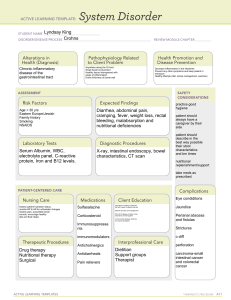
Canadian Jensen’s Nursing Health Assessment Abdominal Assessment Chapter Twenty-two Subjective Assessment Provide privacy Introduce yourself with your first and last name and designation o Hello, my name is Aaron Vale and I am a nursing student at the University of Windsor Clean your equipment Wash your hands Demographic Data Name, age, address, phone number, occupation, marital status, number of children If you ask the date and time this will be part of general survey (behaviour A & O x 4) Chief Concern – The reason they are seeking care “Tell me why you came to the clinic today” or “What brings you to the office today” What they tell you will direct the remainder of your questions. Questions must be relevant to their medical concerns. Past History of the Patient Surgeries including appendicitis, bowel resection, cholecystectomy, hysterectomy Injuries include trauma and work injuries RUQ- liver disease (cirrhosis), hepatitis A, B, C- Gerd, cholecystitis, gastric bypass LUQ- Splenectomy, DM, Pancreatitis or Pancreatic CA, mononucleosis, Renal colic, kidney disease RLQ- appendicitis, Celiac Disease, sickle cell disease LLQ Bowel cancer, bowel obstruction, IBD, Crohn’s, Colitis, polyps GU- Bladder cancer, STD’s, ovarian or uterus problems, enlarged prostate Family History Ask about relevant family history to the present complaint (abdomen). colorectal cancer (first degree relative), GERD, peptic ulcer disease, IBD, anemia/thalassemia (splenomegaly), Celiac disease, DM, pancreatic cancer, Crohn’s, sickle cell anemia, thyroid disease Degree Relatives first-degree relative- individual's parents, full siblings, or children second-degree relative- individual's grandparents, grandchildren, aunts, uncles, nephews, nieces or half-siblings third-degree relative- great grandparents, great grandchildren, first cousins o note they must be related by blood DADSPIES Diet – Consumption of food in the last 24 hours Special diet (example: vegetarian) Alcohol and Drugs – Liver Cirrhosis Heightened hepatitis risk due to possibly sharing needles Physical Exam – FOBT at 50 years old (Faecal occult blood test, used to detect colon cancer and other disease.) Last pap smear (a test carried out on a sample of cells from the cervix to check for abnormalities that may be indicative of cervical cancer.) Immunizations – Hepatitis and shingle vaccines Abdomen Specific Questions Changes in weight can indicate an eating disorder or cancer Number of sexual partners, increasing the risk for Sexually Transmitted Infections (STI) Blood transfusion prior to 1980, before 1980, they did not screen for HIV in donated blood Problems with chewing or swallowing Travel – Hepatitis A Human violence Because of the prevalence of abuse in our society nurses routinely screen for violence o “Within the past year, have you been hurt either physically, sexually, or emotionally by anyone?” O: when did the abdominal pain start? did it come on suddenly or gradual P: Does anything make your abdomen symptom better-? -medication, position, eating Does anything make it worse- Position, eating, meds (NSAIDS) Q: quality &/or quantity- how does it feel- sharp? Burning? Stabbing? Dull? R: Where is the pain located/is it anywhere else? Referred pain- see next slide S: 0-to-10 severity scale -activities of daily living (ADLs)? Can you prepare meals, go to work, bath etc. T: is it better or worse at a certain time of day, has there been a change, U: What do you think is wrong? Pain Visceral pain • hollow organs are distended, stretched, or contracted forcefully • may be difficult to localize • Described as gnawing, burning, cramping, or aching. • may be associated with sweating, pallor, nausea, vomiting, or restlessness Parietal pain • inflammation of the peritoneum • severe and localized over the involved structure • Described as steady, aching, or sharp, especially with movement Referred pain • occurs in more distant sites innervated at approximately the same spinal level as the disordered structure Associated symptoms GI (gastrointestinal) - nausea, vomiting (hematemesis) (describe), indigestion, anorexia, diarrhea (describe), fever, changes to skin colour (jaundice), unplanned changes in weight, Dysphagia (diff swallowing) and odynophagia (painful swallowing) Constipation or changes to bowel pattern (find out what is normal for the patient-Normal frequency ranges from 3 times a day to once a week GU (genital urinary) -change in urine (hematuria) (colour), dysuria (pain with urination) frequency, urgency, change in stream (males-prostate) Increased amount of urine with voiding (polyuria), Urination at night (nocturia), Loss of control of urine (urinary incontinence) (what type- next slide), flank or back (kidney) pain Vaginal (describe) if vaginal bleeding (? Menses- what age started, ? Monthly cycle, patternhow much bleeding Discharge from penis, scrotal pain, prostate concerns Urinary Incontinence Stress: • coughing, sneezing, or increasing intra-abdominal pressure Urge: • sudden urge and loss of continence with little warning Overflow: • continuous dribbling or dripping and weaker urinary stream Functional: • cannot get to toilet in time due to environ- mental factors or impaired health Total: • inability to retain urine; ask also about bowel incontinence • Older adults-considerations Decreased thirst drive/changes to bowel • Who gets your groceries & prepares meals? • What liquids do you have in 24 hrs & how much? • How much fibre is in your diet? • Describe your meals and snacks in the last 24 hours • Do you have any trouble swallowing? • How often do you move your bowels? Describe BM • Meds that may affect BM’s-laxatives, diuretics Objective Exam Preparation Environment should be warm enough & private Adequate lighting essential Have patient empty bladder before assessment Pt to lie supine with arms at sides, knees bent Drape patient appropriately If the head is flexed, the abdominal musculature becomes tensed and the examination made more difficult. Allowing the patient to bend their knees so that the soles of their feet rest on the table will also relax the abdomen. Exam points • Examine any painful areas last • Observe for signs of discomfort • Distract the patient to avoid tensing- make the assessment more difficult Objective Assessment - Inspection • Skin- condition/colour • Contour & Symmetry • Umbilicus- inverted/everted • Peristaltic waves • Pulsation • Any visible organs or masses • Unexpected findings – scars, striae, and veins; umbilical hernia, rashes, lesion • Deep breath and bear down – hernias or organomegaly Epigastric Pulsation AAA – Enlarged aorta (>3cm) or lateral pulsations • • Auscultate the Abdomen • Bowel sounds • Vascular sounds • Auscultate- 2 spots per quadrant • Start at ileocecal valve *** Bowel sounds- high-pitched gurgles or clicks Borborygmic (air through intestines)-stomach growling Vascular Sounds • Bruits – swishing sounds- turbulent blood flow from constriction of vessel – Bruit in hepatic area-liver cancer or alcohol hepatitis • Venous hums – soft-pitched humming noise – partial obstruction vessel-reduced flow to organ • Friction rubs – grating sounds that increase with inspiration- liver tumour, spleen infarction, peritoneal inflammation Objective Assessment - Percussion • determine organ size & tenderness • Detect any fluid, air or masses • Percuss -mid axilla to mid axilla, along costal margins down to supra pubic • Normally most of abdomen tympanic Percussion Expected• Tympanic-left upper quadrant (LUQ) (gastric bubble) • Tympanic- most of the abdomen-gas • Dullness- over organs, masses, or fluid- ascites, GI obstruction, pregnant uterus, and an ovarian tumour • dullness can be due to faeces Percuss-Kidney CVA • Blunt percussion-costovertebral angle CVA • Fingertip pressure may be enough • patient feels a perceptible but painless thud • Should be no pain