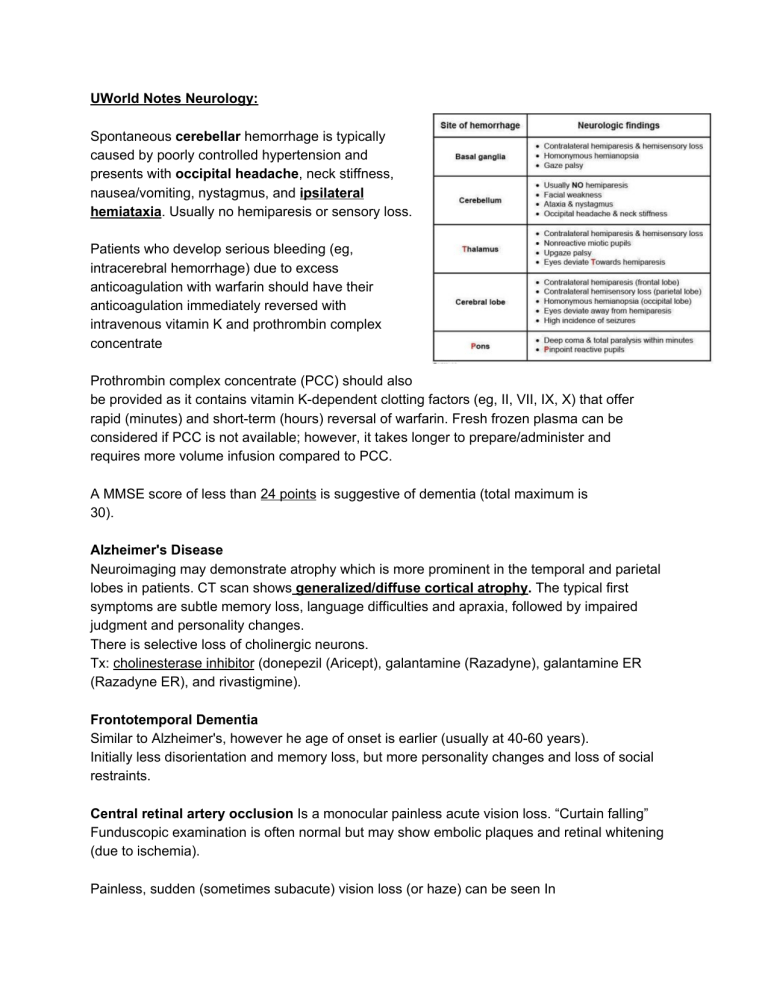
UWorld Notes Neurology: Spontaneous cerebellar hemorrhage is typically caused by poorly controlled hypertension and presents with occipital headache, neck stiffness, nausea/vomiting, nystagmus, and ipsilateral hemiataxia. Usually no hemiparesis or sensory loss. Patients who develop serious bleeding (eg, intracerebral hemorrhage) due to excess anticoagulation with warfarin should have their anticoagulation immediately reversed with intravenous vitamin K and prothrombin complex concentrate Prothrombin complex concentrate (PCC) should also be provided as it contains vitamin K-dependent clotting factors (eg, II, VII, IX, X) that offer rapid (minutes) and short-term (hours) reversal of warfarin. Fresh frozen plasma can be considered if PCC is not available; however, it takes longer to prepare/administer and requires more volume infusion compared to PCC. A MMSE score of less than 24 points is suggestive of dementia (total maximum is 30). Alzheimer's Disease Neuroimaging may demonstrate atrophy which is more prominent in the temporal and parietal lobes in patients. CT scan shows generalized/diffuse cortical atrophy. The typical first symptoms are subtle memory loss, language difficulties and apraxia, followed by impaired judgment and personality changes. There is selective loss of cholinergic neurons. Tx: cholinesterase inhibitor (donepezil (Aricept), galantamine (Razadyne), galantamine ER (Razadyne ER), and rivastigmine). Frontotemporal Dementia Similar to Alzheimer's, however he age of onset is earlier (usually at 40-60 years). Initially less disorientation and memory loss, but more personality changes and loss of social restraints. Central retinal artery occlusion Is a monocular painless acute vision loss. “Curtain falling” Funduscopic examination is often normal but may show embolic plaques and retinal whitening (due to ischemia). Painless, sudden (sometimes subacute) vision loss (or haze) can be seen In central retinal vein occlusion, likely from venous thrombosis. It can progress to an ischemic form that can be painful. Funduscopy usually reveals dilated and tortuous veins leading to scattered and diffuse hemorrhages ("blood and thunder"), disk swelling, and/or cotton wool spots. Detached retina typically have light flashes, floaters, or a curtain across their visual field. Parkinson’s: Amantadine is a dopamine agonist used in the treatment of Parkinson's Disease. DO NOT confuse with memantine which is used for moderate - severe dementia in Alzheimer’s. NPH: Gait impairment is the most prominent clinical feature of NPH and appears early in its course. The gait is broad-based and shuffling. Gait impairment is the most prominent early clinical feature of normal-pressure hydrocephalus but is a later finding in Alzheimer's dementia. Optic neuritis usually presents in women age <50 with monocular vision loss and pain on eye movement. Patients also typically have an afferent pupillary defect with optic disc swelling on fundoscopy. Aminoglycosides can cause ototoxicity (hearing loss) by damaging the cochlear cells. In addition, some aminoglycosides (especially gentamicin) can also damage the motion-sensitive hair cells in the inner ear to cause selective vestibular injury (vestibulopathy) with or without significant ototoxicity. An abnormal head thrust test can help detect vestibular dysfunction due to gentamicin. The patient is asked to look at a fixed target. Rapid head movement away