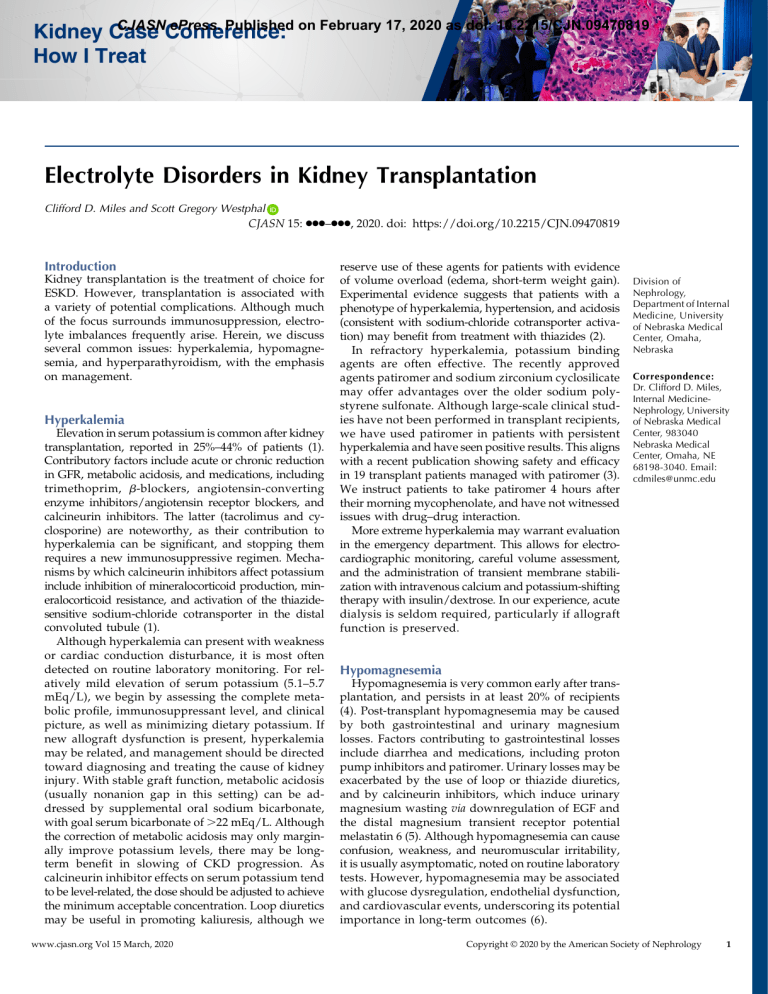
CJASN ePress. Published on February 17, 2020 as doi: 10.2215/CJN.09470819 Kidney Case Conference: How I Treat Electrolyte Disorders in Kidney Transplantation Clifford D. Miles and Scott Gregory Westphal CJASN 15: ccc–ccc, 2020. doi: https://doi.org/10.2215/CJN.09470819 Introduction Kidney transplantation is the treatment of choice for ESKD. However, transplantation is associated with a variety of potential complications. Although much of the focus surrounds immunosuppression, electrolyte imbalances frequently arise. Herein, we discuss several common issues: hyperkalemia, hypomagnesemia, and hyperparathyroidism, with the emphasis on management. Hyperkalemia Elevation in serum potassium is common after kidney transplantation, reported in 25%–44% of patients (1). Contributory factors include acute or chronic reduction in GFR, metabolic acidosis, and medications, including trimethoprim, b-blockers, angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, and calcineurin inhibitors. The latter (tacrolimus and cyclosporine) are noteworthy, as their contribution to hyperkalemia can be significant, and stopping them requires a new immunosuppressive regimen. Mechanisms by which calcineurin inhibitors affect potassium include inhibition of mineralocorticoid production, mineralocorticoid resistance, and activation of the thiazidesensitive sodium-chloride cotransporter in the distal convoluted tubule (1). Although hyperkalemia can present with weakness or cardiac conduction disturbance, it is most often detected on routine laboratory monitoring. For relatively mild elevation of serum potassium (5.1–5.7 mEq/L), we begin by assessing the complete metabolic profile, immunosuppressant level, and clinical picture, as well as minimizing dietary potassium. If new allograft dysfunction is present, hyperkalemia may be related, and management should be directed toward diagnosing and treating the cause of kidney injury. With stable graft function, metabolic acidosis (usually nonanion gap in this setting) can be addressed by supplemental oral sodium bicarbonate, with goal serum bicarbonate of .22 mEq/L. Although the correction of metabolic acidosis may only marginally improve potassium levels, there may be longterm benefit in slowing of CKD progression. As calcineurin inhibitor effects on serum potassium tend to be level-related, the dose should be adjusted to achieve the minimum acceptable concentration. Loop diuretics may be useful in promoting kaliuresis, although we www.cjasn.org Vol 15 March, 2020 reserve use of these agents for patients with evidence of volume overload (edema, short-term weight gain). Experimental evidence suggests that patients with a phenotype of hyperkalemia, hypertension, and acidosis (consistent with sodium-chloride cotransporter activation) may benefit from treatment with thiazides (2). In refractory hyperkalemia, potassium binding agents are often effective. The recently approved agents patiromer and sodium zirconium cyclosilicate may offer advantages over the older sodium polystyrene sulfonate. Although large-scale clinical studies have not been performed in transplant recipients, we have used patiromer in patients with persistent hyperkalemia and have seen positive results. This aligns with a recent publication showing safety and efficacy in 19 transplant patients managed with patiromer (3). We instruct patients to take patiromer 4 hours after their morning mycophenolate, and have not witnessed issues with drug–drug interaction. More extreme hyperkalemia may warrant evaluation in the