolytes status: strict intake and output, including all IV fluids and blood products, output from all drainage tubes, clinical and laboratory indicators of imbalance o pain: nature, type, location, and duration, apprehension, response to analgesics assessment also includes checking all equipment and tubes to ensure that they are functioning properly as the patient regains consciousness and progresses through the post operative period The nurse also assesses indicators of psychosocial and emotional status family needs must be assessed, the nurse ascertains how family members are coping with the situation, determines their psychosocial, emotional, and spiritual needs, and finds out whether they are receiving adequate information about the patient's condition decrease cardiac output is always a threat two patients who have received cardiac surgery o excessive post operative bleeding can lead to decreased intravascular volume, hypo tension, and low cardiac outputs o bleeding problems are common after cardiac surgery because of the facts of CPB, trauma from the surgery, and anticoagulation preload can also decrease if there is a collection of fluid and blood in the pericardium, which impedes cardiac filling cardiac output is also altered if too much volume returns to the heart, causing fluid overload o afterload alterations occur when the arteries are constricted as a result of postoperative hypertension or hypothermia, increasing the workload of the heart possible complications after cardiac surgery o fluid volume and electrolyte imbalances o impaired gas exchange o decrease cardiac output o impaired cerebral circulation