from the target normally causes the eyes to remain fixed on the target. However, patients with vestibulopathy are unable to maintain their eyes on the target. The eyes move away and then return back to the target with a horizontal saccade. Infarction of the medial vermis of the cerebellum can cause severe vertigo and nystagmus. Lateral cerebellar infarction causes dizziness, ataxia, weakness, and a tendency to sway toward the side off the lesion. Meniere disease is due to excess endolymphatic fluid pressure in the inner ear that presents with the triad of episodic dizziness, low-frequency hearing loss, and tinnitus. can develop significant vertigo that lasts for days and is associated with nausea, vomiting, and horizontal-torsional nystagmus during an episode. Spasticity, bulbar symptoms, and exaggerated deep tendon reflexes are signs of upper motor neuron damage, while fasciculations indicate a lower motor neuron damage. Weakness and wasting of the muscles may be due to both upper and lower motor neuron lesions. Riluzole is a glutamate inhibitor that is currently approved for use in patients with amyotrophic lateral sclerosis. plasmapheresis and intravenous immunoglobulins are the main treatment modalities of Guillain-Barre syndrome. Phenytoin is a known teratogen capable of causing fetal hydantoin syndrome (eg, orofacial clefts, microcephaly, nail/digit hypoplasia, cardiac defects, dysmorphic facial features). Valproic acid is an antiepileptic drug that has been linked to an increased risk of congenital anomalies such as neural tube defects (eg, spina bifida) and dysmorphic facial features. Anterior cord syndrome is commonly associated with burst fracture of the vertebra and is characterized by total loss of motor function below the level of lesion with loss of pain and temperature on both sides below the lesion with intact proprioception. Central cord syndrome is characterized by burning pain and paralysis in upper extremities with relative sparing of lower extremities. It is commonly seen in elderly secondary to forced hyperextension type of injury to the neck. Acute disk prolapse will be characterized by severe radicular pain Lesions in the central nervous system occurring above the facial nucleus will typically cause a contralateral lower facial weakness that spares the forehead. It typically presents as bilateral leg weakness that ascends to the arms, respiratory muscles, and face to generalized flaccid paralysis. Distal paresthesias are common, but other sensory symptoms are uncommon or mild. Reflexes are diminished or absent. A utonomic disturbances are common and include tachycardia, bradycardia, hypertens.ion, orthostatic hypotension, and urinary retention. Cerebral spinal fluid (CSF) analysis shows a high protein concentration with normal white blood cell (WBC) counts (albuminocytologic dissociation).Guillain-Barre syndrome (GBS) is characterized by ascending weakness, bulbar symptoms (eg, dysarthria, dysphasia) and respiratory compromise Gold standard treatment includes intravenous immunoglobulin or plasmapheresis. GBS patients are at risk of developing dysautonomia (eg, arrhythmias, orthostatic hypotension, urinary retention, ileus, lack of sweating) due to autonomic nervous system involvement. About two-thirds of patients also complain of severe pain in the back or extremities. Both IVIG and plasmapheresis are equally beneficial and the choice of treatment depends on patient-specific risk factors and