emergency department. This allows for electrocardiographic monitoring, careful volume assessment, and the administration of transient membrane stabilization with intravenous calcium and potassium-shifting therapy with insulin/dextrose. In our experience, acute dialysis is seldom required, particularly if allograft function is preserved. Division of Nephrology, Department of Internal Medicine, University of Nebraska Medical Center, Omaha, Nebraska Correspondence: Dr. Clifford D. Miles, Internal MedicineNephrology, University of Nebraska Medical Center, 983040 Nebraska Medical Center, Omaha, NE 68198-3040. Email: cdmiles@unmc.edu Hypomagnesemia Hypomagnesemia is very common early after transplantation, and persists in at least 20% of recipients (4). Post-transplant hypomagnesemia may be caused by both gastrointestinal and urinary magnesium losses. Factors contributing to gastrointestinal losses include diarrhea and medications, including proton pump inhibitors and patiromer. Urinary losses may be exacerbated by the use of loop or thiazide diuretics, and by calcineurin inhibitors, which induce urinary magnesium wasting via downregulation of EGF and the distal magnesium transient receptor potential melastatin 6 (5). Although hypomagnesemia can cause confusion, weakness, and neuromuscular irritability, it is usually asymptomatic, noted on routine laboratory tests. However, hypomagnesemia may be associated with glucose dysregulation, endothelial dysfunction, and cardiovascular events, underscoring its potential importance in long-term outcomes (6). Copyright © 2020 by the American Society of Nephrology 1 2 CJASN Unfortunately, hypomagnesemia tends to be difficult to correct. Our algorithm starts with dietary modification and oral supplementation with magnesium oxide. Some patients require titration up to 800 mg twice daily, although diarrhea is a frequent dose-limiting side effect. Magnesium chloride is another oral preparation that may be better tolerated, although neither in our experience will reliably increase serum magnesium into the normal range. As with hyperkalemia, it is prudent to ensure immunosuppressant levels are appropriate. The need for loop or thiazide diuretics and proton pump inhibitors should be reviewed, and alternatives considered if appropriate, although thiazideinduced magnesium wasting may be blunted in patients on calcineurin inhibitors (2). We have had success used amiloride, the potassium (and magnesium)-sparing diuretic. It tends to be well tolerated, and we usually administer it while continuing magnesium supplementation. Clearly, one needs to be cognizant of the effect on potassium levels. Post-Transplant Hyperparathyroidism Disorders in bone-mineral metabolism, including hyperparathyroidism, are common in patients with ESKD. After transplantation, restoration of kidney function generally corrects the stimuli for hyperparathyroidism, including hyperphosphatemia and hypovitaminosis D, resulting in the return of autoregulation of parathyroid hormone (PTH) secretion. However, parathyroid regression is frequently incomplete, resulting in persistent post-transplant hyperparathyroidism. The functional allograft responds to elevated PTH and fibroblast growth factor-23 (FGF-23) with hyperphosphaturia, resulting in hypophosphatemia. Likewise, post-transplant hypercalcemia develops in response to persistently elevated PTH, reduced skeletal resistance to PTH, and increasing active vitamin D levels. Hypercalcemia and hypophosphatemia develop in approximately 50% of transplant recipients, often most pronounced 2–8 weeks after