availability. Deep-tendon reflexes are also normal in MG. The CT/MRI findings of a butterfly appearance with central necrosis is classic for GBM, and the heterogenous, serpiginous contrast enhancement is typical of high-grade astrocytoma. low-grade astrocytoma usually present with seizures, and have a longer duration of symptoms. Furthermore, contrast enhancement is less likely. Patients typically develop rapid onset of severe eye pain and may see halos around lights. The affected eye will appear injected and the pupil will be dilated and poorly responsive to light. Patients can also develop tearing and headache with subsequent nausea and vomiting as the intraocular pressure increases. Untreated acute ACG can lead to severe and permanent vision loss within 2-5 hours of symptom onset.Acute angle-closure glaucoma commonly occurs as a response to pupillary dilation from medications (eg, anticholinergics, sympathomimetics) or another stimulus (eg, dim light). Patients typically develop unilateral orbitofrontal headache associated with nausea/vomiting, unilateral eye pain with conjunctival injection, and a dilated pupil with poor light response. Optic neuritis (acute vision loss, pain, afferent pupillary defect) most commonly occurs in women age <50 and is often an initial presentation of multiple sclerosis. Optic neuritis is rarely associated with nausea/vomiting. In temporal arteritis, the erythrocyte sedimentation rate (ESR) is usually >50 mm/h. This patient's mildly elevated ESR may be due to her urinary tract infection. Seizures (UWorld): Evaluation of a first-time seizure: Metabolic (eg, hypoglycemia, electrolyte disturbances) and toxic (eg, amphetamine use, benzodiazepine/alcohol withdrawal) causes. Basic laboratory tests typically include serum electrolytes, glucose, calcium, magnesium, complete blood count, renal function tests, liver function tests, and a toxicology screen. ***If any of these are missing in the question, then this is the next step. THEN do CT & EEG. - Unprovoked, first seizure (CBC, electrolytes, EKG all normal): Get Computed tomography (CT) scan of the brain without contrast is as initial imaging study. **Important: get neuroimaging before you do EEG (which is next step) Helps to exclude acute neurologic problems (eg, intracranial or subarachnoid bleed) that might require urgent intervention. **MRI is more sensitive than CT in identifying most structural causes of epilepsy and is the neuroimaging modality of choice in elective situations. EEG is useful for risk-stratifying patients after a first-time seizure once metabolic and toxic etiologies have been excluded. The presence of epileptiform activity on an EEG indicates a higher risk of seizure recurrence and therefore may justify the need to start anti-epileptic therapy. Brain that has seized for >5 minutes is at increased risk of developing permanent injury due to excitatory cytotoxicity. - Cortical laminar necrosis is the hallmark of prolonged seizures and can lead to persistent neurologic deficits and recurrent seizures. Phenytoin and alcohol abuse can cause cerebellar atrophy. Status epilepticus: any single seizure lasting >5 minutes or a cluster of seizures with the patient not recovering a normal mental status in between. Woman of reproductive age: NEVER give valproic acid. Q60:





![[Physician Letterhead] [Select Today`s Date] . [Name of Health](http://s3.studylib.net/store/data/006995683_1-fc7d457c4956a00b3a5595efa89b67b0-300x300.png)