transplantation (7). Although FGF-23 levels fall quickly, hyperparathyroidism frequently persists, with .85% of recipients having elevated PTH levels 1 year after transplantation. Persistent post-transplant hyperparathyroidism is associated with an increased risk of acute kidney allograft injury, graft loss, fractures, and mortality (8). When hypercalcemia develops, medications that increase serum calcium should be discontinued, including vitamin D analogs, calcium supplements, calcium-based phosphate binders, and thiazide diuretics. Patients should maintain adequate solute and water intake to avoid volume depletion, which can exacerbate hypercalcemia through increased kidney absorption. Post-transplant hypercalcemia is often mild and self-limited; however, when hypercalcemia is severe or prolonged, additional interventions may be warranted. Before calcimimetics, parathyroidectomy was often the only therapy to provide a durable response to hypercalcemia caused by post-transplant hyperparathyroidism. However, with the availability of cinacalcet, this alternative to surgical parathyroidectomy is now widely utilized. In a recent randomized trial, parathyroidectomy was compared with cinacalcet for the treatment of post-transplant hyperparathyroidism (9). All patients treated with parathyroidectomy achieved normocalcemia versus 67% of those treated with cinacalcet, and the PTH reduction was greater in the surgical group. Parathyroidectomy was associated with an improvement in femoral neck bone mineral density with no improvement observed in the cinacalcet group. An economic analysis estimated that the cost of parathyroidectomy was equivalent to 14 months of cinacalcet. There are, however, reasons to avoid surgery, including patient choice, specific surgical risk factors, and the desire to avoid early short-term risk from the transplant program’s standpoint. For such reasons, calcimimetics are being used with increasing frequency, especially in the early post-transplant period, to avoid or delay parathyroidectomy. In a randomized, controlled trial in patients with hypercalcemia attributed to post-transplant hyperparathyroidism, 79% of patients treated with cinacalcet achieved normocalcemia compared with just 4% given placebo (10). PTH in cinacalcet-treated patients dropped significantly and phosphorus normalized, whereas there was minimal change in the placebo group. However, treatment with cinacalcet did not improve clinical outcomes such as bone density, allograft function, or allograft/patient survival. Further, after cinacalcet discontinuation, calcium returned toward pretreatment levels, as did phosphorus and PTH, suggesting that cinacalcet did not facilitate involution of parathyroid hyperplasia. At our center, we attempt to avoid parathyroidectomy when possible, particularly within the first post-transplant year, as some patients will develop at least partial resolution of hypercalcemia. We initiate cinacalcet in patients with moderate hypercalcemia (.11.0 mg/dl), particularly if graft dysfunction or symptoms are present. We start cinacalcet at 30 mg daily, and titrate as tolerated to achieve normocalcemia. Gastrointestinal side effects and cost can be barriers to use and dose escalation. We subsequently attempt to wean cinacalcet after the first transplant year. If hypercalcemia redevelops as cinacalcet is weaned, we discuss the risks and benefits of parathyroidectomy compared with remaining on cinacalcet indefinitely. We consider earlier parathyroidectomy in patients with refractory hypercalcemia that cannot be managed with cinacalcet because of cost, side effects, or ineffectiveness. Although cinacalcet often raises serum phosphate, maintaining normal phosphate levels can be challenging in the early post-transplant period, particularly in those with good allograft function. Fortunately, significant symptoms rarely develop until phosphorus is ,1.0 mg/dl. Mild hypophosphatemia can often be managed through increased dietary intake (e.g., dairy products). When phosphorus levels drop below 1.8 mg/dl, we initiate oral neutral phosphorus salt supplementation. We generally do not titrate the dose above 500 mg two times per day even if phosphorus levels remain low, as excessive supplementation can stimulate PTH and FGF-23, enhancing phosphaturia. Summary Disturbances of potassium, magnesium, and calcium/ phosphorus are common after kidney transplantation, and deserve careful management. Serial laboratory assessment of these electrolytes is central to titration of supplements and other interventions. As a word of CJASN 15: ccc–ccc, March, 2020 caution, the steps we have described here may lead to significant increase in pill burden, as these disorders often coexist. The potential effect on quality of life and adherence to immunosuppressive medications should be borne in mind. Disclosures Dr. Miles and Dr. Westphal have nothing to disclose. References 1. Pochineni V, Rondon-Berrios H: Electrolyte and acid-base disorders in the renal transplant recipient. Front Med (Lausanne) 5: 261, 2018 2. Hoorn EJ, Walsh SB, McCormick JA, Fürstenberg A, Yang CL, Roeschel T, Paliege A, Howie AJ, Conley J, Bachmann S, Unwin RJ, Ellison DH: The calcineurin inhibitor tacrolimus activates the renal sodium chloride cotransporter to cause hypertension. Nat Med 17: 1304–1309, 2011 3. Lim MA, Sawinski D, Trofe-Clark J: Safety, effectiveness, and tolerability of patiromer in kidney transplant recipients. Transplantation 103: e281–e282, 2019 4. De Waele L, Van Gaal PJ, Abramowicz D: Electrolytes disturbances after kidney transplantation. Acta Clin Belg 74: 48–52, 2019 Electrolyte Disorders in Kidney Transplantation, Miles and Westphal 3 5. Van Laecke S, Van Biesen W: Hypomagnesaemia in kidney transplantation. Transplant Rev (Orlando) 29: 154–160, 2015 6. Sinangil A, Celik V, Barlas S, Sakaci T, Koc Y, Basturk T, Akin EB, Ecder T: New-onset diabetes after kidney transplantation and pretransplant hypomagnesemia. Prog Transplant 26: 55–61, 2016 7. Wolf M, Weir MR, Kopyt N, Mannon RB, Von Visger J, Deng H, Yue S, Vincenti F: A prospective cohort study of mineral metabolism after kidney transplantation. Transplantation 100: 184–193, 2016 8. Pihlstrøm H, Dahle DO, Mjøen G, Pilz S, März W, Abedini S, Holme I, Fellström B, Jardine AG, Holdaas H: Increased risk of all-cause mortalityand renal graft loss in stable renal transplant recipients with hyperparathyroidism. Transplantation 99: 351–359, 2015 9. Evenepoel P, Cooper K, Holdaas H, Messa P, Mourad G, Olgaard K, Rutkowski B, Schaefer H, Deng H, Torregrosa JV, Wuthrich RP, Yue S: A randomized study evaluating cinacalcet to treat hypercalcemia in renal transplant recipients with persistent hyperparathyroidism. Am J Transplant 14: 2545–2555, 2014 10. Cruzado JM, Moreno P, Torregrosa JV, Taco O, Mast R, GómezVaquero C, Polo C, Revuelta I, Francos J, Torras J, Garcı́a-Barrasa A, Bestard O, Grinyó JM: A randomized study comparing parathyroidectomy with cinacalcet for treating hypercalcemia in kidney allograft recipients with hyperparathyroidism. J Am Soc Nephrol 27: 2487–2494, 2016 Published online ahead of print. Publication date available at www.cjasn.org.